The Role of Vulnerable and Grandiose Narcissism in the Inpatient Treatment of Stress-Related Depressive Disorders
Article Information
Roberto La Marca1,2, Monika Scheiwiller1,2, Michael Pfaff1, Pearl La Marca-Ghaemmaghami2,3, Heinz Böker1,4*
1Centre for Stress-Related Disorders, Clinica Holistica Engiadina SA, Susch, Switzerland
2Clinical Psychology and Psychotherapy, University of Zurich, Zurich, Switzerland
3International Academy for Human Sciences and Culture, Walenstadt, Switzerland
4Psychiatric University Hospital, Department of Psychiatric Research, University of Zurich, Zurich, Switzerland
*Corresponding Author: Heinz Böker, Psychiatric University Hospital, Department of Psychiatric Research, University of Zurich, Zurich, Switzerland
Received: 25 April 2022; Accepted: 06 May 2022; Published: 08 June 2022
Citation: Roberto La Marca, Monika Scheiwiller, Michael Pfaff, Pearl La Marca-Ghaemmaghami, Heinz Böker. The Role of Vulnerable and Grandiose Narcissism in the Inpatient Treatment of Stress-Related Depressive Disorders. Journal of Psychiatry and Psychiatric Disorders 6 (2022): 142-161.
Share at FacebookAbstract
Depression relapse rates are high, therefore, identifying factors related to mental health and treatment outcome is important. We examined differences between inpatients with a stress-related depression and healthy controls regarding narcissism, stress, resource alterations, exhaustion, and depression. Twenty-one healthy controls and 36 inpatients with a stress-related depressive disorder completed questionnaires assessing vulnerable and grandiose narcissism (PNIvn, PNIgn), perceived stress (PSS), resource gain and actual or threatened resource loss during the past six months (COR-Egain, COR-Eloss, COR-Eloss?), vital exhaustion (MQ), and depression severity (BDI-II). Depression severity was additionally assessed using the HAMD17. Most data was assessed repeatedly, i.e. after treatment initiation, before treatment termination, and at six months follow-up. Inpatients revealed significantly higher levels of PSS, COR-Eloss, COR-Eloss?, MQ, BDI-II, HAMD17, and PNIvn, while PNIgn reached a trend significance level. In healthy controls, PNIvn correlated positively with COR-Eloss. In inpatients, PNIvn was positively related to levels of PSS, COR-Eloss, COREloss?, and BDI-II, while PNIgn was positively correlated with levels of PSS. Higher PNIvn at the beginning was further significantly associated with a stronger decrease in PSS until follow-up, and in BDI-II until the end or followup. These results underline the importance of personality factors in the treatment of stress-related depression.
Keywords
Depression; Stress; Narcissism; Grandiose; Vulnerable; Resource loss; Resource gain
Depression articles; Stress articles; Narcissism articles; Grandiose articles; Vulnerable articles; Resource loss articles; Resource gain articles
Depression articles Depression Research articles Depression review articles Depression PubMed articles Depression PubMed Central articles Depression 2023 articles Depression 2024 articles Depression Scopus articles Depression impact factor journals Depression Scopus journals Depression PubMed journals Depression medical journals Depression free journals Depression best journals Depression top journals Depression free medical journals Depression famous journals Depression Google Scholar indexed journals Stress articles Stress Research articles Stress review articles Stress PubMed articles Stress PubMed Central articles Stress 2023 articles Stress 2024 articles Stress Scopus articles Stress impact factor journals Stress Scopus journals Stress PubMed journals Stress medical journals Stress free journals Stress best journals Stress top journals Stress free medical journals Stress famous journals Stress Google Scholar indexed journals Narcissism articles Narcissism Research articles Narcissism review articles Narcissism PubMed articles Narcissism PubMed Central articles Narcissism 2023 articles Narcissism 2024 articles Narcissism Scopus articles Narcissism impact factor journals Narcissism Scopus journals Narcissism PubMed journals Narcissism medical journals Narcissism free journals Narcissism best journals Narcissism top journals Narcissism free medical journals Narcissism famous journals Narcissism Google Scholar indexed journals Grandiose articles Grandiose Research articles Grandiose review articles Grandiose PubMed articles Grandiose PubMed Central articles Grandiose 2023 articles Grandiose 2024 articles Grandiose Scopus articles Grandiose impact factor journals Grandiose Scopus journals Grandiose PubMed journals Grandiose medical journals Grandiose free journals Grandiose best journals Grandiose top journals Grandiose free medical journals Grandiose famous journals Grandiose Google Scholar indexed journals Vulnerable articles Vulnerable Research articles Vulnerable review articles Vulnerable PubMed articles Vulnerable PubMed Central articles Vulnerable 2023 articles Vulnerable 2024 articles Vulnerable Scopus articles Vulnerable impact factor journals Vulnerable Scopus journals Vulnerable PubMed journals Vulnerable medical journals Vulnerable free journals Vulnerable best journals Vulnerable top journals Vulnerable free medical journals Vulnerable famous journals Vulnerable Google Scholar indexed journals Resource loss articles Resource loss Research articles Resource loss review articles Resource loss PubMed articles Resource loss PubMed Central articles Resource loss 2023 articles Resource loss 2024 articles Resource loss Scopus articles Resource loss impact factor journals Resource loss Scopus journals Resource loss PubMed journals Resource loss medical journals Resource loss free journals Resource loss best journals Resource loss top journals Resource loss free medical journals Resource loss famous journals Resource loss Google Scholar indexed journals Resource gain articles Resource gain Research articles Resource gain review articles Resource gain PubMed articles Resource gain PubMed Central articles Resource gain 2023 articles Resource gain 2024 articles Resource gain Scopus articles Resource gain impact factor journals Resource gain Scopus journals Resource gain PubMed journals Resource gain medical journals Resource gain free journals Resource gain best journals Resource gain top journals Resource gain free medical journals Resource gain famous journals Resource gain Google Scholar indexed journals perceived stress articles perceived stress Research articles perceived stress review articles perceived stress PubMed articles perceived stress PubMed Central articles perceived stress 2023 articles perceived stress 2024 articles perceived stress Scopus articles perceived stress impact factor journals perceived stress Scopus journals perceived stress PubMed journals perceived stress medical journals perceived stress free journals perceived stress best journals perceived stress top journals perceived stress free medical journals perceived stress famous journals perceived stress Google Scholar indexed journals mental health articles mental health Research articles mental health review articles mental health PubMed articles mental health PubMed Central articles mental health 2023 articles mental health 2024 articles mental health Scopus articles mental health impact factor journals mental health Scopus journals mental health PubMed journals mental health medical journals mental health free journals mental health best journals mental health top journals mental health free medical journals mental health famous journals mental health Google Scholar indexed journals personality factor articles personality factor Research articles personality factor review articles personality factor PubMed articles personality factor PubMed Central articles personality factor 2023 articles personality factor 2024 articles personality factor Scopus articles personality factor impact factor journals personality factor Scopus journals personality factor PubMed journals personality factor medical journals personality factor free journals personality factor best journals personality factor top journals personality factor free medical journals personality factor famous journals personality factor Google Scholar indexed journals
Article Details
1. Introduction
1.1. Depressive Disorders and Stress
Mood disorders have high prevalence rates [1, 2]. A recent study conducted in a community sample in Switzerland applying the DSM-5 criteria found a lifetime prevalence of 28.2% for major depressive disorder [3]. In addition, depressive disorders are highly debilitating, ranking third with regard to years lived with disability (YLDs) (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018) [4] and thirteenth regarding disability-adjusted life-years (DALYs) (GBD 2019 Diseases and Injuries Collaborators, 2020) [5]. Besides the subjective burden, economic burden is very high too [6]. In Switzerland, the annual costs of depression were estimated at 8.1-8.3 billion Euros [7]. Furthermore, Major Depressive Disorder (MDD) is a major contributor to the burden of suicide and ischemic heart disease.
