The Effect of SGLT-2i and GLP-1RA on Major Cardiovascular Conditions: A Meta-Analysis
Article Information
Arjun V. Jogimahanti1*, Kevin A. Honan1, Talha Ahmed2, Luis Leon-Novelo3, Tarif Khair, M.D.2
1University of Texas Medical School at Houston, Department of Internal Medicine, Houston, TX, United States of America
2University of Texas Medical School at Houston, Department of Cardiology, Houston, TX, United States of America
3University of Texas School of Public Health, Department of Biostatistics, Houston, TX, United States of America
*Corresponding author: Arjun V. Jogimahanti, University of Texas Medical School at Houston, Department of Internal Medicine, Houston, TX, United States of America
Received: 14 January 2024; Accepted: 19 January 2024; Published: 12 February 2024
Citation: Arjun V. Jogimahanti, Kevin A. Honan, Talha Ahmed, Luis Leon-Novelo, Tarif Khair. The Effect of SGLT-2i and GLP-1RA on Major Cardiovascular Conditions: A Meta-Analysis. Cardiology and Cardiovascular Medicine. 8 (2024): 60-74.
Share at FacebookAbstract
Purpose: Sodium-glucose co-transporter 2 inhibitors (SGLT-2i) and Glucagon-like Peptide-1 Receptor Agonists (GLP-1RA) are two common anti-hyperglycemic agents prescribed by clinicians. The effects on cardiovascular conditions such as heart failure (HF) hospitalization, stroke, myocardial infarctions (MI), and other cardiovascular conditions are not well studied. The purpose of this study is to analyze existing data on the effect of SGLT-2i and GLP-1RA on preventing these cardiovascular conditions.
Methods: A retrospective meta-analysis of all existing literature of the effect of SGLT-2i and GLP-1RA on the rates of the following categories was researched: primary cardiovascular outcomes, HF hospitalizations, atrial fibrillation (AF), stroke, MI and HF symptoms. Hazard ratios for each category were obtained, and overall Hazard Ratio (HR)’s to determine overall statistical significance were computed.
Result: Both medication classes provided statistically significant reduction in preventing major cardiovascular events. Only SGLT-2i provided statistically significant reduction in heart failure hospitalizations. Only GLP-1RA provided statistically significant reduction in preventing stroke. Neither medication class provided a statistically significant benefit in preventing myocardial infarctions. More studies are needed on effects of either SGLT-2i or GLP-1RA agonists on preventing HF symptoms or AF.
Conclusion: This study demonstrates that SGLT-2i and GLP-1RA are important for improving both diabetic and cardiovascular health. In patients at risk for a major cardiovascular event, SGLT-2i or GLP-1RA may be prescribed by clinicians. More studies must be performed to draw more conclusions.
Keywords
Cardiovascular; SGLT-2i; GLP-1RA
Article Details
List of Abbreviations
- SGLT-2 Inhibitors: Sodium-glucose co-transporter 2 inhibitors
- GLP-1RA Agonists: Glucagon-like Peptide-1 agonists
- FDA: Food and Drug Administration
- T2DM: Type 2 Diabetes Mellitus
- AF: Atrial Fibrillation
- MI: Myocardial Infarction
- HF: Heart Failure
Background
Cardiovascular disease (CVD) remains the leading cause of morbidity and mortality in patients with diabetes mellitus. Sodium-glucose co-transporter 2 inhibitors (SGLT-2i) and Glucagon-like Peptide-1 Receptor Agonists (GLP-1RA) are two anti-hyperglycemic agents that have emerged as new therapies for patients with Type Two Diabetes Mellitus (T2DM) and are currently being prescribed by a vast number of clinicians. SGLT-2i prevent the reuptake of sodium, glucose, and water at the proximal convoluted tubule of the nephron1. GLP-1RA help stimulate the endogenous production of insulin2. While elevated blood glucose and T2DM were the original indications of use for these medications, utility in heart failure (HF) and other cardiac conditions have been recently explored. Some of the mechanisms that have been postulated that have helped include afterload reduction as well as improved glycemic control. Afterload reduction, achieved through proper blood pressure management, is thought to improve cardiac strain. Glycemic control is thought to reduce the risk for metabolic events and coronary artery disease [1,2].
