Weight Growth of Low Birth Weight Infants According to the Type of Breastfeeding
Article Information
Gueye Modou1, Sow Amadou1*, Sow Aminata2, Cisse Dieynaba Fafa2, Ly Fatou2, Boiro Djibril1, Ngola Glen2, Dieng Yaay Joor3, Papa Moctar Faye3, Boubacar Camara2, Ousmane Ndiaye3
1Abass Ndao Hospital Center, Dakar, Senegal
2Pikine Hospital Center, Dakar, Senegal
3Albert Royer Children's National Hospital, Dakar, Senegal
*Corresponding Author: Amadou Sow, Pediatrician, University Hospital Center of Dakar, Senegal
Received: 26 June 2020; Accepted: 20 July 2020; Published: 24 July 2020
Citation:
Gueye Modou, Sow Amadou, Sow Aminata, Cisse Dieynaba Fafa, Ly Fatou, Boiro Djibril, Ngola Glen, Dieng Yaay Joor, Papa Moctar Faye, Boubacar Camara, Ousmane Ndiaye. Weight Growth of Low Birth Weight Infants According to the Type of Breastfeeding. Journal of Pediatrics, Perinatology and Child Health 4 (2020): 065-072.
Share at FacebookAbstract
Introduction: Breastfeeding is the benchmark for feeding infants during the first months of life, regardless of their birth weight. The objective of our study was to compare the weight growth of a cohort of low birth weight (LBW) newborns in the first 6 months of life according to the type of breastfeeding adopted by the mother.
Methodology: It was a prospectiveand analytical study of a cohort of newborns from LBW. It took place over a period of 17 months at the level of a reference structure in Dakar. We have included all newborns born “in-born” weighing less than 2500 g with a threshold of 1000 g. The data was analyzed with SPSS version 17 software.
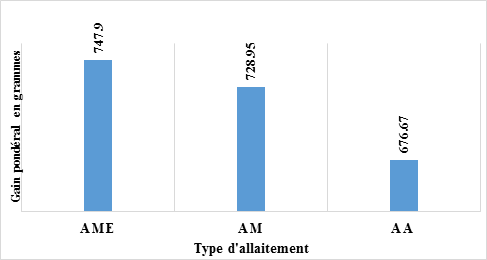
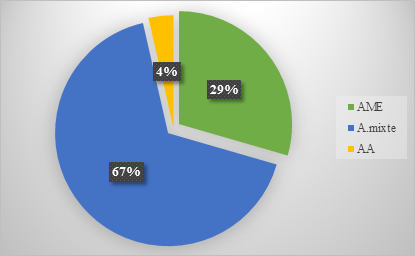
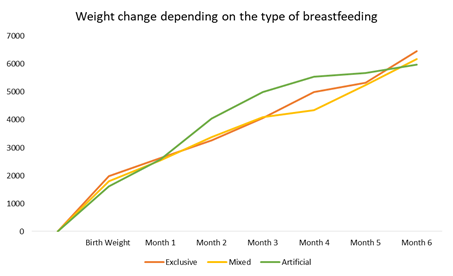
Results: The average birth weight of newborns was 1821.8 g with extremes ranging from 1000 g to 2400 g and the median weight of 1840 g. The majority of our population had a birth weight ≥ 1500 g (83%) with more than half of them being premature (58.9%). Depending on the type of breastfeeding adopted by the mother, 33/112 newborns were on exclusive breastfeeding (EBF). During the first 6 months of life, the average weight gain was significantly better in infants on EBF (747.9 g) compared to infants on mixed breastfeeding (728.9 g) and artificial breastfeeding (676.6 g).
Conclusion: Better awareness of mothers should be made during hospitalization and during follow-up consultations for newborns of LBW to encourage the continuation of the EBF which remains the best food for this infant population.