Stress is an important aetiopathogenic factor in the development of depressive disorders [8-10]. Similarly, loss of resources is related to depression [11-13]. According to the Conservation Of Resources (COR) theory, experiencing a loss of resources (e.g., material, personal and social resources), facing the threat of resource loss, and failing to gain resources after investing resources can cause psychological distress [14, 56]. The COR theory further assumes that losses of resources are disproportionately more impactful than resource gain (i.e. primacy of resource loss), and that lacking and loosing resources makes people more vulnerable to further losses (i.e. loss spirale). With time, continuing losses of resources can lead to chronic depletion of energy, leading to burnout with emotional detachment, defensive behaviour, and finally to depression [15].
1.2. Narcissism and Stress
Besides stress, personality factors are a further risk factor in the development of depressive disorders. One construct of interest is narcissism. The construct of narcissism is inconsistently defined, including normal to more pathological forms of the construct. Pincus et al. [16] developed the Pathological Narcissism Inventory (PNI). The PNI is a self-report measure assessing seven dimensions of pathological narcissism, spanning problems with narcissistic grandiosity (Entitlement Rage, Exploitativeness, Grandiose Fantasy, Self-sacrificing Self-enhancement) and narcissistic vulnerability (Contingent Self-esteem, Hiding the Self, Devaluing). “Grandiose PNI scales are positively related to a range of vindictive, domineering, intrusive, and overly-nurturant interpersonal problems. […] Vulnerable PNI scales are positively related to cold, socially avoidant, exploitable interpersonal problems.” (p. 376 [16]). Vulnerable narcissism involves the experience of helplessness, emptiness, low self-esteem, and shame and is also linked with "the use of social avoidance to cope with threats to the self by shamefully withdrawing when ideal self-presentation is not possible or needed admiration is not forthcoming" (p. 367 [16; 51]). In a sample of undergraduates (N=251) [50], mainly vulnerable but also grandiose narcissism (PNI) was significantly positively related to perceived stress (Perceived Stress Scale, PSS; [17]). Differently, in a community sample (N=346) [18], vulnerable narcissism (Hypersensitive Narcissism Scale, HSNS; 31) was significantly positively, while grandiose narcissism (Narcissistic Personality Inventory, NPI-13; [19]) was significantly negatively correlated with perceived stress (PSS-10; [17]).
1.3. Narcissism and Depression
With regard to depression, the association with grandiose and vulnerable narcissism was examined within assumably healthy subjects, outpatients and inpatients. Morf et al. [20] tested different subgroups mainly consisting of students and found a positive association mainly between vulnerable but also grandiose narcissism (PNI) and depressive symptoms (CES-D), while a second questionnaire assessing mainly grandiose narcissism (NPI; [21]) was negatively correlated with the CES-D score. The authors explain the inconsistent associations between depressive symptoms and grandiose narcissism by pointing out that the grandiose scales have some overlap (with regard to entitlement, pride and aggression), while there are also divergences (with regard to self-esteem, negative emotions, dysfunctional behaviour, and interpersonal problems). Similarly, Papageorgiou et al. [22], who also examined students, found a positive association of vulnerable narcissism (Five-Factor Narcissism Inventory - Short Form; FFNI-SF; [23] with depressive symptoms (BDI), but a negative association of grandiose narcissism (FFNI-SF) with depressive symptoms. Tritt et al. [24], who examined depressive temperament instead of symptoms in undergraduates, found a positive correlation with vulnerable narcissism, but no significant association with grandiose narcissism (PNI). Inpatients at a hospital specialized in the treatment of job stress-related disorders were examined with regard to the above mentioned link, revealing a significant positive association between overall narcissism (Narcissism Inventory, NI-20; [25] and depressive symptoms (BDI) [26]. In a sample of psychiatric outpatients (primary diagnosis: depressive disorders: 28.5%; psychoactive substance use disorders: 23%; anxiety disorders: 21%; etc.), Marcinko et al. [53] showed a positive correlation between depressive symptoms (Depression, Anxiety, Stress Scales; DASS-21; [28] and narcissistic vulnerability and grandiosity (PNI). In outpatients from a community mental health center, Ellison et al. [43] found a significant positive association between narcissistic vulnerability but not grandiosity (PNI) and depression symptoms (Treatment Outcome Package, TOP; [29]. Similarly, Jaksic et al. [27] investigated the relationships between pathological narcissism (PNI) and suicidal ideation in psychiatric outpatients, and found narcissistic vulnerability but not grandiosity to be significantly positively correlated with acute suicidal ideation (Suicide Assessment Scale - self-report, SUAS-S; [30]. A further study examining the association of vulnerable narcissism (assessed with the Hypersensitive Narcissism Scale, HSNS: [31]) and depression severity (BDI) in dysthymic outpatients supported a significant positive association between the two constructs [32]. Differently, in mixed samples of psychiatric outpatients [33, 34], positive but non-significant direct associations were revealed between narcissistic vulnerability and grandiosity (PNI) and depressive symptom severity (Patient Health Questionnaire, PHQ-9; [35]). In addition, De Page and Merckelbach [36] examined the association between narcissism (NPI; [37]) and depression (BDI-2) in 147 mixed patients (referral reasons: depression: 20%; personality and/or adjustment disorders: 20%; occupational stress: 10%; etc.) and found an inverse but non-significant association. Watson et al. [38] applied different narcissism scales in a large sample of patients at a private medical/surgical hospital, meeting the DSM-III criteria for alcohol and drug abuse, which were participating in a 4-6 week alcoholism treatment program. While covert (i.e. vulnerable) narcissism (MMPI Narcissistic Personality Disorder Scale, NPDS; [52]) revealed to be significantly positively related to depression, overt (i.e. grandiose) narcissism (as measured with various scales) was significantly negatively related to depression. In conclusion, studies in healthy as well as clinical samples provide evidence for depressive symptoms to be positively associated with vulnerable narcissism, while the association with narcissistic grandiosity holds incongruent results, probably in part due to different questionnaires used to assess narcissism.
