The Impact of JCI Accreditation on the Clinical, Operational, and Financial Performance of Chinese Private Hospitals
Article Information
HongFan Zhang1, Mark J Bittle1, Herng-Chia Chiu1,2, Leiyu Shi1, Siou-Tang Huang2
1Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD 21205, USA
2Institute for Hospital Management, Tsinghua University, Shenzhen 518055, China
*Corresponding Author: HongFan Zhang, Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Johns Hopkins University, Baltimore, 21205, USA
Received: 22 June 2023; Accepted: 03 July 2023; Published: 10 July 2023
Citation: HongFan Zhang, Mark J Bittle, HerngChia Chiu, Leiyu Shi, Siou-Tang Huang. The Impact of JCI Accreditation on the Clinical, Operational, and Financial Performance of Chinese Private Hospitals. Journal of Radiology and Clinical Imaging. 6 (2023): 138-145.
Share at FacebookAbstract
Background: Joint Commission International (JCI) accreditation is well known as an international healthcare services organization accreditation body focused on improving the quality of healthcare and patient safety. Over 90% of JCI-accredited hospitals in China are private hospitals. Our study is the first to examine JCI accreditation's impact on Chinese private hospitals. The study objective was to assess the association between JCI accreditation and clinical, operational, and financial performance measures.
Methods: We used the multiple-group interrupted time series analysis (ITSA) to compare intervention Hospital A and comparison Hospital B in terms of eight performance measures based on monthly observations over eight years from January 2015 to December 2022. The clinical quality measures used were the C-section rate, perineal incision rate, the incidence of macrosomia, and the preterm birth rate. The operational performance indicators were the number of outpatient visits and the number of deliveries. The financial performance measures were revenue and earnings before interest, tax, depreciation & amortization (EBITDA).
Results: P value of <0.05 was used for statistical significance. The regression analysis indicated that JCI accreditation is significantly associated with the C-section rate, the number of outpatient visits, the number of deliveries, and revenue. However, JCI accreditation had no statistically significant association with the other three clinical measures, namely, the perineal incision rate, incidence of macrosomia, and preterm birth rate. No evidence demonstrated that JCI accreditation is statistically associated with EBITDA.
Conclusions: This is the first study to evaluate the impact of JCI accreditation on select clinical, operational, and financial performance measures in Chinese private hospitals, which account for over 90% of all JCI-accredited hospitals in China. JCI accreditation is significantly associated with decreasing C-section rates and increasing revenue, outpatient visits, and deliveries. The associated external assessment promotes the continuous improvement of care quality and patient safety. Hospital management may use JCI accreditation as a management tool to drive integration, collaboration, and constant improvement.
Keywords
Joint Commission International; Impact of Accreditation; Chinese Private Hospitals; Interrupted Time Series Analysis
Joint Commission International articles; Impact of Accreditation articles; Chinese Private Hospitals articles; Interrupted Time Series Analysis articles
Joint Commission International articles Joint Commission International Research articles Joint Commission International review articles Joint Commission International PubMed articles Joint Commission International PubMed Central articles Joint Commission International 2023 articles Joint Commission International 2024 articles Joint Commission International Scopus articles Joint Commission International impact factor journals Joint Commission International Scopus journals Joint Commission International PubMed journals Joint Commission International medical journals Joint Commission International free journals Joint Commission International best journals Joint Commission International top journals Joint Commission International free medical journals Joint Commission International famous journals Joint Commission International Google Scholar indexed journals Impact of Accreditation articles Impact of Accreditation Research articles Impact of Accreditation review articles Impact of Accreditation PubMed articles Impact of Accreditation PubMed Central articles Impact of Accreditation 2023 articles Impact of Accreditation 2024 articles Impact of Accreditation Scopus articles Impact of Accreditation impact factor journals Impact of Accreditation Scopus journals Impact of Accreditation PubMed journals Impact of Accreditation medical journals Impact of Accreditation free journals Impact of Accreditation best journals Impact of Accreditation top journals Impact of Accreditation free medical journals Impact of Accreditation famous journals Impact of Accreditation Google Scholar indexed journals Chinese Private Hospitals articles Chinese Private Hospitals Research articles Chinese Private Hospitals review articles Chinese Private Hospitals PubMed articles Chinese Private Hospitals PubMed Central articles Chinese Private Hospitals 2023 articles Chinese Private Hospitals 2024 articles Chinese Private Hospitals Scopus articles Chinese Private Hospitals impact factor journals Chinese Private Hospitals Scopus journals Chinese Private Hospitals PubMed journals Chinese Private Hospitals medical journals Chinese Private Hospitals free journals Chinese Private Hospitals best journals Chinese Private Hospitals top journals Chinese Private Hospitals free medical journals Chinese Private