The Impact of the COVID-19 Pandemic on Utilization of Healthcare Services among Individuals with Schizophrenia in the United States
Article Information
Joshua N. Liberman1, Jacqueline Pesa2, Mary Pat Petrillo2
1Health Analytics, LLC, Columbia,
2Janssen Scientific Affairs, Titusville
*Corresponding Author: Joshua Liberman, Health Analytics, LLC, Columbia
Received: 21 June 2023; Accepted: 03 July 2023; Published: 26 September 2023
Citation:
Joshua N. Liberman, Jacqueline Pesa, Mary Pat Petrillo. The Impact of the COVID-19 Pandemic on Utilization of Healthcare Services among Individuals with Schizophrenia in the United States. Journal of Psychiatry and Psychiatric Disorders. 7 (2023): 156-166.
Share at FacebookAbstract
Background: Individuals with schizophrenia were at high risk for negative outcomes during the COVID-19 pandemic.
Objective: Determine if the COVID-19 pandemic disrupted healthcare utilization among individuals with schizophrenia.
Methods: Using insurance claims licensed from Clarivate, a retrospective cohort study was conducted among 493,796 adults with schizophrenia between 1/1/2019 and 9/30/2020. Healthcare utilization was measured six months prior to (baseline) and following (follow up) 3/1/2020 and included primary care, psychiatry, psychotherapy, Community Mental Health Centers (CMHC), Emergency Department (ED), partial-day and inpatient hospitalizations, and medication use. Changes in long-acting injectable (LAI) antipsychotic use were presented by state-level policies authorizing pharmacists to administer drugs.
Results: During follow up, primary care utilization increased 11%, inperson visits declined 32.5% and telehealth-delivered visits increased 496%. Psychiatry and psychotherapy visits increased 36.6% and 17.2%, with a 53% and 40.4% decline in in-person visits offset by 1174% and 4836% increase in telehealth-delivered services. Partial-day hospitalizations declined by 37.8% and CMHC visits declined 15.1%. Oral antipsychotic medication days’ supply increased by 2.8%, driven by a sustained increase in 90-day supply of prescription fills. LAI antipsychotic use declined 1.3% and change in LAI utilization varied among states with different policies regarding pharmacist authorization to administer LAI antipsychotic medications.
Conclusions: Following pandemic onset, partial-day hospitalizations and CMHC visits declined substantially but primary care and other outpatient mental healthcare services increased. Sustained use of telehealth suggests the acceptability of this modality to both patients and providers. LAI utilization varied among states with different policies that authorize pharmacist administration.
Keywords
COVID-19, Schizophrenia, Healthcare Resource Utilization, LAI
COVID-19 articles; Schizophrenia articles; Healthcare Resource Utilization articles; LAI articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Schizophrenia articles Schizophrenia Research articles Schizophrenia review articles Schizophrenia PubMed articles Schizophrenia PubMed Central articles Schizophrenia 2023 articles Schizophrenia 2024 articles Schizophrenia Scopus articles Schizophrenia impact factor journals Schizophrenia Scopus journals Schizophrenia PubMed journals Schizophrenia medical journals Schizophrenia free journals Schizophrenia best journals Schizophrenia top journals Schizophrenia free medical journals Schizophrenia famous journals Schizophrenia Google Scholar indexed journals Healthcare Resource Utilization articles Healthcare Resource Utilization Research articles Healthcare Resource Utilization review articles Healthcare Resource Utilization PubMed articles Healthcare Resource Utilization PubMed Central articles Healthcare Resource Utilization 2023 articles Healthcare Resource Utilization 2024 articles Healthcare Resource Utilization Scopus articles Healthcare Resource Utilization impact factor journals Healthcare Resource Utilization Scopus journals Healthcare Resource Utilization PubMed journals Healthcare Resource Utilization medical journals Healthcare Resource Utilization free journals Healthcare Resource Utilization best journals Healthcare Resource Utilization top journals Healthcare Resource Utilization free medical journals Healthcare Resource Utilization famous journals Healthcare Resource Utilization Google Scholar indexed journals stress articles stress Research articles stress review articles stress PubMed articles stress PubMed Central articles stress 2023 articles stress 2024 articles stress Scopus articles stress impact factor journals stress Scopus journals stress PubMed journals stress medical journals stress free journals stress best journals stress top journals stress free medical journals stress famous journals stress Google Scholar indexed journals LAI articles LAI Research articles LAI review articles LAI PubMed articles LAI PubMed Central articles LAI 2023 articles LAI 2024 articles LAI Scopus articles LAI impact factor journals LAI Scopus journals LAI PubMed journals LAI medical journals LAI free journals LAI best journals LAI top journals LAI free medical journals LAI famous journals LAI Google Scholar indexed journals disorders articles disorders Research articles disorders review articles disorders PubMed articles disorders PubMed Central articles disorders 2023 articles disorders 2024 articles disorders Scopus articles disorders impact factor journals disorders Scopus journals disorders PubMed journals disorders medical journals disorders free journals disorders best journals disorders top journals disorders free medical journals disorders famous journals disorders Google Scholar indexed journals Obsessive compulsive disorder articles Obsessive compulsive disorder Research articles Obsessive compulsive disorder review articles Obsessive compulsive disorder PubMed articles Obsessive compulsive disorder PubMed Central articles Obsessive compulsive disorder 2023 articles Obsessive compulsive disorder 2024 articles Obsessive compulsive disorder Scopus articles Obsessive compulsive disorder impact factor journals Obsessive compulsive disorder Scopus journals Obsessive compulsive disorder PubMed journals Obsessive compulsive disorder medical journals Obsessive compulsive disorder free journals Obsessive compulsive disorder best journals Obsessive compulsive disorder top journals Obsessive compulsive disorder free medical journals Obsessive compulsive disorder famous journals Obsessive compulsive disorder Google Scholar indexed journals Sleep articles Sleep Research articles Sleep review articles Sleep PubMed articles Sleep PubMed Central articles Sleep 2023 articles Sleep 2024 articles Sleep Scopus articles Sleep impact factor journals Sleep Scopus journals