Xen Gel Stent Implantation with Deep Sclerectomy in the Management of Neovascular Glaucoma
Article Information
Cenk ZEKI FIKRET
Ankara City Hospital, Department of Ophthalmology, Ankara, Turkey
*Corresponding author: Cenk ZEKI FIKRET, Ankara City Hospital, Department of Ophthalmology, Ankara Sehir Hastanesi, Universiteler Mahallesi, Turkey.
Received: 31 January 2022; Accepted: 07 February 2022; Published: 09 February 2022
Citation: Cenk ZEKI FIKRET. Xen Gel Stent Implantation with Deep Sclerectomy in the Management of Neovascular Glaucoma. Journal of Ophthalmology and Research 5 (2022): 29-34.
Share at FacebookAbstract
Background: To evaluate the efficacy and safety profile of Xen gel stent implantation combined with deep sclerectomy in eyes with neovascular glaucoma.
Methods: Twenty five patients with neovascular glaucoma due to central retinal vein occlusion were included in our study. Panretinal photocoagulation treatment was completed within a break period of two weeks. Intravitreal 0.05 ml bevacizumab was injected seven days before surgery. Despite iris and angle neovascularization regression, full antiglaucomatous treatment to patients whose intraocular pressures (IOP) were 21mm Hg and above were operated. Xen gel stent implantation with deep sclerectomy was performed to all patients. Complete success was defined as IOP ≤18 mm Hg and ≥20% IOP reduction without antiglaucomatous medication and another IOP lowering procedure. Partial success was defined as IOP ≤18 mm Hg and ≥20% IOP reduction with antiglaucomatous medi-cation or needling. Surgical failure was considered in eyes requiring a secondary antiglaucomatous surgery.
Results: The mean preoperative IOP was 35.88±8.24 mm Hg under medication, which was reduced to 14.92±1.68 mm Hg at the 1st year visit (p<0.001). Complete success occurred in 15 (60%) patients and partial success occurred in 9 (36%) patients after surgery. Ahmed glaucoma valve implantation was performed in one patient at the end of the first month due to surgical failure (4%).
Conclusion: Xen gel stent implantation with deep sclerectomy is demonstrated to be an effective treatment with a good safety profile in neovascular glaucoma patients at the 1 year follow-up period.
Keywords
Xen gel stent; deep sclerectomy; neovascular glaucoma; central retinal vein occlusion; glaucoma
Article Details
1. Intruduction
Neovascular glaucoma (NVG) develops in central retinal vein occlusions (CRVO), within 3 months a frequency of 13%. In ischemic central retinal vein occlusions, this rate varies between 22-50%. NVG that develops secondary to CRVO is actually known as 100 day glaucoma. After the development of central retinal vein occlusion, the time to develop neovascular glaucoma was found to be 421 days. Therefore, anti-vascular endothelial growth factor (anti-VEGF) injections are effective in prolonging this period. In intravitreal anti-VEGF injected eyes, this period has been reported to be 212 days after the last injection [1].
Primarily, treatment of neovascularization in the iris and angle should be aimed with panretinal photocoagulation and intravitreal anti-VEGF injections. Topical β-blockers, topical α-agonists, topical and oral carbonic anhydrase inhibitors can be used in intraocular pressure (IOP) control by reducing aqueous production. Since prostaglandin analogues act by increasing the uvea-scleral output, their effect is less in patients with neovascular glaucoma due to the fibrovascular structures at the angle. Surgical treatment is required in patients in whom the targeted intraocular pressures cannot be achieved with medical treatment [2, 3].
