Ways to Improve Workflow and Morale in an Ophthalmology Clinic: Survey Advice from Clinic Staff
Article Information
Rebekah C Smith1, Terisa Yiin2, Cindy Monelavongsy3, Cherrie Soledad Tan4, Marta Rodriguez4, Michele C. Lim4, Yin Allison Liu4,5*
1School of Medicine, University of California Davis, X St, Sacramento, 95817, California, USA
2College of Medicine, University of Central Florida, Lake Nona Blvd, Orlando, 32827, Florida, USA
3Department of Internal Medicine, Office of Population Health and Accountable Care, University of California Davis, V St, Sacramento, 95817, California, USA
4Department of Ophthalmology, University of California Davis, Y St, Sacramento, 95817, California, USA
5Departments of Neurology and Neurosurgery, University of California Davis, Y St, Sacramento, 95817, California, USA
*Corresponding author: Yin Allison Liu, Department of Ophthalmology, University of California Davis, Y St, Sacramento, 95817, California, USA.
Received: 21 September 2023; Accepted: 26 September 2023; Published: 06 October 2023
Citation: Rebekah C Smith, Terisa Yiin, Cindy Monelavongsy, Cherrie Soledad Tan, Marta Rodriguez, Michele C. Lim, Yin Allison Liu. Ways to Improve Workflow and Morale in an Ophthalmology Clinic: Survey Advice from Clinic Staff. Journal of Biotechnology and Biomedicine. 6 (2023): 460-467.
Share at FacebookAbstract
Objective: We aim to improve job workflow and satisfaction amongst clinic staff at an academic ophthalmology department.
Methods: We analyzed survey data given over a 2-week period in July 2021. The participants were support staff (N = 18) from an academic ophthalmology department. Paper surveys were distributed to participants and returned anonymously for analysis.
Results: The survey contained 9 Likert-style categorical questions, 2 of which were free response options. A total of 22 participants attempted the survey, 18 of these (82%) were complete and included in analysis. About half of the staff were satisfied with the current workflow 10/18 (56%). Staff who were clinical care coordinators had the lowest average satisfaction (2/5 on a 5-point scale) and the nursing team had the highest average (4.75/5). The most common staff suggestion for improving workflow efficiency was to train residents on forwarding and answering messages more effectively.
Conclusion: This survey suggests that assigning patient message processing to the nursing staff can improve job satisfaction and workflow. Staff told us that the most exciting part of the job was appreciation from coworkers 9/30 (30%) and from physicians 8/30 (27%). The findings provide advice to physicians for optimizing communication, and staff experience, within their own ophthalmology clinics.
Keywords
Workflow efficiency; Job satisfaction; Survey results
Workflow efficiency articles Workflow efficiency Research articles Workflow efficiency review articles Workflow efficiency PubMed articles Workflow efficiency PubMed Central articles Workflow efficiency 2023 articles Workflow efficiency 2024 articles Workflow efficiency Scopus articles Workflow efficiency impact factor journals Workflow efficiency Scopus journals Workflow efficiency PubMed journals Workflow efficiency medical journals Workflow efficiency free journals Workflow efficiency best journals Workflow efficiency top journals Workflow efficiency free medical journals Workflow efficiency famous journals Workflow efficiency Google Scholar indexed journals Job satisfaction articles Job satisfaction Research articles Job satisfaction review articles Job satisfaction PubMed articles Job satisfaction PubMed Central articles Job satisfaction 2023 articles Job satisfaction 2024 articles Job satisfaction Scopus articles Job satisfaction impact factor journals Job satisfaction Scopus journals Job satisfaction PubMed journals Job satisfaction medical journals Job satisfaction free journals Job satisfaction best journals Job satisfaction top journals Job satisfaction free medical journals Job satisfaction famous journals Job satisfaction Google Scholar indexed journals Survey results articles Survey results Research articles Survey results review articles Survey results PubMed articles Survey results PubMed Central articles Survey results 2023 articles Survey results 2024 articles Survey results Scopus articles Survey results impact factor journals Survey results Scopus journals Survey results PubMed journals Survey results medical journals Survey results free journals Survey results best journals Survey results top journals Survey results free medical journals Survey results famous journals Survey results Google Scholar indexed journals Healthcare articles Healthcare Research articles Healthcare review articles Healthcare PubMed articles Healthcare PubMed Central articles Healthcare 2023 articles Healthcare 2024 articles Healthcare Scopus articles Healthcare impact factor journals Healthcare Scopus journals Healthcare PubMed journals