Sleep PubMed journals Sleep medical journals Sleep free journals Sleep best journals Sleep top journals Sleep free medical journals Sleep famous journals Sleep Google Scholar indexed journals Bipolar depression articles Bipolar depression Research articles Bipolar depression review articles Bipolar depression PubMed articles Bipolar depression PubMed Central articles Bipolar depression 2023 articles Bipolar depression 2024 articles Bipolar depression Scopus articles Bipolar depression impact factor journals Bipolar depression Scopus journals Bipolar depression PubMed journals Bipolar depression medical journals Bipolar depression free journals Bipolar depression best journals Bipolar depression top journals Bipolar depression free medical journals Bipolar depression famous journals Bipolar depression Google Scholar indexed journals dysthymia articles dysthymia Research articles dysthymia review articles dysthymia PubMed articles dysthymia PubMed Central articles dysthymia 2023 articles dysthymia 2024 articles dysthymia Scopus articles dysthymia impact factor journals dysthymia Scopus journals dysthymia PubMed journals dysthymia medical journals dysthymia free journals dysthymia best journals dysthymia top journals dysthymia free medical journals dysthymia famous journals dysthymia Google Scholar indexed journals
Article Details
1. Introduction
On January 31, 2020, the World Health Organization declared SARS-CoV-2 infections a global health emergency [1] and the U.S. Secretary of Health and Human Services declared a national public health emergency [2]. On March 11, the World Health Organization declared COVID-19 a pandemic [3]. On March 13, the U.S. government declared a national emergency [4]. Following these declarations, and in response to rising COVID-19 infection rates [5], many jurisdictions implemented guidelines and policies to limit interactions between people: physical distancing, limits to the number of individuals who could legally gather, closure of indoor entertainment and recreational venues, among numerous others. Simultaneously, healthcare providers were implementing significant changes to the practice of medicine: canceling or deferring elective and non-urgent in-person appointments and procedures, [6] implementing virtual (telehealth) visit technology, (APA) reducing office hours and patient volume, [7] adopting more aggressive infection prevention and control procedures (CDC) and physical distancing guidelines, [8] and re-allocating hospital beds for COVID-19 patients [9]. The potential for COVID-19 infection and the associated changes in health care delivery practices raised concerns among mental health care providers [10,11]. Individuals with pre-existing serious mental illness, and in particular, those with schizophrenia, were deemed at particularly high risk for negative outcomes following COVID-19 infection [12, 13], including hospitalization [14] and in-hospital mortality [15]. These concerns were raised, in part, because individuals with schizophrenia have high rates of psychiatric comorbidity, [16] and have a therapeutic regimen that requires routine engagement with healthcare providers, including psychiatry, primary care, pharmacy, and psychotherapy, to achieve optimal outcomes. Previous studies have explored the pandemic’s impact on the mental health of individuals with schizophrenia [17], reported changes in health care resource utilization among individuals with pre-existing mental health conditions overall [18, 19, 20] and for specific health care services such as inpatient hospitalizations [21,22] outpatient mental health services [23], telehealth use [18,19], or antipsychotic medication use [24]. However, to our knowledge no studies have evaluated comprehensive changes in outpatient, inpatient, and prescription drug utilization among a nationally representative sample of individuals with schizophrenia or schizoaffective disorder in the United States. The objective of the current study was to evaluate those changes in the early months of the pandemic.
2. Materials and Methods
This study was a retrospective cohort study among individuals with schizophrenia comparing healthcare resource utilization in the six months prior to (September 1, 2019, through February 28, 2020) and six months following (March 1, 2020, through August 31, 2020) the COVID-19 pandemic onset in the United States.
2.1 Data Sources
Individuals were identified and selected from the medical and pharmacy claims data licensed from Clarivate (www.clarivate.com/products/real-world-data/) and linked, at the county level to the Area Health Resources Files (AHRF) available from the Department of Health and Human Services (www.data.hrsa.gov/topics/health-workforce/ahrf). Participant-specific age, sex, state of residence, 3-digit ZIP, insurance provider (Medicaid, Medicare, commercial, or VA/other), and healthcare resource utilization measures were identified and calculated from claims data. Other demographic characteristics were defined by county of residence and assigned as a continuous variable based on the county’s mean value from AHRF data. Individuals were assigned to a county based on a combination of their 3-digit ZIP code, linked to the 5-digit ZIP code associated with their provider, assigned hierarchically beginning with the primary care provider, then the mental health care provider or clinic. State policy regarding the pharmacist authorization for administering LAI formulations of antipsychotic medications was identified from the National Alliance of State Pharmacy Associations website (NASPA). Pharmacist authorization was categorized as: not allowed to administer LAI antipsychotics, allowed to administer LAI antipsychotics, and allowed to administer LAI antipsychotics under a physician’s supervision via a collaborative practice agreement. A collaborative practice agreement is a formal agreement between a prescriber and pharmacist that authorizes the pharmacist to deliver a specific set of patient care services, which can include authorization to administer an LAI antipsychotic.
2.2 Identification and Selection of Study Participants
Eligible individuals met each of the following criteria: diagnosis of schizophrenia or schizoaffective disorder (ICD-10-CM: F20.x, F25.x) defined by two or more outpatient claims (or one inpatient claim) between January 1, 2019 and June 30, 2020, 18 years of age or older as of January 1, 2019, a resident of the 50 United States or District of Columbia, and continuous use of healthcare services as measured by at least one medical or pharmacy claim between each of January 1, 2019 and June 30, 2019; January 1 and June 30, 2020; and July 1 to September 30, 2020.
