Thenar Atrophy and Syncope as Signs of Thoracic Outlet Syndrome (TOS): A Clinical Electrophysiological Exploration of Three Cases
Article Information
Juna Musa1*, Luis Compres2, Adriano Valdez3, Adrian Puello3, Loran Rakovica4, Ali Guy5, Masum Rahman6, Barbara Martinez7, Ina Kola8, Ruben Blanco2
1Postdoctoral Research Fellow, Department of Surgery, Critical Care Trauma, Mayo Clinic, Rochester, MN, USA
2Department of Neurology, Centro Medico Vista del jardin Santa Domingo, Pontifica Universidad Catolica Madrey, Maestra, Dominican
3Doctor Hospital Metropolitano de Santiago, Faculty of Medicine HOMS, Dominican
4Medical Doctor, Faculty of Medicine, Prishtina, Kosovo
5Clinical Assistant Professor of Physical Medicine& Rehabilitation at NYU School of Medicine, NYU Medical center NY, USA
6Department of neurosurgery, Mayo clinic Rochester Minnesota, USA
7Department of Surgery, Universidad Autonoma de Bucaramanga, Columbia
8Department of “Burns and Plastic Surgery”, Tirana, Albania
*Corresponding Author: Juna Musa, Postdoctoral Research Fellow, Department of Surgery, Critical Care Trauma, Mayo Clinic, Rochester, MN, USA
Received: 27 July 2020; Accepted: 12 August 2020; Published: 14 September 2020
Citation: Juna Musa, Luis Compres, Adriano Valdez, Adrian Puello, Loran Rakovica, Ali Guy, Masum Rahman, Barbara Martinez, Ina Kola, Ruben Blanco. Thenar Atrophy and Syncope as Signs of Thoracic Outlet Syndrome (TOS): A Clinical Electrophysiological Exploration of Three Cases. Archives of Clinical and Medical Case Reports 4 (2020): 890-897.
Share at FacebookAbstract
Thoracic outlet syndrome (TOS) is a rare disease that presents with neurogenic and vascular symptoms and is caused by compression of the brachial plexus and/or subclavian vessels as they pass through the cervico thoraco brachial region. However, making the diagnosis of TOS can be challenging due to a lack of standardized objective confirmatory tests. We present three cases of neurovascular TOS where electrophysiological exploration was conducted to develop the diagnose.
Keywords
Neurogenic compression; Thenar atrophy; Thoracic outlet syndrome; Brachial plexus nerve compression; Venous compression
Neurogenic compression articles, Thenar atrophy articles, Thoracic outlet syndrome articles, Brachial plexus nerve compression articles, Venous compression articles
Neurogenic compression articles Neurogenic compression Research articles Neurogenic compression review articles Neurogenic compression PubMed articles Neurogenic compression PubMed Central articles Neurogenic compression 2023 articles Neurogenic compression 2024 articles Neurogenic compression Scopus articles Neurogenic compression impact factor journals Neurogenic compression Scopus journals Neurogenic compression PubMed journals Neurogenic compression medical journals Neurogenic compression free journals Neurogenic compression best journals Neurogenic compression top journals Neurogenic compression free medical journals Neurogenic compression famous journals Neurogenic compression Google Scholar indexed journals Thenar atrophy articles Thenar atrophy Research articles Thenar atrophy review articles Thenar atrophy PubMed articles Thenar atrophy PubMed Central articles Thenar atrophy 2023 articles Thenar atrophy 2024 articles Thenar atrophy Scopus articles Thenar atrophy impact factor journals Thenar atrophy Scopus journals Thenar atrophy PubMed journals Thenar atrophy medical journals Thenar atrophy free journals Thenar atrophy best journals Thenar atrophy top journals Thenar atrophy free medical journals Thenar atrophy famous journals Thenar atrophy Google Scholar indexed journals Thoracic outlet syndrome articles Thoracic outlet syndrome Research articles Thoracic outlet syndrome review articles Thoracic outlet syndrome PubMed articles Thoracic outlet syndrome PubMed Central articles Thoracic outlet syndrome 2023 articles Thoracic outlet syndrome 2024 articles Thoracic outlet syndrome Scopus articles Thoracic outlet syndrome impact factor journals Thoracic outlet syndrome Scopus journals Thoracic outlet syndrome PubMed journals Thoracic outlet syndrome medical journals Thoracic outlet syndrome free journals Thoracic outlet syndrome best journals Thoracic outlet syndrome top journals Thoracic outlet syndrome free medical journals Thoracic outlet syndrome famous journals Thoracic outlet syndrome Google Scholar indexed journals syndrome articles syndrome Research articles syndrome review articles syndrome PubMed articles syndrome PubMed Central articles syndrome 2023 articles syndrome 2024 articles syndrome Scopus articles syndrome impact