Use of Teriparatide for the Treatment of MRONJ in Non-Cancer Patients Refractory to the Traditional Conservative Therapy: A Systematic Review
Article Information
Catalfamo Luciano*, De Rinaldis Danilo, Nastro Siniscalchi Enrico, De Ponte Francesco Saverio
Department of Biomedical and Dental Sciences and of Morphological and Functional Images, University of Messina, Italy
*Corresponding Author: Catalfamo Luciano, Department of Biomedical and Dental Sciences and of Morphological and Functional Images, University of Messina, Italy
Received: 07 October 2022; Accepted 14 October 2022; Published: 30 November 2022
Citation: Catalfamo Luciano, De Rinaldis Danilo, Nastro Siniscalchi Enrico, De Ponte Francesco Saverio. Use of Teriparatide for the Treatment of MRONJ in Non-Cancer Patients Refractory to the Traditional Conservative Therapy: A Systematic Review. Dental Research and Oral Health 5 (2022): 102-110.
Share at FacebookAbstract
Teriparatide (TPTD) is the synthetic analogue of ParaThyroid Hormone (PTH) commonly used for the treatment of osteoporosis in place of Bisphosphonates. In 2007 it was proposed also for the treatment of Medication Related Osteonecrosis of the Jaws (MRONJ) in non cancer patient. However, nowadays TPTD is still off-label in these patients, because of the lack of the scientific evidence of its safety and efficacy. We propose a Systematic Review of clinical reports dealing with the use of TPTD in non-oncological patients with refractory MRONJ. Using Pubmed as research engine, we researched and included only Case Reports or Case Series dealing with the use of TPTD in non cancer patients with MRONJ (Eligibility Criterion). We excluded all experimental studies on animals and laboratory work conducted in vitro (Exclusion Criterion). We found 23 papers, published from February 2007 to May 2020, with the eligibility criteria established. A total of 97 patients have been included in our analysis, 86 women (88.7%) and 11 men (11.3%), age 52-88 years old (mean 77 y.o.). Most of them, 86.6% (84 out 97) were classified as positive outcome, while the 13.4% (13 out 97) as negative outcome. Although further randomized clinical trials are needed, TPTD seems to represent a valid support to surgery for the treatment of non oncological patients affected by MRONJ in advanced stage.
Keywords
ParaThyroid Hormone, Non Cancer patient, Medication Related Osteonecrosis of the Jaws (MRONJ)
ParaThyroid Hormone articles; Non Cancer patient articles; Medication Related Osteonecrosis of the Jaws (MRONJ) articles
ParaThyroid Hormone articles ParaThyroid Hormone Research articles ParaThyroid Hormone review articles ParaThyroid Hormone PubMed articles ParaThyroid Hormone PubMed Central articles ParaThyroid Hormone 2023 articles ParaThyroid Hormone 2024 articles ParaThyroid Hormone Scopus articles ParaThyroid Hormone impact factor journals ParaThyroid Hormone Scopus journals ParaThyroid Hormone PubMed journals ParaThyroid Hormone medical journals ParaThyroid Hormone free journals ParaThyroid Hormone best journals ParaThyroid Hormone top journals ParaThyroid Hormone free medical journals ParaThyroid Hormone famous journals ParaThyroid Hormone Google Scholar indexed journals Non Cancer patient articles Non Cancer patient Research articles Non Cancer patient review articles Non Cancer patient PubMed articles Non Cancer patient PubMed Central articles Non Cancer patient 2023 articles Non Cancer patient 2024 articles Non Cancer patient Scopus articles Non Cancer patient impact factor journals Non Cancer patient Scopus journals Non Cancer patient PubMed journals Non Cancer patient medical journals Non Cancer patient free journals Non Cancer patient best journals Non Cancer patient top journals Non Cancer patient free medical journals Non Cancer patient famous journals Non Cancer patient Google Scholar indexed journals Medication Related Osteonecrosis of the Jaws articles Medication Related Osteonecrosis of the Jaws Research articles Medication Related Osteonecrosis of the Jaws review articles Medication Related Osteonecrosis of the Jaws PubMed articles Medication Related Osteonecrosis of the Jaws PubMed Central articles Medication Related Osteonecrosis of the Jaws 2023 articles Medication Related Osteonecrosis of the Jaws 2024 articles Medication Related Osteonecrosis of the Jaws Scopus articles Medication Related Osteonecrosis of the Jaws impact factor journals Medication Related Osteonecrosis of the Jaws Scopus journals Medication Related Osteonecrosis of the Jaws PubMed journals Medication Related Osteonecrosis of the Jaws medical journals Medication Related Osteonecrosis of the Jaws free journals Medication Related Osteonecrosis of the Jaws best journals Medication Related Osteonecrosis of the Jaws top journals Medication Related Osteonecrosis of the Jaws free medical journals Medication Related Osteonecrosis of the Jaws famous journals Medication Related Osteonecrosis of the Jaws Google Scholar indexed journals osteonecrosis articles osteonecrosis Research articles osteonecrosis review articles osteonecrosis PubMed articles osteonecrosis PubMed Central articles osteonecrosis 2023 articles osteonecrosis 2024 articles osteonecrosis Scopus articles osteonecrosis impact factor journals osteonecrosis Scopus journals osteonecrosis PubMed journals osteonecrosis medical journals osteonecrosis free journals osteonecrosis best journals osteonecrosis top journals osteonecrosis free medical journals osteonecrosis famous journals osteonecrosis Google Scholar indexed journals implant articles implant Research articles implant review articles implant PubMed articles implant PubMed Central articles implant 2023 articles implant 2024 articles implant Scopus articles implant impact factor journals implant Scopus journals implant PubMed journals implant