2.3 Data Management and Analysis
The index date for the pandemic in the United States was defined as March 1, 2020. Outcome measures for all-cause and psychiatric-specific healthcare utilization included office visits for primary care, ED visits, and inpatient hospitalizations. Outcome measures for schizophrenia-specific (defined by an ICD-10 code for schizophrenia or schizoaffective disorder in the primary position) healthcare resource utilization included office visits for psychiatry, psychotherapy, community mental health centers (CMHC), partial-day hospitalizations, and inpatient hospitalizations. Visits were measured per thousand patients per month (PkPPM) and prescription use measured per thousand patients per week (PkPPW). Office visits and psychotherapy sessions categorized by delivery method: in-person, telehealth, and total. Prescription medications were categorized by therapeutic class (antipsychotics, antidepressants, mood stabilizers, and anxiolytics), and characterized by route of administration (oral vs. injectable), by days’ supply per prescription (<90 days’ supply vs. 90+ days’ supply), and by claims. Psychotherapy visits were defined by a claim for CPT 90832, 90834, 90837, 90839, 90840, 90845, 90847, 90849, 90853, or 96152. Psychiatric and medical comorbidities were identified from claims between April 1, 2019, and March 30, 2020. Psychiatric comorbidities included anxiety (F41.x), adjustment disorders (F43.2x), bipolar depression (F30.x, F31.x), obsessive-compulsive disorder (F42.x), PTSD (F43.1x), sleep-wake disorders (G47.x), alcohol and substance use disorders (F10.x – F19.x), F32.x, F33.x, F34.1), and depressive disorders (F32.x, F33.x). Medical comorbidities were measured by the Charlson Comorbidity Index [25]. COVID-19 infection was defined by ICD-10-CM B97.29 (from January 1 – March 31, 2020) and by U07.1 (from April 1 through September 30, 2020).
2.4 Analysis
Rates were calculated for each outcome variable, by month for outpatient and inpatient services and by week for prescription medication fills. March through August 2020 defined the pandemic period, while September 2019 thru February 2020 defined the pre-onset period, allowing a comparison between the six months prior to and following pandemic onset. Post-onset percent changes in utilization were calculated for the entire six-month period and by month, compared to the six-month average during the pre-onset period. Monthly average changes were tested for statistical significance using t-tests with standard error calculation methods depending on equal/unequal variance tests. Results are based on independent sample testing rather than paired testing, as the former is more conservative given that utilization pre- and post-onset are correlated within an individual. Post-pandemic onset changes in prescription drug utilization were also examined within regression models. The period between September 2019 and August 2020 was split into four three-month calendar quarters, labeled as Fall (September-November 2019), Winter (December 2019 – February 2020), Spring (March-May 2020), and Summer (June-August 2020), and with the COVID-19 pandemic represented by two consecutive periods: Spring 2020 and Summer 2020. These temporal indicators entered the model as a categorical variable to compare the utilization during the pre- and post-onset periods. Dependent variables included each outcome measure referenced above. The models controlled for the following time-invariant covariates: age (continuous, in years), sex, insurance type, indicator for each psychiatric comorbidity, and county-level median household income, county-level race-ethnicity characteristics (percentages of Black/African American, Hispanic, Asian/other), and county-level indicators distinguishing between metro, urban, or rural areas. State policy regarding the pharmacist authorization for administering LAI formulations of antipsychotic medications is included in the pharmacy utilization models. To determine if the pandemic’s association with changes in utilization differed by race/ethnicity or by state-level policy regarding pharmacist authorization to administer LAI antipsychotics, models also included interaction terms between these variables and calendar quarter. All analyses were performed using SAS v9 (Cary, NC). The research protocol was approved by the Advarra Institutional Review Board.
3. Results
A total of 493,796 (69.5%) individuals met study eligibility criteria (Table 1), with most qualifying with unspecified schizophrenia (29.1%), followed by bipolar type schizoaffective disorder (25.5%), unspecified schizoaffective disorder (14.5%), paranoid schizophrenia (13.6%), and depressive type schizoaffective disorder (10.8%). The population was 55.2% male, with an average age of 50.1 years, and 68.2% of the population was insured by Medicaid. The sample included residents of all 50 U.S. states and the District of Columbia, with most from New York (10.7%), followed by California (8.8%), Florida (6.9%), Ohio (6.6%), and Texas (5.8%). The most common mental health comorbidities were anxiety disorder (31.5%), followed by depressive disorders (29.7%), bipolar depression (24.5%), and sleep-wake disorders (16.7%). The Charlson Comorbidity Index score was 1.27 (SD: 1.88).
Table 1: Select Demographic Characteristics
|
Total Population N=493,796 |
||
|
n= |
% |
|
|
Gender* |
||
|
Female |
2,21,217 |
44.80% |
|
Male |
2,72,369 |
55.20% |
|
Age |
||
|
18-30 |
66,513 |
13.50% |
|
31-49 |
1,58,898 |
32.20% |
|
50-64 |
1,76,889 |
35.80% |
|
Over 65 |
91,496 |
18.50% |
|
Insurance |
||
|
Commercial |
66,630 |
13.50% |
|
Medicaid |
3,36,542 |
68.20% |
|
Medicare |
89,676 |
18.20% |
|
VA/ Other |
857 |
0.20% |
|
Urbanicity* |
||
|
Metro |
4,36,295 |
88.40% |
|
Urban |
54,150 |
11.00% |
|
Rural |
3,198 |
0.60% |
|
Charlson Comorbidity Index |
||
|
0 |
2,38,540 |
48.30% |
|
01-Feb |
1,70,127 |
34.50% |
|
03-Apr |
50,395 |
10.20% |
|
5+ |
34,734 |
7.00% |
|
State of residence, by pharmacist authorization** |
||
|
Not authorized |
75,975 |
15.40% |
|
Authorized with CPA |
1,04,827 |
21.20% |
|
Authorized |
3,12,994 |
63.40% |
|
Schizophrenia-associated diagnosis |
||
|
Schizophrenia, unspecified |
1,43,543 |
29.10% |
|
Schizoaffective disorder, bipolar type |
1,26,066 |
25.50% |
|
Schizoaffective disorder, unspecified |
71,745 |
14.50% |
|
Paranoid schizophrenia |
67,077 |
13.60% |
|
Schizoaffective disorder, depressive type |
53,412 |
10.80% |
|
Schizophrenia, other |
27,044 |
5.50% |
|
Schizoaffective disorder, other |
4,909 |
1.00% |
|
Behavioral, Psychiatric Comorbidities |
||
|
Depressive disorders: MDD, dysthymia |
1,46,594 |
29.70% |
|
Bipolar depression |
1,21,164 |
24.50% |
|
Sleep-wake disorders |
82,560 |
16.70% |
|
Alcohol use disorder |
59,207 |
12.00% |
|
Post-traumatic stress disorder |
45,473 |
9.20% |
|
Adjustment disorders |
14,561 |
2.90% |
|
Obsessive compulsive disorder |
10,817 |
2.20% |
|
* Missing values: patient gender - n= 210; urbanicity n=153 |
||
|
** State-specific authorization to administer LAI antipsychotics |
||
3.1 Outpatient Services
In the pandemic’s first six months in-person primary care office visit rate declined by 32.5% (declining by 56.9% in April 2020), remaining below pre-pandemic levels through August 2020 (Table 2, Figure 1). During this period, telehealth-delivered primary care visits increased dramatically, peaking at 62.4% of all primary care visits in May 2020, remaining elevated through August (34.0%). The increase in primary care telehealth visits more than offset the reduction in in-person visits. The total primary care visit rate recovered to pre-pandemic levels by May 2020 and stayed elevated through September.