Healthcare medical journals Healthcare free journals Healthcare best journals Healthcare top journals Healthcare free medical journals Healthcare famous journals Healthcare Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals equipment articles equipment Research articles equipment review articles equipment PubMed articles equipment PubMed Central articles equipment 2023 articles equipment 2024 articles equipment Scopus articles equipment impact factor journals equipment Scopus journals equipment PubMed journals equipment medical journals equipment free journals equipment best journals equipment top journals equipment free medical journals equipment famous journals equipment Google Scholar indexed journals energy articles energy Research articles energy review articles energy PubMed articles energy PubMed Central articles energy 2023 articles energy 2024 articles energy Scopus articles energy impact factor journals energy Scopus journals energy PubMed journals energy medical journals energy free journals energy best journals energy top journals energy free medical journals energy famous journals energy Google Scholar indexed journals ophthalmology articles ophthalmology Research articles ophthalmology review articles ophthalmology PubMed articles ophthalmology PubMed Central articles ophthalmology 2023 articles ophthalmology 2024 articles ophthalmology Scopus articles ophthalmology impact factor journals ophthalmology Scopus journals ophthalmology PubMed journals ophthalmology medical journals ophthalmology free journals ophthalmology best journals ophthalmology top journals ophthalmology free medical journals ophthalmology famous journals ophthalmology Google Scholar indexed journals anonymous articles anonymous Research articles anonymous review articles anonymous PubMed articles anonymous PubMed Central articles anonymous 2023 articles anonymous 2024 articles anonymous Scopus articles anonymous impact factor journals anonymous Scopus journals anonymous PubMed journals anonymous medical journals anonymous free journals anonymous best journals anonymous top journals anonymous free medical journals anonymous famous journals anonymous Google Scholar indexed journals Demographic articles Demographic Research articles Demographic review articles Demographic PubMed articles Demographic PubMed Central articles Demographic 2023 articles Demographic 2024 articles Demographic Scopus articles Demographic impact factor journals Demographic Scopus journals Demographic PubMed journals Demographic medical journals Demographic free journals Demographic best journals Demographic top journals Demographic free medical journals Demographic famous journals Demographic Google Scholar indexed journals
Article Details
Introduction
Healthcare quality and safety in the United States are subjects of continuous importance. The National Academy of Medicine addresses this by discussing guidelines for healthcare professionals in two major works [1,2]. Our study addresses two of the six specific aims detailed in Crossing the Quality Chasm [1]. First is ‘timely’ care – avoiding delays which cause harm to patients and providers. Second is ‘efficient’ care – preventing unnecessary waste of equipment, supplies, and energy. Both timeliness and efficiency affect a clinic’s workflow, which are the steps that people take to complete their job responsibilities [3]. An ideal workflow requires minimal time and uses staff energy, equipment, and supplies efficiently. In the field of Ophthalmology clinics have had to reorganize their prior workflows and practices due to the COVID-19 pandemic. A review of the scientific literature reveals restructured staffing departments, increased implementation of telemedicine, drastically higher volume of online patient messages with higher expectations in response time, and the need to increase staff work schedules and office open hours to accommodate urgent care and reduce patient backlogs following the relaxation of pandemic restrictions [4-7]. In addition to the new strain of COVID-19, ophthalmology has consistently been a department that requires a smooth clinic flow to process a high volume of patients. This is related to its unique nature as both a medical and surgical specialty that relies heavily on imaging, a wide range of laboratory and radiologic studies, and less commonly, hand-drawn sketches, to operate [8]. Resident and support staff contributions are two crucial factors affecting success. One of the challenges faced by ophthalmology practices is in resident training, where a balance of resident autonomy and attending supervision must be achieved. Medical malpractice lawsuits involving residents is a potential consequence of unaddressed problem areas in residency training [9]. Another consideration for clinics is the job satisfaction of support staff. Satisfaction can be related to multiple factors, including demographic population of the staff, job