To Maximize the Advantage of the Uprising Visualization System: Modified Retro-Sigmoidal Approach for Purely Endoscopic MVD Surgery for HFS
Article Information
Chongjing Sun1, Puyuan Zhao1, Chenghui Qu2, Jin Xu1, Xiaobiao Zhang1, Wei Zhu1*, Yu Zhang1*
1Department of Neurosurgery, Zhongshan Hospital, Fudan University, 180 Fenglin Road, Shanghai 200032, China
2Department of Anesthesiology, Zhongshan Hospital, Fudan University, 180 Fenglin Road, Shanghai 200032, China
*Corresponding Author: Wei Zhu and Yu Zhang. Department of Neurosurgery, Zhongshan Hospital, Fudan University, 180 Fenglin Road, Shanghai 200032, China.
Received: 17 January 2023; Accepted: 27 January 2023; Published: 03 February 2023
Citation:
Chongjing Sun, Puyuan Zhao, Chenghui Qu, Jin Xu, Xiaobiao Zhang, Wei Zhu, Yu Zhang. Modified Retro-Sigmoidal Approach for Purely Endoscopic MVD Surgery for HFS. Journal of Psychiatry and Psychiatric Disorders 7 (2023): 12-16.
Share at FacebookAbstract
Aim: The number of reports on endoscopic MVD for HFS has been growing swiftly. However, the majority of the literature has been focusing on the advantage of endoscope and the comparison between endoscope and microscope. Little was mentioned to modify the surgical approach to promote the use of endoscope. In order to maximize the advantage of endoscope, we present a series of HFS cases treated with MVD, using a retro-sigmoidal approach that is specially modified for purely endoscopic surgeries.
Method: 86 consecutive cases with primary HFS treated by our team with purely endoscopic MVD were retrospectively included in this study. During surgery, the patient’s head remained in a horizontal position without rotation for a face-down tendency and the vertex of the head was only slightly tilt towards the floor. Angled endoscopes were used for better view and more manipulating space.
Results: Of all the 86 patients, the symptom of 67 cases (77.9%) was released immediately after operation and in 15 (17.4%) cases there was a delayed relief. Post-operative neck and shoulder pain, mild transient hearing loss and transient facial paralysis were reported in 5 (5.8%), 3 (3.5%) and 2 cases (2.3%) respectively.
Conclusion: The modification of the retro-sigmoidal approach in order to facilitate the application of endoscope improved the intra-operative exposure and space for manipulation, and reduced the post-operative discomfort of the patients. Purely endoscopic MVD surgery is a safe and effective treatment for HFS.
Keywords
Modified approach; Retro-sigmoidal approach; Endoscope; Microvascular decompression; Hemifacial spasm
Modified approach articles; Retro-sigmoidal approach articles; Endoscope articles; Microvascular decompression articles; Hemifacial spasm articles
Modified approach articles Modified approach Research articles Modified approach review articles Modified approach PubMed articles Modified approach PubMed Central articles Modified approach 2023 articles Modified approach 2024 articles Modified approach Scopus articles Modified approach impact factor journals Modified approach Scopus journals Modified approach PubMed journals Modified approach medical journals Modified approach free journals Modified approach best journals Modified approach top journals Modified approach free medical journals Modified approach famous journals Modified approach Google Scholar indexed journals Retro-sigmoidal approach articles Retro-sigmoidal approach Research articles Retro-sigmoidal approach review articles Retro-sigmoidal approach PubMed articles Retro-sigmoidal approach PubMed Central articles Retro-sigmoidal approach 2023 articles Retro-sigmoidal approach 2024 articles Retro-sigmoidal approach Scopus articles Retro-sigmoidal approach impact factor journals Retro-sigmoidal approach Scopus journals Retro-sigmoidal approach PubMed journals Retro-sigmoidal approach medical journals Retro-sigmoidal approach free journals Retro-sigmoidal approach best journals Retro-sigmoidal approach top journals Retro-sigmoidal approach free medical journals Retro-sigmoidal approach famous journals Retro-sigmoidal approach Google Scholar indexed journals Endoscope articles Endoscope Research articles Endoscope review articles Endoscope PubMed articles Endoscope PubMed Central articles Endoscope 2023 articles Endoscope 2024 articles Endoscope Scopus articles Endoscope impact factor journals Endoscope Scopus journals Endoscope PubMed journals Endoscope medical journals Endoscope free journals Endoscope best journals Endoscope top journals Endoscope free medical journals Endoscope famous journals Endoscope Google Scholar indexed