medical journals implant free journals implant best journals implant top journals implant free medical journals implant famous journals implant Google Scholar indexed journals mandibular articles mandibular Research articles mandibular review articles mandibular PubMed articles mandibular PubMed Central articles mandibular 2023 articles mandibular 2024 articles mandibular Scopus articles mandibular impact factor journals mandibular Scopus journals mandibular PubMed journals mandibular medical journals mandibular free journals mandibular best journals mandibular top journals mandibular free medical journals mandibular famous journals mandibular Google Scholar indexed journals oral fistula articles oral fistula Research articles oral fistula review articles oral fistula PubMed articles oral fistula PubMed Central articles oral fistula 2023 articles oral fistula 2024 articles oral fistula Scopus articles oral fistula impact factor journals oral fistula Scopus journals oral fistula PubMed journals oral fistula medical journals oral fistula free journals oral fistula best journals oral fistula top journals oral fistula free medical journals oral fistula famous journals oral fistula Google Scholar indexed journals mandible articles mandible Research articles mandible review articles mandible PubMed articles mandible PubMed Central articles mandible 2023 articles mandible 2024 articles mandible Scopus articles mandible impact factor journals mandible Scopus journals mandible PubMed journals mandible medical journals mandible free journals mandible best journals mandible top journals mandible free medical journals mandible famous journals mandible Google Scholar indexed journals
Article Details
Introduction
Background
Medication-Related OsteoNecrosis of the Jaws (MRONJ) is a rare, but potentially serious, adverse event associated with anti-resorptive therapy (Figure 1) [1]. The incidence of MRONJ is related to poor oral conditions, old age, sex male, drug type (e.g. amino-BPs), concomitant drug therapies (e.g. corticosteroid), comorbidity (e.g. diabetes), cancer [2]; besides local factors, as tooth infections, dental implants or even osteosynthesis devices could be associated with a higher risk of MRONJ [3-8]. Initially, the drugs-related osteonecrosis of the jaws was associated with the administration of bisphosphonates only (Bisphpsphonates Related OsteoNecrosis of Jaws-BRONJ). Afterwards, another anti-resorptive drug (denosumab) has been related to this pathology. The term ARONJ (Antiresorptive Related OsteoNecrosis of the Jaw) was then adopted [9]. However the acronym MRONJ (Medication Related OsteoNecrosi of Jaws) seems to be more correct, being other drugs like anti-angiogenic ones (bevacizumab, sunitinib, imatinib, ranibizumab) capable of giving such side effects [10-16]. The recommended treatment of MRONJ is antibiotic and surgical debridement, protocol known as “conventional conservative treatment” [17,18]. However, most of the patients are refractory to the conservative treatment and the patient were informed about the possible irreversibility of the exposed bone (2007) [19]. Patients with MRONJ refractory to the conservative therapy or in advanced stages are often treated with resective surgery, with sometimes disfiguring and dysfunctional outcomes limiting the quality of life. During the last years, several alternative therapeutic approaches have been proposed for the treatment of refractory MRONJ, as HyperBaric Oxygen Therapy (HBOT) [20] and Ozone therapy [21].

Figure 1: An advanced case of BRONJ (stage 3); a patient with left maxillary osteonecrosis complicated with periorbital oro-cutaneous fistula (arrow).

Figure 2: An intra-operatory image of maxillary osteonecrosis that shows the ipovascularity of bone tissue.
In 2007, Teriparatide (Forsteo) was proposed for the treatment of refractory MRONJ [22]. Teriparatide (TPTD) is the active fragment of parathyroid hormone (PTH 1-84), specifically it is the recombinant human fragment 1-34 (rhPTH 1-34) with the same effects of the natural hormone (Figure 3) [22]. Nowadays, TPTD is approved by the Food and Drug Administration (FDA) for the treatment of glucocorticoid-induced osteoporosis and in postmenopausal women with a high risk of fracture [23] but it was not approved for MRONJ, in which TPTD must be considered off label. The exact mechanism of action of TPTD in ONJ is stil unknown. Recent studies shown that TPTD, analogue of PTH, has opposite effects depending on its blood levels: in disease states associated with continuous excess of PTH in blood, such as primary hyperparathyroidism, increased osteoclast activity and accelerated bone resorption occurs, resulting in “catabolic effect”. Conversely, intermittent exposure to low-dose of PTH (like daily administration of Teriparatide) induces bone formation, causing an “anabolic effect” [23]. TPTD, with its N-terminal fragment, binds the PTH-type-1 receptors (PTH-1-R), that are G-proteine coupled receptors expressed on the surface of various cells, especially on osteoblast, osteocytes and renal tubular cells, all of them implicated in the regulation of phospho-calcium homeostasis. The binding of PTH to PTH-1-R actives the adenylate cyclase enzyme, it catalyzes the generation of cAMP second messenger, which ultimately activates protein kinase A (PKA) [23].
The anabolic effects of intermittent PTH depending on:
- up-regulation of transcriptional expression of pro-osteoblastogenic growth factors like IGF-1 (insulin-like growth factor-1) and FGF-2 (fibroblast growth factor-2);
- down-regulation of the synthesis of wnt-antagonist sclerostin, which is part of wnt/beta catenin osteoanabolic signaling pathway;
- increased expression of Runx-2, a transcriptional factor essential for the differentiation of osteoblastic cells [23].