Hospitals famous journals Chinese Private Hospitals Google Scholar indexed journals Interrupted Time Series Analysis articles Interrupted Time Series Analysis Research articles Interrupted Time Series Analysis review articles Interrupted Time Series Analysis PubMed articles Interrupted Time Series Analysis PubMed Central articles Interrupted Time Series Analysis 2023 articles Interrupted Time Series Analysis 2024 articles Interrupted Time Series Analysis Scopus articles Interrupted Time Series Analysis impact factor journals Interrupted Time Series Analysis Scopus journals Interrupted Time Series Analysis PubMed journals Interrupted Time Series Analysis medical journals Interrupted Time Series Analysis free journals Interrupted Time Series Analysis best journals Interrupted Time Series Analysis top journals Interrupted Time Series Analysis free medical journals Interrupted Time Series Analysis famous journals Interrupted Time Series Analysis Google Scholar indexed journals earnings before interest, tax, depreciation & amortization articles earnings before interest, tax, depreciation & amortization Research articles earnings before interest, tax, depreciation & amortization review articles earnings before interest, tax, depreciation & amortization PubMed articles earnings before interest, tax, depreciation & amortization PubMed Central articles earnings before interest, tax, depreciation & amortization 2023 articles earnings before interest, tax, depreciation & amortization 2024 articles earnings before interest, tax, depreciation & amortization Scopus articles earnings before interest, tax, depreciation & amortization impact factor journals earnings before interest, tax, depreciation & amortization Scopus journals earnings before interest, tax, depreciation & amortization PubMed journals earnings before interest, tax, depreciation & amortization medical journals earnings before interest, tax, depreciation & amortization free journals earnings before interest, tax, depreciation & amortization best journals earnings before interest, tax, depreciation & amortization top journals earnings before interest, tax, depreciation & amortization free medical journals earnings before interest, tax, depreciation & amortization famous journals earnings before interest, tax, depreciation & amortization Google Scholar indexed journals Joint Commission on the Accreditation of Healthcare Organizations articles Joint Commission on the Accreditation of Healthcare Organizations Research articles Joint Commission on the Accreditation of Healthcare Organizations review articles Joint Commission on the Accreditation of Healthcare Organizations PubMed articles Joint Commission on the Accreditation of Healthcare Organizations PubMed Central articles Joint Commission on the Accreditation of Healthcare Organizations 2023 articles Joint Commission on the Accreditation of Healthcare Organizations 2024 articles Joint Commission on the Accreditation of Healthcare Organizations Scopus articles Joint Commission on the Accreditation of Healthcare Organizations impact factor journals Joint Commission on the Accreditation of Healthcare Organizations Scopus journals Joint Commission on the Accreditation of Healthcare Organizations PubMed journals Joint Commission on the Accreditation of Healthcare Organizations medical journals Joint Commission on the Accreditation of Healthcare Organizations free journals Joint Commission on the Accreditation of Healthcare Organizations best journals Joint Commission on the Accreditation of Healthcare Organizations top journals Joint Commission on the Accreditation of Healthcare Organizations free medical journals Joint Commission on the Accreditation of Healthcare Organizations famous journals Joint Commission on the Accreditation of Healthcare Organizations Google Scholar indexed journals obstetrics and gynecology articles obstetrics and gynecology Research articles obstetrics and gynecology review articles obstetrics and gynecology PubMed articles obstetrics and gynecology PubMed Central articles obstetrics and gynecology 2023 articles obstetrics and gynecology 2024 articles obstetrics and gynecology Scopus articles obstetrics and gynecology impact factor journals obstetrics and gynecology Scopus journals obstetrics and gynecology PubMed journals obstetrics and gynecology medical journals obstetrics and gynecology free journals obstetrics and gynecology best journals obstetrics and gynecology top journals obstetrics and gynecology free medical journals obstetrics and gynecology famous journals obstetrics and gynecology Google Scholar indexed journals neurology articles neurology Research articles neurology review articles neurology PubMed articles neurology PubMed Central articles neurology 2023 articles neurology 2024 articles neurology Scopus articles neurology impact factor journals neurology Scopus journals neurology PubMed journals neurology medical journals neurology free journals neurology best journals neurology top journals neurology free medical journals neurology famous journals neurology Google Scholar indexed journals Standard Deviation articles Standard Deviation Research articles Standard Deviation review articles Standard Deviation PubMed articles Standard Deviation PubMed Central articles Standard Deviation 2023 articles Standard Deviation 2024 articles Standard Deviation Scopus articles Standard Deviation impact factor journals Standard Deviation Scopus journals Standard Deviation PubMed journals Standard Deviation medical journals Standard Deviation free journals Standard Deviation best journals Standard Deviation top journals Standard Deviation free medical journals Standard Deviation famous journals Standard Deviation Google Scholar indexed journals American College of Surgeons articles American College of Surgeons Research articles American College of Surgeons review articles American College of Surgeons PubMed articles American College of Surgeons PubMed Central articles American College of Surgeons 2023 articles American College of Surgeons 2024 articles American College of Surgeons Scopus articles American College of Surgeons impact factor journals American College of Surgeons Scopus journals American College of Surgeons PubMed journals American College of Surgeons medical journals American College of Surgeons free journals American College of Surgeons best journals American College of Surgeons top journals American College of Surgeons free medical journals American College of Surgeons famous journals American College of Surgeons Google Scholar indexed journals