journals Microvascular decompression articles Microvascular decompression Research articles Microvascular decompression review articles Microvascular decompression PubMed articles Microvascular decompression PubMed Central articles Microvascular decompression 2023 articles Microvascular decompression 2024 articles Microvascular decompression Scopus articles Microvascular decompression impact factor journals Microvascular decompression Scopus journals Microvascular decompression PubMed journals Microvascular decompression medical journals Microvascular decompression free journals Microvascular decompression best journals Microvascular decompression top journals Microvascular decompression free medical journals Microvascular decompression famous journals Microvascular decompression Google Scholar indexed journals Hemifacial spasm articles Hemifacial spasm Research articles Hemifacial spasm review articles Hemifacial spasm PubMed articles Hemifacial spasm PubMed Central articles Hemifacial spasm 2023 articles Hemifacial spasm 2024 articles Hemifacial spasm Scopus articles Hemifacial spasm impact factor journals Hemifacial spasm Scopus journals Hemifacial spasm PubMed journals Hemifacial spasm medical journals Hemifacial spasm free journals Hemifacial spasm best journals Hemifacial spasm top journals Hemifacial spasm free medical journals Hemifacial spasm famous journals Hemifacial spasm Google Scholar indexed journals Root Entrance Zone articles Root Entrance Zone Research articles Root Entrance Zone review articles Root Entrance Zone PubMed articles Root Entrance Zone PubMed Central articles Root Entrance Zone 2023 articles Root Entrance Zone 2024 articles Root Entrance Zone Scopus articles Root Entrance Zone impact factor journals Root Entrance Zone Scopus journals Root Entrance Zone PubMed journals Root Entrance Zone medical journals Root Entrance Zone free journals Root Entrance Zone best journals Root Entrance Zone top journals Root Entrance Zone free medical journals Root Entrance Zone famous journals Root Entrance Zone Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals microscope articles microscope Research articles microscope review articles microscope PubMed articles microscope PubMed Central articles microscope 2023 articles microscope 2024 articles microscope Scopus articles microscope impact factor journals microscope Scopus journals microscope PubMed journals microscope medical journals microscope free journals microscope best journals microscope top journals microscope free medical journals microscope famous journals microscope Google Scholar indexed journals visualization system articles visualization system Research articles visualization system review articles visualization system PubMed articles visualization system PubMed Central articles visualization system 2023 articles visualization system 2024 articles visualization system Scopus articles visualization system impact factor journals visualization system Scopus journals visualization system PubMed journals visualization system medical journals visualization system free journals visualization system best journals visualization system top journals visualization system free medical journals visualization system famous journals visualization system Google Scholar indexed journals Abnormal Muscle Reaction articles Abnormal Muscle Reaction Research articles Abnormal Muscle Reaction review articles Abnormal Muscle Reaction PubMed articles Abnormal Muscle Reaction PubMed Central articles Abnormal Muscle Reaction 2023 articles Abnormal Muscle Reaction 2024 articles Abnormal Muscle Reaction Scopus articles Abnormal Muscle Reaction impact factor journals Abnormal Muscle Reaction Scopus journals Abnormal Muscle Reaction PubMed journals Abnormal Muscle Reaction medical journals Abnormal Muscle Reaction free journals Abnormal Muscle Reaction best journals Abnormal Muscle Reaction top journals Abnormal Muscle Reaction free medical journals Abnormal Muscle Reaction famous journals Abnormal Muscle Reaction Google Scholar indexed journals
Article Details
1. Introduction
Hemifacial Spasm (HFS) is a facial movement disorder, featured by involuntary and unilateral spasm of muscles innervated by facial nerve. It is caused by vascular compression on the Root Entrance Zone (REZ) of the facial nerve. A procedure aiming to identify the offending vessels and remove them from the facial nerve was invented by Jannetta. The procedure was named Microvascular Decompression (MVD) and has been established as the only cure for HFS. Traditionally the procedure was carried out under a surgical microscope.