Table 2: Healthcare resource utilization in the six-month pre-pandemic period and six-month period following pandemic onset (March 1, 2020) in the United States.
|
Pre-Pandemic |
Pandemic |
% Change |
p-value |
||
|
(9/1/19 – 2/29/20) |
(3/1/20 – 8/31/20) |
||||
|
Utilization Rate |
Utilization Rate |
||||
|
Outpatient, non-acute services (PkPPM) |
|||||
|
Primary Care |
|||||
|
Telehealth |
9.87 |
58.83 |
496.00% |
<0.001 |
|
|
In-person |
109.91 |
74.14 |
-32.50% |
<0.001 |
|
|
Total |
119.78 |
132.97 |
11.00% |
<0.001 |
|
|
Psychiatry |
|||||
|
Telehealth |
4.2 |
53.7 |
1172.50% |
<0.001 |
|
|
In-person |
53.6 |
25.2 |
-53.00% |
<0.001 |
|
|
Total visits |
57.8 |
78.9 |
36.50% |
<0.001 |
|
|
Psychotherapy |
|||||
|
Telehealth |
1 |
48 |
4848.50% |
<0.001 |
|
|
In-person |
81.4 |
48.5 |
-40.40% |
<0.001 |
|
|
Total visits |
82.4 |
96.6 |
17.20% |
<0.001 |
|
|
CMHC |
|||||
|
Telehealth |
2.5 |
11.9 |
367.70% |
<0.001 |
|
|
In-person |
188.1 |
147.5 |
-21.60% |
<0.001 |
|
|
Acute care services (PkPPM) |
|||||
|
ED |
93.3 |
85.6 |
-8.30% |
<0.001 |
|
|
Hospitalization |
28.9 |
28.7 |
-1.00% |
<0.05 |
|
|
Partial-day hospitalizations |
7.6 |
4.7 |
-37.80% |
<0.001 |
|
|
Medication (PkPPW) |
|||||
|
Antipsychotics |
|||||
|
<90-day supply prescriptions |
88.91 |
88.81 |
-0.10% |
NS |
|
|
90+ day supply prescriptions |
2.98 |
3.86 |
29.50% |
<0.001 |
|
|
Total days’ supply, oral |
2657 |
2731 |
2.80% |
<0.001 |
|
|
LAI antipsychotic claims |
16.6 |
16.4 |
-1.30% |
<0.001 |
|
|
Antidepressants |
|||||
|
<90-day supply prescriptions |
52.8 |
52.5 |
-0.40% |
NS |
|
|
90+ day supply prescriptions |
1.69 |
2.08 |
23.10% |
<0.001 |
|
|
Total days |
1747 |
1812 |
3.70% |
<0.001 |
|
|
Mood stabilizers |
|||||
|
<90-day supply prescriptions |
39.3 |
39.7 |
0.90% |
<0.001 |
|
|
90+ day supply prescriptions |
1.69 |
2.08 |
23.10% |
<0.001 |
|
|
Anxiolytics |
|||||
|
<90-day supply prescriptions |
19.1 |
19.3 |
0.50% |
<0.05 |
|
|
90+ day supply prescriptions |
0.39 |
0.48 |
23.10% |
<0.001 |
|
|
Total days |
550 |
571 |
3.80% |
<0.001 |
|
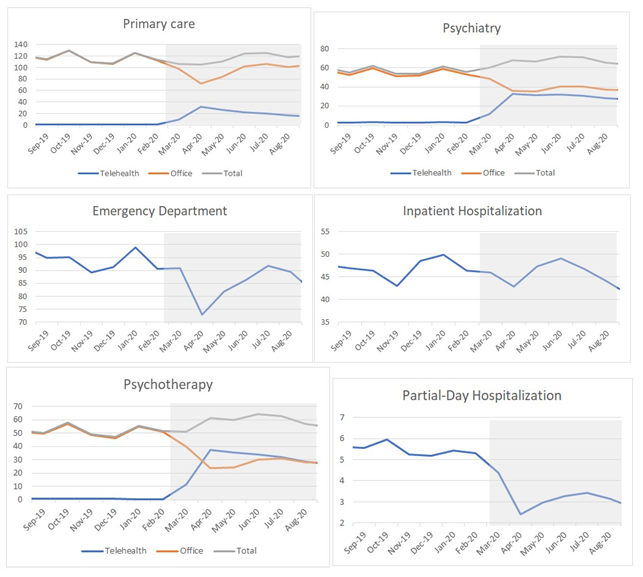
Figure 1: Utilization of select healthcare services (visits PkPPM) between September 1, 2019, and August 31, 2020, among 493,796 individuals with schizophrenia
The post-pandemic onset psychiatry visit rate increased rapidly, up 9.7% in March, reaching a peak increase of 48.1% in June 2020, while remaining elevated through August (up 31.7%). Telepsychiatry was uncommon prior to March 2020, representing approximately 7% of all visits; however, the percent of psychiatry visits delivered via telehealth increased to more than 70% between April and August 2020. Psychotherapy sessions increased by 17.2% overall. Prior to the pandemic, less than 2% of psychotherapy sessions were delivered via telehealth, a rate which increased to 77.8% in April 2020 before declining steadily to 67.3% by August 2020. (Table 2, Figure 1). CMHC visits declined by an average of 15.1%, with in-person visits declining by 21.6%.
