Tocilizumab As A Potential Treatment for SARS-CoV2 Pneumonia in Cancer Patients: A Case Report of A Patient with Clinical-Radiological Dissociated Response
Article Information
Irene Moreno MD*, Maro de Miguel MD, PhD, Rafael Álvarez MD, Antonio Cubillo MD, PhD, Emiliano Calvo MD, PhD
HM Sanchinarro Hospital-START Madrid, Madrid, Spain
*Corresponding Author: Irene Moreno MD, HM Sanchinarro Hospital-START Madrid, Madrid, Spain
Received: 05 June 2020; Accepted: 29 June 2020; Published: 01 September 2020
Citation: Irene Moreno, Maro de Miguel, Rafael Álvarez, Antonio Cubillo, Emiliano Calvo. Tocilizumab As A Potential Treatment for SARS-CoV2 Pneumonia in Cancer Patients: A Case Report of A Patient with Clinical-Radiological Dissociated Response. Archives of Clinical and Medical Case Reports 4 (2020): 733-737.
Share at FacebookAbstract
In December 2019, a novel virus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused an outbreak of pneumonia in China. As known, this infection then resulted in a pandemia, being still some territories accross the World suffering from that. Currently, there is no specific treatment or approved vaccine and many clinical trials are investigating potential drugs. Among them, immunomodulators seems a group of drugs that could be useful in the Coronavirus-19 disease (Covid-19). Specially, in those cases where a cytokine storm occurs. This involves a considerable release of proinflammatory cytokine including several interleukins and tumour necrosis factor α (TNF-α) . Here, we report the successful treatment of a metastatic colorectal cancer patient hospitalized due to SARS-CoV-2 pneumonia with tocilizumab, an humanized monoclonal antibody against the interleukin-6 receptor (IL-6R).
Keywords
Acute respiratory syndrome; SARS-CoV-2; Immunomodulators; Tocilizumab
Acute respiratory syndrome articles, SARS-CoV-2 articles, Immunomodulators articles, Tocilizumab articles
Acute respiratory syndrome articles Acute respiratory syndrome Research articles Acute respiratory syndrome review articles Acute respiratory syndrome PubMed articles Acute respiratory syndrome PubMed Central articles Acute respiratory syndrome 2023 articles Acute respiratory syndrome 2024 articles Acute respiratory syndrome Scopus articles Acute respiratory syndrome impact factor journals Acute respiratory syndrome Scopus journals Acute respiratory syndrome PubMed journals Acute respiratory syndrome medical journals Acute respiratory syndrome free journals Acute respiratory syndrome best journals Acute respiratory syndrome top journals Acute respiratory syndrome free medical journals Acute respiratory syndrome famous journals Acute respiratory syndrome Google Scholar indexed journals syndrome articles syndrome Research articles syndrome review articles syndrome PubMed articles syndrome PubMed Central articles syndrome 2023 articles syndrome 2024 articles syndrome Scopus articles syndrome impact factor journals syndrome Scopus journals syndrome PubMed journals syndrome medical journals syndrome free journals syndrome best journals syndrome top journals syndrome free medical journals syndrome famous journals syndrome Google Scholar indexed journals SARS-CoV-2 articles SARS-CoV-2 Research articles SARS-CoV-2 review articles SARS-CoV-2 PubMed articles SARS-CoV-2 PubMed Central articles SARS-CoV-2 2023 articles SARS-CoV-2 2024 articles SARS-CoV-2 Scopus articles SARS-CoV-2 impact factor journals SARS-CoV-2 Scopus journals SARS-CoV-2 PubMed journals SARS-CoV-2 medical journals SARS-CoV-2 free journals SARS-CoV-2 best journals SARS-CoV-2 top journals SARS-CoV-2 free medical journals SARS-CoV-2 famous journals SARS-CoV-2 Google Scholar indexed journals Immunomodulators articles Immunomodulators Research articles Immunomodulators review articles Immunomodulators PubMed articles Immunomodulators PubMed Central articles Immunomodulators 