efficiency, communication styles, and longitudinal opportunities for growth [10-14]. Studies on lean six sigma process improvement show how these techniques can improve job satisfaction of staff and enhance patient care in ophthalmology practices.1516 There has also been increasing evidence that job satisfaction and morale among workers in healthcare settings have suffered during the COVID-19 pandemic, making it increasingly difficult to retain staff to support clinical practices [17-19]. It is crucial to hear from support staff working in ophthalmology clinics on how best to improve workflow and employee happiness. While there has been research on nurse job satisfaction on a hospital-wide basis, [20] even during the COVID-19 pandemic, [21] there is limited literature investigating what components lead to support staff job satisfaction in ophthalmology. The goal of this study is to evaluate workflow improvement and to identify possible ways to enhance employee morale among administrative, clinical, and nursing staff in an academic ophthalmology department.
Methods
This study is an anonymous survey of ophthalmology clinic support staff using a categorical, free-response, and Likert questionnaire. It contained nine questions within the categories of recognition, efficiency, completion, and job satisfaction (Table 1). Physicians, medical students, and medical scribes were excluded. The questionnaires were hand delivered to the survey participants and collected in an anonymous return box. The study was deemed exempt by the University of California Davis Institutional Review Board. All survey respondents verbally confirmed agreement in study participation before proceeding with survey questions.
|
What is your role in clinical care? |
No. (%) |
|
Clinical care team |
3/21 (14) |
|
Administrative assistant |
4/21 (19) |
|
Nurse team |
4/21 (19) |
|
Scheduling team |
10/21 (48) |
|
On average, how many messages do you need to handle each week? |
|
|
1-50 |
5/18 (28) |
|
51-100 |
5/18 (28) |
|
100-150 |
2/18 (11) |
|
151-200 |
2/18 (11) |
|
>200 |
4/18 (22) |
|
On average, what percent of the questions you get each week are you unable to answer and feel necessary to forward? |
|
|
0-20% |
7/18 (39) |
|
20-50% |
9/18 (50) |
|
50-70% |
2/18 (11) |
|
70-90% |
0/18 (0) |
|
100% |
0/18 (0) |
|
What type of messages are most difficult/hard to answer? |
|
|
Medications related questions |
4/23 (17) |
|
Scheduling related issues |
6/23 (26) |
|
Medical advice questions |
7/23 (30) |
|
Other, please specify: |
6/23 (26) |
|
On a scale of 1-5, with 1 being the least comfortable and 5 being very comfortable, how comfortable do you feel with the current workflow? |
|
|
1 |
2/18 (11) |
|
2 |
1/18 (6) |
|
3 |
5/18 (28) |
|
4 |
6/18 (33) |
|
5 |
4/18 (22) |
|
Do you have adequate response from the providers you forward questions to? |
|
|
My questions are answered adequately |
16/18 (89) |
|
My questions are not answered adequately |
2/18 (11) |
|
Continued from Question 6: If your questions are not answered adequately—what are the barriers for adequate response? |
|
|
Delay in timeliness of response |
6/21 (29) |
|
Answer comprehensiveness |
0/21 (0) |
|
Contradiction of information |
3/21 (14) |
|
Other, please specify: |
0/21 (0) |
|
None, my questions are answered adequately |
12/21 (57) |
|
What is the most exciting part of your job? |
|
|
Appreciation from coworkers |
9/30 (30) |
|
Appreciation from physicians |
8/30 (27) |
|
Free Samples |
2/30 (7) |
|
Department parties |
2/30 (7) |
|
Smooth clinic workflow |
4/30 (13) |
|
Other, please specify: |
5/30 (17) |
|
What do you think would help to improve efficiency of workflow and reduce staff messages? |
|
|
Educate and orient residents to each individual practice’s workflow |
12/39 (31) |
|
Improved specificity of scope and responsibilities of each role |
9/39 (23) |
|
Improved triage communication between residents/fellows and clinical staff |
5/39 (13) |
|
More administrative/nursing/scheduling support |
6/39 (15) |
|
Continued training in ophthalmology, eg. Observe doctors in their clinic, etc. |
7/39 (18) |
Table 1: Summary of survey data for questions 1-9 (n=18)
Study Participants
The survey was administered at three clinic locations of an academic ophthalmology department in Sacramento, California, and distributed to all support staff members including administrative assistants, clinic nurses, clinic schedulers, and clinical care coordinators. The administrative assistants are responsible for providing academic support to faculty and answering patient after-clinic care related questions. The nursing team’s duties consist of supporting physicians in clinic, with urgent triages and coordinating urgent add-on appointments. The scheduling staff handles routine appointment scheduling. The clinical care coordinators duties include triaging patient phone calls and requesting prior authorizations for upcoming appointments.