Regarding the prediction of mental health treatment outcome, personality traits have received some attention. A meta-analysis examining the effect of comorbid personality disorder in depressive disorders [39] found that having a comorbid personality disorder, in contrast to none, is associated with a poorer outcome of depression. In line with this, meeting criteria for a comorbid cluster B personality disorder (i.e. histrionic, borderline, narcissistic, antisocial) in patients with a major depressive disorder being treated with fluoxetine for 8 weeks revealed a non-significantly smaller absolute and/or percentage reduction in HAMD-17 scores [40, 41] as well as in perceived stress [40]. Similarly, comorbid cluster B personality disorder predicted higher rates of depression recurrence over a two-year course of maintenance interpersonal psychotherapy [42]. With regard to the PNI, neither vulnerable nor grandiose narcissism predicted rates of linear change in depression during early psychotherapy (i.e. after seven therapy sessions) in a sample of outpatients with mainly mood, anxiety, and/or personality disorders [43].
The aim of the present analyses was to examine the association of narcissistic vulnerability and grandiosity with stress, resource alterations and depressive symptoms at baseline as well as in response to treatment.
2. Methods
2.1. Subjects and study design
This study is part of a larger study examining biopsychological differences between healthy controls and inpatients with stress-related depressive (or adjustment) disorders, as well as the effects of inpatient treatment. Inpatients at a specialized clinic for stress-related mental disorders (Clinica Holistica Engiadina SA, Susch, Switzerland) and healthy controls were recruited through flyers, advertisements at the clinic, and verbally by the clinic staff. Interested participants received written information and were additionally offered to participate in an optional briefing addressing the most important aspects of the study. General inclusion criteria were an age range between 18-65 years and fluency in the German language. Moreover, inpatients were included if they had an assumed stress-related depressive or adjustment disorder (i.e. a primary diagnosis of F32, F33, F34.1 or F43.2, combined with a Z73 code), while healthy controls were included if they had neither a current nor a past mental disorder, i.e. never received a diagnosis and in- or outpatient treatment. Furthermore, healthy controls were age-, sex-, and education matched to fit comparisons with the inpatients. Exclusion criteria were the same for all subjects. They consisted of acute risk for suicide, a history of organic brain disorders or severe cognitive impairment, a serious or disruptive medical condition (e.g., neoplasms, underweight, class III obesity (BMI>40.0), neurological, endocrine, cardiovascular, inflammatory and autoimmune disease), a serious or disruptive psychiatric disorder (i.e. substance abuse, bipolar, psychotic, eating, obsessive, compulsive, impulse control, attention deficit hyperactivity, and post-traumatic stress disorder), a current and regular medication with severe or disruptive drugs (i.e. antihypertensives, anti-inflammatory drugs, neuroleptics, amphetamines, benzodiazepine (daily or within the last 2 days), statins, steroids, antiepileptics, thyroid hormone, antiparkinsonian, analgesics, antibiotics within the last month, hay fever or cold medication (within the last 7 days), pain medication (daily or within the last 2 days)), pregnancy or lactation. This study was conducted in accordance with the declaration of Helsinki and was approved by the Ethics Committee of the Canton of Zurich. Subjects, who signed an informed consent before participating, were remunerated with 100 Swiss Francs before the end of the treatment. This study was integrated in a routinely conducted treatment program for stress-related mental disorders at the Clinica Holistica Engiadina, which is in line with recommendations for the multimodal treatment of clinical burnout [44]. Questionnaires were completed at three time points: 1) shortly after the beginning of treatment, 2) shortly before the end of the treatment, and 3) 6 months after the end of treatment (= follow-up).
2.2. Psychometric Measures
2.2.1. Pathological Narcissism Inventory
To assess pathological narcissism, the German version of the Pathological Narcissism Inventory (PNI; [20] was completed at the beginning of the treatment. The PNI consists of 54 items, which can be answered on a 6-point Likert scale (from 1=’not at all like me’ to 6=’very much like me’). Besides a total score, the 54 items can be divided into seven subscales, which can be subsumed into two superordinate subscales, i.e. grandiose narcissism (including the items of the four subscales ‘entitlement rage’, ‘exploitative’, ‘grandiose fantasy’, and ‘self-sacrificing self-enhancement’) and vulnerable narcissism (including the items of the three subscales ‘contingent self-esteem’, ‘hiding the self’, ‘devaluating’). To avoid multiple testing, we conducted analyses only considering the total, narcissistic grandiosity and narcissistic vulnerability scales. The coefficient alpha for the total score is .94 and .95 [20].
2.2.2. Loss and Gain of Resources and Stress
To assess resource loss as an index of stress, the ‘Conservation of Resources’ questionnaire (COR-E;[54]) was applied. The COR-E contains 74 items, which can be answered on a 5-point Likert scale (from 0=’not at all’ to 4=’to a great degree’). This questionnaire was adapted to assess the extent of actual loss (COR-Eloss) and threatened loss (COR-Eloss?) in the last six months. Additionally, the questionnaire was used to assess the extent of gain (COR-Egain) in the past six months. The COR-E was completed twice, at the beginning of the treatment and at 6 months follow-up.
With regard to perceived stress, the ‘Perceived Stress Scale (PSS;[17]) was applied. The 14 items of the PSS can be answered on a 5-point Likert scale (from 0=‘never’ to 4=‘very often’) and summed up to define a sum score. The answers refer to the last month. Like the COR-E, the PSS was completed twice, at treatment beginning and at 6 months follow-up. Cronbach’s alpha is reportedly high, i.e. .84 to .86 [17].
2.2.3. Vital exhaustion
Vital exhaustion was assessed using the Shortened Maastricht Exhaustion Questionnaire (MQ; [45]), consisting of 9 items which are rated on a 3-point Likert scale (from 0=’no’ to 2=’yes’), referring to symptoms at present. The sum lies between 0 and 18 points, with higher values indicating higher exhaustion. The MQ was completed at all three time points. Cronbach’s alpha is reported to be .83 [46].
2.2.4. Depression
The severity of depressive symptoms was assessed with the Beck Depression Inventory (BDI-II; [47]). Each of the 21 item is rated on a 4-point Likert scale (from 0=’not at all’ to 3=’extreme form of every symptom’) covering symptoms over the previous two weeks. The BDI-II total score ranges between 0 and 63 points, with higher values indicating higher severity. The questionnaire was distributed at all three time points. Cronbach’s alpha is reported to be .89 to .93 [48].