factor journals syndrome Scopus journals syndrome PubMed journals syndrome medical journals syndrome free journals syndrome best journals syndrome top journals syndrome free medical journals syndrome famous journals syndrome Google Scholar indexed journals Brachial plexus nerve compression articles Brachial plexus nerve compression Research articles Brachial plexus nerve compression review articles Brachial plexus nerve compression PubMed articles Brachial plexus nerve compression PubMed Central articles Brachial plexus nerve compression 2023 articles Brachial plexus nerve compression 2024 articles Brachial plexus nerve compression Scopus articles Brachial plexus nerve compression impact factor journals Brachial plexus nerve compression Scopus journals Brachial plexus nerve compression PubMed journals Brachial plexus nerve compression medical journals Brachial plexus nerve compression free journals Brachial plexus nerve compression best journals Brachial plexus nerve compression top journals Brachial plexus nerve compression free medical journals Brachial plexus nerve compression famous journals Brachial plexus nerve compression Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Venous compression articles Venous compression Research articles Venous compression review articles Venous compression PubMed articles Venous compression PubMed Central articles Venous compression 2023 articles Venous compression 2024 articles Venous compression Scopus articles Venous compression impact factor journals Venous compression Scopus journals Venous compression PubMed journals Venous compression medical journals Venous compression free journals Venous compression best journals Venous compression top journals Venous compression free medical journals Venous compression famous journals Venous compression Google Scholar indexed journals tomography articles tomography Research articles tomography review articles tomography PubMed articles tomography PubMed Central articles tomography 2023 articles tomography 2024 articles tomography Scopus articles tomography impact factor journals tomography Scopus journals tomography PubMed journals tomography medical journals tomography free journals tomography best journals tomography top journals tomography free medical journals tomography famous journals tomography Google Scholar indexed journals
Article Details
1. Introduction
The thoracic outlet includes three confined spaces extending from the cervical spine and mediastinum to the lower border of the pectoralis minor muscle. The three compartments are the interscalene triangle, the costoclavicular space, and the retropectoralis minor space. The subclavian artery and the brachial plexus pass through these spaces. The subclavian vein does not cross the interscalene triangle, but runs beneath the anterior scalene before joining the internal jugular vein to form the brachiocephalic vein [1]. TOS classifications are based on the pathophysiology of symptoms with subgroups consisting of neurogenic (nTOS), venous (vTOS), and arterial (aTOS) etiologies. nTOS is by far the most common, representing about 95% of cases [2]. Numerous mechanisms elicit the characteristic pathology of TOS, including trauma, repetitive motions, and anatomic variations [3].
Patients with NTOS often present with pain, paresthesia, weakness, or numbness in the upper limbs. Symptoms of VTOS include acute pain, arm swelling, and blue discoloration. ATOS accounts for less than 5% of all TOS cases. Affected patients often experience arm pain, weakness, coolness, pallor, and paresthesia [4-6]. Making the diagnosis of TOS can be challenging, as criteria are controversial, and currently, there are no confirmatory tests, which commonly lead to delayed diagnosis in clinical practice [7]. A meticulous physical examination of potential TOS patients is a basic step in establishing a TOS diagnosis, followed by the collection of evidence related to history and clinical manifestations. Maneuvers such as the Adson, Wright, and Roos tests, as well as hyperabduction, can support the diagnosis. Imaging can also be helpful in confirming suspected cases of TOS. Anatomical abnormalities are demonstrated in radiographs. For suspected vascular TOS, ultrasound maintains high sensitivity and specificity, is noninvasive and inexpensive, and should be the initial imaging test of choice. CT or MR angiography can differentiate equivocal cases or provide additional anatomic detail required for surgical planning [8]. This case reports shows the importance of a meticulous examination and the use of imaging in the diagnosis of TOS.