Figure 3: PTH effects and vitamin D metabolism in humans
The catabolic effects of PTH are mediated by its binding to the same receptors on the same cells but which, at constant blood levels, increases the expression of pro-osteoclastogenic cytochines, like RANKL. The binding of RANKL to its receptor RANK, expressed on the surface of hematopoietic precursor cells, promotes osteoclastic differentiation and activation [23]. However, to date, numerous other studies are needed to clarify the different molecular effects dependent on intermittent/continuous exposure to PTH and, consequently, the beneficial effects of Teriparatide on maxillary ONJ. TPTD is contraindicated in patients with Multiple Myeloma or any other kind of solid tumor, for the risk of malignant hypercalcemia, thus its use must be limited to the treatment of patients with MRONJ associated with osteometabolic disease, above all osteoporosis. In the past, TPTD was associated with osteosarcoma in rats model [24] representing a great limitation to its use. However, that risk seems comparable to the general population one [25].
Objectives
In this paper, we propose a Systematic Review of all clinical reports published in the last fifteen years in which Teriparatide has been administrated in non-oncological patients with refractory MRONJ. Our purpose is to unify all the works present in literature to prove the potentiality of the drug in these patients.
Material and Methods
We conducted our research according to PRISMA 2020 guidelines, using PubMed as research engine. We collected all clinical reports published in literature reporting the topic <> since the first work presented in May 2007 to the last one in February 2020.
Search strategies
We used as key words for the research “Teriparatide” and “Osteonecrosis of the jaws”.
Eligibility criteria
We established the following inclusion conditions:
- Articles must be a Case Report or a Case Series;
- The outcomes must be clearly reported;
- Authors must reported the administration period of TPTD.
We excluded all experimental studies on rats and laboratory works conducted in vitro on cells cultures.
Selection process
Five authors participated to this research, each of us worked independently but comparisons were frequent. A first selection was conducted by one author on Pubmed, using the key words “Teriparatide” and “Osteonecrosis of the jaws”. He collected 102 manuscripts since May 2007 to February 2020. By the title, the author excluded all experimental studies on rats and laboratory works conducted in vitro. So, only 37 manuscripts were accepted for a second selection. In fact, only 65 articles were clinical trials on humans. The second selection was performed, through the abstracts, by another author. This procedure allowed us to confirm the eligibility criteria established and to exclude dubious on works previously collected. Fourteen papers were discarded because they didn’t respect the eligibility criteria established. Only 23 articles were selected for the last phase of selection that required the full reading of all works collected. This phase was conducted by two authors independently. Through the full reading, we extrapolated the data established for the research. Data were put together and statistically analyzed by the last author.
Data collection process
At the end of the selection process, we found 23 papers suitable for our research and we collected the following data:
- number of patients included;
- age and sexual gender of patients;
- site of osteonecrosis (maxilla, mandible or both);
- antiangiogenic/antiresorptive drug previously assumed by patients (oral BPs, iv BPs or denosumab);
- period of antiangiogenic/antiresorptive drug exposure;
- trigger of ONJ (spontaneous, post-extractive, post-implant placement, periodontitis induced);
- MRONJ stage according to AAOMS Staging System;
- protocol of TPTD therapy administrated (20 μg daily/56.5 μg weekly);
- range time of TPTD administration;
- outcomes and follow up period.
Data items
The main data that we considered was the outcome of the TPTD treatment. However, we extended the informations of patients included in the study for a most complete frame of work. For example, according to us, the range time of TPTD administration was very important to know, as it was important to know the stage of the disease and the protocol of TPTD administrated (daily or weekly).
Study risk of bias assessment
We found the major risk of bias during the phase of full reading of the articles selected. Specifically we considered the risk of misinterpretation of the outcome, that could be false positive if the authors didn’t describe clearly the evolution of the case. This risk was avoided using the method of a double reading of the works by two authors in charge of the full reading. Each of them read again the works already read by the other one.
Effect measures
In table 1 we listed all studies selected in alphabetical order of the first author. For each work we reported the number of patients, the protocol of TPTD administration (daily/weekly), the period of TPTD therapy and the outcome of treatment.
|
Author |
Number of Patients (97) |
Dose TPTD |
Period of TPTD Administration |
Outcome |
|
Cheung et al [18] |
1 |
20 μg/die |
2 months |
+ |
|
Doh et al [29] |
1 |
20 μg/die |
6 months |
+ |
|
Harper et al [11] |
1 |
20 μg/die |
24 months |
+ |
|
Jung et al [33] |
4 |
20 μg/die |
1-4 months |
+4 |
|
Kakehashi et al [30] |
10 |
20 μg/die |
4-24 months/ few days (2 patients) |
+(7)/-(3) |
|
Kim et al [26] |
15 |
20 μg/die |
2 months |
+15 |
|
Kim et al [34] |
1 |
56,5 μg/week |
2 months |
+ |
|
Kwon et al [20] |
6 |
20 μg/die |
1-3 months |
+6 |
|
Lau et al [15] |
1 |
20 μg/die |
18 months |
+ |
|
Lee et al [19] |
1 |
20 μg/die |
10 months |
+ |
|
Morishita et al [36] |
29 |
20 μg/die |
1-26 months/ few days (1 patient) |
+(22)/-(7) |
|
Narongroeknawin et al [17] |
1 |
20 μg/die |
4 months |
+ |
|
Narvàez et al [24] |
1 |
20 μg/die |
8 months |
- |
|
Neuprez et al [28] |
1 |
20 μg/die |
4,3 months |
+ |
|
Ohbayashy et al [35] |
12 |
20 μg/die (6) 56,5 μg/week (6) |
6 months |
+(12) |
|
Ohbayashi et al [23] |
1 |
20 μg/die |
6 months |
+ |
|
Pelaz et al [27] |
4 |
20 μg/die |
4-10 months |
+(2)/-(2) |
|
Yao et al [31] |
1 |
56,5 μg/week |
18 months |
+ |
|
Yoshiga el al [25] |
2 |
20 μg/die (1) 56,5 μg/week (1) |
3 months |
+(2) |
|
Ywamoto et al [21] |
1 |
20 μg/die |
3 months |
+ |
|
Thumbigere-Math et al [22] |
1 |
20 μg/die |
3 months |
+ |
|
Tsai et al [16] |
1 |
20 μg/die |
5 months |
+ |
|
Zushi et al [32] |
1 |
20 μg/die |
24 months |
+ |
Table 1: Complete collection of clinical studies published from 2007 to 2020 on the use of teriparatide in the treatment of MRONJ.