Furthermore, depressive symptoms were assessed using the clinician-administered Hamilton Depression scale (HAMD-17, [49]). The intensity of some symptoms (e.g., depressed mood, suicidal ideation, decreased interest, or psychomotor retardation) was rated from 0 to 4 (0=’none/absent’ to 4=’most severe’), whereas other symptoms’ intensity (e.g., decreased appetite or general somatic symptoms) was rated from 0 to 2 (0=’none/absent’ to 2=’severe’). The HAMD-17 was assessed at the beginning and the end of the treatment.
3. Data Analyses
Analyses were conducted using IBM SPSS Statistics version 24.0 for Macintosh (IBM Corp., Armonk, N.Y., USA). Besides absolute values, delta values were used, obtained by subtracting scores at the beginning from scores at the end of the treatment (Δpost) or at follow-up (Δfollow-up). Since the COR-E, with its 74 items, revealed some missings, means were calculated in cases where a maximum of three answers were missing. Prior to analyses, the Kolmogorov-Smirnov test was used to examine violations of the assumption of normal distribution, while the Levene’s test was applied to examine violations of the assumption of homogeneity of variance. Concerning differences in demographic variables between patients and healthy controls, the Pearson’s Chi2 or Mann-Whitney U test were applied. The latter was also computed when examining group differences in psychometric data. In order to assess associations between variables, Pearson’s product-moment or Spearman rank-order correlations were conducted. When interested in alterations related to the inpatient treatment, repeated-measures analyses of variances (rANOVA) were computed. In case a Mauchly test indicated that the assumption of sphericity was violated, a Huynh-Feldt correction was applied. If assumptions for rANOVA were not met, a Friedman test was conducted instead. All analyses were two-tailed and the level of significance was set at p < .05, while trends towards significance (.05 < p < .10) are also mentioned.
4. Results
4.1. Participants and Group Differences
From the originally included 21 healthy controls and 39 inpatients, three inpatients had to be excluded retrospectively based on the exclusion criteria (one inpatient revealed an F31 diagnosis, another had exercise-induced asthma, and in the case of a third inpatient, the Z73 code was removed). In the remaining sample of participants, the inpatients did not differ significantly from the healthy controls concerning gender distribution, age, BMI and education (Table 1).
|
Variables |
Patients |
Healthy controls |
Statistics |
|
Sex: female/male [absolute numbers] |
19/17 |
11/10 |
X2 = .001, p=.98 |
|
Age [years] |
46.42 (10.38) |
48.67 (9.84) |
U=335.000, p=.48 |
|
Body Mass Index, BMI [kg/m2] |
24.93 (3.89) |
24.59 (3.34) |
U=352.000, p=.79 |
|
P-values represent two-sided tests. |
|||
Table 1: Means and standard deviations of demographic variables of patients and healthy controls.
In contrast, both groups differed significantly with regard to depression (BDI-II, HAMD17: both p < .001), vital exhaustion (MQ: p < .001), and perceived stress (PSS: p < .001) (Table 2), with patients showing higher values. Concerning the conservation of resources, patients reported a significant larger extent of actual and threatened loss (both p < .001), while they did not differ from healthy controls with regard to the extent of resource gains (p = .34).
Compared to healthy controls, patients also had significant higher scores in total and vulnerable narcissism (both p < .001), and a trend towards significantly higher levels of grandiose narcissism (p = .07; Table 2).
|
Questionnaires |
(Sub-)scales |
Patients |
Healthy controls |
Statistics |
|
BDI-II |
23.188 (9.11) |
1.86 (2.20) |
U=.000; p<.001 |
|
|
HAMD17 |
17.28 (6.16) |
2.00 (1.95) |
U=2.500; p<.001 |
|
|
MQ |
15.06 (2.51) |
3.19 (3.16) |
U=5.500; p<.001 |
|
|
PSS |
32.44 (7.10) |
15.10 (4.23) |
U=3.500; p<.001 |
|
|
COR-E |
COR-Eloss |
1.19 (.57) |
.19 (.31) |
U=35.000; p<.001 |
|
COR-Eloss? |
1.28 (.66) |
.31 (.34) |
U=42.500; p<.001 |
|
|
COR-Egain |
.54 (.55) |
.73 (.70) |
U=304.500; p=.34 |
|
|
PNI |
PNItotal |
3.10 (.83) |
2.32 (.55) |
U=148.000; p<.001 |
|
PNIgn |
3.04 (.90) |
2.59 (.66) |
U=270.000; p=.07 |
|
|
PNIvn |
3.18 (.82) |
2.13 (.55) |
U=107.500; p<.001 |
|
|
P-values represent two-sided tests. |
||||
Table 2: Means and standard deviations of psychometric variables of patients and healthy controls.
4.2. Association between Narcissism and Disorder-specific Variables
Within healthy controls, a trend towards a significant positive correlation between grandiose narcissism (PNIgn) and resource gains (COR-Egain) was found (p = .07; Table 3). Therefore, more narcissistic grandiose, healthy participants reported higher resource gains. Additionally, healthy controls revealed a significant positive correlation between vulnerable narcissism (PNIvn) and the extent of actual resource loss (COR-Eloss: p = .022; Figure 1) as well as a trend towards a significant positive correlation between vulnerable narcissism (PNIvn) and vital exhaustion (MQ) (both p = .06; Figure 2). Therefore, healthy participants with higher vulnerable narcissism reported a larger extent of actual resource loss in the past six months and greater vital exhaustion. No other association attained statistical significance in the group of healthy controls (Table 3).
The analyses regarding the inpatients, on the other hand, revealed a significant positive correlation between vulnerable narcissism and depression (BDI-II: p < .001), the extent of actual resource loss (COR-Eloss: p = .022; Figure 1) and threatened loss (COR-Eloss?: p = .015) in the last 6 months prior to treatment, as well as perceived stress (PSS: p = .002; Table 3). Similar to the healthy controls, a trend towards a significant positive correlation between vulnerable narcissism (PNIvn) and vital exhaustion (MQ) was found in the patients (p = .06; Figure 2). Patients who had higher values in narcissistic vulnerability were also more depressed, lost more resources, were under the threat to lose further ones, and were more vitally exhausted. Differently, within patients, grandiose narcissism (PNIgn) correlated positively with perceived stress (p = .005), depression (BDI-II: p = .08) and the extent of threatened loss (p = .05), with the latter two reaching marginal significance. Therefore, within patients, also grandiose narcissism was positively associated with depression, resource loss and perceived stress, but to a lesser extent than vulnerable narcissism.