Following its robust development in the past two decades, neuro-endoscope, as a visualization system, has participated in many aspects of neurosurgery. In a number of surgeries, the endoscope has even taken the place of microscope and functioned as the major visualization tool, e.g. trans-nasal skull base surgeries and ventricular surgeries. In MVD surgery for HFS, endoscope was initially used to provide supplementary view that was beyond the capacity of microscope [1,2]. As far as we are aware, the first report of fully endoscopic MVD was published in 2008 [3]. Since then, the number of reports on endoscopic MVD for HFS has been growing swiftly.
Up to now, the majority of the literature has been focusing on the advantage of endoscope and the comparison between endoscope and microscope. The application of endoscope provides superior illumination and visualization, revealing neurovascular conflicts that might be missed by microscopic survey, and minimizes the need for brain retraction and extensive dissection that might be inevitable in purely microscopic procedures [2-4]. There have been at least three reports comparing endoscope and microscope in MVD for HFS directly. Based on their meta-analysis, two team concluded that endoscopic MVD was superior to microscopic MVD both in perioperative and postoperative efficacy [4-8]. Conversely, Zhu J [9] stated that fully endoscopic MVD for HFS had a higher total incidence of complications than microscopic MVD. Generally speaking, in the setting of MVD procedure for HFS, endoscope can function at least as well as microscope according to the published data by far.
The retro-sigmoidal approach is one of the most classic neurosurgical approaches. Countless details of the approach have been modified for better surgical outcomes of MVD surgery in the era of microscope in which there were no other options if considerable accuracy and delicateness were required. Therefore, the retro-sigmoidal approach currently used in most centers, can be considered as achievement of continuous refinement to facilitate the application of microscope over decades. In most literature concerning endoscopic MVD, endoscope functioned merely as a supplement or replacement for microscope. Even in reports of purely endoscopic MVD, little was mentioned to modify the approach to promote the use of endoscope. Hence, in order to maximize the advantage of endoscope, we present a series of HFS cases treated with MVD, using a retro-sigmoidal approach that is specially modified for purely endoscopic surgeries.
2. Methods
2.1 Patient data
Patients’ date was retrospectively collected from cases of HFS treated with purely endoscopic MVD from October, 2019 to June, 2021 in our center. 86 cases with full follow-up data, including 24 (27.9%) male patients and 62 (72.1%) females, were enrolled. The symptom was on the left side in 47 cases (54.7 %) and on the right side in 39 cases (45.3%). There were no cases with bilateral symptom. The age of the patients ranged from 27 to 79 years old, with an average of 53.8 years. All patients were diagnosed by sign, symptom and cranial imaging studies. In all cases, Magnetic Resonance Tomographic Angiography (MRTA) was inspected preoperatively. Follow-up duration ranged from 6 to 26 months, with an average of 15.2 months.
2.2 Surgical procedure
All MVD procedures were performed via a suboccipital retro-sigmoid approach, using endoscope (Karl Storz GmbH and Co., Tuttlingen, Germany) as the only visualization system. The endoscope was fixed to a self-retaining holding device most of the time, and would be held by the assistant on condition that more flexible view was needed. The patients were under general anesthesia and Abnormal Muscle Reaction (AMR) monitoring was carried out intra-operatively.