3.2 Acute Care Services
All-cause ED visits dropped by 8.3% attributable primarily to declines in April 2020 (-21.9%) and May 2020 (-12.3%). All-cause hospitalizations declined by 1.0% and partial-day hospitalizations declined by 37.8%. (Table 2; Figure 1)
3.3 Medication Use
Compared to pre-pandemic levels, increases were observed in total days’ supply for oral antipsychotic medications (2.8%), antidepressants (3.7%), mood stabilizers (4.3%), and anxiolytics (3.8%). Each therapeutic class realized a significant increase in claims for 90-day supply prescription fills: oral antipsychotics (up 29.5%), antidepressants (up 23.1%), mood stabilizers (up 23.1%), and anxiolytics (up 23.1%). LAI antipsychotic prescription claims declined by 1.3% during the pandemic months examined (Table 2).
3.4 Pharmacist Scope of Practice Policy and LAI Antipsychotic Use
Most LAI antipsychotic prescriptions (63.4%) were dispensed in states that authorize pharmacists to dispense LAI antipsychotics, followed by states that authorize with a collaborative practice agreement (21.2%) and those that do not authorize (15.4%) (Table 1). States that require pharmacists to establish a collaborative practice agreement to administer LAI antipsychotics had the largest decline in utilization following pandemic onset (down 4.9% in June to August 2020) (Figure 2). In the multivariate modeling, the policies that limited scope of practice were associated with greater declines in LAI antipsychotic utilization compared to states that allowed pharmacists to dispense (represented by the negative interaction terms between pharmacist authorization and pandemic period in Table 3).
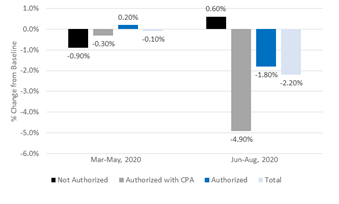
Figure 2: Percent change in average LAI antipsychotic prescription claims during the COVID-19 pandemic compared to pre-onset levels by state policy regarding pharmacist authorization to administer LAI antipsychotics
Table 3: Adjusted* association between time (in-3-month periods) and antipsychotic medication utilization during the COVID-19 pandemic among individuals with schizophrenia or schizoaffective disorder. ±
|
LAI Antipsychotic Claims |
Oral Antipsychotics (Days Supply) |
Oral Antipsychotics (90+ Days) |
||||
|
Co-efficient |
p-value |
Co-efficient |
p-value |
Co-efficient |
p-value |
|
|
Base Terms |
||||||
|
Pandemic Q1 (Mar - June 2020) |
- |
- |
1.47 |
<0.001 |
0.01 |
<0.001 |
|
Pandemic Q2 (Jul - Sept 2020) |
- |
- |
- |
- |
0.01 |
<0.0001 |
|
Pharmacist Authorization (No) |
0.05 |
<0.0001 |
- |
- |
-0.01 |
<0.0001 |
|
Pharmacist Authorization (CPA) |
0.05 |
<0.0001 |
7.69 |
<0.0001 |
- |
- |
|
African American (County %) |
0.13 |
<0.0001 |
-22.2 |
<0.0001 |
-0.04 |
<0.0001 |
|
Asian (County %) |
0.08 |
<0.01 |
- |
- |
-0.07 |
<0.0002 |
|
Hispanic (County %) |
- |
- |
-15.36 |
<0.0001 |
-0.03 |
<0.0003 |
|
Interaction with Pandemic (Q1: Mar - June 2020) |
||||||
|
African American*Pandemic Q1 |
- |
- |
- |
- |
-0.01 |
<0.05 |
|
Asian*Pandemic Q1 |
- |
- |
- |
- |
- |
- |
|
Hispanic*Pandemic Q1 |
- |
- |
- |
- |
-0.01 |
<0.05 |
|
Pharmacist Authorization (No)*Pandemic Q1 |
-0.02 |
<0.01 |
- |
- |
- |
- |
|
Pharmacist Authorization (CPA)*Pandemic Q1 |
- |
- |
- |
- |
- |
- |
|
Interaction with Pandemic (Q2: July - Sept 2020) |
||||||
|
African American*Pandemic Q2 |
0.06 |
<0.0001 |
3.03 |
<0.05 |
- |
- |
|
Asian*Pandemic Q2 |
- |
- |
8 |
<0.01 |
- |
- |
|
Hispanic*Pandemic Q2 |
-0.03 |
<0.05 |
- |
- |
- |
- |
|
Pharmacist Authorization (No)*Pandemic Q2 |
-0.02 |
<0.01 |
1.23 |
<0.05 |
- |
- |
|
Pharmacist Authorization (CPA)*Pandemic Q2 |
-0.01 |
<0.01 |
- |
- |
- |
- |
± Compared to utilization in the three months preceding the pandemic (December 1, 2019 - February 29, 2020)
4. Discussion
Early in the pandemic, public health professionals and clinicians emphasized the potential impact of the COVID-19 pandemic on the health of individuals with serious mental illness, especially individuals with schizophrenia or schizoaffective disorder [11, 12, 7]. Contemporaneously, concerns were raised about the mental healthcare delivery system, including the ability to deliver high quality care while reducing in-person contact between patients and care providers, the appropriateness of psychiatric and behavioral healthcare settings designed for in-person care, [11] and the ability to ensure continuity of medication use through transitions to mail pharmacy use [26] or home-delivery of medications [11]. Of note, use of LAI antipsychotic medications received mixed recommendations, some suggesting that transition to oral antipsychotics would reduce in-person contact [11] and others recommending a shift to LAI antipsychotics given the longer duration of effect and reduced monitoring requirements [26]. These concerns have been confirmed, at least in part, by research that reports increased risk of poor outcomes among individuals with pre-existing mental health conditions. In a recently published systematic literature review and meta-analysis, Vai, et al. [27] reported that individuals with pre-existing psychotic disorders or mood disorders were at increased risk of COVID-19 mortality and individuals with pre-existing mental health conditions were at increased risk of hospitalization. This result was confirmed by a subsequent systematic literature review which reported that individuals with pre-existing schizophrenia had a risk of mortality that was 2.2 times higher compared to individuals without schizophrenia [28]. In regard to the impact of the pandemic on mental health, however, a recently published systematic literature review that included eight longitudinal studies of individuals with schizophrenia spectrum disorder concluded that there is no consistent evidence that the pandemic led to worsening symptoms [17]. Further, a survey of 32 individuals with schizophrenia spectrum diagnoses reported consistent following of COVID-19 health and safety precautions and no post-pandemic worsening of schizophrenia symptoms [29].