Article Details
1. Background
1.1 Joint Commission International Accreditation
The Joint Commission International (JCI) extends the Joint Commission's mission and standards worldwide by helping international healthcare organizations improve patient care quality and safety. The Joint Commission originated from the American College of Surgeons (ACS), founded in 1910 [1]. According to the history of the Joint Commission, the American College of Physicians, the American Hospital Association, the American Medical Association, and the Canadian Medical Association joined with ACS to create the Joint Commission on the Accreditation of Hospitals (JCAH) in 1950. JCAH was renamed the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) to reflect its expanded scope of services in 1987. JCAHO shortened its name to the Joint Commission in 2007. JCAHO formed JCI to provide international clients with education and consulting services in 1994. JCI published its first international quality standards for hospitals in 2000 [2]. As of December 2022, 946 healthcare organizations had obtained JCI accreditation worldwide [3].
In total, there were 36,570 hospitals, including 11,804 public hospitals and 24,766 private hospitals, in China at the end of 2021. Public hospitals are significant providers, and they served 83.9% of outpatients and 81.5% of inpatients in China from January to April 2022 [4]. Public hospitals, sponsored by the Chinese government, are not-for-profit healthcare organizations. However, most private hospitals are for-profit organizations whose shareholders and investors expect investment returns. As of December 2022, 44 Chinese hospitals had obtained valid JCI accreditation, and private hospitals accounted for 93.2% (41/44) of all accredited hospitals. General and OBGYN (obstetrics and gynecology) hospitals accounted for 45.5% (20/41) and 27.3% (12/41) of all private accredited hospitals, respectively. The other nine private accredited hospitals are specialty hospitals in the fields of plastic surgery (six), pediatrics (one), neurology (one), and rehabilitation (one) [3]. Those hospitals lose accreditation when they fail to participate in the JCI reaccreditation survey every three years after successfully passing the initial JCI accreditation survey.
1.2 Literature Review on the Impact of Hospital Accreditation
Hospital accreditation is an external, independent assessment of healthcare organizations based on accepted standards. An accreditation program should be a significant driver of improvements to the quality and safety of healthcare organizations. However, critics question the value and impact of accreditation [5]. Empirical studies on the effects of hospital accreditation conducted worldwide have shown inconsistent findings. In one study, the authors found that hospital accreditation improves care processes and outcomes. The authors pointed out that accreditation could be a tool to enhance the quality of care [6]. Other studies have concluded that hospital accreditation helps improve safety culture, process-related performance, and efficiency [7] and [8]. However, some researchers have failed to find robust evidence supporting a causal inference between hospital accreditation and measurable changes in the quality of care. They have argued that hospital accreditation programs distract healthcare professionals from their primary clinical goals and burden them with financial and labor costs [9]. The effects of JCI accreditation on the quality of care and performance have been assessed in different countries since 2010. In one study, the author concluded that pursuing JCI accreditation positively impacted 75% (9/12) of a select list of clinical measures at the 550-bed King Fahd Hospital in Saudi Arabia [10]. In another study, 60% (3/5) of the studied performance indicators achieved significant improvements due to JCI accreditation; this was found by comparing two 133-bed accredited hospitals and two 115-bed unaccredited hospitals in Jordan [11]. It was also determined that JCI accreditation helped improve operating room efficiency for patients under general anesthesia [12] and topical anesthesia at Juntendo University Hospital in Japan [13]. In a study of a JCI-accredited 150-bed acute care hospital in the United Arab Emirates, researchers raised the concern that it is challenging to sustain improved outcomes. They found an immediate drop in performance after completing the JCI accreditation survey. During the post-accreditation period, only 4% (1/27) of the selected quality measures showed a significant positive trend, but 48% (13/27) showed substantial negative changes [14]. In their comparative study of a JCI-accredited 650-bed tertiary academic hospital in the United Arab Emirates, these authors concluded that participating in reaccreditation surveys is the solution to continuous improvement [15].