The patients were placed in a lateral oblique position that was slightly different from the traditional manner. Unlike microscopic surgeries in which tremendous efforts have been made to create enough space for the operative microscope and the operating surgeons, more consideration could be taken into account for other aspects of the procedure in purely endoscopic MVD: (1) The head remain in a horizontal position without rotation for a face-down tendency in order that the cerebellum would be easily pulled away from the petrous bone by gravity (Figure 1). (2) For the purpose of patients’ post-operative comfort, the vertex of the head was only slightly tilt towards the floor and the upper shoulder needed not to be intensively retracted away from the neck.
Angled endoscopes, 30 degrees or 45 degrees, were used in most cases. Angled lenses can be used to look around the corner, enabling visualization of pathology that was not seen at 0 degree. In addition, the angled endoscope would be usually placed in a position that was more distant from the working instruments than 0-degree endoscope, creating an overlooking view. The precious space provided by the placement of the angled endoscope would greatly benefit the endoscopic manipulation, which was normally completed in a very crowded environment with 0-degree endoscope (Figure 2).
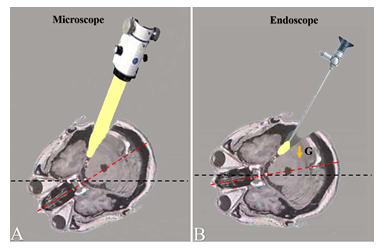
Figure 1: The difference between the head positions of the microscopic and endoscopic MVD surgeries. A: In microscopic MVD, the head of the patient is usually rotated face-down for a more vertical working angle. B: In microscopic MVD, the patient’s head can be placed in a more neutral position, which would allow gravity pull the cerebellum away from the petrosum (G= gravity).
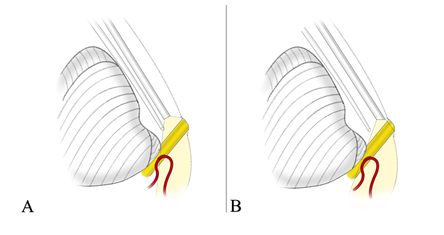
Figure 2: 0-degree lens and angled lens. A: When 0-degree endoscope is used, the view is regional and the endoscope is close to the surgical instrument, which leaves limited space for manipulation. B: Angled endoscope provides an over-looking view and more space for manipulation.
3. Results
3.1 Intra-operative findings
In all 86 cases, offending vessels were identified intra-operatively (Figure 3, 4 and 5). The responsible arteries included anterior inferior cerebellar artery (42, 48.8%), posterior inferior cerebellar artery (36, 41.99%), vertebral artery (17, 19.8%) and unspecific artery (5, 5.8%). More than one offending vessel was found in 14 cases (16.3%). The endoscope provided excellent view of the REZ of the facial nerve and the angled lenses made it even more difficult for the neurovascular compression to hide from surgical inspection. During the procedures, AMR was recorded in all the 86 cases. AMR disappeared in 81 cases at the end of the surgery (Figure 3, 4 and 5).
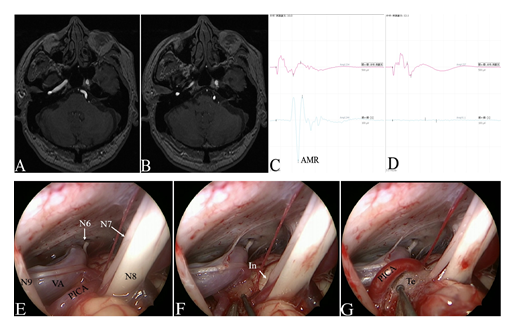
Figure 3: The case of left HFS (48 year’s old, male). A-B: Pre-operative MRTA images. C-D: AMR disappeared at the time of decompression. E-G: Intra-operative images showed the recognition and decompression of the offending vessels under endoscopic view. (N6=abducent nerve; N7=facial nerve; N8=vestibulocochlear nerve; N9=Glossopharyngeal nerve. VA= vertebral artery; PICA=posterior inferior cerebellar artery; In=indentation; Te=Teflon).