4.1 Post-pandemic Changes in Healthcare Resource Utilization
Our results document rapid implementation and sustained use of telehealth-delivered psychiatric outpatient services. Despite the initial decline in in-person visits that occurred during the ramp-up of telehealth, overall outpatient care service rates for primary care, psychiatry, and psychotherapy all increased during the first six months of the pandemic. These results are consistent with clinical reports that individuals with serious mental illness, especially those with stable illness, continued to utilize preventative healthcare services [30]. Psychotherapy is perhaps the most complex healthcare service included in our analysis. Psychotherapy includes various therapeutic techniques and effectiveness is profoundly dependent upon both the continuity of care and the development and maintenance of an effective interpersonal relationship between provider and patient. This complexity is coupled with practical challenges, including differences in available technologies and limited access to private locations. Without a roadmap to guide this transition, providers have found success by personalizing transitions on a patient-by-patient basis. In combination with the well-documented reduction in missed appointments, [31] several of these approaches may contribute to the overall increase in psychotherapy contacts, including reducing visit duration but increasing frequency, offering flexible telehealth options (audio only vs. video calls), and implementing a between-visit call schedule to better monitor patients. [32,33,34].Though in-person visits to community mental health centers declined and telehealth-delivered visits increased during the pandemic, the overall visit rate declined and as of September 2020 had not returned to pre-onset levels. These results are consistent with the challenges faced by community mental health centers [35] to maintain adequate care coordination during the pandemic. Further, our results document the substantial and sustained use of telehealth for psychiatry visits, psychotherapy services, and community mental health center services, overall and specifically for care related to schizophrenia. This conforms with calls for psychiatric and psychosocial care to be delivered via telehealth [26, 36] and with evidence of significant increases in remote contacts in psychiatry [31]. Despite evidence that behavioral health services delivered via telehealth are effective, the use of telehealth-delivered psychiatry services has raised concerns about privacy, information security, different levels of access to technology, and other issues [37, 38].
In contrast, acute care services – including all-cause ED visits, inpatient and partial-day hospitalizations – show a modest but consistent decline in post-pandemic utilization. These results compare to studies conducted in the U.K. and Australia which noted 20% and 12% drop-in psychiatric inpatient admission rate, respectively [39, 40].
Antipsychotic medication use increased during the pandemic period, driven primarily by an increase in 90-day supply prescriptions. Patel et al. [31] noted changes in the delivery of psychiatric care with significant increases in remote care did not significantly influence the prescribing of antipsychotic or mood stabilizer medications. In a brief report MacLaurin et al. [41] profiled various methods used to successfully ensure continuation of antipsychotic pharmacotherapy during the early stages of the pandemic. Their model included a patient-by-patient review and personalized plan with options for switching to an LAI with a longer interval, switching to oral antipsychotics, and transition to at-home administration by a visiting nurse. The modest changes in overall LAI antipsychotic utilization in the present study are consistent with a report on antipsychotic medication use in a Canadian population [42] and with a recent survey of LAI prescribers who reported little change in oral and LAI antipsychotic prescribing practices during the COVID-19 pandemic [43].In the U.S. and worldwide, the pandemic highlighted the important role of pharmacists in ensuring continuity of care and led to an array of expanded roles and responsibilities in patient care [44]. Specific to the care of individuals with schizophrenia, the most relevant issue in the U.S. may relate to the impact of state-level policies authorizing pharmacists to administer LAI antipsychotics. According to NASPA [45], 34 states authorize pharmacists to administer LAI antipsychotics, four states and the District of Columbia do not, and 12 states authorize pharmacists to administer LAI antipsychotics with a collaborative practice agreement [46]. States that require a collaborative practice agreement to allow pharmacists to administer LAI antipsychotics were associated with less utilization of LAI antipsychotics and more utilization of oral antipsychotics following the pandemic’s onset. As LAI antipsychotic use among individuals with schizophrenia is associated with lower rates of acute care services, including hospitalization, readmission, and ED visits [47], and higher levels of medication adherence [48], ongoing innovation in and evaluation of pharmacist scope of practice may be warranted. Finally, the current study indicates a modest association between race/ethnicity and post-pandemic changes in antipsychotic medication use. Our results contribute to a growing body of evidence regarding the impact of the pandemic by racial and ethnic populations. As an example, there is compelling evidence that racial and ethnic minority populations had less access to monoclonal antibody treatment for SARS-CoV-2 infection [49] and had higher rates of COVID infection, hospitalization, and mortality [50]. Other research has reported on the association of socioeconomic and demographic factors associated with healthcare inequalities during the COVID-19 pandemic [51, 52]. In contrast, however, a recent study of over three million U.S. adults concluded the pandemic did not increase disparities in access to surgical care [53]. Despite this variability, there continue to be calls to address inequalities through policy [54] and by systematically incorporating social determinants into the healthcare delivery model [55].