Results
Study selection
Most of the 23 studies collected are single Case Report. Overall, we found 16 Case Reports and 7 Case Series.
Study characteristics and results of individual studies
Harper et al [22] described the case of a 75-year-old woman treated with alendronate for post-menopausal osteoporosis who developed a post-extractive refractory ONJ. The authors reported the complete remission, both clinical and radiological, after 24 months of treatment with 20 μg daily of subcutaneous TPTD. Lau et al [26] described the case of a 56-year-old woman exposed to BPs for glucocorticoid osteoporosis that she assumed for fibromyalgia. The patient developed osteonecrosis both in the maxilla and in the mandible following to teeth extractions and she was refractory to conventional therapy. The authors reported the clinical complete remission after 18 months of 20 μg/day s.c. TPTD. Tsai et al [27] reported the case of a 72-year-old woman treated with alendronate for post-menopausal osteoporosis. She developed an extensive mandibular osteonecrosis after implant placement. The woman, refractory to traditional therapy, completely healed (both clinically and radiologically) after administration for 5 months of 20 μg per day of TPTD. Narongroeknawin et al [28] published the case of a 63-year-old man in treatment with alendronate for osteoporosis which developed a maxillary osteonecrosis after implants placement. The patient was treated with 20 μg/day s.c. TPTD for 4 months and the authors reported an improvement of clinical and radiological conditions. Cheung et al [29] described the case of a 88-year-old woman treated with alendronate. The patients developed a refractory mandibular ONJ. She was treated with 20 μg/day of TPTD. The authors reported the complete clinical remission of symptoms and the improvement of radiological findings after 8 weeks of treatment. Lee et al [30] described the case of a 78-year-old woman received alendronate for postmenopausal osteoporosis and developed mandibular osteonecrosis after tooth extractions. The authors reported the complete clinical and radiographic recovery after 10 months of TPTD 20 μg/day. Kwon et al [31] published a case series of 6 patients (4 women and 2 men), range age 68-88 years old, with refractory MRONJ (5 mandibular and 1 maxillary). The patients were treated with 20 μg/day of TPTD for a period of 1-3 months. The authors reported the complete clinical remission of all patients. Ywamoto et al [32] described the case of a 79-year-old woman with mandibular ONJ treated with 20 μg/day of TPTD for 3 months. The authors reported the complete clinical recovery of the disease associated with a significant improvement in the mandibular bone defect found on CT scan. Thumbigere-Math et al [33] reported the case of a 58-year-old woman affected by refractory BRONJ treated with 20 μg/day of TPTD for 3 months. The authors reported the complete clinical remission of the symptoms. Ohbayashi et al [34] described the case of a 78-year-old osteoporotic woman treated with alendronate that developed a mandibular ONJ following a tooth extraction. She was refractory to the traditional therapy and she was treated with 20 μg/day of TPTD for 6 months. The authors reported the complete clinical healing just after 1 month of treatment and an improvement in bone density at the end of treatment relived through CT scan. Narvàez et al [35] reported the case of a 79-year-old man that was exposed to ibandronate for osteoporosis and to methotrexate, prednisone and rituximab for rheumatoid arthritis also. The patient was refractory to the traditional conservative therapy, so he was treated with 20 μg per day of TPTD but after 8 months of treatment no improvement was noted, so the therapy was suspended. However, the authors believed that the failure of therapy had to be attributed to the interaction of other drugs that the patient assumed for the treatment of rheumatoid arthritis (methotrexate, prednisone, rituximab). Yoshiga et al [36] compared two clinical cases of stage 3 refractory BRONJ treated with Teriparatide. The patients received a different protocol of administration: one patient received 20 μg daily of TPTD while the other one 56.5 μg weekly. The authors reported no differences of outcome in the two patients: they were clinically recovered after 3 months of treatment and CT scan demonstrated an improvement of the bone density in both patients. Kim et al [37] published the first randomized clinical trial on the use of TPTD in refractory MRONJ. The authors treated a group of 9 patients with a supplement of Calcium and vitamin D only (non-TPTD group) and a group of 15 patients with Calcium and vitamin D supplement and with TPTD 20 μg per day for 6 months (TPTD group). All 15 patients of TPTD group had an improvement in clinical and in the radiographic reports: 9 of them reported only improvement while 6 patients reported complete remission. Pelaz et al [38] treated a group of patients with surgical debridement and application of PRF (growth Factor Rich Plasma) and another group of patients with TPTD only (20 μg/day) without surgical therapy. All patients presented a stage 3 MRONJ and were evaluated clinically and radiologically through CT scan. At the end of the follow-up all patients surgically treated (5 out of 5) were healed, while only the 25% of patients of the TPTD group (1 out of 4) were healed, the 25% (1 out of 4) still had bone exposure but was asymptomatic, the 50% (2 out of 4) had exposed bone and remained symptomatic also. Although the results appear against TPTD, we must consider that the group treated with Forsteo was composed of patients affected by an advanced neurodegenerative disease that didn’t allow to perform any surgical treatment. Neuprez et al [39] published the first clinical case of a patient with MRONJ post denosumab treated with TPTD. This is a 58-year-old man with osteoporosis who developed spontaneous mandibular osteonecrosis. The patient was treated with 20 μg/day of TPTD. CT, performed 65 days after onset of the