Keywords
New-born, Growth, Weight, Breastfeeding, Dakar
New-born articles, Growth articles, Weight articles, Breastfeeding articles, Dakar articles
Article Details
1. Introduction
Low birth weight (LBW) is defined as a birth weight less than 2500 g [1]. Its prevalence remains very high worldwide. In 2015, 20.5 million children were born with a LBW, or around one in 7 births worldwide. Almost 90% of these births take place in low- and middle-income countries, particularly in South Asia and sub-Saharan Africa [2]. In Senegal, its national prevalence is estimated at 12% of live births [3]. These figures are certainly underestimated and the prevalence of LBW poorly evaluated since in many developing countries, there are still a large number of home births which escape national statistics and even when these births are counted, the birth weight is not always known, thus generating considerable missing data [2, 4]. At the level of referral hospital structures, the prevalence of LBW seems even higher with rates sometimes approaching 30% [5]. LBW represents an increased risk of morbidity and neonatal mortality worldwide [6]. In addition to these immediate complications, there is the risk of developing metabolic and cardiovascular diseases in adulthood, as shown by the work of Barker [7]. The occurrence of these short- and long-term consequences depends very much on the quality of the infant's initial nutrition. Breastfeeding is the benchmark for infant feeding during the first months of life. It promotes the physical and emotional growth of the child, favors the mother-child bond and strengthens the immunity of the child. Breast milk contains all the nutrients that an infant needs during the first six months of life to ensure satisfactory growth and protect him from disease [8]. Therefore, all newborns and infants, including those with low or very low birth weight, should be fed their mother's milk [9]. Despite everything, for various reasons [10] (lack of information, lack of lactation, resumption of professional activity, hospitalization at birth, etc.), the rate of exclusive breastfeeding (EBF) remains low worldwide. In fact, only 43% of infants under the age of six months are fed exclusively with breast milk worldwide; this rate is 42% in Senegal [3].
The objective of our study was to compare the weight growth of a cohort of newborn infants in the first 6 months of life according to the type of breastfeeding adopted by the mother.
2. Methodology
It was a prospective, observational, descriptive and analytical study of a cohort of low birth weight infants. It took place over a period of 17 months from October 2016 to March 2018 at the Center National Hospital of Pikine. This hospital represents a benchmark public health structure with a large influx of people from the Dakar suburbs. With a capacity of 12 beds including 4 incubators, the neonatology service receives an average of 1000 newborns per year. The populations admitted to it often have low incomes. We have included all newborns born “in-born” weighing less than 2500 g with a threshold of 1000g. Out-born LBW as well as those with severe birth defects were excluded from our study. The parameters studied were the age of the mother, profession, parity, maternal pathologies during pregnancy, monitoring of pregnancy and gestational age. In the newborn we studied gender, birth weight, type of low birth weight, type of breastfeeding adopted by the mother, monthly weight gain. Data were collected from hospital records and follow-up of low birth weight infants. The gestational age in weeks of amenorrhea (WA) was determined from the date of the last period recorded on the health book or from early ultrasound. Otherwise, the calculation of the BALLARD neuro-morphological score was used [11]. During the follow-up, the weight was collected with an electronic balance with a precision of 10 g.
3. Results
Our study involved a cohort of 112 newborns of LBW out of a total of 3,399 live births at the hospital maternity, a prevalence of 3.33%. The majority of mothers were between the ages of 18 and 35. They had no professional activity (95%) and were poor in the majority of cases (32.1%). The sex ratio was 0.78. The average birth weight of newborns was 1821.8 g with extremes ranging from 1000 g to 2400 g and the median weight of 1840 g. The majority of our population had a birth weight ≥ 1500 g (83%) with more than half of them being premature (58.9%). Table 1 shows the characteristics of mothers and newborns at birth. Depending on the type of breastfeeding adopted by the mother, 33 newborns were on exclusive breastfeeding (EBF), 75 on mixed breastfeeding (MB) and 4 on artificial breastfeeding (AB) or 3.57% (Figure 1). During the first 6 months of life, the average weight gain was 747.9 g in infants on EBF, 728.9 g in infants on MB and 676.6 g in infants on AB (Figure 2). Regarding the growth of newborns, we noted a better growth of newborns on EBF with superimposable growth of the 3 curves during the first month than a nearly linear trend in the weight curve of infants under exclusive breastfeeding whereas the growth of infants on mixed and artificial breastfeeding was less regular (Figure 3).