Survey Content and Delivery
Demographic questions of the participants were not included in this survey to protect the identity of the staff. Survey content included: 1) participant role in the clinic, 2) the number of patient messages received weekly, 3) the percent of patient messages that is too difficult to respond to without forwarding to physicians, 4) the type of patient messages that is the most difficult to respond to, 5) how comfortable the respondent feels about the current workflow, 6) if they receive an adequate response to their forwarded patient messages from providers, 7) barriers to receiving adequate responses, 8) most exciting aspects of the respondent’s job, and 9) possible areas to improve workflow efficiency and reduce staff messaging. Survey questions 2,3,5, and 6 were single select, and the rest of the questions were multiple select.
The study team distributed the survey via pen and paper. Participants understood that the survey was completely voluntary, anonymous, and not associated with their performance in their job. Participants began the survey in July 2021, and submitted their results anonymously within two weeks of the survey distribution.
Analysis
Study staff manually transcribed survey responses from hard-copy questionnaires completed by participants onto Microsoft Excel for all nine questions. Next, they tallied participant responses to each question. For the multiple-select and Likert scale questions, the study team tallied results of each question and copied and pasted them into Prism GraphPad 9.5 (San Diego, CA) to create graphical summaries. There was a single question that allowed for a free-text answer format. Study personnel read these answers individually and analyzed them qualitatively for any thematic grouping and patterns. All nine survey questions were first tallied irrespective of participant role in the ophthalmology clinic. Next, the survey responses were grouped according to the clinical role(s) of the participant. This was accomplished by examining how each participant answered question one, which asked survey participants to select their role(s) in the clinic. Two respondents selected multiple clinic roles, and these were analyzed as a single response for each clinical team selected. Study personnel assessed all responses for trends in answer choices with respect to the clinic role of the participant. Based on this assessment, we created two additional graphs on Prism GraphPad to visualize how each group answered survey questions 4 (most difficult patient messages) and 5 (current job satisfaction).
Results
A total of 22 surveys were distributed to support staff in the ophthalmology department, including administrative assistants, nursing team, clinic schedulers, and clinical care coordinators. A 100% response rate was received; however, 4 surveys were excluded due to lack of thorough completion or of survey instruction misunderstanding, leading to a total of 18/22 (81%) surveys being included in the final data analysis.
Clinical roles
The clinical care coordinators made up the smallest group 3/18 (17%), and most people within this role 2/3 (67%) were involved in multiple roles. One participant had two roles - scheduling and clinical care – and another participant was involved in three separate teams - scheduling, clinical care coordination, and administrative. There were 4/18 participants from the administrative team and 4/18 on the nursing team. Over half 10/18 (56%) of the responders were part of the scheduling team (Figure 1A).