2023 articles Immunomodulators 2024 articles Immunomodulators Scopus articles Immunomodulators impact factor journals Immunomodulators Scopus journals Immunomodulators PubMed journals Immunomodulators medical journals Immunomodulators free journals Immunomodulators best journals Immunomodulators top journals Immunomodulators free medical journals Immunomodulators famous journals Immunomodulators Google Scholar indexed journals Tocilizumab articles Tocilizumab Research articles Tocilizumab review articles Tocilizumab PubMed articles Tocilizumab PubMed Central articles Tocilizumab 2023 articles Tocilizumab 2024 articles Tocilizumab Scopus articles Tocilizumab impact factor journals Tocilizumab Scopus journals Tocilizumab PubMed journals Tocilizumab medical journals Tocilizumab free journals Tocilizumab best journals Tocilizumab top journals Tocilizumab free medical journals Tocilizumab famous journals Tocilizumab Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals pneumonia articles pneumonia Research articles pneumonia review articles pneumonia PubMed articles pneumonia PubMed Central articles pneumonia 2023 articles pneumonia 2024 articles pneumonia Scopus articles pneumonia impact factor journals pneumonia Scopus journals pneumonia PubMed journals pneumonia medical journals pneumonia free journals pneumonia best journals pneumonia top journals pneumonia free medical journals pneumonia famous journals pneumonia Google Scholar indexed journals caval syndrome articles caval syndrome Research articles caval syndrome review articles caval syndrome PubMed articles caval syndrome PubMed Central articles caval syndrome 2023 articles caval syndrome 2024 articles caval syndrome Scopus articles caval syndrome impact factor journals caval syndrome Scopus journals caval syndrome PubMed journals caval syndrome medical journals caval syndrome free journals caval syndrome best journals caval syndrome top journals caval syndrome free medical journals caval syndrome famous journals caval syndrome Google Scholar indexed journals
Article Details
1. Case Report
Human-affecting coronaviruses (HCoV) can produce clinical symptoms ranging from the common cold to more serious ones such as those caused by the Severe Acute Respiratory Syndrome (SARS) viruses and Middle East Respiratory Syndrome (MERS-CoV). Covid-19 is the term that encompassed the various clinical manifestations
(included SARS-COV2 pneumonia) caused by the emerging virus SARS-CoV-2 [1].
We report the successful treatment of a cancer patient hospitalized due to SARS-CoV-2 pneumonia with tocilizumab. Tocilizumab [2] is a humanized monoclonal antibody against the interleukin-6 receptor (IL-6R), mainly used for the treatment of rheumatoid arthritis and cytokine-release syndrome.Higher plasma levels of cytokines found in ICU patients in China [2] demonstrated that in the pathogenesis of SARS-CoV-2 pneumonia, a cytokine storm occurred, involving a considerable release of proinflammatory cytokine (including IL-6).
We present the case of a 64 year old gentleman with a history of well-controlled hypertension and KRAS-wildtype metastatic colorectal cancer. His last CT scan done as a F/U for his CRC showed no lung abnormalities with low volumen tumoral disease in partial response - just lymph node involvement on his inguinal area. Patient was at the time receiving treatment inhibiting LAG3 and PDL, being in response for almost a year. He presented to the emergency department (ED) with myalgia, anosmia, dyspnoea and temperature of more than 102,2 °F (39ºC) for 4 days. The physical examination was normal, except for tachycardia (as patient was febrile) and right basal rhonchi. Basal oxygen saturation was 88%. Lymphocites count was 0.47 × 10e3/μL (1.2 - 3.4 × 10e3/μL), D -Dimer was 643,0 ng/mL (< 500 ng/mL), C-reactive protein (CRP) was 409,64 mg/L (< 5 mg/L) (Figure 1).