|
Characteristics |
Workforce (N = 106) |
Percentage(%) |
|
Maternal age |
||
|
<18 years old |
1 |
0.98 |
|
18-35 years old |
89 |
84.1 |
|
Over 35 |
16 |
15.1 |
|
Maternal profession N = 106 |
||
|
Official |
6 |
5.6 |
|
Shopkeeper |
5 |
4.7 |
|
Unemployed |
95 |
89.7 |
|
Parity |
||
|
Primiparous |
49 |
43.8 |
|
Pauciparous (2-3) |
36 |
32.1 |
|
Multipar (≥ 4) |
27 |
24.1 |
|
Pathologies during pregnancy |
||
|
Pre eclampsia / eclampsia |
18 |
16.9 |
|
Urogenital infection |
16 |
15.1 |
|
Twin pregnancy |
6 |
5.6 |
|
Diabetes |
3 |
2.8 |
|
Asthma |
3 |
2.8 |
|
Other |
5 |
4.7 |
|
Pregnancy visit |
||
|
≤ 3 |
78 |
73.5 |
|
> 3 |
28 |
26.5 |
|
Term of pregnancy (AW) |
||
|
> 28 AW |
1 |
0.9 |
|
28 - 32 |
11 |
10.4 |
|
33 - 36 |
77 |
72.6 |
|
≥ 37 |
17 |
16.1 |
|
Sex |
||
|
Male |
50 |
43.7 |
|
Feminine |
62 |
55.3 |
|
Birth weight |
||
|
≤ 1500 |
19 |
17 |
|
> 1500 |
93 |
83 |
|
LBW type |
||
|
Premature |
66 |
58.9 |
|
Hypotrophy |
20 |
17.9 |
|
Prematurity + hypotrophy |
26 |
23.2 |
Table 1: General characteristics of mothers and newborns at birth.
AME: Exclusive breastfeeding; AM: Mixed breastfeeding; AA: Artificial breastfeeding
AME: Exclusive breastfeeding; AM: Mixed breastfeeding; AA: Artificial breastfeeding
4. Discussion
LBW is one of the leading causes of morbidity and neonatal mortality in the world [12]. Its prevalence is low in our service compared to hospital data at the national and African level [5, 13]. The systematic transfer of our structure to other reference hospitals in the Dakar region of certain high-risk pregnancies, particularly very low birth weight (BW <1000 g) could explain this low prevalence. In our cohort, we noted a clear predominance of women. This result is reported by several authors [14, 15]. It could be linked to the higher rate of female births in the world. LBW is often associated with mild or moderate prematurity. Globally, 80% of premature births are moderate with a weight greater than 1500 g [2]. This very high proportion of light to moderate prematurity justifies the adoption, in low-income countries, of certain simple, effective and inexpensive strategies such as the Kangaroo method of care which, in addition to protection against hypothermia promotes the initiation and continuation of exclusive breastfeeding [16-18]. Breast milk regardless of birth weight is the benchmark for infant feeding during the first 6 months of life. It strengthens its immunity and promotes its physical growth [8]. The prevalence of LBW in Senegal from 2010 to 2017 increased from 39% to 42%, which proves that a lot of efforts have been made to raise awareness of EBF [3, 19]. In our work, only 29% of children have benefited from an EBF. It should be noted that there is sometimes a very long delay between birth and the time when feeds become effective in newborns of LBW. Also, the success of breastfeeding is sometimes more complicated in EBF infants, especially when they are hospitalized at birth, as is often the case in this population [20]. So in developed countries, faced with the need to feed these infants with human milk, the choice was made to set up milk banks. In our countries with limited resources, given the high cost of donor milk and the logistics necessary to manage such structures [21], the best alternative seems to be the development of mother-child kangaroo units which encourage the pursuit of breastfeeding throughout the child's hospital stay [16-18].
In our series, EBF was associated with better weight gain compared to MB and AB with growth that is more stable and more regular. These results confirm the results reported by Li Yong-Wei [22] on the benefits of breastfeeding compared to artificial breastfeeding on weight growth of premature infants in neonatal intensive care unit. Indeed, although the amount of protein in breast milk is much lower compared to cow's milk, the proteins in breast milk benefit from better bioavailability with optimal absorption thus allowing better growth of the child [8]. In addition to these weight-gaining benefits, in hospitalized LBW newborns, there is a significant reduction in the risk of ulcerative enterocolitis, a shortening of the time for complete enteral feeding and the length of stay, a reduction in the burden of staff work and the cost of hospitalization [23]. However, this better growth of children under breast milk is not found by some authors. Indeed, Quigley et al. [24], in a meta-analysis, which compared infant formula with mother or donor milk, found better growth in weight, size and head circumference of children under formula. The digestive tolerance of infant formula was also lower with a significant increase in the risk of developing ulcerative necrotizing enterocolitis. The poor growth of infants on exclusive AB could be explained by the difficulty of implementing this food method and its cost. It should be noted that in our context AB is rarely chosen by mothers.