treatment, demonstrated a significant reduction in the necrotic area and after 130 days the patient was completely clinically healed. Doh et al [40] reported the case of a 75-year-old woman, in treatment with alendronate for post-menopausal osteoporosis, who developed a post-implant osteonecrosis of the jaw. The patient was treated with 20 micrograms per day of TPTD for 6 months. After 5 months of treatment the oral mucosa was completely healed. Radiographic control, performed 5 months after beginning of the treatment, demonstrated a normal bone density. Kakehashi et al [41] published the results of an open clinical trial. They treated 10 patients with BPs osteonecrosis of the jaws with 20 mcg/daily of TPTD. The patients were all women treated with BPs for post-menopausal osteoporosis, with a range of age between 63 and 91 years old. Two patients discontinued treatment after a few days because of side effects. In the other patients the time range of TPTD therapy was 4-24 months. After 1 year, the therapy resulted in a complete clinical recovery for seven patients while one patient, despite the pain disappeared, still presented an intra-oral fistula and no evolution of the bone sequestration. However, the latter patient received also prednisone which may interfered with the TPTD effects. Yao et al [42] reported the clinical case of an osteoporotic 87-year-old woman in treatment with minodronate that developed a mandibular ONJ after a tooth extraction. The patient was treated with 56.5 micrograms weekly subcutaneous TPTD. After 6 months of treatment, the patient developed bone sequestration and underwent to sequestrectomy. After 7 months of treatment, symptoms regressed and the oral fistula resolved. After 18 months of therapy, CT scan demonstrated significant bone regeneration. Zushi et al [43] described the case of a 66-year-old woman treated with alendronate for post-menopausal osteoporosis. The woman developed an ONJ of the mandible following to implant placement. After 5 months of TPTD, the patient developed bone sequestration and underwent to sequestrectomy. After other 5 months, patient was clinically and radiologically healed. Jung et al [44] published a controlled clinical trial performed on 17 patients (16 women and 1 man, age range 59-86 years old) with refractory MRONJ. Authors compared the effect of topical application of rhBMP2 and subcutaneous TPTD (20 μg/day) for 1-4 months. Clinically, all patients treated with TPTD recovered completely. The radiological evaluation showed a bone regeneration of almost double entity in TPTD group compared to rhBMP2 one. Kim et al [45] reported a clinical case of an 85-year-old osteoporotic woman with refractory mandibular MRONJ after two implant placements treated with 56.5 μg/weekly TPTD. After 4 weeks of treatment, the bone sequestration disappeared spontaneously. Six weeks after, the implants were spontaneously expelled while 6 months after the patient was completely healed. Ohbayashy et al [46] published the results of a randomized clinical trial in which efficacy of daily TPTD (20 mcg) was compared to weekly one (56.5 mcg). Twelve patients were randomly divided in two groups: a group of 6 patients treated with daily TPTD (20 μg/day) and a group of 6 patients treated with weekly TPTD (56.5 μg/week). Both groups of patients received TPTD for 6 months and underwent radiological evaluation with CT scan that showed an improvement of bone density in 5 of the patients of the daily TPTD group and in 3 patients of the weekly TPTD group. All patients were clinically asymptomatic. The authors did not find substantial differences between the two groups. Morishita et al [47] presented a multicentre retrospective study in which were collected the data of 29 patients with refractory MRONJ treated with TPTD since 2012 to 2016. Patients included 6 men and 23 women (56-88 years old). Median administration of TPTD was 14 months (range 0.3-26 months). Seven patients discontinued therapy for adverse effects while 22 patients had a favorable outcome (complete or partial remission).
Results in synthesis
A total of 97 patients have been included in our analysis, 86 women (88.7%) and 11 men (11.3%) (Figure 4), range age 52-88 years old, mean age 77. The sites of ONJ were 16 in maxilla (16.5%), 71 in the mandible (73.2%), 6 both in maxilla and mandible (6.2%), and in four cases there were no information about the site (4.1%) (Figure 5). Among 97 patients, oral alendronate was the most prescribed BPs: 42 patients (43.3%) were treated for osteoporosis with only alendronate. Oral risedronate was assumed by 20 patients (20.6%), while minodronate per os was assumed by 6 patients (6.2%), and oral ibandronate by 4 patients (4.1%). Most of patients were subjected to oral BPs therapy, only 5 patients (5.1%) assumed iv BPs. Zoledronate was the first iv BPs administrated, 3 out 5 patients. Pamidronate was administrated to one patient, while another one patient was exposed to a subsequent therapy with etidronate per os, clodronate iv and pamidronate iv. More than one oral BPs were assumed by 4 patients (4.1%). Only 3 patients (3.1%) assumed denosumab (Figure 6). Range of antiangiogenic/antiresorptive therapy was 0.3-10 years, with a mean period of 5 years. Mean period of TPTD administration was 8 months, range 0-26 months. In most cases the trigger factor of ONJ was teeth extractions, 39 out of 97 (40.2%). The second trigger was dental implant placement: 11 patients (11.35%), while in 8 patients (8.25%) the trigger was periodontitis, in 33 cases (34%) trigger factor was not specificated and 6 out of 97 cases (6.2%) were spontaneous ONJ (Figure 7).
Most of patients had AAOMS stage 2 or 3:
- 58 out of 97 (59.8%) stage 2;
- 29 out of 97 (29.9%) stage 3.
Only one patient had stage 1 (1.03%) and in 9 cases (9.27%) the stage wasn’t declared (Figure 8). Most all of patients (90.73%) were treated with the traditional protocol of 20 μg daily of subcutaneous TPTD. Only 9 out of 97 (9.27%) were treated with the alternative protocol of 56.5 μg weekly (Figure 9).