Staff and patient message response
Most of the staff, 10/18 (56%), received less than 100 messages each week (Figure 1B). Other staff, 4/18 (22%) needed to handle more than 200 messages weekly, or roughly 40 messages daily. Most staff members, 16/18 (89%), could independently answer up to 50% of patients’ messages that they received (Figure 1C). This means that they need to forward about half of the messages to physicians for further input. Interestingly, some staff, 2/18 (11%), forwards up to 70% of patient messages to physicians. Almost all staff, 16/18 (89%), indicated that their questions were answered adequately by providers on the first reply (Figure 1D). Barriers to receiving an adequate response included the timeliness of response 6/9 (67%) and contradiction of information between trainees’ answers and faculty’s’ answers causing confusion 3/9 (33%) (Figure 1E).
Improvement Opportunities
When asked what strategies would best improve workflow efficiency and reduce staff messages, most respondents mentioned to educate and orient residents 12/39 (31%) (Figure 1F). Other suggestions included improved specificity in the scope of work and responsibility description 9/39 (23%), continued training on the job 7/39 (18%), more staff support 6/39, (15%), and improved triage communication 5/39 (13%) (Figure 1F).
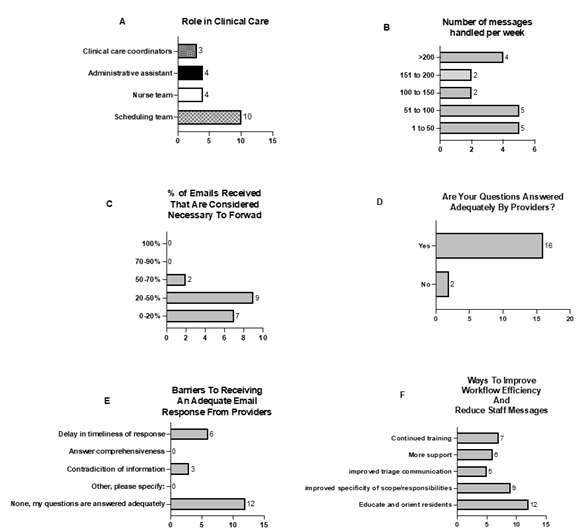
Figure 1: Survey results by question. (A) Respondent roles; (B) Number of patient messages handled per week; (C) Percentage of patient messages to be forwarded, (D) If providers answered questions adequately; (E) Barriers to receiving an adequate response; and (F) Suggestions for improvement.
The culprit: patient messages that are difficult to answer
The message types that are most difficult to answer include medical advice 7/23 (30%), scheduling related issues 6/23 (26%), and ‘medication’ related questions 4/23 (17%) (Figure 2A). Other difficult to answer question types cited by participants included insurance related questions 1/23 (<1%), and messages sent to a recipient who was not able to answer the question, resulting in a chain of forwarded patient messages 1/23 (<1%) (Figure 2A). Notably, from among the participants involved with scheduling, 5/10 (50%) selected ‘scheduling’ as one of the most difficult message types to answer (Figure 2B). This group formed the majority, 5/7 (71%), of respondents who found answering scheduling related questions most difficult. From the administration team, 0/7 (0%), found ‘scheduling’ related questions difficult to answer (Figure 2B) but did have trouble with both ‘medical advice’ messages 3/7 (43%) (Figure 2C) and ‘medication’ related questions 1/6 (17%) (Figure 2D). The clinical care coordinators had the most difficulty answering ‘medication’ related questions and formed 2/6 (33%) of respondents who found this message type difficult to respond to (Figure 2D). The nurse team did not have trouble with ‘medication’ related questions 0/6 (0%) (Figure 2D), but some trouble with ‘scheduling’ 1/7 (14%) (Figure 2B) and ‘medical advice’ 1/7 (14%) questions (Figure 2C).