5. Conclusion
Exclusive breastfeeding remains the best LBW infant food in our context. Thus, a better awareness of mothers should be made during hospitalization and during follow-up consultations for newborns of LBW to encourage the continuation of EBF which remains weak in our country.
Conflicts of Interest
No
References
- International statistical classification of diseases and related health problems. 10th revision ICD-10 version (2014).
- Tanya Doherty, Mary Kinney. Low birth weight: will new estimates accelerate progress? Lancet Glob Health 7 (2019): 809-810.
- National Agency for Statistics and Demography (ANSD) [Senegal], and ICF. Senegal: Demographic and Continuous Health Survey (EDS-Continue 2017). Rockville, Maryland, USA: ANSD and ICF (2018).
- UNICEF-WHO. Low birth weight: country and regional estimates, UNICEF and WHO 9 (2004): 2-3.
- Ndiaye O, Fall AL, Drama A, et al. Etiological factors of prematurity at the regional hospital center of Ziguinchor Senegal. Bull Soc Patho Exot 99 (2006): 113-114.
- For each child, a chance to experience the urgency of ending neonatal mortality (2018).
- Barker DJ. The fetal and infant origins of adult diseases. Br Med J 301 (1990).
- Tackoen M. Breast milk: nutritional composition and functional properties. Rev Med Brux 33 (2012): 309-317.
- World Health Organization. Guidelines on optimal feeding of low birthweight infants in low-and middle-income countries. ISBN 978 92 4 154836 6 (2011).
- Neifert M, Bunik M. Overcoming Clinical Barriers to Exclusive Breastfeeding. Pediatr Clin N Am 60 (2013): 115-145.
- Ballard JL. A simplified score for assessment of fetal maturation of newly born infants. J. Pediatr 95 (1979): 769-774.
- World Health Organization. Newborns: reduce mortality (2018).
- Mabiala-Babela JR, Matingou VC, Senga P. risk factors for low birth weight in Brazzaville Congo. J Gynecol Obstet Biol Reprod 136 (2007): 795-798.
- Diouf FN, Faye PM, Gueye M, et al. Socio-demographic, epidemiological, clinical and prognostic aspects of prematurity in the neonatology unit of the Albert Royer Child Hospital in Dakar/Senegal Rev. Health Cams 4 (2016): 19-24.
- PM Faye, NR Diagne-Guèye, IL Paraiso A, et al. Postnatal weight gain in newborns with low birth weight in the neonatology department of the Albert Royer National Children's Hospital: incidence of ectopic growth retardation. J Pediatr Pueric 29 (2016): 20-27.
- Charpak N, Ruiz PJG, Figueroa DCZ, et al. Kangaroo mother versus traditional care for newborn infants <2000 grams: a randomized controlled trial. Pediatrics 100 (1997): 682-688.
- Faye PM, Thiongane A, Diagne-Gueye NR, et al. Kangaroo care for newborns with low birth weight at the Albert-Royer National Children's Hospital in Dakar. Arch. Pediatr 23 (2016): 268-274.
- Mekonnen AG, Yehualashet SS, Bayleyegn AD. The effects of kangaroo mother care on the time to breastfeeding initiation among preterm and LBW infants: a meta-analysis of published studies. Int Breastfeed J 14 (2019): 12.
- Diagne-Guèye NR, Diack-Mbaye A, Dramé M. Knowledge and practices of Senegalese mothers living in rural or suburban areas on the feeding of their children, from birth to the age of six months. J Pediatr Pueric 24 (2011): 161-166.
- Hoban R, Bigger H, Patel AL, et al. Goals for Human Milk Feeding in Mothers of Very Low Birth Weight Infants: How Do Goals Change and Are They Achieved During the NICU Hospitalization? Breastfeed Med 10 (2015): 305-311.
- Fengler J, Heckmann M, Lange A, et al. Cost analysis showed that feeding preterm infants with donor human milk was significantly more expensive than mother's milk or formula Acta Pediatrica 00 (2019): 1-8.
- Li Yong-Wei, Yan Chao-Ying, Yang Lei, et al. Effect of breastfeeding versus formula milk feeding on preterm infants in the neonatal intensive care unit. CJCP 19 (2017): 572-575.
- Assad M, Elliott MJ and JH Abraham JH. Decreased cost and improved feeding tolerance in VLBW infants fed an exclusive human milk diet. J Perinatology (2015): 1-5.
- Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev 6 (2018): CD002971.