For the analysis of the results, we divided all 97 patients in two groups:
- patients with a positive outcome (improvement of clinical and/or pathological conditions);
- patients with a negative outcome (no improvement, or withdrawal of treatment).
We found 84 out of 97 cases reported as positive outcome (86.6%) and 13 out of 97 cases as negative outcome (13.4%) (Figure 10,11). The follow up period was reported by seven authors only, just for 10 patients; range was 4-10 months, mean 7 months after TPTD suspension.
Reporting bias
Although the encouraging results, we must consider some bias in this work. First of all the different period of administration of Teriparatide, whose range was between 1 month (in some cases few days) until 2 years. Another important bias is the different evaluation criteria of outcomes. In most cases the authors reporting results after a clinical and radiological evaluation. Generally, the radiological exam consists in an orthopanoramic radiography, only in few cases patients underwent a CT evaluation. In four studies, overall comprehensive of 49 patients, just the authors attested the improvement/healing of the pathology. In one study, comprehensive of 6 patients, authors reported only clinical evaluation without any radiological exams. Finally, we found a bias in the follow up times: only in 7 studies, comprehensive of 10 patients, the authors reported it.
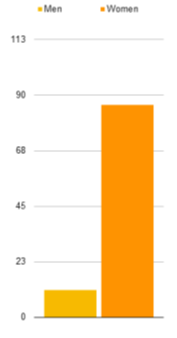
Figure 4: Sex distribution of the 97 cases collected.
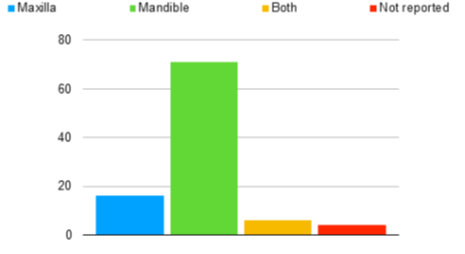
Figure 5: Sites of ONJ in the 97 cases collected.
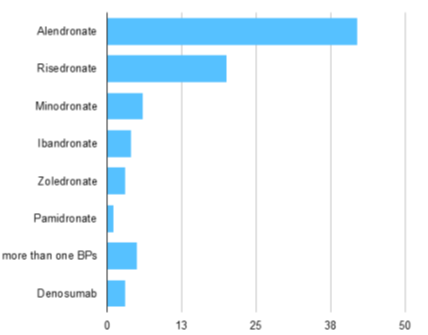
Figure 6: Antiangiogenic/antiresorptive drugs exposure.
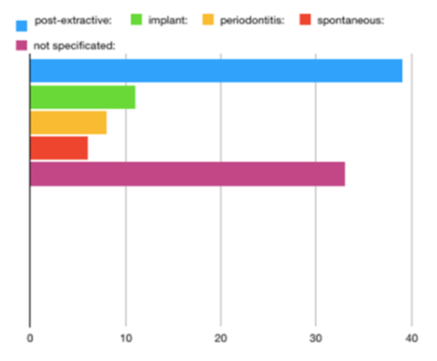
Figure 7: Trigger factors of MRONJ in the 97 cases examined.
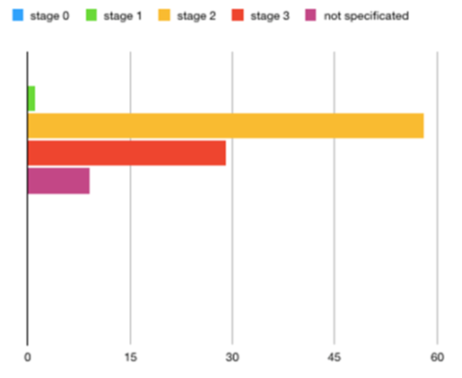
Figure 8: ONJ Stages according to AAOMS 2014 Staging System
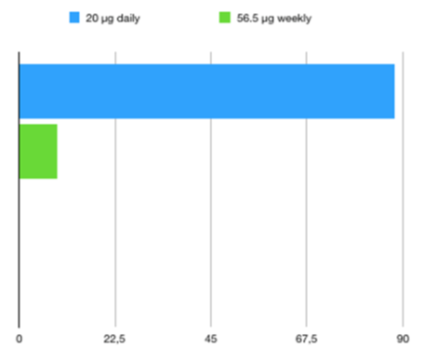
Figure 9: Protocol of TPTD administration.
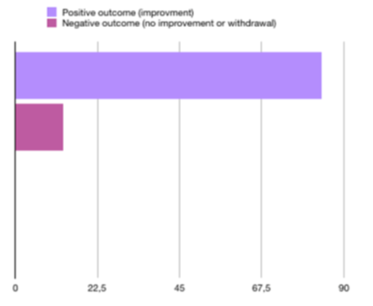
Figure 10: Outcomes of TPTD protocol treatment, expressed in percentage value.
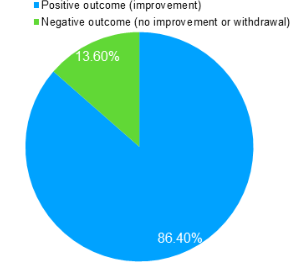
Figure 11: Outcomes of TPTD protocol treatment, expressed in percentage value.