2. Case Report
A 27-year-old female presented with periodic episodes of loss of consciousness, and progressive right thenar atrophy (Figure 1). Electroneuromyography (ENMG) evaluation showed a right lower primary trunk brachial plexus lesion sings (C8-T1) (Figure 2). A Computed Tomography Angiogram displayed an accessory right cervical rib, and a concomitant compression of the right subclavian artery by the scalene muscle (Figure 3). A neck MRI, showed compressions sings of the lower primary trunk of the brachial plexus (Figure 4).

Figure 1: Right thenar atrophy
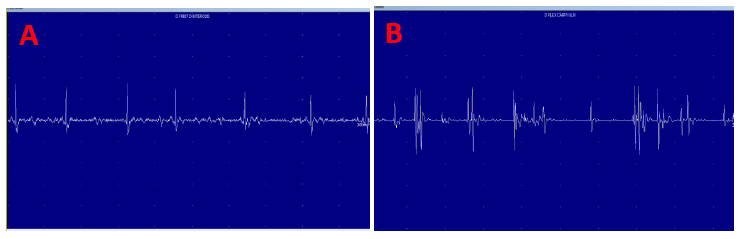
Figure 2: Neurogenic Atrophy signs of first interosseous muscle (A) Neurogenic atrophy signs of flexor Carpi Ulnaris (B).
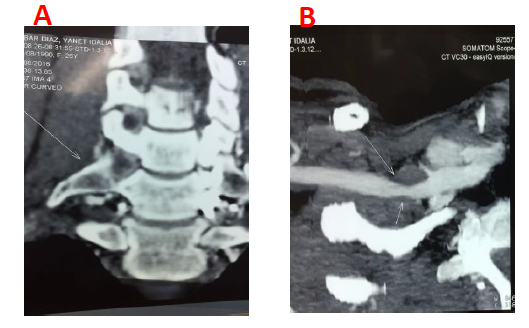
Figure 3: Accessory right cervical rib (A). Compression of the right subclavian artery by the scalene muscle (B).

Figure 4: Neck MRI showed compression sings of right lower primary trunk the brachial plexus.
A 33-year-old woman presented with progressive left thenar atrophy (Figure 5). ENMG studies pointed out to a left lower brachial plexus lesion C8-T1 (Figures 6-7). Cervical radiograph showed an accessory left cervical rib (Figure 8).

Figure 5: Left thenar atrophy.
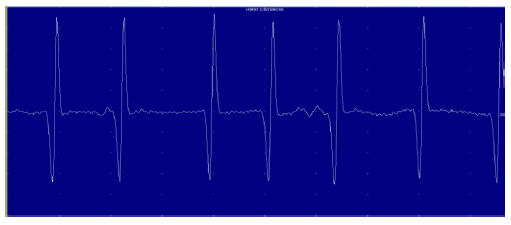
Figure 6: Neurogenic Atrophy signs of First Interosseous muscle.
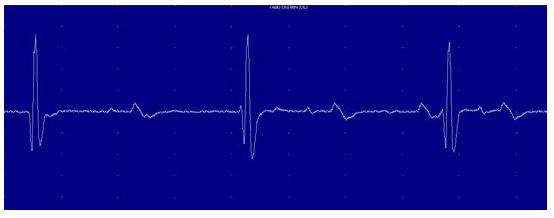
Figure 7: Neurogenic Atrophy signs of Abductor digiti minimi.
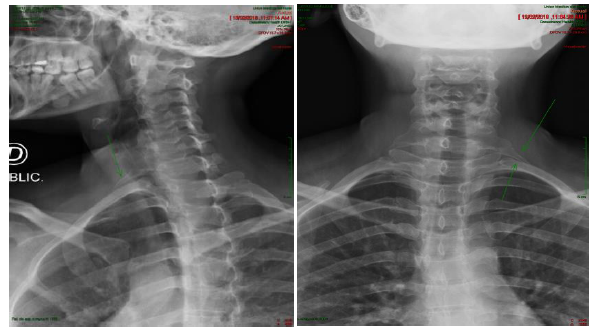
Figure 8: Cervical radiograph showed an accessory left cervical rib.