The filtering surgical procedure commonly used in NVG is trabeculectomy with mitomycine C or 5-fluororacil. NVG is one of the most common causes of bleb failure in trabeculectomy. Glaucoma drainage devices are used to increase surgical success in NVG. Xen gel stent is one of the minimally invasive glaucoma drainage devices [2, 4, 5]. Xen gel stent is a hydrophilic tube made with a gelatine and cross-linked with glutaraldehyde. The current version of the implant in our country is Xen 45. The Xen 45 gel stent is 6.0 mm long and has a 45 μm lumen inner diameter. Although the Xen gel stent is rigid when it’s dry, it becomes flexible when hydrated. This stent is designed without a valve in order to create resistance to outflow at pressures below 6-8 mmHg. It is reported that it works in accordance with the Hagen-Poiseuille principle [6].
When trabeculectomy surgery is performed in eyes with high IOP, it may cause some complications like hyphema, hypotony, shallow anterior chamber, choroidal detachment. These complications are less common in the deep sclerectomy procedure. We applied deep sclerectomy with Xen gel implantation simultaneously to increase surgical success and prevent complications. In this study, we evaluated the effects of deep sclerectomy with Xen gel stent implantation in eyes with neovascular glaucoma.
2. Methods
This study was performed in accordance with the tenets of the Declaration of Helsinki and Ankara City Hospital Ethics Committee approved the protocol for the study (E1-21-1648). Written informed consent was obtained from all patients. Twenty five pseudophakic eyes of 25 patients with neovascular glaucoma due to central retinal vein occlusion were included in our study. First of all, argon laser panretinal photocoagulation and intravitreal injection of 0.05 ml bevacizumab (Altuzan 100mg/4ml, Roche) were applied to the patients. Patients whose intraocular pressures were 21 mm Hg and above under full antiglaucomatous treatment were taken to surgery. It was ensured that the iris and angle neovascularization in the eyes were regressed preoperatively.
Postoperative visits were done at the 1st week, 1st, 3rd, 6th and first year. Complete success was determined as an eye with IOP ≤18 mm Hg and ≥20% IOP reduction without antiglaucomatous medication and another IOP lowering procedure. Partial success was determined as IOP ≤18 mm Hg and ≥20% IOP reduction with antiglaucomatous medication or needling. Surgical failure was considered in eyes requiring a second antiglaucomatous surgery. IOP was measured using Goldmann applanation tonometry. Surgical procedure: All surgeries were performed under topical anesthesia and steril condition by placing sterile drapes. Fornix-based conjunctiva and tenon's membrane were dissected. 4×4 mm2 in size one-third of the scleral thickness superficial scleral flap was executed at 12 o'clock. Triangular sponge soaked with Mitomycin-C (MMC) (0.2 mg/mL) is applied under the superficial scleral flap for 2 minutes then irrigated by 20 ml balanced salt solution (BSS). Deep scleral flap (3 × 3 mm2) is then formed up to the Schlemm canal to create a trabeculodescemet membrane. The deep flap is excised. The outher wall of the Schlemm’s canal was removed and aqueous percolation ‘’oozing’’ occured.
The anterior chamber is entered with a 27 G needle under the scleral flap parallel to the iris plane and The Xen 45 gel stent was taken out of the neede manually and was implanted 1mm in to the anterior chamber from the beginning of the blue zone . Xen implant was sutured 2 mm from the limbus to scleral bed with one 10/0 nylon sutur. The superficial scleral flap was sutured to the sclera with 10-0 nylon sutures at the two corners. The tip of the Xen implant was placed 1 mm outside the upper edge of the superficial scleral flap. After controlling the presence of flow by applying BSS to the anterior chamber, the tenon and conjunctiva were sutured continuously with 8-0 vicryl suture. All data were processed into SPSS (version 20) for statistical analysis. All parameters used in our study is written as mean ± standard deviation (SD). p<0.05 was taken as the significance level. The Repeated Measure Anova test was used to compare the preoperative, 1st week, 1st month, 3rd month, 6th month and 1st year IOP measurements of the patients.
3. Results
The mean age of the patients was 59.72 ± 4.62 years. Sixteen (64%) of the patients were male and 9 (36%) of them were male. All patients’ follow up was completed to the first year. After surgical procedure, the mean change in IOP (mm Hg) was -43.20±7.16, -53.56±8.82, -58.36±9.81, -57.57±9.00, -56.75±9.16 at 1 week, and 1, 3, 6 months and 1 year.