Discussion
Although randomized clinical trials with an great number of patients are still lacking, administration of subcutaneous TPTD can be considered a promising supplement to the standard treatment of MRONJ in non oncological patients. Our research demonstrate that the cases of osteonecrosis treated with TPTD present in literature are a in fair number, and those resolved with positive outcome are the majority. In addition, analyzing individually the cases reported in literature with unfavorable outcomes, we can note that 9 out of 13 are cases of withdrawal treatment because of intolerable adverse effects (Morishita [36], Kakehashi [30]). The remaining 4 cases with unfavorable outcomes include: one patient with rheumatoid arthritis received methotrexate, prednisone and rituximab also (Narvàez [24]), two patients with only one TPTD therapy but with no possibility of surgical treatment because of advanced neurodegenerative disease (Pelaz [27]). In conclusion, we believe that TPTD has the potential to fully enter the treatment protocol of MRONJ in non cancer patients but further large-scale clinical trials are still needed. TPTD could be used to avoid resective surgery of the jaws or to obtain a “debulking” of the disease so to allow a less demolitive surgery, as neoadjuvant therapy. In other cases, TPTD could be used in patients with early bone lesions but not eligible for surgery.
References
- Nicolatou-Galitis O, Schiødt M, Mendes RA, et al. Medication-related osteonecrosis of the jaw: definition and best practice for prevention, diagnosis, and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol 127 (2019): 117-135.
- Ishimaru M, Ono S, Morita K, et al. Prevalence, incidence rate and risk factors of Medication-Related Osteonecrosis of the Jaw in patients with osteoporosis and cancer: A nationwide population-based in Japan. J Oral Maxillofac Surg 12 (2021) 01511.
- Soutome S, Otsuru M, Hayashida S, et al. Relationship between tooth extraction and development of medication-related osteonecrosis of the jaw in cancer patients. Sci Rep 11 (2021): 17-22.
- Pichardo SEC, Van der Hee JG, Fiocco M, et al. Dental implants as risk factors for patients with medication-related osteonecrosis of the jaws (MRONJ). Br J Oral Maxillofac Surg 58 (2020): 771-776.
- Sher J, Kirkham-Ali K, Luo JD, et al. Dental Implant Placement In Patients With History of Medications Related Osteonecrosis of the Jaws: A Systematic Review. J Oral Implantol 47 (2021): 249-268.
- Escobedo MF, Cobo JL, Junquera S, et al. Medication-related osteonecrosis of the jaw. Implant presence-triggered osteonecrosis: Case series and literature review. J Stomatol Oral Maxillofac Surg 121 (2020): 40-48.
- Ueda N, Imada M, Kato Y, et al. Bevacizumab-associated implant presence-triggered osteonecrosis: A case report and literature review. J Oral Implantol 16 (2021): 89-97.
- Nastro ES, Catalfamo L, Allegra A, et al. Titanium miniplates: a new risk factor for the development for the bisphosphonate-related osteonecrosis of the jaw. J Craniofac Surg 24 (2013): 5698.
- Shibahara T. Antiresorptive Agent-Related Osteonecrosis of the Jaw (ARONJ): A Twist of Fate in the Bone. Tohoku J Exp Med 247 (2019): 75-86.
- Nastro ES, Allegra A, Oteri G, et al. Avascular necrosis in leukemia and osteonecrosis of jaw by bisphosphonates. J Oral Maxillofac Surg 67 (2009): 2701-2703.
- Nastro ES, Cutroneo G, Catalfamo L, et al. Immunoistochemial evaluation of sarcoglycans and integrins in gingival epithelium of multiple myeloma patients with bisphosphonate-induced osteonecrosis of the jaw. Oncol Rep 24 (2010): 129-134.
- Kudva A, Koshy J, Jacob JG. Oral mucosal pseudotumor - Novelty complication in patient undergoing bevacizumab therapy. Oral Oncol 122 (2021): 105543.
- Hofmann E, Eggers B, Heim N, et al. Bevacizuab and sunitinib mediate osteogenic and pro-inflammatory molecular changes in primary human alveolar osteoblast in vitro. Odontology 16 (2022): 2365
- Ratzkowski B, Koth VS, Azambuja AA, et al. Effect of tyrosine kinase inhibitor sunitinib on tissue repair at tooth extraction sites. Oral Dis 11 (2021): 36-58
- Okubo-Sato M, Yamagata K, Fukuzawa S, et al. Medication-Related Osteonecrosis of the Jaw Spontaneously Occurred In a Patient with Chronic Myelogenous Leukemia Only by Imatinib: A Report of a Rare Case. Case Rep Dent 21 (2021): 6621937.
- Oz I, Kaplan I, Kleinman S, et al. Medication-related osteonecrosis of the jaws associated with intravitreal administration of ranibizumab. Int J Oral Maxillofac Surg 49 (2020): 1589-1591.
- Varoni EM, Lombardi N, Villa G, et al. Conservative Management of Medication-Related Osteonecrosis of the Jaws (MRONJ): A Retrospective Cohort Study. Antibiotics (Basel) 10 (2021): 195.
- Nisi M, Karapetsa D, Gennai S, et al. Conservative surgical treatment of medication related osteonecrosis of the jaw (MRONJ) lesions in patients affected by osteoporosis exposed to oral bisphosphonates: 24 months follow-up. J Craniomaxillofac Surg 46 (2018): 1153-1158.
- Nastro ES, Musolino C, Allegra A, et al. Bisphosphonate-Associated Osteonecrosis of the Jaw in Patients with Multiple Myeloma and Breast Cancer. Acta Haematol 117 (2007): 181-187.
- Lawrence JL, Alfonso AR, Ross FL, Chiu ES, Fleisher KE. Management of stage 0 medication-related osteonecrosis if the jaw with hyperbaric oxygen therapy: a case report and review of the literature. Undersea Hyperb Med 47 (2021): 241-251.
- Maluf G, Caldas RJ, Fregnani ER, et al. A rare case of bevacizumab-related osteonecrosis of the jaw associated with dental implants. Int J Implant Dent 5 (2019): 34.