The third case is a 22-year-old female presented with episodes of conscience alteration and paresthesia in C8- T1 territory of the left upper limb. No involuntary movements or sphincter relaxation. Adson and Ross tests were positive on the left side. No ptosis, miosis, anhidrosis or atrophy of the hands was observed. EMG of the upper limbs revealed no abnormalities. Suspicion for thoracic outlet syndrome prompted Angio MRI study, which revealed impingement of the left subclavian artery due to an extrinsic compression of the scalene muscle.
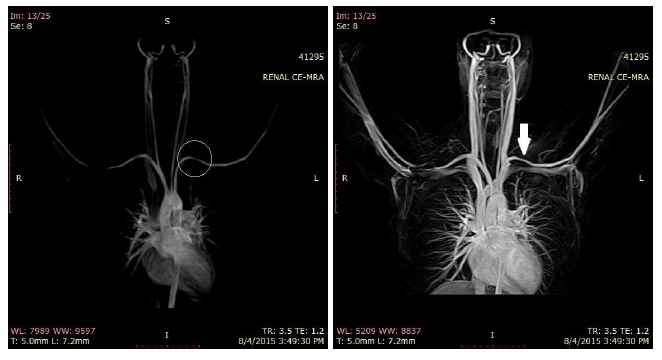
Figure 9: Angio MRI
3. Discussion
The initial presentation depends on structure primarily compressed, neurogenic, vascular, or a combination of both. Symptomatic patterns can be purely vascular, neurogenic, or nonspecific-type thoracic outlet syndrome. The vascular variant is rare and occurs due to the subclavian artery or vein compression and tends to occur in young individuals who perform heavily overhead arm activity. Upper extremity swelling, diffuse pain and venous distention are usual presentations in case of venous obstruction Whereas, patients with predominantly arterial obstruction frequently report upper extremity claudication, color changes, or constant dull pain. However, due to the presence of collateral circulation, most of the patient does not seek medical attention until the advanced stage of the disease, such as ulceration and gangrene. Chronic ischemia may result in generalized upper limb wasting. Nevertheless, as in one our cases, specific thenar atrophy is an infrequent and unusual presentation of the mixed variant of thoracic outlet syndrome. Neurogenic thoracic outlet syndrome involves the brachial plexus compression. A pure neurogenic variety is also unusual, and overhead arm activity is the contributing factor regardless. Most of the patients with nerve compression report difficulty grasping objects or hand weakness due to intrinsic muscle weakness. Moreover, pain, paraesthesia, and sensory loss are also reported frequently. However, isolated thenar atrophy is rarely seen, and may lead to a missed diagnosis. The nonspecific variant of thoracic outlet syndrome denotes a large group of patients with unexplained arm, shoulder, and neck pain.
Thoracic outlet syndrome is diagnosed by a combination of history, physical examination findings, and imaging. Physical examination findings are primarily related to the structure affected, thus the type of thoracic outlet syndrome. Depending on the variant suspected, patients are assessed with a variety of physical examinations that aid in confirming the diagnosis. Standard tests for neurogenic variants include Adson’s maneuver or the elevated arm stress test, and Elvey’s test, also known as the upper extremity tension test. In the Adson’s maneuver, the radial pulse is felt following the complete arm abduction and holding above the head. Elvey’s test is also performed similarly to provoke the symptoms. Dermatomal sensory test is also performed to demonstrate sensory disturbances as nerve compression in the thoracic outlet is considered to be exacerbated during this upper extremity tension test.
The vascular-thoracic outlet syndrome has distinct physical findings depending on whether the vein or artery is affected. Patients with predominant venous compression show edema and cyanosis of the upper extremity. Dilated superficial veins in the forearm, arm, shoulder, or chest also frequently demonstrated. Predominant arterial compression is characteristically presented with pallor, a diminished or absent pulse, and cold upper extremity. Blood pressure drop greater than 20 mm Hg in the affected side is also a reliable indicator of arterial involvement. In rare instances, small ischemic ulcers are noted in the hands and fingers. The classic physical examination finding in patients with neurogenic thoracic outlet syndrome includes atrophy of thenar, interosseous and hypothenar muscles along with reduced sensation along the ulnar nerve distribution as the lower trunk involve more frequently than the upper trunk.