2. Methods
A JCI-accredited hospital should comply with JCI standards, usually updated every three years, regarding new healthcare practices, quality management, and technology. JCI accreditation is an intervention for healthcare organizations. Most studies on the impact of JCI accreditation have conducted qualitative in-depth interviews, cross-sectional surveys, and statistical regression analyses.
2.1 Study Design
Treating JCI accreditation as an intervention, we assessed the relationship between the impact of JCI accreditation and the selected clinical, financial, and operational performance measures in Chinese private hospitals. When randomization is impossible, ITSA can be used as a robust quasi-experimental study approach to evaluate an intervention's effects in a longitudinal dataset [16]. ITSA focuses on quality improvement and requires a minimum of eight observations (data points) before and after the intervention to identify the change in an outcome between the periods before and after the intervention [17]. One of the strengths of ITSA is that it is unaffected by typical confounding variables. To deal with time-varying confounders that change relatively rapidly, researchers can add a control group to the ITSA [18]. ITSA has a high degree of internal validity, given adequate observations of an outcome variable. Researchers can further enhance this internal validity by comparing the treated group's outcomes with those of one or more control groups [19]. With one or more control groups, ITSA is more flexible and powerful than difference-in-difference (DID) methods [20]. Given the characteristics of the study population and the number of retrospective observations, a multiple-group ITSA is an appropriate design for our study. In the studies cited in the paragraph, researchers treated JCI accreditation as an intervention and used quasi-experimental approaches, such as ITSA and DID methods, to assess the impact of JCI accreditation on selected measures.
2.2 Study Population
Our study was conducted in two 200-bed private hospitals, Kunming Angel OBGYN Hospital (Hospital A) and Xi'an Angel OBGYN Hospital (Hospital B). Hospitals A and B are comparable because they are subsidiaries of the same OBGYN specialty hospital group (the parent company) and provide the same medical services in China. Hospital A began operating in 2013, and Hospital B began operating in 2014. The chief executive officer of the parent company appoints the presidents and vice presidents of Hospitals A and B, which apply the same administration system. Hospitals A and B have the same brand strategy and similar marketing tactics even though they are in different cities. From the perspective of the addressable market, Hospitals A and B are comparable in terms of the city population and residents' income. We treated Hospital A as the intervention group and Hospital B as the comparison group because Hospital A participated in the initial JCI accreditation survey in 2014 and re-accreditation surveys in 2017 and 2020. However, Hospital B decided not to join JCI reaccreditation after passing the initial JCI survey in 2015.
2.3 Data source and study variables for performance measures
The eight outcome measures of clinical, financial, and operational performance are shown in Table 1. The clinical quality measures used in the Chinese OBGYN specialty hospital were the C-section rate (Y1), the perineal incision rate (Y2), the incidence of macrosomia (Y3), and the preterm birth rate (Y4). The operational performance indicators were the number of outpatient visits (Y5) and the number of deliveries (Y6). The financial performance measures were revenue (Y7) and earnings before interest, tax, depreciation & amortization (EBITDA) (Y8). We compared Hospital A and Hospital B's performance across monthly intervals between the preintervention (from January 2015 to December 2015) and postintervention periods (from January 2016 to December 2022).
Table 1: Clinical, operational and financial performance measure descriptions
|
Measures |
Value |
Dimension of measurement |
|
|
Y1 |
C-Section Rate |
Percentage |
Process of care |
|
Y2 |
Perineal Incision Rate |
Percentage |
Outcome of care |
|
Y3 |
Incidence of Macrosomia |
Percentage |
Outcome of care |
|
Y4 |
Preterm Birth Rate |
Percentage |
Outcome of care |
|
Y5 |
No. of Outpatient Visits |
Number |
Operational performance |
|
Y6 |
No. of Deliveries |
Number |
Operational performance |
|
Y7 |
Revenue |
Number |
Financial performance |
|
Y8 |
EBITDA |
Number |
Financial performance |
2.4 Data Analysis
In the following regression equation, β_0 to [ β]_3 represent the comparison group, and β_4 to [ β]_7 represent the intervention group. The critical assumption in multiple-group ITSA is that the confounding variables affect both the intervention and comparison groups similarly [19].
Yt = + + + + + + + +et
where:
i. Yt: the outcome variable at time t;
ii. Tt: the time in months from the start of the study period to the last time point in the series, representing the frequency of monthly observations;
iii. Xt: a dummy variable representing the preintervention period (coded as "0") or postintervention period (coded as 1);
iv. Z: a dummy variable indicating the intervention group (coded as "1") or the comparison group (coded as "0");
v. β_0: the intercept (the baseline level at T=0 in the comparison group);
vi. β_1: the slope before the intervention (the change in outcome associated with a time unit increase representing the underlying preintervention trend);
vii. β_2: the level change in the period immediately following the intervention;
viii. β_3: the slope change between the preintervention and postintervention periods (using the interaction XT between the intervention and time)
ix. β_4: the difference in the intercept between the intervention and comparison groups before the intervention;
x. β_5: the difference in the slope between the intervention and comparison groups before the intervention;
xi. β_6: the difference in the level between the intervention and comparison groups in the period immediately following the intervention;
xii. β_7: the difference in the slope between the intervention and comparison groups after the intervention compared to that prior to the intervention.