- Harper RP, Fung E. Resolution of Bisphosphonate-Associated Osteonecrosis of the Mandible: Possible Application for Intermittent Low-Dose Parathyroid Hormone [rhPTH(1-34)]. J Oral Maxillofacial Surg 65 (2007): 573-580.
- Vall H, Parmar M. Teriparatide. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2022).
- Watanabe A, Yoneyama S, Nakajima M, et al. Osteosarcoma in Sprague-Dawley rats after long-term treatment with teriparatide (human parathyroid hormone (1-34)). J Toxicol Sci 37 (2012): 617-629.
- Gilsenan A, Midkiff K, Harris D, et al. Teriparatide did not increase adult osteosarcoma incidence in a 15-Years US Postmarketing Surveillance Study. J Bone Miner Res 36 (2021): 244-251.
- Lau A, Adachi N. Resolution of osteonecrosis of the jaw after teriparatide [recombinant human PTH-(1-34)] therapy. J Rheumatol 36 (2009): 1835-1837.
- Tsai KY, Huang CS, Huang GM, et al. More on the resolution of bisphosphonate-associated osteonecrosis of the jaw. J Rheumatol 37 (2010): 675.
- Narongroeknawin P, Danila MI, Humphreys LG, et al. Bisphosphonate-associated osteonecrosis of the jaw, with healing after teriparatide: a review of the literature and a case report. Spec Care Dentist 30 (2010): 77-82.
- Cheung A, Seeman E. Teriparatide therapy for alendronate-associated osteonecrosis of the jaw. New England J Med 363 (2010): 2473-2474.
- Lee JJ, Cheng SJ, Jeng JH, et al. Successful treatment of advanced bisphosphonate-related osteonecrosis of the mandible with adjunctive teriparatide therapy. Head Neck 33 (2011): 1366-1371.
- Kwon YD, Lee DW, Choi BJ, et al. Short-term teriparatide therapy as an adjunctive modality for bisphosphonate-related osteonecrosis of the jaws. Osteoporos Int 23 (2012): 2721-2725.
- Ywamoto J, Yago K, Sato Y, et al. Teriparatide therapy for bisphosphonate associated osteonecrosis in the jaw in an elderly Japanese woman with severe osteoporosis. Clin Drug Investig 32 (2012): 547-553.
- Thumbigere-Math V, Gopalakrishnan R, Michalowicz BS. Teriparatide therapy for bisphosphonate related osteonecrosis of the jaw: a case report and narrative review. Northwest Dent 92 (2013): 12-18.
- Ohbayashi Y, Miyake M, Saway F, et al. Adjunct teriparatide therapy with monitoring of bone turnover markers and bone scintigraphy for bisphosphonate related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pat Oral Rad Endod 115 (2013): 5632.
- Narvàez J, Narvàez JA, Gòmez-Vaquero C, et al. Lack of response to teriparatide therapy for bisphosphonate-associated osteonecrosis of the jaw. Osteoporosis Int 24 (2013): 731-733.
- Yoshiga D, Yamashita Y, Nakamichi I, et al. Weekly teriparatide injenction successfuly treated advanced bisphosphonate related osteonecrosis of the jaws. Osteoporosis Int 24 (2013): 2365-2369.
- Kim KM, Park W, Oh SY, et al. Distinctive role of 6 month teriparatide treatment on intractable bisphosphonate related osteonecrosis of the jaw. Osteoporos Int 25 (2014): 1625-1632.
- Pelaz A, Junquera L, Gallego L, et al. Alternative treatments for oral bisphosphonate related osteonecrosis of the jaws: a pilot study comparing fibrin rich in growth factors and teriparatide. Med Oral Pat Oral Circ Bucal 19 (2014): 36-45.
- Neuprez A, Rompen E, Crielaard JM, et al. Teriparatide therapy for Denosumab induced osteonecrosis of the jaw in a male osteoporotic patient. Calcif Tissue Int 95 (2014): 94-96.
- Doh RM, Park HJ, Rhee Y, et al. Teriparatide therapy for bisphosphonate related osteonecrosis of the jaw associated with dental implants. Implant Dent 24 (2015): 222-226.
- Kakehashi H, Ando T, Minamizato T, et al. Administration of teriparatide improves the symptoms of advanced bisphosphonate related osteonecrosis of the jaw: preliminary findings. Int J Oral Maxillofac Surg 44 (2015): 1558-1564.
- Yao M, Shimo T, Ono Y, et al. Successful treatment of osteonecrosis induced fractured mandible with teriparatide therapy: a case report. Int J Surg Case Rep 21 (2016): 151-153.
- Zushi Y, Takaoka K, Tamaoka J, et al. Treatment with teriparatide for advanced Bisphosphonate Related Osteonecrosis of the Jaw around dental implants: a case report. Int J Implant Dent 3 (2017): 11.
- Jung J, Yoo HY, Kim JT, et al. Short-Term teriparatide and recombinat human Bone Morphogenetic Proteine 2 for rigenerative approach to Medication-Related Osteonecrosis of the Jaw: a preliminary study. Journal of Bone and Mineral Research 32 (2017): 2445-2452.
- Kim JY, Park JH, Jung HD, et al. Treatment of medication-related osteonecrosis of the jaw around the dental implant with a once weekly teriparatide: a case report and literature review. J Oral Implantol 45 (2019): 403-407.
- Ohbayashy Y, Iwasaki A, Nakai F, et al. A comparative effectiveness pilot study of teriparatide for medication-related osteonecrosis of the jaw: daily versus weekly administration. Osteoporos Int 31 (2019): 577-585.
- Morishita K, Yamada SI, Kawakita A, et al. Treatment outcomes of adjunctive teriparatide therapy for medication-related osteonecrosis of the jaw (MRONJ): a multicenter retrospective analysis in Japan. J Ortop Science 25 (2020): 1079-1083.