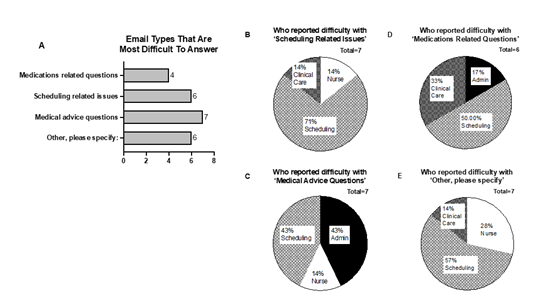
Figure 2: Patient message triage analysis by staff role and question type. (A) Most difficult message types to answer; Staff role that reported most difficulty with: (B) scheduling related issues, (C) medical advice questions, (D) medications related questions, and (E) ‘other, please specify’.
Job comfort levels
On a scale of 1 to 5 for comfort level at their current workflow, with 5 being the most comfortable, over half of staff 10/18 (56%) selected either 4 or 5 (Figure 3A). Staff who were clinical care coordinators had an average comfort level of 2 (Figure 3B). Staff who served on the administrative team displayed the most variability in response with an average response of 2.25 (Figure 3B). The nursing team displayed the highest comfort level with 3/4 (75%) indicating a 5 for maximum comfort, and 1/4 (25%) indicating a 4 (Figure 3B). The scheduling team had an average comfort level of 3.4 (Figure 3B).
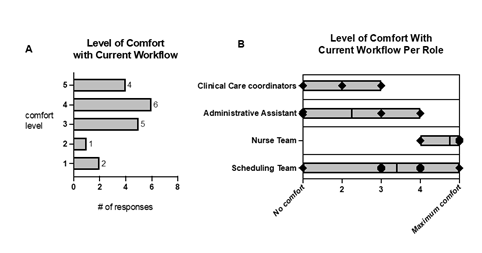
Figure 3: Level of comfort among staff total (A), and by participant role (B)
Job satisfaction: the positives
Appreciation from coworkers 9/30 (30%) and appreciation from physicians 8/30 (27%) were the two most exciting parts of the respondent’ job (Figure 4). Another important aspect that made their job exciting is a smooth clinic flow 4/18 (22%). Analysis of the free text responses to this question revealed two responses that cited positive recognition from doctors 2/18 (11%). When these free responses are added to the ‘appreciation from physicians’ category, this total makes up the largest group, 10/18 (56%), for most exciting aspects of their job. Also mentioned in the free text responses was “providing meaningful care to patients” 2/18 (11%). Department parties were voted less favorable for morale building 2/18 (11%).
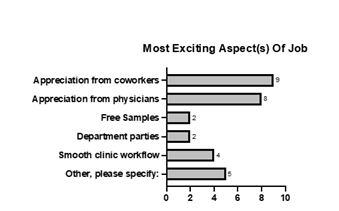
Figure 4: Most exciting aspect(s) of the job.
Study Limitations
The major limitation of this study is the small sample size as well as the single specialty department in which the survey was conducted. Ophthalmology is one specialty that is uniquely reliant on support staff for workflow optimization, which makes this study relevant specifically to ophthalmology departments [15,16]. Similarly, the small data sample size makes it difficult to understand variables that may play a role in job satisfaction, such as staff demographics and physician communication styles. Quality improvement studies can be performed on a larger scale to investigate the relationship between staff job satisfaction and specialty-specific or location-specific trends, as well as further subdivided to account for the effect of factors such as job growth opportunities, career length, demographic backgrounds, and physician communication styles [17,18,22]. In addition, the survey was conducted during the COVID-19 pandemic. As patient expectations and message volumes have dramatically increased since the pandemic, [23] we plan to repeat this survey after a new medical assisting system is fully implemented to compare the results with the post-COVID era.
Discussion
We gained three main discussion points from this survey. The first is that most of the non-medical trained staff are uncomfortable with patient care related questions. Secondly, improved resident orientation and guidance is recommended to enhance workflow efficiency. Finally, appreciation among coworkers and from physicians to staff is the most exciting aspect of working in the clinic.