Procalcitonine levels were low. Arterial Blood Gas (ABG) was: pH 7,47 (7.35 - 7.45), pCO2 32,0 mmHg (35.0 - 45.0) and pO2 53,0 mmHg (75.0 - 100.0). Chest x-ray showed a right basal infiltration. The initial diagnosis was an infectious pneumonia (possibly Covid-19 as per epidemiological situation). Because there was not seen the typical pattern on x-ray for Covid infection and patient had an active cancer being at risk of bacterial/fungal infections, antibiotics/antifungal treatment was also given (with EKG monitorization). A nasopharyngeal (NP) sample was taken for Covid-19 testing coming back as positive in the following day. Patient was started, following the hospital protocol, on colchicine, montelukast, hydroxychloroquine, lopinavir/ritonavir, azithromycin, meropenem, oseltamivir, fluconazole and linezolid. From day 2 to 3 patient had a rapid clinical worsening despite the treatment implemented with maintained high fever and need for oxygen supply with reservoir mask at 15 lpm. This clinical impairment was accompained by a radiological one (with consolidations involving all lobes on the chest film). CRP was up to almost 600 mg/L, lymphocytes went slightly down and D-D was also increased. Ferritine was elevated, as well as IL6 levels 118,3 pg/mL (<7). As blood cultures/legionella-pneumococco urinary antigent tests came back as negative and the Covid infection was confirmed, it was decided to take off antitibiotics/antifungal therapy and a high dose bolus of steroids was given (250 mg methylperdnisolone) on day 3. Later, on day 4, and despite steroids, patient had no improvement of his shortness of breath and oxygen saturation was again worsened (91-92% with 15 lpm reservoir mask). At this point it was decided to infuse him a single dose of 400 mg tocilizumab on the ward. From day 5 to day 8, patient improved rapidly with less dypsnoea since the following day of the tocilizumab infusion. Inflamatory markers were also better (including IL6 levels, RCP, Lymphocytes count and DD). There was first an impaitment on lung xray lesions after the tocilizumab infusion but followed with a reduction in the consolidative lesions in the next days. This clinical-radiological dissociation in COVID-19 has been previously described [4] (Figure 2). For instance, several previous reports described asymptomatic cases who had evidence of lung opacities on chest CT [5, 6].

Figure 1: Clinical/laboratory parameters over hospitalization time.
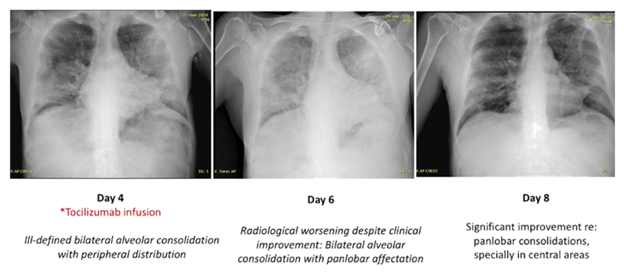
Figure 2: Chest xraybefore (day 4) and after (day 6 and 8) tocilizumab infusion.
On day 10 patient was not requiring any supplemental oxygen and a new NP sample was taken again for Covid19 being this negative. Patient was finally discharged home on day 12, with no medications. Outcomes from twenty-one patients treated with tocilizumab after being diagnosed of SARS-Cov2 pneumonia were reported in a retrospective clinical study from China [5]. It was shared a significant improvement on symptoms in a relevant number of patients (19/21 patients), oxygen intake and radiological/laboratorios features; with no obvious adverse reactions.
This clinical case shows how anti-IL6 therapy, as tocilizumab, may be effective for patients with severe SARS-COV2 pneumonia. This could be specially useful in patients who have no options for intensive therapies (such as mecanical ventilation or ICU treatments). In these patients, a prompt use of tocilizumab may reduce hospitalization times and fatal outcomes.
Furthermore, this case could be considered as another example of clinical-radiological dissociation in COVID-19. To the best of our knowledge, this discrepancy have not been reported in either MERS-CoV or SARS-Cov infection. Several hypotheses could explain this disparity. One possibility is that there would be a mismatch between the timing of CT/Xray positivity and clinical symptoms like in other types of pneumonia. Positive results in terms of symptoms, time of hospitalization and recovery derived from our patient experience are encouraging for the use of anti-interleukin therapy. However, there are several shortcomings on the assumptions derived from this single case report. Randomized and prospective trials with a higher number of patients are needed [6].
Conflicts of Interest
The authors declare no conflicts of interest.
References
- SARS-CoV-2: an Emerging Coronavirus that Causes a Global Threat. Int J Biol Sci 16 (2020): 1678-1685.
- Tocilizumab: A Review in Rheumatoid Arthritis. Drugs 77 (2017): 1865-1879.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (2020): 497-506.
- Chest CT Findings in Cases from the Cruise Ship “Diamond Princess” with Coronavirus Disease 2019 (COVID-19). Radiology: Cardiothoracic imaging (2020).
- Ng M-Y, Lee EY, Yang J, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiology: Cardiothoracic Imaging 2 (2020): e200034.
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. The Lancet Infectious Diseases (2020): 30086.
- Xu X, Han M, Li T, et al. Effective Treatment of Severe COVID-19 Patients with Tocilizumab. ChinaXiv:202003.00026v1.
- Mahase E. Covid-19: what treatments are being investigated? BMJ 368 (2020): 1252.