Strengths and Limitations
The study population of 493,796 individuals, represents a substantial proportion of all individuals with diagnosed schizophrenia in the United States, increasing the generalizability of results. The population included individuals across a spectrum of ages, insurance types, and geographic regions. The study included both healthcare utilization and social determinants of health data, though it’s important to note that social determinants are measured at the county, rather than individual, level and only approximate individual’s specific situations. The most significant limitation is the open dataset, which does not include insurance eligibility information and thus may result in incomplete measures of healthcare utilization. Further, the dataset does not include mortality information and the criteria to ensure ongoing utilization excludes individuals who died during the pandemic from the study population.
5. Conclusions
In the early months of the pandemic, individuals with schizophrenia experienced a significant shift in the way primary care, psychiatric care, and psychotherapy was delivered. The dramatic and sustained increase in primary care, psychiatry, and psychotherapy delivered via telehealth indicates this is a viable delivery model in this population. Use of 90-day supply prescriptions for oral antipsychotic medications increased dramatically while LAI antipsychotic use decreased 1.3%. Further, changes in LAI antipsychotic use varied by state-level policy regarding pharmacist authorization to administer this medication. Given the requirement for ongoing in-person visits with a healthcare provider to receive LAI antipsychotic medication, both issues warrant further investigation. Declines in outpatient services, such as partial-day hospitalizations, may have long-term implications for mental health.
Acknowledgements
Acknowledgements: The authors wish to thank Pei Liu for analytical support and Apothecom for copy-editing and communications support.
Disclosures: The research was sponsored by Janssen Scientific Affairs. Two authors (JP, MPP) are employees of Janssen Scientific Affairs. One author (JNL) is an employee of Health Analytics, LLC which received funding to conduct the study.
References
- World Health Organization. COVID-19 public health emergency of international concern (PHEIC) (2020).
- Office of the Assistant Secretary of Emergency Preparedness and Response. Determination that a public health emergency exists. Department of Health and Human Services (2020).
- World Health Organization WHO Director – General’s opening remarks at the media briefing on COVID-19 11 (2022).
- S. White House. Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak (2020).
- Lee SY, Lei B, Mallick B. Estimation of COVID-19 spread curves integrating global data and borrowing information. PLoS One 14 (2020).
- Reynolds KA. ACP urges halting in-office visits during COVID-19 pandemic. Medical Economics (2020).
- Mehrotra A, Chernew ME, Linetsky D, et al. The Impact of the COVID-19 Pandemic on Outpatient Visits: A Rebound Emerges. The Commonwealth Fund (2020).
- Arora VM, Chivu M, Scharm A, et al. Implementing physical distancing in the hospital: A key strategy to prevent nosocomial transmission of COVID-19. J Hosp Med 15 (2020).
- Liebman D, Patel N. To Save Staff and Supplies, Designate Specialized COVID-19 Referral Centers. Health Affairs (2020).
- Druss BG. Addressing the COVID-19 Pandemic in Populations With Serious Mental Illness. JAMA Psychiatry 77 (2020).
- Shinn AK, Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. Journal of Clinical Psychiatry 81 (2020).
- Zhand N, Joober R. Implications of the COVID-19 pandemic for patients with schizophrenia spectrum disorders: narrative review. BJPsych Open 7 (2021): 35.
- Barlati S, Nibbio G, Vita A. Schizophrenia during the COVID-19 pandemic. Current Opinion in Psychiatry 34 (2021): 203-210.
- Bitan DT, Krieger I, Kridin K, Komantscher D, et al. COVID-19 prevalence and mortality among schizophrenia patients: A large-scale retrospective cohort study. Schizophrenia Bulletin 47 (2021): 1211-1217.
- Fond G, Pauly V, Leone M, et al. Disparities in intensive care unit admission and mortality among patients with schizophrenia and COVID-19: A national cohort study. Schizophrenia Bulletin 47 (2021): 624-634.
- Green AI, Canuso CM, Brenner MJ, et al. Detection and management of comorbidity in patients with schizophrenia. Psychiatric Clinics of North America 26 (2003): 115-139.
- Kunzler, AM, Lindner S, Röthke N, et al. Mental Health Impact of Early Stages of the COVID-19 Pandemic on Individuals with Pre-Existing Mental Disorders: A Systematic Review of Longitudinal Research. International Journal of Environmental Research and Public Health 20 (2023): 948.
- Miu AS, Vo HT, Palka JM, et al. Teletherapy with serious mental illness populations during COVID-19: telehealth conversion and engagement. Counselling Psychology Quarterly 34 (2020): 704-721.
- Costa M, Reis G, Pavlo A, et al. Tele-mental health utilization among people with mental illness to access care during the COVID-19 pandemic. Community Mental Health Journal 57 (2021): 720-726.
- Busch AB, Huskamp HA, Raja P, et al. Disruptions in care for Medicare beneficiaries with severe mental illness during the COVID-19 pandemic. JAMA Network Open 5 (2022).
- Ryu S, Nam HJ, Baek SH, et al. Decline in hospital visits by patients with schizophrenia early in the COVID-19 outbreak in Korea. Clinical Psychopharmacology and Neuroscience 20 (2022): 185-189.
- Hamlin M, Ymerson T, Carlsen HK, et al. Changes in Psychiatric Inpatient Service Utilization During the First and Second Waves of the COVID-19 Pandemic. Frontiers in Psychiatry 13 (2022).
- Zhu JM, Myers R, McConnell KJ, et al. Trends in outpatient mental health services use before and during the COVID-19 pandemic. Health Affairs (Millwood) 41 (2022): 573-580.
- Kisely S, Dangelo-Kemp D, Taylor M, et al. The impact of COVID-19 on antipsychotic prescriptions for patients with schizophrenia in Australia. Australian & New Zealand Journal of Psychiatry 56 (2021): 642-647.
- Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. Journal of Clinical Epidemiology 47 (1994): 1245-1251.
- Kahl KG, Correll CU. Management of patients with severe mental illness during the coronavirus disease 2019 pandemic. JAMA Psychiatry 77 (2020): 977-978.
- Vai B, Mazza MG, Colli DL, et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry 8 (2021): 797-812.
- Pardamean E, Roan W, Iskandar KTA, et al. Mortality from coronavirus disease 2019 (Covid-19) in patients with schizophrenia: A systematic review, meta-analysis and meta-regression. General Hospital Psychiatry 75 (2022): 61-67.
- Macdonald KI, Spilka, MJ, Bartolomeo LA, et al. Adherence to recommended health and social distancing precautions during the COVID-19 pandemic in individuals with schizophrenia and youth at clinical high-risk for psychosis. Schizophrenia Research 243 (2022): 446-448.
- Pinkham AE, Ackerman RA, Depp CA, et al. COVID-19-related psychological distress and engagement in preventative behaviors among individuals with severe mental illnesses. NPJ Schizophrenia 7 (2021).
- Patel R, Irving J, Brinn A, et al. Impact of the COVID-19 pandemic on remote mental healthcare and prescribing in psychiatry: an electronic health record study. BMJ 11 (2021).
- Hasson-Ohayon I, Lysaker PH. Special challenges in psychotherapy continuation and adoption for persons with schizophrenia in the age of coronavirus (COVID-19). Counselling Psychology Quarterly 17 (2021): 4811.
- Humer E, Probst T. Provision of remote psychotherapy during the COVID-19 pandemic. Digital Psychology 4 (2020): 27-31.
- Fernandez-Alvarez J, Fernandez-Alvarez H. Videoconferencing psychotherapy during the pandemic: Exceptional times with enduring effects? Frontiers in Psychology 12 (2021).
- Kopelovich SL, Monroe-DeVita M, Buck BE, et al. Community mental health care delivery during the COVID-19 pandemic: practical strategies for improving care for people with serious mental illness. Community Mental Health Journal 57 (2021): 405-415.
- Shore JH, Schneck CD, Mishkind M. Telepsychiatry and the coronavirus disease 2019 pandemic – current and future outcomes of the rapid virtualization of psychiatric care. JAMA Psychiatry 77 (2022): 1211-1212.
- Hilty DM, Parish MB, Chan S, et al. A comparison of In-Person, Synchronous and Asynchronous Telepsychiatry: Skills/Competencies, Teamwork, and Administrative Workflow. J. technol. behav. sci 5 (2020): 273–288.
- Hilty DM, Torous J, Parish MB, et al. A literature review comparing clinicians' approaches and skills to in-person, synchronous, and asynchronous care: moving toward competencies to ensure quality care. Telemedicine and e-Health 27(2021): 356-373.
- Abbas MJ, Kronenberg G, McBride M, et al. The Early Impact of the COVID-19 Pandemic on Acute Mental Health Services. Psychiatric Services 72 (2021): 242-246.
- Jagadheesan K, Danivas V, Itrat Q, et al. COVID-19 and psychiatric admissions: An observational study of the first six months of lockdown in Melbourne. Psychiatry Research 300 (2021).
- MacLaurin SA, Mulligan C, Van Alphen MU, et al. Optimal long-acting injectable antipsychotic management during COVID-19. Journal of Clinical Psychiatry 82 (2021).
- McKee KA, Crocker CE, Tibbo PG. Long-acting injectable antipsychotic (LAI) prescribing trends during COVID-19 restrictions in Canada: a retrospective observational study. BMC Psychiatry 21 (2021): 633.
- Zhdanava M, Starr HL, Totev TI, et al. Impact of COVID-19 pandemic on prescribing of long-acting injectable antipsychotics for schizophrenia: Results from a United States prescriber survey. Neuropsychiatric Disease and Treatment 18 (2022).
- Merks P, Jakubowska M, Drelich E, et al. The legal extension of the role of pharmacists in light of the COVID-19 global pandemic. Research in Social and Administrative Pharmacy 17 (2021).
- Pharmacist Authority to Administer Long-Acting Antipsychotics (2019).
- Weaver KK. Collaborative practice agreements: Explaining the basics. Pharmacy Today (2018): 55.
- Lafeuille MH, Dean J, Carter et al. Systematic review of long-acting injectables versus oral atypical antipsychotics on hospitalization in schizophrenia. Current Medical Research and Opinion 30 (2014).
- Marcus SC, Zummo J, Pettit AR, et al. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. Journal of Managed Care & Specialty Pharmacy 21 (2015): 754-769.
- Wiltz JL, Feehan AK, Molinari NAM, et al. Racial and Ethnic Disparities in Receipt of Medications for Treatment of COVID-19 – United States, March 2020-August 2021. Morbidity and Mortality Weekly Report 71 (2022).
- Khanijahani A, Iezadi S, Gholipour K, et al. A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. International Journal for Equity in Health 20 (2021).
- Maffly-Kipp J, Eisenbeck N, Carreno DF, et al. Mental health inequalities increase as a function of COVID-19 pandemic severity levels. Social Science & Medicine 285 (2021).
- Lacson R, Shi J, Kapoor N, et al. Exacerbation of inequities in the use of diagnostic radiology during the early stages of reopening after COVID-19. Journal of the American College of Radiology 18 (2021): 696-703.
- Glance LG, Chandrasekar EK, Shippey E, et al. Association Between the COVID-19 Pandemic and Disparities in Access to Major Surgery in the US. JAMA Network Open 5 (2022).
- Bambra C, Riordan R, Ford J, et al. The COVID-19 pandemic and health inequalities. Journal of Epidemiology & Community Health 74 (2020): 964-968.
- McCartan C, Adell T, Cameron J, et al. A scoping review of international policy responses to mental health recovery during the COVID-19 pandemic. Health Research Policy and Systems 58 (2021).