|
COR-E |
|||||||||
|
Groups |
PNI |
BDI-II |
HAMD17 |
MQ |
COR-Eloss |
COR-Eloss? |
COR-Egain |
PSS |
|
|
Healthy controls |
PNItotal |
rS=.19 |
rS=.28 |
rS=.32 |
rS=.43 t |
r=-.03 |
rS=.32 |
rS=-.03 |
|
|
PNIgn |
rS=.11 |
rS=-.12 |
rS=.32 |
rS=.36 |
r=.07 |
rS=.41 t |
rS=-.09 |
||
|
PNIvn |
rS=.29 |
rS=.32 |
rS=.42t |
rS=.51* |
r=.12 |
rS=.22 |
rS=.20 |
||
|
Patients |
PNItotal |
r=.44** |
r=.28 |
rS=.26 |
r=.24 |
rS=.43* |
rS=.25 |
r=.50** |
|
|
PNIgn |
r=.30 t |
r=.23 |
rS=.20 |
r=.12 |
rS=.33 t |
rS=.24 |
r=.46** |
||
|
PNIvn |
r=.57, p*** |
r=.32 t |
rS=.32 t |
r=.36* |
rS=.41* |
rS=.20 |
r=.49** |
||
|
P-values represent two-sided tests. P-value: ***: p≤.001; **: p≤.01; *: p≤.05; t: p≤.10 |
|||||||||
|
Legend: BDI-II: Beck Depression Inventory-II; COR-E: Conservation of Resources – Evaluation; COR-Eloss: COR-E, extent of actual loss; COR-Eloss?: COR-E, extent of threatened loss; COR-Egain: COR-E, extent of gain; HAMD17: Hamilton Depression Rating Scale; MQ: Maastricht Exhaustion Questionnaire; PNI: Pathological Narcissism Inventory; PNItotal: PNI, total score; PNIgn: PNI, grandiose narcissism; PNIvn: PNI, vulnerable narcissism; PSS: Perceived Stress Scale |
|||||||||
Table 3: Pearson and Spearman correlations between narcissism and disorder-specific variables.
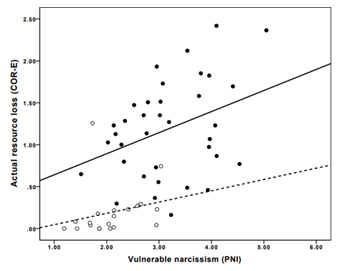
Figure 1: Association between vulnerable narcissism (PNIvn) and the extent of actual resource loss (COR-Eloss) in the last six months before treatment, in healthy controls (white circles, dotted line) and in inpatients (black circles, solid line).
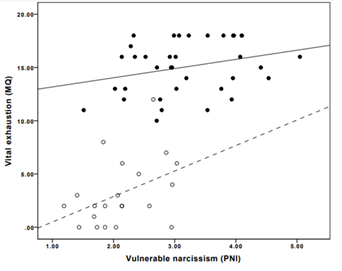
Figure 2: Association between vulnerable narcissism (PNIvn) and vital exhaustion (MQ), in healthy controls (white circles, dotted line) and in inpatients (black circles, solid line).
4.3. Treatment-related Changes in Disorder-specific Variables
The inpatient treatment led to a significant reduction in the BDI-II (p < .001), vital exhaustion (MQ: p < .001), the extent of actual resource loss (COR-Eloss: p < .001), and perceived stress (PSS: p < .001). Additionally, the increase in resource gains (COR-Egain) was significant (p = .001), while the alteration of threatened loss was not (table 4). Therefore, the treatment was effective in decreasing all disorder-specific variables.
|
Measuring time point |
|||||
|
Fragebogen |
(sub-)scales |
Beginning |
End |
Follow-up |
Statistics |
|
BDI-II (n=28) |
22.79 (7.63) |
9.93 (7.00) |
6.32 (5.96) |
F(2/54)=85.082, p<.001 |
|
|
HAMD17 (n=36) |
17.28 (6.16) |
6.67 (4.01) |
F(1/35)=158.240, p<.001 |
||
|
MQ (n=23) |
15.22 (2.73) |
5.48 (3.80) |
5.17 (5.18) |
X2(2)=37.95, p<.001 |
|
|
PSS (n=24) |
30.92 (6.83) |
20.75 (7.84) |
F(1/23)=29.727, p<.001 |
||
|
COR-E |
COR-Eloss (n=23) |
1.11 (.45) |
.52 (.43) |
F(1/22)=19.813, p<.001 |
|
|
COR-Eloss? (n=19) |
1.17 (.60) |
.84 (.69) |
X2(1)=2.58, p=.11 |
||
|
COR-Egain (n=27) |
.59 (.62) |
1.09 (.88) |
X2(1)=10.704, p=.001 |
||
|
P-values represent two-sided tests. |
|||||
Table 4: Treatment-related changes in disorder-specific variables.
4.4. Association between Narcissism and Treatment-related Changes in Disorder-specific Variables
A trend towards a positive correlation was found between grandiose narcissism (PNIgn) and the treatment-related alteration in extent of resource gain (ΔCOR-Egain) (p = .06; Figure 3). Patients with a higher grandiose narcissism, therefore, showed a stronger increase in resource gains. No other significant association was found with regard to PNIgn (all p = n.s.).
Differently, vulnerable narcissism (PNIvn) was negatively correlated with changes in depression severity
from beginning till the end of treatment (ΔpostBDI-II; p = .001; Table 5) as well as from beginning till follow-up (Δfollow-upBDI-II; p = .003; Figure 4). Similarly, the association between PNIvn and the alteration in perceived stress from beginning until follow-up (Δfollow-upPSS) was significantly negatively correlated (p = .048; Figure 5). More vulnerably narcissistic patients had therefore a stronger reduction in depressive severity and perceived stress as compared to less vulnerably narcissistic patients.
Table 5: Pearson correlations between narcissism and treatment-related alterations in disorder-specific symptoms.
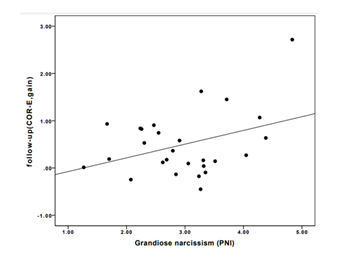
Figure 3: Association between grandiose narcissism and the alterations in the extent of resource gain (Δfollow-upCOR-Egain) from the beginning of the treatment until the follow-up in inpatients.
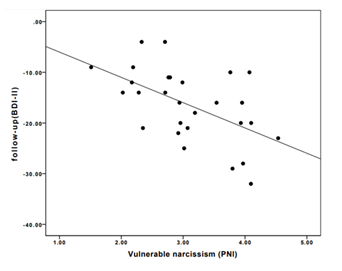
Figure 4: Association between vulnerable narcissism and the alterations in the extent of depression severity (Δfollow-upBDI-II) from the beginning of the treatment until the follow-up in inpatients.
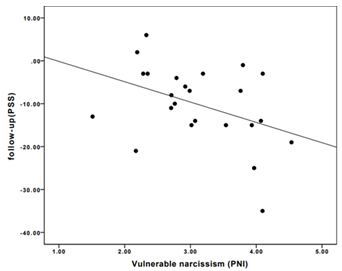
Figure 5: Association between vulnerable narcissism and the alterations in perceived stress (Δfollow-upPSS) from the beginning of the treatment until the follow-up in inpatients.