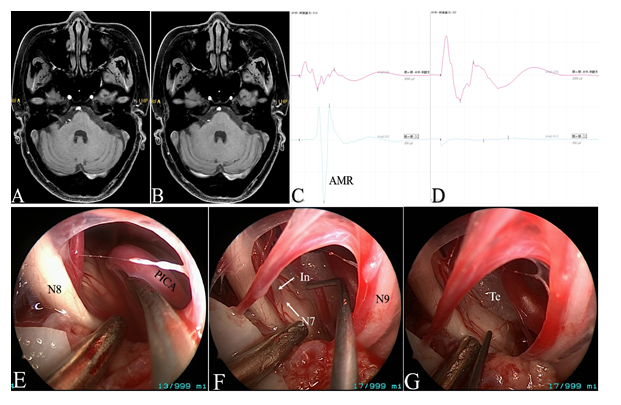
Figure 4: The case of right HFS (59 year’s old, female). A-B: Pre-operative MRTA images. C-D: AMR disappeared after decompression. E-G: Intra-operative endoscopic images. (N7=facial nerve; N8=vestibulocochlear nerve; N9=Glossopharyngeal nerve; PICA=posterior inferior cerebellar artery; In=indentation; Te=Teflon).
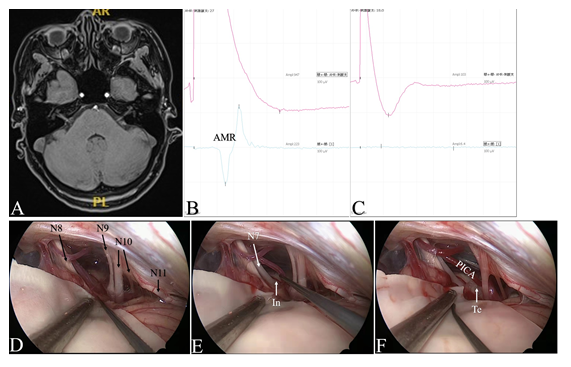
Figure 5: The case of right HFS (44 year’s old, female). A: Pre-operative MRTA images. B-C: AMR disappeared in the process of decompression. D-F: Intra-operative images under endoscopic view. (N7=facial nerve; N8=vestibulocochlear nerve; N9=Glossopharyngeal nerve; N10= vagus nerve; N11= accessory nerve; PICA=posterior inferior cerebellar artery; In=indentation; Te=Teflon).
3.2 Surgical outcomes
Of all the 86 patients, the symptom of 67 cases (77.9%) was released immediately after operation and in 15 (17.4%) cases there was a delayed relief. In 4 (4.7%) cases, there was no relief even at the latest follow-up (at least 6 months). 3 cases of recurrence were reported at the end of the follow-up period. Only 5 (5.8%) patients reported post-operative neck and shoulder pain, all of which resolved within 3 days. No critical complications, e.g. intra-cranial hematomas, intracranial infection, occurred in this series. Mild transient hearing loss was reported in 3 (3.5%) cases but the hearing all recovered at 3-months follow-up. 2 (2.3%) patients reported transient facial paralysis which was all resolved at early follow-up. There were no other post-operative complications.
|
Factors |
Value |
|
Age(years), mean ± SD |
53.8 ± 10.8 |
|
Sex |
|
|
Male (%) |
24 (27.9%) |
|
Female (%) |
62 (72.1%) |
|
HFS side |
|
|
Left (%) |
47 (54.7%) |
|
Right (%) |
39 (45.3%) |
|
Follow-up period (months), mean ± SD |
14.1 ± 7.6 |
|
(SD=standard deviation) |
|
Table 1: Clinical characteristics of the included cases.
|
Outcomes |
Number of cases (%) |
|
Relief |
82 (95.3%) |
|
Immediate Relief |
67 (77.9%) |
|
Delayed Relief |
15 (17.4%) |
|
No Relief |
4 (4.7%) |
|
Complications |
|
|
Post-operative neck and should pain |
5 (5.8%) |
|
Transient hearing loss |
3 (3.5%) |
|
Transient facial paralysis |
2 (2.3%) |
Table 2: Major surgical outcomes.