We aimed to assess the associations between the independent variable X, JCI accreditation, and the dependent variable Y, representing clinical, financial, and operational performance. We used STATA 17.0 to conduct multiple-group ITSA to compare the postintervention trends in the outcome variables between Hospital A (the intervention group) and Hospital B (the comparison group). The study period spanned eight years, including the pre-intervention period from January 2015 to December 2015 and the post-intervention period from January 2016 to December 2022. The scatter plot of monthly observations against time revealed certain data features, including trends, seasonality, outliers, and turning points, as shown in Figures 1-4. Hospitals A and B followed the same organizational governance and marketing strategies during the study period. We assumed the JCI accreditation intervention was the critical event impacting the time series.
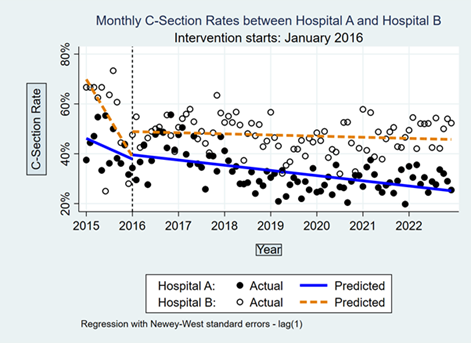
Figure 1: Monthly C-Section Rate; January 2015 to December 2022.
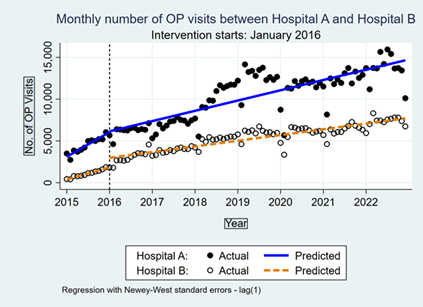
Figure 2: Monthly Outpatient Visits; January 2015 to December 2022.
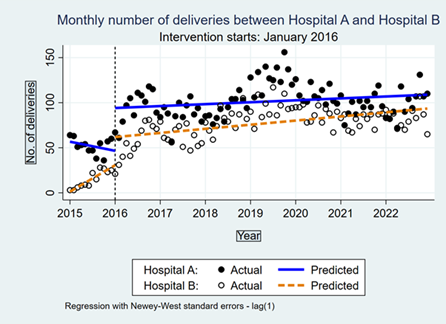
Figure 3: Monthly Deliveries; January 2015 to December 2022.
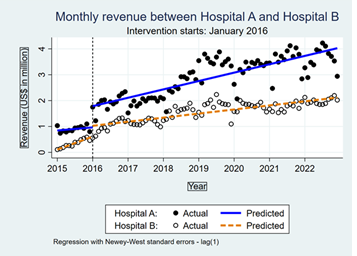
Figure 4: Monthly Revenue; January 2015 to December 2022.
3. Results
3.1 Descriptive Statistics
Data were collected for 96 months between January 2015 and December 2022 in each hospital with no gaps. The mean, median, standard deviation (SD), min (the lowest value), max (the highest value), and percentiles (p5, p25, p75, and p95) of the dependent variables are depicted in Table 2. The data were symmetrical because the measures' means and medians were similar.