5. Discussion
5.1. Summary
Inpatients and healthy controls differed significantly regarding levels of depression (BDI-II, HAMD17), vital exhaustion (MQ), stress (PSS), actual as well as threatened loss of resources (COR-Eloss, COR-Eloss?), and vulnerable narcissism (PNIvn), with inpatients having higher values. Inpatients further had higher values compared to healthy controls regarding grandiose narcissism (PNIgn), with the difference reaching a trend towards significance. Regarding healthy controls, we found that PNIvn correlated positively with COR-Eloss. Furthermore, there was a trendwise positive significant association between PNIvn and MQ. PNIgn, on the other hand, was positively correlated with gain of resources (COR-Egain), which reached trendwise significance. In inpatients, PNIvn was significantly positively associates with levels of BDI-II, COR-Eloss, COR-Eloss?, and PSS. Positive associations at trend level were also reached for externally assessed depression (HAMD17) and MQ. On the other hand, PNIgn was significantly positively correlated with levels of PSS, and trendwise significantly correlated with BDI-II and COR-Eloss? levels. Regarding possible predictions, higher PNIvn at onset was associated with a stronger BDI-II decrease until the end / follow-up, and a stronger PSS decrease until follow-up. Differently, PNIgn was positively and trendwise significantly correlated to the increase in COR-Egain from the six months prior to treatment until the six months following treatment termination.
5.2. Embedding in the Literature
Since we studied patients with a stress-related depressive (or adjustment) disorder, levels of stress, actual and threatened loss of resources, vital exhaustion, and depression were expectably higher as compared to the sample of healthy controls. With regard to depression severity, inpatients’ mean HAMD17 and BDI-II scores indicate a moderated depression [55] and no depression in healthy controls.
Additionally, we found higher values of vulnerable narcissism in inpatients as compared to healthy controls as well as positive correlations in inpatients between PNIvn and BDI-II and HAMD17, with the latter reaching only trend significance. This is in line with most literature on the topic (e.g., [20; 53]. These associations were positive but did not reach significance in healthy controls, which might be explained by the small sample size. In inpatients, PNIvn was additionally positively and at least trendwise significantly related to MQ, COR-Eloss, COR-Eloss?, and PSS levels. The associations with MQ and COR-Eloss were also found in healthy controls. This is overall in line with most studies supporting vulnerable narcissism to be inversely related to depression (e.g., [20], as well as with stress (e.g., [50].
Since published findings on the relation of grandiose narcissism and depression are inconsistent, our results regarding the samples mean difference and correlational analysis were highly anticipated, in healthy controls as well as in inpatients. In healthy controls, PNIgn was unrelated to depression severity, vital exhaustion and perceived stress, but was trendwise significantly and positively related to a higher gain of resources. It is not surprising when looking at the subscales of the PNIgn (e.g., Entitlement Rage, Exploitativeness, and Self-Sacrificing Self-Enhancement) that individuals with higher grandiose narcissism levels can gain more resources than individuals with lower values. Another interpretation would be that grandiose narcissistic individuals might perceive an aggrandizement of the the self [26] and, therefore, maybe also of individual (gained) resources. When focusing on the inpatients, we found at least a trend towards significant associations between PNIgn levels and higher levels of PSS and COR-Eloss?, which is in line with the findings from Besser and Zeigler-Hill [50] in healthy subjects, as well as with depression severity, which is in line with the results presented by Morf et al. [20] in mainly students, or Marcinko et al. [53] in psychiatric outpatients. The reason for the inconsistency in these associations in literature might be due to different instruments being used among other to assess narcissism.
As expected, the treatment was highly effective in significantly reducing some core complaints in inpatients with a stress-related depressive or adjustment disorder, namely depression severity, vital exhaustion, and stress, including the actual loss of resource. The decrease in threatened resource loss did not reach significance. Additionally, the inpatient treatment revealed an increase in COR-Egain, which is not surprising since resource-fostering was part of the inpatient treatment, as recommended in the treatment of clinical burnout [44].
Regarding the prediction of treatment-related alterations, PNIvn was negatively correlated with the absolute changes in depression severity from beginning till the end of treatment as well as from beginning till follow-up. Similarly, the inverse association between PNIvn and the change in PSS levels from treatment initiation until follow-up was significant. More vulnerably narcissistic patients had therefore a stronger reduction in depressive severity and perceived stress as compared to less vulnerably narcissistic patients. Our findings related to pathological narcissism are in contrast to studies considering comorbid personality disorders (i.e. dichotomous variable), which indicate a worse therapy outcome in depressed patients with a comorbid personality disorder [40]. On the one hand, this might be explained by the more severe disorder, when a personality disorder is diagnosed in contrast to the continuous measure of narcissism used in the present study. On the other hand, this might be explained by the fact that we examined patients during an intensive inpatient treatment with various training opportunities to correct dysfunctional strategies (see ‘therapeutic implications’), while published research on depression and comorbid personality disorders often referred to outpatients mainly participating in real life, where dysfunctional strategies are not (enough) actively trained. Furthermore, our findings also differ from the results reported by Ellison et al. [43], who examined outpatients and missed to find an association between vulnerable and grandiose narcissism and depression alterations during early psychotherapy.
Interestingly, a trend towards a significantly positive correlation between PNIgn and a treatment-related increase in the extent of resource gain (ΔCOR-Egain) was found. Therefore, patients with higher initial grandiose narcissism show a stronger increase in resource gains. This finding might be explained by the relation between grandiose narcissism and ‘orientation to happiness’ [20], probably leading to a more resource-oriented focus in treatment.
5.3. Therapeutic Implications
The results of the study underline the importance of personality factors in the treatment of stress-associated depression, especially the importance of narcissistic homeostasis and self-worth regulation. Furthermore, the results throw a light on the double-sided aspects of vulnerable narcissism: as vulnerable personality factor on the one hand, and as an essential dimension of therapeutic change on the other hand.
The multimodal therapy approach - as a "structured psychosocial training field" with holding function as well as confronting aspects - enables to focus on negative emotions, control loss, anxieties, different dimensions of narcissistic vulnerability (low self-esteem, hiding the self, devaluing, social-avoidant behaviour) and to promote the development of more functional coping mechanisms by means of a combination of psychotherapy, creative therapies and body-oriented therapy interventions. The loss of resources may be overcome by experiencing resource gain, self-efficacy, and coping skills, as competencies when being confronted with stressful challenges. Starting to fill resource reservoirs can help to initiate a gain spiral [15] and to face challenges after leaving the inpatient clinic.
Thus, the inpatient treatment might be the fundament for the necessary continuation of the outpatient treatment after dismissal in order to assist their sustainable development. It might be concluded that clinical intervention targeting the avoidance of narcissistic injury and focusing on dysfunctional attitudes (e.g., perfectionism and dependency) in a resource-strengthening environment might help depressed patients develop self-esteem that is not overly dependant upon recognition from others.