4. Discussion
As one of the pioneering neurosurgical centers in the field of endoscopic surgery in China, we have been performing and promoting purely endoscopic MVD surgery for years. According to our experience, endoscopic MVD procedures require smaller craniotomy and less retraction, and provide superior view of neurovascular compression with merely controlled dissection. Nonetheless, the focus of our study is not the advantage of the endoscope. In order to further promote the application of the endoscope in MVD surgeries, we aimed to adjust the surgical approach. The present study demonstrated that the modification of the retro-sigmoidal approach in order to facilitate the application of endoscope, especially the adjustment of patients’ position and the use of angled endoscope, improved the intra-operative exposure and space for manipulation, and reduced the post-operative discomfort of the patients. Excellent relief rate and minimum complication rate were achieved in this series.
The adjustment of patients’ positions not only promoted the application of endoscope, but also embodied its advantage. Theoretically, manipulation under a surgical microscope can be performed at any desired working angle. In practice, however, a more vertical angle is preferred, because a more horizontal working angle would require the surgeons to stretch their arms much more forward to make up for the space that was occupied by the microscope, which would greatly influence the persistence and stability of the manipulation. Therefore, when microscope is used, the head of the patient is usually rotated face-down for a more vertical working angle, which would unfortunately leave the cerebellum resting on the petrosum and probably require more retraction for adequate exposure (Figure 2). On the contrary, the endoscope provides the surgeons equal comfort level at all working angles. Hence in an endoscopic MVD procedure, the patient’s head can be placed in a more neutral position. Head position like this would allow gravity pull the cerebellum away from the petrosum, which would increase the exposure, decrease or even eliminate the need for retraction (Figure 2). In addition, outside the surgical field, the endoscope itself does not require so much space as the microscope. As a consequence, all the measures aimed for creating space for the operative microscope and the operating surgeons such as tilting the head towards the floor and retracting the shoulder caudally, became dispensable, erasing the discomfort that was frequently complained in microscopic cases.
The application of angled lenses provided superior view and space for manipulation. It was natural to consider lenes with different angles when endoscope was used to complete MVD, enabling visualization of pathology that was not seen at 0-degree [1]. In addition, according to our experience, the use of angled endoscope provided an over-looking view. The over-looking view improved the control of the overall situation, superior to the view of 0-degree lens that was more close-up and more regional. More importantly, under the current tendency towards smaller incision and smaller bone window, when the endoscope was added to the intracranial space, the endoscope itself became an obstacle for manipulation, especially for surgeons who had just taken up endoscope. The angled endoscope would be usually placed in a position that was more distant from the working instruments than 0-degree endoscope, creating precious extra space for the endoscopic manipulation.
Although the improvement provided by our modification might be trivial, it symbolized a new era for endoscopic neurosurgery. In the time of microscope, with no other options for MVD procedure, neurosurgeons had to tailor their surgical plans to the use of microscope. When the use of endoscope was introduced and even popularized, the majority of the neurosurgical community simply replaced the microscope with the endoscope and stuck to the surgical approach that was tailored to the microscope. When endoscope has already proved its safety and capacity in MVD [4,6,8], modification would be required to facilitate its application. Indeed, endoscope has its drawbacks, including blind areas in its lateral and rear visual fields, susceptibility to get dirtied by blood, water or fog, and relatively crowded space for manipulation. Nonetheless, it is all these limitations that require us to modify the procedure and allow us to expect an even better outcomes for endoscopic procedure in the future. On top of our research, efforts were made in other centers to promote the application of endoscope. Nagata et al. [7] described a multi-scope Technique, in which MVD is performed fully endoscopically using an exoscope that compensates for the intracranial blind area of the endoscopic view. Iwami et al. [5] reported their experience with underwater endoscopic surgery, in which the surgical field was continuously irrigated with artificial cerebrospinal fluid.