Table 2: Summary statistics of monthly observation over eight years from Jan 2015 to Dec 2022
|
Hospital A |
Mean |
Median |
SD |
Min |
Max |
P5 |
p25 |
p75 |
p95 |
|
C-Section Rate |
34% |
32% |
8% |
20% |
56% |
23% |
28% |
37% |
50% |
|
Perineal Incision Rate |
25% |
25% |
10% |
8% |
52% |
12% |
18% |
31% |
44% |
|
Incidence of Macrosomia |
2% |
2% |
2% |
0% |
9% |
0% |
1% |
3% |
5% |
|
Preterm Birth Rate |
6% |
6% |
3% |
0% |
15% |
2% |
4% |
8% |
12% |
|
No. of Outpatient Visits |
9,657 |
11,078 |
3,453 |
2,733 |
15,949 |
3,936 |
6,413 |
12,426 |
14,164 |
|
No. of Deliveries |
95 |
98 |
24 |
36 |
156 |
51 |
84 |
108 |
134 |
|
Revenue (US$ million) |
2.7 |
2.8 |
1.0 |
0.7 |
4.2 |
0.8 |
2.0 |
3.5 |
4.0 |
|
EBITDA (US$ million) |
0.4 |
0.4 |
0.4 |
-1.2 |
1.4 |
-0.1 |
0.2 |
0.8 |
1.1 |
|
Hospital B |
Mean |
Median |
SD |
Min |
Max |
P5 |
p25 |
p75 |
p95 |
|
C-Section Rate |
48% |
48% |
9% |
25% |
73% |
33% |
43% |
53% |
67% |
|
Perineal Incision Rate |
16% |
15% |
10% |
0% |
66% |
0% |
10% |
20% |
30% |
|
Incidence of Macrosomia |
6% |
6% |
4% |
0% |
33% |
0% |
3% |
8% |
12% |
|
Preterm Birth Rate |
4% |
4% |
3% |
0% |
17% |
0% |
2% |
6% |
9% |
|
No. of Outpatient Visits |
4,806 |
5,393 |
2,026 |
400 |
8,317 |
825 |
3,462 |
6,303 |
7,566 |
|
No. of Deliveries |
69.8 |
78.0 |
26.9 |
3.0 |
117.0 |
8.0 |
58.0 |
87.5 |
105.0 |
|
Revenue (US$ million) |
1.4 |
1.6 |
0.6 |
0.1 |
2.2 |
0.3 |
1.1 |
1.9 |
2.0 |
|
EBITDA (US$ million) |
0.2 |
0.2 |
0.1 |
-0.8 |
0.6 |
0.0 |
0.2 |
0.3 |
0.3 |
3.2 Regression Statistics
We used STATA 17.0 to obtain the results shown in Table 3 and Figures 1-4, which show the levels and trends of Hospitals A and B. Table 3 displays the regression statistics of the time series before and after the intervention in January 2016 for the dependent variables corresponding to Hospital A and Hospital B. Lower values of the clinical measures, such as the C-section rate, perineal incision rate, incidence of macrosomia, and preterm birth rate, indicates better clinical quality. A higher number of OP visits or deliveries shows better operational performance. Higher revenue or EBITDA indicates better financial performance. P value of <0.05 was used for statistical significance.
Table 3: Time series analysis for the eight performance measures
The C-section rate is a critical indicator used to measure the quality of care in Chinese OBGYN hospitals. A decreasing trend in the C-section rate implies continuous improvement. Before the intervention, Hospital B showed a downward trend (β1=-2.6%, P<0.001, 95% CI [-3.9%, -1.2%]). However, immediately following the intervention time point, when Hospital B decided not to participate in the JCI accreditation survey, the C-section rate downward trend became slower (β3=2.5%, P<0.001, 95% CI [1.2%,3.9%]). Compared with the change in the downward trend of Hospital B, the downward trend of Hospital A became faster after the intervention (β5=1.9%, P=0.024, 95% CI [0.2%, 3.5%]; β7=-2%, P=0.016, 95% CI [-3.7%, -0.4%]). Moreover, the JCI accreditation intervention had a significant association with the C-section rate, as illustrated by the decreasing trend in Figure 1. However, the results did not show a statistically significant impact of JCI accreditation on the other clinical performance measures, including the perineal incision rate, the incidence of macrosomia, and preterm birth rate, in our study.
We hypothesized that JCI accreditation to increase the number of outpatient visits and the number of deliveries, leading to improved financial performance. The outpatient visits of Hospitals A and B increased during the pre-and postintervention periods. As seen in Figure 2, monthly outpatient visits grew faster in Hospital A than in Hospital B. Notably, in Hospital A, monthly outpatient visits increased by 102.492 visits (P<0.001, 95% CI [88.529, 116.455]), and in Hospital B, they increased by only 56.946 visits (P<0.001, 95% CI [50.676, 63.215]) after the intervention. The difference between the hospitals (Hospital A minus Hospital B) was 45.547 outpatient visits per month (P<0.001, 95% CI [30.241,60.853]). Regarding the impact of JCI accreditation on the growth trends in monthly deliveries, the trend of deliveries in Hospital B was worse in the postintervention period than it was in the preintervention period (β1=2.451, P<0.001, 95% CI [1.945, 2.957]; β3=-2.070, P<0.001, 95% CI [-2.623, -1.518]). Compared with the trend of Hospital B, Hospital A's trend improved after the intervention (β5=-3.294, P<0.001, 95% CI [-4.966, -1.622]; β7=3.090, P<0.001, 95% CI [1.408, 4.773]). Figure 3 displays these trends. The economic impact of JCI accreditation on monthly revenue (US$ million) could be quantified as the estimated coefficient of the difference (coefficient=0.014, P<0.001, 95% CI [0.009, 0.019]) between Hospital A and Hospital B after the intervention. Hospital A generated US$14,000 more in revenue over the postintervention period than Hospital B. And the estimated coefficient of the difference in monthly EBITDA (coefficient=0.004, P=0.019, 95% CI [0.0006, 0.0067]) indicated that Hospital A could generate more US$ 4,000 of monthly EBITDA over the postintervention period than Hospital B. Figure 4 displays the comparison trends after the intervention.