5.4. Strengths and Limitations
One of the strength of the study is the comparison of inpatients with healthy controls, thus enabling the detection of clinically relevant traits of patients with stress-associated depressive disorders. Moreover, the use of the PNI allowed to examine both aspects of narcissism, grandiose and vulnerable narcissism, allowing for a more precise insight into its role in stress-related depression and its treatment. In addition, the use of the COR-E allowed to a broader understanding of the construct stress. The study is limited by the rather small sample size, but still allowing to statistically examine mean differences and associations. Additionally, subjects were not diagnosed by the use of a structured clinical interview. Furthermore, psychometric data was assessed approximately one week after treatment initiation, therefore, not representing clear pre-treatment baseline values, but maybe expressing already some early treatment effect. Another limitation concerns the effectivity of specific therapies in the multimodal inpatient-treatment approach, since the outcome is only attributable to the treatment as a whole.
6. Conclusion
Patients with stress-associated depression showed among others higher losses of resources and higher scores of vulnerable narcissism compared to healthy controls. Thereby, narcissism turned out to be a correlate of depression as well as a predictor of treatment-induced alterations. Losses of resources and dysfunctional coping strategies may jeopardise the self value of a person, thus increasing the vulnerability for the development of depressive disorders. Approaches offering treatment opportunities strengthening resources, preventing further resource losses, and reducing stress should be initiated at an early stage, in order to improve mental health. It is concluded that personality factors, especially vulnerable narcissism and its association with depressive symptoms, should be considered in clinical burnout research and therapy in the future.
7. Highlights
- Inpatients with a stress-related depression reveal higher levels of actual or threatened loss of resources as compared to healthy controls.
- Vulnerable narcissism positively correlates with actual loss of resources in the past six months, in inpatients as well as in healthy controls.
- Grandiose narcissism is positively associated with resource gains in the past six months in healthy controls, but missed significance in inpatients.
- Higher levels of vulnerable narcissism is related to a stronger treatment-related decrease in depression severity, while higher levels of grandiose narcissism is related to a stronger treatment-related increase in resource gain.
Acknowledgment
We would like to thank Stevan Hobfoll for providing us support regarding the analyses of the COR-E questionnaire and his valuable theoretical input and feedback to the manuscript. Similarly, we would like to thank Carolyn C. Morf for providing us with the PNI and giving us feedback on the manuscript. Furthermore, we would like to thank the team of the Clinica Holistica Engiadina (CHE) for the support during the time of data collection as well as all the patients and control subjects participating in the study. Our thanks goes also to the research team including interns at the University of Zurich. We would like to thank the CHE for funding the study and for allowing data collection in the CHE.
Conflict of Interest
MP works as head doctor and medical director at the Clinica Holistica Engiadina (CHE). HB is part of the Scientific Advisory Council Board of the CHE as well as a clinical supervisor at the CHE. RLM and MS were initially not associated with the CHE, but started working at the CHE only after the study examinations started. Nevertheless, the CHE did not have any influence on the selection of the analyses nor on the manuscript.
Author Contributions
HB and RL acquired the funding. RL and HB conceptualized the study. RL, PLG, and HB defined the methods. RL, MS and HB planned, and MS conducted the investigation. RL and MS concluded data curation. RL conducted the analysis. RL and HB wrote the original draft. RL, MS, MP, PLG and HB reviewed and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The Clinica Holistica Engiadina (CHE), Switzerland, funded this study, which was conducted at the CHE. The views expressed are solely those of the authors. They do not reflect the official policy or position of the CHE.
Ethics Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and informed consent was obtained from all subjects involved in the study. The study was approved by the Ethics Committee of the Canton of Zurich.
Data Availability Statement
Participants did not give consent to share their data, therefore, data is confidential and not available.
References
- Bretschneider J, Janitza S, Jacobi F, et al. Time trends in depression prevalence and health-related correlates: results from population-based surveys in Germany 1997-1999 vs. 2009-2012. BMC Psychiatry 18 (2018): 394.
- Kessler RC, Berglund P, Demler O, et al. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 6 (2005): 593-602.
- Vandeleur CL, Fassassi S, Castelao E, et al. Prevalence and correlates of DSM-5 major depressive and related disorders in the community. Psychiatry Res 250 (2017): 50-58.
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392 (2017): 1789-1858.
- GBD 2019 Diseases and Injuries Collaborators, 2020. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 (2019): 1204-1222.
- Greenberg PE, Fournier AA, Sisitsky T, et al. The Economic Burden of Adults With Major Depressive Disorder in the United States (2005 and 2010). J Clin Psychiatry 76 (2015): 155-162.
- Tomonaga Y, Haettenschwiler J, Hatzinger M, et al. The economic burden of depression in Switzerland. Pharmacodconomics 31 (2013): 237-250.
- Hotzheimer PE, Mayberg HS. Stuck in a rut: Rethinking depression and its treatment. Trends Neurosci 34 (2011): 1-9.
- Roy A, Campbell MK. A unifying framework for depression: Bridging the major biological and psychosocial theories through stress. Clin Invest Med 36 (2013): E170-E190.
- Willner P, Scheel-Kruger J, Belzung C. The neurobiology of depression and antidepressant action. Neurosci Biobehav Rev 37 (2013): 2331-2371.
- Ehrlich M, Harville E, Xiong X, et al. Loss of resources and hurricane experience as predictors of postpartum depression among women in southern louisiana. J Women’s Health 19 (2010): 877-884.
- Hobfoll SE, Tracy M, Galea S. The Impact of Resource Loss and Traumatic Growth on Probable PTSD and Depression Following Terrorist Attacks. J Trauma Stress 19 (2006): 867-878.
- Sattler DN, Glower de Alvaro AM, Blandon de Castro M, et al. El Salvador earthquakes: Relationship among acute stress disorder symptoms, depression, traumatic event exposure, and resource loss. J Trauma Stress 19 (2006): 879-893.
- Goldfarb R, Ben-Zur H. Resource Loss and Gain Following Military Reserve Duty in Israel: An assessment of conservation of resources (COR) theory. Int J Stress Manag 24 (2017): 135-155.
- Morgenroth S, Buchenwald P, Braasch M. Stress prevention among German teachers. In M. Israelashvili & J. L. Romano. The cambridge handbook of international preventive sciences. Cambridge University Press, Cambridge (2016).
- Pincus AL, Ansell EB, Pimentel CA, et al. Initial Construction and Validation of the Pathological Narcissism Inventory. Psychol Assess 21 (2009): 365-379.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 24 (1983): 385-396.
- Kajonius PJ, Björkman T. Dark malevolent traits and everyday perceived stress. Curr Psychol 39 (2020): 2351-2356.