Our survey results suggest that administrative staff or non-medical trained personnel should not be required to answer patient phone calls and clinical care related message. Nearly all of them were uncomfortable with these requests and needed to forward those messages to physicians anyway. This increases staff stress, decreases job satisfaction, and delays response time. The nursing team, however, is confident and competent in handling most of the messages with all members on the team rating at least 4/5 comfort level with the current workflow. This suggests that transitioning to a nursing team for patient message processing will improve staff and patient experience [24]. Additionally, the survey identified trainee error as a barrier to messaging workflow. When discussing the best ways to improve job efficiency and to decrease unnecessary staff messages, 12/39 (31%) of participants suggested implementing better education and orientation of incoming and current residents on how to forward messages appropriately. Specifically, a common discussion point was that incoming residents would forward questions in the EMR system to the wrong “pool” of staff, delaying response time to these questions. One way this can be addressed is by delivering a brief workshop on clinic guidelines for sending messages at the start of the residency training. Clearly established expectations governing patient message usage is vitally important because professionalism and communication skills are as critical as medical knowledge for patient care in residency training.25 Additionally, poor communication skills of residents can have serious consequences, including medical malpractice lawsuits [9].
Interestingly, despite the reported increase in job dissatisfaction during the COVID-19 pandemic, 10/18 56% of the surveyed group expressed job satisfaction, even with scheduling and clinical workflow changes. Staff expressed that the most positive part of the job by majority was the appreciation from coworkers and physicians. This study highlights the invaluable role ophthalmologists play in increasing clinic morale and job satisfaction by pausing to recognize the work of the support staff. Previous studies have emphasized the importance of interprofessional communication and gratitude towards colleagues in healthcare, which has been associated with better staff job satisfaction, work engagement, and lower turnover rates, and possibly patient outcomes [14,26-31].
Conclusions
This survey emphasized the importance of physician communication, and orientation of trainees in maximizing workflow efficiency and appreciation in the workplace. Positive feedback from physicians is critical in improving employee morale and job satisfaction, which may eventually impact patient care quality and patient satisfaction. A larger study can help identify areas for system-level improvements in work environments to reduce staff burnout and enhance patient satisfaction.
Acknowledgements and Declarations
Acknowledgments
The authors would like to thank Dr. Robert O’Donnell for his critical review of this manuscript. The authors would also like to thank Ms. Emily Schofield for her assistance in the literature review.
Declaration of conflicting interests
The Authors declare that there is no conflict of interest.
Funding
Rebekah Smith received partial financial support from the UC Davis Medical Student Research Fellowship Fund. Dr. Yin Allison Liu is partially supported by UC Davis School of Medicine Dean’s Scholarship for Career Development.
References
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press (2001).
- Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US), (2000).
- What is workflow?. Digital Healthcare Research (2023).
- Romano MR, Montericcio A, Montalbano C, et al. Facing COVID-19 in Ophthalmology Department. Curr Eye Res 45 (2020): 653-658.
- Liebmann JM. Ophthalmology and Glaucoma Practice in the COVID-19 Era. J Glaucoma 29 (2020): 407-408.
- Conway J, Krieger P, Hasanaj L, et al. Telemedicine Evaluations in Neuro-Ophthalmology During the COVID-19 Pandemic: Patient and Physician Surveys. J Neuroophthalmol 41 (2021): 356-361.
- Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc 27 (2020): 1132-1135.
- Chiang MF, Boland MV, Brewer A, et al. Special requirements for electronic health record systems in ophthalmology. Ophthalmology 118 (2011): 1681-1687.
- Watane A, Kalavar M, Chen EM, et al. Medical malpractice lawsuits involving ophthalmology trainees. Ophthalmology 128 (2021): 938-942.
- Renzi C, Tabolli S, Ianni A, et al. Burnout and job satisfaction comparing healthcare staff of a dermatological hospital and a general hospital. J Eur Acad Dermatol Venereol 19 (2005): 153-157.
- Chang E, Cohen J, Koethe B, et al. Measuring job satisfaction among healthcare staff in the United States: a confirmatory factor analysis of the Satisfaction of Employees in Health Care (SEHC) survey. Int J Qual Health Care 29 (2017): 262-268.