4. Discussion
This study is the first to evaluate the impact of JCI accreditation on Chinese private hospitals. Maintaining a hospital's accreditation requires resources such as money and time; whether a hospital's accreditation is associated with a measurable improvement in its performance is critical for healthcare policymakers and hospital management to know who aims to support investments in the accreditation program. JCI accreditation is designed to evaluate healthcare organizations' full range of functions. The systems and processes supporting patient care and leadership in a JCI-accredited hospital comply with JCI standards, which are typically updated every three years based on new healthcare practices, quality management methods, and technology guidance. We hypothesized that JCI accreditation results in better clinical outcomes and financial and operational performance. Hospital A engaged in three JCI accreditation surveys from 2014 to 2020, but Hospital B participated in only the JCI accreditation survey in 2015. Some researchers found that the number of years that a hospital has been engaged in hospital accreditation can affect organizational changes that enhance the quality of care [21]. Our results showed a significant association between the C-section rate and JCI accreditation. JCI accreditation had no statistically significant impact on the other selected clinical performance measures. This evidence confirms findings from previous studies conducted in other countries. Some studies did not find strong evidence of a relationship between hospital accreditation and specific quality indicators [22]. Other studies found a complex relationship when comparing the indicator performance of accredited and unaccredited hospitals. The accredited hospitals performed better than the unaccredited hospitals on some quality indicators but failed to perform better on others [23]. In an updated systematic review, authors found positive, negative, and no association between hospital accreditation and organizational performance [24]. JCI accreditation could be used as a marketing tool, as it may reassure patients and enhance their confidence in the high quality of care and safety [22]. Hospital accreditation requires external assessments because patients cannot observe the quality of healthcare services benchmarked against standards and processes [25]. Our results showed that Hospital A performed better in increasing revenue, outpatient visits, and deliveries than Hospital B during the postintervention period. We think the gold seal of JCI accreditation could cause more patients to visit an accredited hospital than a comparable unaccredited hospital because of the JCI's reputation for assessing excellence in the quality of care and patient safety. Hospital A achieved a better EBTIDA trend than Hospital B during the postintervention period. One reason is that more revenue would improve financial margin given the fixed cost structure.
4.1 Implications
The management of Hospital B may argue that they have learned the JCI standards even though they decided not to participate in the JCI survey after passing the initial survey. Most Chinese private hospitals are for-profit hospitals. Only when a for-profit hospital believes its revenue exceeds the costs of obtaining an accreditation will the hospital be motivated to seek the accreditation [25]. For Chinese healthcare policymakers, if there is evidence showing that the JCI standards help improve the quality of care and patient safety, foreign hospital accreditation can complement local accreditation. Additionally, Chinese private hospital management may use JCI accreditation as a management tool to drive integration, collaboration, and improvement. When a private hospital is newly set up based on various teams with different backgrounds, the accreditation process might accelerate the integration of clinical procedures and promote a safety culture. In addition, there may be value in participating in the JCI accreditation survey process since the associated external assessment promotes the continuous improvement of care quality.
4.2 Limitations
The study results cannot be generalized to Chinese public hospitals, but generally, Chinese public hospitals have far fewer motivations than private hospitals to pursue JCI accreditation. The evidence provided in our study stems from OBGYN specialty hospitals, so the conclusions may not be generalized to other types of hospitals. Also, the study findings might not be generalized to other OBGYN hospitals either. Although our quantitative outcome-based analysis may examine the value of JCI accreditation, it is not easy to evaluate the challenges related to accreditation. We recommend that further research be conducted to explore the sustainability of JCI accreditation within Chinese private hospitals. The comparison group was exposed to the JCI program. Our study could not differentiate between the impact of such exposure on the comparison group's performance and the effects of JCI reaccreditation on the intervention group.
5. Conclusions
Over 90% of JCI-accredited Chinese hospitals are private hospitals. This paper is the first study to use a multiple-group time series analysis to evaluate the impact of JCI accreditation on clinical, operational, and financial performance in Chinese private hospitals. The evidence we obtain by comparing Hospitals A and B demonstrates that the subsequent JCI accreditation surveys improve one of the four selected clinical indicators and increase outpatient visits, deliveries, and revenue. Therefore, we conclude that although JCI accreditation may not be significantly associated with the improvement of all the select performance measures, it does seem to be associated with continuous improvement in accredited Chinese private hospitals.