- Gentile B, Miller JD, Hoffman BJ, et al. A test of two brief measures of grandiose narcissism: The narcissistic personality inventory-13 and the narcissistic personality Inventory-16. Psychol Assess 25 (2013): 1120-1136.
- Morf CC, Schurch E, Kufner A, et al. Expanding the nomological net of the Pathological Narcissism Inventory: German validation and extension in a clinical inpatient sample. Assessment 24 (2017): 419-443.
- Raskin RN, Terry H. A principal component analysis of the Narcissistic Personality Inventory and further evidence of its construct-validity. J Person Soc Psychol 54 (1988): 890-902.
- Papageorgiou KA, Denovan A, Dagnall N. The positive effect of narcissism on depressive symptoms through mental toughness: Narcissism may be a dark trait but it does help with seeing the world less grey. Eur Psychiatry 55 (2019): 74-79.
- Sherman E, Miller J, Few L, et al. Development of a short form of the five-factor narcissism inventory: the FFNI-SF. Psychol Assess 27 (2015): 1110-1116.
- Tritt SM, Ryder AG, Ring AJ, et al. Pathological narcissism and the depressive temperament. J Affect Disord 122 (2010): 280-284.
- Daig I, Burkert S, Fischer HF, et al. Development and factorial validation of a short version of the Narcissism Inventory (NI-20). Psychopathology 43 (2010): 150-158.
- Schwarzkopf K, Strauss D, Porschke H, et al. Empirical evidence for a relationship between narcissistic personality traits and job burnout. Burnout Res 3 (2016): 25-33.
- Jaksic N, Marcinko D, Skocic Hanzek M, et al. Experience of shame mediates the relationship between pathological narcissism and suicidal ideation in psychiatric outpatients. J Clin Psychol 73 (2017): 1670-1681.
- Lovibond SH, Lovibond PF. Manual for the Depression, Anxiety and Stress Scales, second ed. Psychological Foundation, Sydney (1995).
- Kraus DR, Seligman DA, Jordan JR. Validation of a behavioral health treatment outcome and assessment tool designed for naturalistic settings: The Treatment Outcome Package. J Clin Psychol 61 (2005): 285-314.
- Nimeus A, Hjalmarsson SF, Sunnqvist C, et al. Evaluation of a modified interview version and of a self-rating version of the Suicide Assessment Scale. Eur Psychiatry 21 (2006): 471-477.
- Hendin HM, Cheek JM. Assessing hypersensitive narcissism: a reexamination of Murray's Narcism Scale. J Res Personal 31 (1997): 588-599.
- Erkoreka L, Navarro B. Vulnerable narcissism is associated with severity of depressive symptoms in dysthymic patients. Psychiatry Res 257 (2017): 265-269.
- Kealy D, Tsai M, Ogrudniczuk JS. Pathological Narcissism and somatic symptoms among men and women attending an outpatient mental health clinic. Int J Psychiatry Clin Pract 20 (2016): 175-178.
- Kealy D, Laverdiére O, Pincus AL. Pathological narcissism and symptoms of major depressive disorder among psychiatric outpatients. The mediating role of impaired emotional processing. J Nervous Mental Dis 208 (2020): 161-164.
- Kroenke K, Spither RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 16 (2001): 606-613.
- De Page L, Merckelbach H. Associations between supernormality (‘faking good’), narcissism and depression: An exploratory study in a clinical sample. Clin Psychol Psychother 28 (2020): 182-188.
- Raskin RN, Hall CS. A narcissistic personality inventory. Psychol Rep 45 (1979): 590-590,
- Watson PJ, Sawrie SM, Greene RL, et al. Narcissism and depression: MMPI-2 evidence for the continuum hypothesis in clinical samples. J Pers Assess 79 (2002): 85-109.
- Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: meta-analysis of published studies. Br J Psychiatry 188 (2006): 13-20.
- Candrian M, Schwartz F, Farabaugh A, et al. Personality disorders and perceived stress in major depressive disorder. Psychiatry Res 160 (2008): 184-191.
- Fava M, Farabaugh AH, Sickinger AH, et al. Personality disorders and depression. Psychol Med 32 (2002): 1049-1057.
- Cyranowski JM, Frank E, Winter E, et al. Personality pathology and outcome in recurrently depressed women over 2 years of maintenance interpersonal psychotherapy. Psychol Med 34 (2004): 659-669.
- Ellison WD, Levy KN, Cain NM, et al. The Impact of Pathological Narcissism on Psychotherapy Utilization, Initial Symptom Severity, and Early-Treatment Symptom Change: A Naturalistic Investigation. J Pers Assess 95 (2013): 291-300.
- Hochstrasser B, Bru?hlmann T, Cattapan K, et al. Burnout-Behandlung Teil 2: Praktische Empfehlungen. Swiss Medical Forum 16 (2016): 561-566.
- Schnorpfeil P, Noll A, Wirtz P, et al. Assessment of exhaustion and related risk factors in employees in the manufacturing industry - a cross-sectional study. Int Arch Occup Environ Health 75 (2002): 535-540.
- Preckel D, von Känel R, Kudielka BM, et al. Overcommitment to work is associated with vital exhaustion. Int. Arch. Occup. Environ. Health 78 (2005): 117-122.
- Hautzinger M, Keller F, Kühner C. Beck-Depressions-Inventar, BDI-II, Manual, second ed. Pearson Assessment, Frankfurt (2009).
- Wintjen L, Petermann F. Beck-Depressions-Inventar Revision (BDI-II). Zeitschrift Psychiatr Psychol Psychother 58 (2010): 243-245.
- Internationale Skalen für Psychiatrie. Beltz Test, Weinheim (1977).
- Besser A, Zeigler-Hill V. Pathological forms of narcissism and perceived stress during the transition to the university: the mediating role of humor styles. Int J Stress Manag 18 (2011): 197-221.
- Akhtar S. New clinical realms: Pushing the envelope of theory and technique. Aronson, London (2003).
- Ashby HU, Lee RR, Duke EH. A narcissistic personality disorder MMPI scale. Paper presented at the 87th annual meeting of the American Psychological Association, New York (1979).
- Marcinko D, Jaksic N, Ivezic E, et al. Pathological narcissism and depressive symptoms in psychiatric outpatients: mediating role dysfunctional attitudes. J Clin Psychol 70 (2014): 341-352.
- Ungerath S. Towards a refined understanding of resource gain spirals - A theoretical discussion of existing research, and novel empirical evidence from two longitudinal intervention studies, Dissertation. Bergische Universita?t Wuppertal, Wuppertal (2012).
- Zimmerman M, Martinez JH, Young D., Chelminski I. Severity classification on the Hamilton depression rating scale. Journal of Affective Disorders 150 (2013): 384-388.
- Hobfoll SE. Conservation of Resources – A new attempt at conzeptualizing stress. American Psychologist 44 (1989): 513-524.