Complete success occurred in 15 (60%) patients and partial success occurred in 9 (36%) patients 1 year after surgery. Ahmed glaucoma valve implantation was performed in one patient at the end of the first month due to surgical failure (4%).
Table 1: Preoperative and postoperative IOP values
|
Time |
Complete success IOP mm Hg mean ±SD n=15 |
Partial success |
Total |
P value* |
|
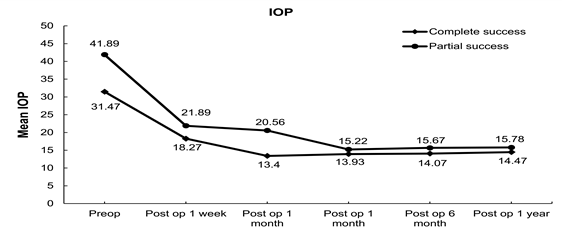
Preoperative |
31.47±5.31 |
41.89±7.68 |
35.88±8.24 |
<0.001 |
|
Postoperative 1. week |
18.27±1.75 |
21.89±2.47 |
19.96±3.11 |
<0.001 |
|
Postoperative 1. month |
13.40±1.63 |
20.56±1.42 |
16.48±4.26 |
<0.001 |
|
Postoperative 3. month |
13.93±2.01 |
15.22±1.39 |
14.32±1.90 |
<0.001 |
|
Postoperative 6. month |
14.07±1.58 |
15.67±1.41 |
14.64±1.65 |
<0.001 |
|
Postoperative 1. year |
14.49±1.64 |
15.78±1.56 |
14.92±1.68 |
<0.001 |
In Table 1, the mean IOP values of the patients before and after surgery are reported.
Preoperative and postoperative IOP changes of the patients with complete and partial success at 1 week, 1 month, 3 months, 6 months and 12 months are shown in Figure 1.
Table 2: Postoperative treatment status
|
Treatment Status |
n |
% |
|
No additional treatment |
15 |
60 |
|
Topical antiglaucomatous |
6 |
24 |
|
Needling |
3 |
12 |
|
Secondary surgery |
1 |
4 |
Postoperative treatment conditions are reported in Table 2. No complications such as hyphema, hypotony, shallow anterior chamber, choroidal detachment or implant dislocation occurred during or after surgery in our patients.
4. Discussion
Xen gel stent is an effective, safe and minimally invasive glaucoma drainage device in the treatment of primary open angle glaucoma. It is reported in the literature that the Xen gel stent reduces IOP by 25 to 56 % (mean 42%). When trabeculectomy and Xen gel stent implantation results were compared, no difference was found in the failure and safety profile. Complication rates were found to be higher in patients who underwent trabeculectomy when compared to patients who underwent Xen gel stent. The most common complications are hypotonia and choroidal effusion after trabeculectomy (5% and 10%). In the literature, these rates were found to be 1.5% for the Xen gel stent. However, it has been reported that needling rates are higher in eyes with Xen gel stent implanted [8, 9].
The advantage of deep sclerectomy over trabeculectomy is that deep sclerectomy does not cause excessive filtration and hypotonia. In deep sclerectomy surgery, space occupying devices are used as a space maintainer to create a permanent intrascleral lake and to prevent collapse of the scleral flap and impairment of the scleral drainage. Thus, inadequate scleral drainage can be avoided. Collagen implants combined with deep sclerectomy have been reported to increase bleb size and further reduce IOP [10, 11]. Kozobolis et al. developed the penetrating deep sclerectomy method in primary open-angle and pseudoexfoliative glaucoma. They reported the success rate without medication as 58.6%, with and without medication as 75.86% at the end of 3 years follow up [12].