The current study was a single-centered retrospective study, with relatively small sample size and short follow-up period. Therefore, in the future, research with a larger sample size and control design is required to confirm the existing assumptions. Although the diameters of the endoscopes used in our series were identical, the diameter of the endoscope might be another factor that could influence the endoscopic procedure. Endoscope with a smaller diameter would take up less space, but the quality and range of the view would be compromised. Whether the application of thinner endoscope will benefit the surgical outcomes requires further study. We will consider addressing all these questions in future investigations.
5. Conclusion
The modification of the retro-sigmoidal approach in order to facilitate the application of endoscope, especially the adjustment of patients’ position and the use of angled endoscope, improved the intra-operative exposure and space for manipulation, and reduced the post-operative discomfort of the patients. Purely endoscopic MVD surgery is a safe and effective treatment for HFS.
Sources of funding:
The study was supported by the Clinical Research Project of Zhongshan Hospital, Shanghai, China. (No. 2020ZSLC18)
Highlights:
Through improvements in retro-sigmoidal approach, patients’ positioning, and use of angled endoscopes, purely endoscopic MVD surgery is a safe and effective treatment for HFS.
Disclosures:
The authors declare that they have no financial or other conflicts of interest in relation to this research and its publication.
Guarantors:
Wei Zhu M.D, Yu Zhang M.D.
Contributors:
Chongjing Sun and Puyuan Zhao have contributed equally to this work and should be considered as co-first authors.
References
- Blue R, Howard S, Spadola M, et al. Endoscopic Microvascular Decompression for Hemifacial Spasm: A Technical Case Report Demonstrating the Benefits of the Angled Endoscope and Intraoperative Neuromonitoring. Cureus 13 (2021): e16586.
- Broggi M, Acerbi F, Ferroli P, et al. Microvascular decompression for neurovascular conflicts in the cerebello-pontine angle: which role for endoscopy. Acta Neurochir (Wien) 155 (2013): 1709-1716.
- Cheng WY, Chao SC, Shen CC. Endoscopic microvascular decompression of the hemifacial spasm. Surg Neurol 70 (2008): 40-46.
- Feng BH, Zhong WX, Li ST, et al. Fully endoscopic microvascular decompression of the hemifacial spasm: our experience. Acta Neurochir (Wien) 162 (2020): 1081-1087.
- Iwami K, Watanabe T, Yokota M, et al. Feasibility of underwater microvascular decompression for hemifacial spasm: a technical note. Acta Neurochir (Wien) 163 (2021): 2435-2444.
- Li Y, Mao F, Cheng F, et al. A Meta-Analysis of Endoscopic Microvascular Decompression versus Microscopic Microvascular Decompression for the Treatment for Cranial Nerve Syndrome Caused by Vascular Compression. World Neurosurg 126 (2019): 647-655.e7.
- Nagata Y, Watanabe T, Nagatani T, et al. The Multiscope Technique for Microvascular Decompression. World Neurosurg 103 (2017): 310-314.
- Zhao Z, Chai S, Xiao D, et al. Microscopic versus endoscopic microvascular decompression for the treatment of hemifacial spasm in China: A meta-analysis and systematic review. J Clin Neurosci 91 (2021): 23-31.
- Zhu J, Sun J, Li R, et al. Fully endoscopic versus microscopic vascular decompression for hemifacial spasm: a retrospective cohort study. Acta Neurochir (Wien) 163 (2021): 2417-2423.