Imaging is the mainstay to diagnose thoracic outlet syndrome. Cervical spine and upper thoracic spine X-ray can reveal bony abnormalities if present. Besides, Chest X-ray may also identify bony abnormalities. However, CT and MRI are more sensitive to identify anatomical defects causing the thoracic outlet syndrome or excluding the other possible diagnosis. Among all of the imaging, MRA is the best modality to detect arterial compression in vascular-thoracic outlet syndrome. Similarly, venography and duplex ultrasonography is used to demonstrate subclavian vein compression or thrombosis. These tests can be performed with dynamic position changing that reproduce the compression placed on the thoracic outlet by certain motions such as external rotation and abduction.
Electrodiagnostic studies are helpful when neurogenic thoracic outlet syndrome is highly suspect and useful when the results are positive. However, a negative test does not rule out the diagnosis. The most important findings on electroneuromyography evaluation of neurogenic outlet thoracic are signs brachial plexus lower primary trunk lesion as: medial brachial cutaneous and ulnar sensitive’s branches alterations, and neurogenic atrophy signs on the C8-T1 muscular territories. Nerve conduction velocity less than 85 m/s of either the ulnar or median nerves while crossing the thoracic outlet and has found to correlate the clinical diagnosis. Whereas, the conduction velocity of lower than 60 m/s is considered an indication for intervention. The somatosensory evoked potential is also considered as a useful diagnostic test, although controversial.
Conservative treatment with rest, NSAIDs, cervicoscapular strengthening exercises is effective in most patients. Additional modalities of conservative care can be installed as transcutaneous nerve stimulation and biofeedback. In general, surgical intervention and decompression should be considered for the patient’s refractory to conservative care, presented with acute vascular complications or progressive neurologic dysfunction. However, surgical decompression is indicated in patients with atrophy of hand muscles primarily due to thoracic outlet syndrome regardless of the neurovascular exam finding, as done in our cases. The thoracic outlet can be accessed by a trans-axillary or supraclavicular approach depending on the surgeon's preference. Either of these approaches sufficiently allow supraclavicular decompression.
4. Conclusion
The diagnosis of TOS remains challenging due to its varied clinical manifestations and lack of confirmatory testing and generally accepted diagnostic criteria. Based on this case reports and the reviewed literature, to optimize the diagnosis and treatment of the Thoracic outlet syndrome clinicians may suspect it when patients present episodes of altered consciousness and thenar atrophy and also be aware of the use of imaging techniques such as cervical spine or chest radiograph, CT angiography (CTA) and magnetic resonance angiography (MRA) as important tools in order to help to elucidate the diagnosis.
References
- Mackinnon SE, Novak CB. Thoracic outlet syndrome. Current Problems in Surgery 39 (2002): 1070-1145.
- Freischlag J, Orion K. Understanding thoracic outlet syndrome. Scientifica 2014 (2014).
- Ferrante MA, Ferrante ND. The thoracic outlet syndromes: Part 2. The arterial, venous, neurovascular, and disputed thoracic outlet syndromes. Muscle & Nerve 56 (2017): 663-673.
- Orlando MS, Likes KC, Mirza S, et al. A decade of excellent outcomes after surgical intervention in 538 patients with thoracic outlet syndrome. Journal of the American College of Surgeons 220 (2015): 934-939.
- Buller LT, Jose J, Baraga M, et al. Thoracic outlet syndrome: current concepts, imaging features, and therapeutic strategies. Am J Orthop 44 (2015): 376-382.
- Fugate MW, Rotellini-Coltvet L, Freischlag JA. Current management of thoracic outlet syndrome. Current Treatment Options in Cardiovascular Medicine 11 (2009): 176.
- 7. Wang XT, Yao M, Zhong M, et al. Thoracic outlet syndrome in a postoperative cervical spondylotic myelopathy patient: A case report. Medicine 98 (2019).
- Kuhn JE, Lebus GF, Bible JE. Thoracic outlet syndrome. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 23 (2015): 222-232.