Urcola et al. applied Xen implantation to 40 eyes of 20 patients and achieved 70% complete success [13]. In the literature, there was a case report indicating Xen implant application in NVG. They reported that IOP control was still sufficient at the end of 2 years follow-up [14]. Gupta and Mathews reported migration of the Xen stent into the anterior chamber or under the conjunctiva [15]. In our patients, we prevented implant dislocation by suturing the Xen gel implant to the scleral bed.
Our surgical success rate in patients with neovascular glaucoma is 60% and incomplete success rates are 36%. We provided a standard penetration into the anterior chamber and a permanent scleral bed by applying Xen gel stent implantation together with deep sclerectomy. IOP control is difficult in neovascular glaucoma surgeries. It is understood that the simultaneous application of Xen gel stent and deep sclerectomy is beneficial in order to increase the surgical success rates. Best of our knowledge, our study is the first to report the results of Xen gel stent implantation combined with deep sclerectomy in neovascular glaucoma.
Acknowledgements
Funding:
The authors do not have any funding support for the study.
Conflict of interest:
None of the authors has any conflict of interest.
References
- Rong AJ, Swaminathan SS, Vanner EA, Parrish RK 2nd. Predictors of Neovascular Glaucoma in Central Retinal Vein Occlusion. Am J Ophthalmol 204 (2019) :62-69.
- Havens SJ, Gulati V. Neovascular Glaucoma. Dev Ophthalmol 55 (2016):196-204.
- Bhagat PR, Agrawal KU, Tandel D. Study of the Effect of Injection Bevacizumab through Various Routes in Neovascular Glaucoma. J Curr Glaucoma Pract 10 (2016):39-48.
- Shchomak Z, Cordeiro Sousa D, Leal I, Abegão Pinto L. Surgical treatment of neovascular glaucoma: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 257 (2019):1079-1089.
- Hayreh SS. Neovascular glaucoma. Prog Retin Eye Res 26 (2007):470-85.
- Sheybani A, Reitsamer H, Ahmed II. Fluid Dynamics of a Novel Micro-Fistula Implant for the Surgical Treatment of Glaucoma. Invest Ophthalmol Vis Sci 56 (2015):4789-95.
- Shaaraway TM, Sherwood MB, Grehn F, eds. World Glaucoma Association. Guidelines on design and reporting of glaucoma surgical trials. Accessed 15 May (2019).
- Buffault J, Baudouin C, Labbé A. XEN® Gel Stent for management of chronic open angle glaucoma: A review of the literature. J Fr Ophtalmol 42 (2019): e37-e46.
- Schlenker MB, Gulamhusein H, Conrad-Hengerer I, Somers A, Lenzhofer M, Stalmans I, et al. Efficacy, Safety, and Risk Factors for Failure of Standalone Ab Interno Gelatin Microstent Implantation versus Standalone Trabeculectomy. Ophthalmology 124 (2017):1579-1588.
- Roy S, Mermoud A. Deep Sclerectomy. Dev Ophthalmol 59 (2017):36-42.
- Elmekawey H, Abdelrahman A, Kotb MS, Mostafa DA. Effect of filtering bleb dimensions on postoperative intraocular pressure in deep sclerectomy with collagen implant: a comparative study. Int Ophthalmol 40 (2020):7-12.
- Kozobolis V, Kalogianni E, Sideroudi H. Penetrating deep sclerectomy in primary open-angle and pseudoexfoliative glaucoma. Eur J Ophthalmol 30 (2020):264-268.
- Urcola A, Garay-Aramburu G. Safety and efficacy of bilateral simultaneous XEN implant surgery: a pilot study. Int Ophthalmol 41 (2021):859-866.
- Tailor R, Lalias T. A Case of Refractory Neovascular Glaucoma Treated With a XEN 45 Implant. J Glaucoma. 27 (2018): 929-930.
- Gupta C, Mathews D. XEN® stent compli-cations: a case series. BMC Ophthalmol 19 (2019) :253.