- Kalisch BJ, Lee H, Rochman M. Nursing staff teamwork and job satisfaction. J Nurs Manag 18 (2010): 938-947.
- Coleman G, Hyde E. Is there a role for professional supervision in supporting the professional and personal wellbeing of the sonographic workforce? A literature review. Radiography (Lond) 28 (2022): 991-998.
- Kelly LA, Lefton C. Effect of meaningful recognition on critical care nurses’ compassion fatigue. Am J Crit Care 26 (2017): 438-444.
- Ciulla TA, Tatikonda MV, ElMaraghi YA, et al. LEAN SIX SIGMA TECHNIQUES TO IMPROVE OPHTHALMOLOGY CLINIC EFFICIENCY. Retina (Philadelphia, Pa) 38 (2018): 1688-1698.
- Kam AW, Collins S, Park T, et al. Using Lean Six Sigma techniques to improve efficiency in outpatient ophthalmology clinics. BMC Health Serv Res 21 (2021): 38.
- O’Donnell P, Farrar A, BrintzenhofeSzoc K, et al. Predictors of ethical stress, moral action and job satisfaction in health care social workers. Soc Work Health Care 46 (2008): 29-51.
- Ulrich C, O’Donnell P, Taylor C, et al. Ethical climate, ethics stress, and the job satisfaction of nurses and social workers in the United States. Soc Sci Med 65 (2007): 1708-1719.
- Wright KB. A communication competence approach to healthcare worker conflict, job stress, job burnout, and job satisfaction. J Healthc Qual 33 (2011): 7-14.
- Koltuniuk A, Witczak I, Mlynarska A, et al. Satisfaction with Life, Satisfaction with Job, and the Level of Care Rationing Among Polish Nurses-A Cross-Sectional Study. Front Psychol 12 (2021): 734789.
- Al Sabei SD, Al-Rawajfah O, AbuAlRub R, et al. Nurses’ job burnout and its association with work environment, empowerment and psychological stress during COVID-19 pandemic. Int J Nurs Pract 28 (2022): e13077.
- Youn H, Lee M, Jang SJ. Person-centred care among intensive care unit nurses: A cross-sectional study. Intensive Crit Care Nurs 73 (2022): 103293.
- Holmgren AJ, Downing NL, Tang M, et al. Assessing the impact of the COVID-19 pandemic on clinician ambulatory electronic health record use. J Am Med Inform Assoc 29 (2022): 453-460.
- Huang M, Fan J, Prigge J, et al. Characterizing Patient-Clinician Communication in Secure Medical Messages: Retrospective Study. J Med Internet Res 24 (2022): e17273.
- Schmitt M, Blue A, Aschenbrener CA, et al. Core competencies for interprofessional collaborative practice: reforming health care by transforming health professionals’ education. Acad Med 86 (2011): 1351.
- House S, Crandell J, Stucky C, et al. Relational coordination as a predictor of job satisfaction and intent to stay among nurses and physicians in the military health system. Mil Med 188 (2023): e316-e325.
- Willgerodt MA, Blakeney EA-R. Can relational coordination theory be used to understand and improve interprofessional care coordination in schools? A pilot study. J Interprof Care 36 (2022): 761-764.
- Gittell JH, Logan C, Cronenwett J, et al. Impact of relational coordination on staff and patient outcomes in outpatient surgical clinics. Health Care Manage Rev 45 (2020): 12-20.
- House S, Wilmoth M, Kitzmiller R. Relational coordination and staff outcomes among healthcare professionals: a scoping review. J Interprof Care 36 (2022): 891-899.
- Adeyemo OO, Morelli EE, Kennedy HP. How to Foster Effective Midwife-Obstetrician Collaboration on Labor and Birth Units: Qualitative Analysis of Experiences of Clinicians in the United States. J Midwifery Womens Health 67 (2022): 552-560.
- Manojlovich M. Linking the practice environment to nurses’ job satisfaction through nurse-physician communication. J Nurs Scholarsh 37 (2005): 367-373.