List of abbreviations
ACS: American College of Surgeons
JCAH: Joint Commission on the Accreditation of Hospitals
JCAHO: Joint Commission on the Accreditation of Healthcare Organizations
JCI: Joint Commission International
ITSA: Interrupted Time Series Analysis
OBGYN: obstetrics and gynecology
OP: Outpatient
DID: Difference-In-Difference
EBITDA: Earnings before interest, tax, depreciation & amortization
SD: Standard Deviation
Declarations
Ethics Approval and Consent to Participate
Not applicable
Consent for Publication
Not applicable
Availability of Data and Materials
The dataset supporting the conclusions of this article is included within the article.
Competing Interests
The authors declare that they have no competing interests.
Funding
Not applicable
Authors' Contributions
HZ conducted the study and drafted the manuscript under MJB’s supervision. HCC and STH participated in the study design. All authors read and approved the final manuscript.
Acknowledgments
Not applicable
References
- Bord S, Sass I, Hayms G, et al. Involvement and skepticism towards the JCI Accreditation process among hospital's four sectors employees: suggestions for cultural change. Isr J Health Policy Res 10 (2021): 74.
- The Joint Commission. The Joint Commission History Timeline. In: History of the Joint Commission (2022).
- The Joint Commission International. Country/Region/Territory: China. In: Search for JCI-accredited organizations (2022).
- National Health Commission of the People's Republic of China. 2021 China's health development statistical bulletin. China: National Health Commission of the People's Republic of China (2022).
- Shaw CD, Kutryba B, Braithwaite J, et al. Sustainable healthcare accreditation: messages from Europe in 2009. Int J Qual Health Care 22 (2010): 341-50.
- Alkhenizan A, Shaw C. Impact of accreditation on the quality of healthcare services: a systematic review of the literature. Ann Saudi Med 31 (2011): 407-16.
- Araujo CAS, Siqueira MM, Malik AM. Hospital accreditation impact on healthcare quality dimensions: a systematic review. Int J Qual Health Care 32 (2020): 531-44.
- Hussein M, Pavlova M, Ghalwash M, et al. The impact of hospital accreditation on the quality of healthcare: a systematic literature review. BMC Health Serv Res 21 (2021): 1057.
- Brubakk K, Vist GE, Bukholm G, et al. A systematic review of hospital accreditation: the challenges of measuring complex intervention effects. BMC Health Serv Res 15 (2015): 280.
- Al Shawan D. The effectiveness of the joint commission international accreditation in improving quality at king fahd university hospital, Saudi Arabia: a mixed methods approach. J Healthc Leadersh 13 (2021): 47-61.
- Halasa YA, Zeng W, Chappy E, et al. Value and impact of international hospital accreditation: a case study from Jordan. East Mediterr Health J 21 (2015): 90-9.
- Inomata T, Mizuno J, Iwagami M. The impact of joint commission international accreditation on time periods in the operating room: A retrospective observational study. PloS One 13 (2018).
- Okumura Y, Inomata T, Iwagami M, et al. Shortened cataract surgery by standardisation of the perioperative protocol according to the Joint Commission International accreditation: a retrospective observational study. BMJ Open 9 (2019): 028656.
- Devkaran S, O'Farrell PN. The impact of hospital accreditation on quality measures: an interrupted time series analysis. BMC Health Serv Res 15 (2015): 137.
- Devkaran S, O'Farrell PN, Ellahham S, et al. Impact of repeated hospital accreditation surveys on quality and reliability, an 8-year interrupted time series analysis. BMJ Open 9 (2019):
- Kontopantelis E, Doran T, Springate DA, et al. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ 350 (2015): 2750.
- Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr 13 (2013): 38-44.
- Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 46 (2017): 348-55.
- Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J 15 (2015): 480-500.
- Bernal JL, Cummins S, Gasparrini A. Difference in difference, controlled interrupted time series and synthetic controls. Int J Epidemiol 48 (2019): 2062-3.
- Pomey MP, Lemieux-Charles L, Champagne F, et al. Does accreditation stimulate change? A study of the impact of the accreditation process on Canadian healthcare organizations. Implement Sci 5 (2010): 31.
- Braithwaite J, Greenfield D, Westbrook J, et al. Health service accreditation as a predictor of clinical and organisational performance: a blinded, random, stratified study. Qual Saf Health Care 19 (2010): 14-21.
- Greenfield D, Braithwaite J. Health sector accreditation research: a systematic review. Int J Qual Health Care 20 (2008): 172-83.
- Hinchcliff R, Greenfield D, Moldovan M, et al. Narrative synthesis of health service accreditation literature. BMJ Quality and Safety 21 (2012): 979–991.
- Grepperud S. Is the hospital decision to seek accreditation an effective one? Int J Health Plann Manage 30 (2015): 56-68.