Due to initial landmark trials demonstrating the benefit of SGLT-2i, the Food and Drug Administration (FDA) approved the use of this medication class for use in heart failure and other heart-related medical conditions in 2020 [3]. Many other anti-hyperglycemic medications, including GLP-1RA, have been studied for their role in improving cardiovascular outcomes. Some GLP-1RA, including Dulaglutide, have also been approved for reduction of cardiovascular events [4]. Randomized controlled trials (RCTs) have demonstrated the benefit in many aspects of the cardiovascular profile including Major Adverse Cardiac Events (MACE), heart failure (HF) hospitalization rates, atrial fibrillation (AF) rates, and the development of HF symptoms. Data regarding the benefit of different medications in either of the two medication classes in the aforementioned disease categories needs to be explored further. Thus, the purpose of this meta-analysis is to determine which cardiac diseases have been shown by the current literature to be most positively impacted by SGLT-2i and GLP-1RA and to discuss the relative performance of both drugs in various cardiovascular disease categories. The results of this study would allow clinicians to effectively manage patients with these co-morbidities or at risk for these co-morbidities. If these medications demonstrated statistically significant benefit in any of the studied cardiovascular conditions, this could help reduce the rate of development of condition or incidence of severe outcomes.
Methods
A literature search, conducted by all authors listed in the authorship, using the databases PubMed and Google Scholar were performed, ranging from the years 2010-2022. The search for studies lasted three months, occurring mostly in the first quarter of 2022. The following keywords and their MeSH terms were used for the search: ‘(sodium-glucose co-transporter inhibitor OR SGLT2 inhibitor OR SGLT-2 inhibitor OR SGLT 2 inhibitor), (Glucagon-like Peptide-1 Receptor agonist OR GLP-1RA OR GLP1 agonist), (heart failure or cardiac failure OR CHF)’. The effect of both drug classes (SGLT-2i and GLP-1RA) on the rates of the following categories was researched: Major Adverse Cardiac Events (MACE), HF symptoms and hospitalizations, AF, stroke, and myocardial infarction. MACE was defined as the traditional three-point definition: death from cardiovascular cause, nonfatal stroke, or nonfatal myocardial infarction. The criteria used for selection of the categories included availability of data from chart review and results of prior available studies. While most other studies focus on MACE and HF, other aspects of cardiovascular disease, such as atrial fibrillation, stroke, and MI, are not well-covered. This was decided after database review on PubMed and Google Scholar platforms. As a result, the decision to study the effects of SGLT-2i and GLP-1RA on these other cardiovascular diseases was made.
Regarding the criteria of studies chosen, those that met the criteria above were included in the study. It is approximated that more than 50% of the search results did not meet the inclusion criteria.
Inclusion Criteria and Outcomes of Interest
Inclusion criteria for the studies included: 1. Large randomized controlled trials (RCTs) or meta-analyses of previously performed RCTs. Large Randomized controlled trials were defined as studies whose patient populations were greater than 1,000 participants. 2. Patients who took either SGLT-2i or GLP-1RA. The outcomes of interest included the hazard ratios (HR) and percent changes compared to placebo within each disease type for both SGLT-2i and GLP-1RA. 3. Studies that assessed the effect of SGLT-2 or GLP-1 agonists on any of the following cardiovascular profiles: primary cardiovascular outcomes, HF symptoms and hospitalizations, AF, stroke, and myocardial infarction.
Statistical Analysis
For all meta-analyses, the Bayesian Hierarchical model for Meta Analysis was applied as presented in section 5.6 of Gelman to estimate the overall hazard ratio along with central 95% credible interval. This model is the Bayesian version of the random-effects meta-analysis introduced by DerSimonian and Laird (1986) [5,6]. More specifically, for each study , we performed the log of the hazard ratio, , and computed the standard deviation of the log hazard ratio estimate, , based on the length of the log transformed confidence intervals. We fit the Bayesian mode with standard deviation and priors and proportional to 1. For meta-analysis that consider four or fewer studies, priors proportional to 1 and a standard normal restricted to the positive real line were used. The overall hazard ratio estimate is the posterior expected value of with central 95% credible interval given by the 0.025 and 0.975 posterior quantiles of . To standardize notation, in this paper we call P-Value the Bayesian measure of evidence against the Null hypothesis (Pereira and Stern, 1999), defined as the smallest number ev such that the 1-ev central credible interval for estimate overall HR (i.e., exp(mu)) does not contain the null value (HR=1) indicating overall no difference between the treatment groups [7]. The Bayesian measure of evidence is a P-value in the sense that it is the result of “inverting the credible interval” similar to the inversion of the confidence interval to compute a p-value. Additionally, as a measurement of heterogenicity in the outcomes across studies, we compute the Bayesian version of that is interpreted as the total variation in the estimates of treatment effect that is due to heterogeneity between studies8. Values of close to zero indicate that the clinical trials are homogeneous for the category while values close to 1 indicate heterogenicity [8].
P-values, for determination of statistical significance, were evaluated against an alpha value of 0.05. A p-value less than the alpha value of 0.05 was determined to be statistically significant and the null hypothesis of no difference between treatment and placebo was rejected. For the Ejection Fraction analysis, analysis of variance was performed to detect the main effects, and difference between SGLT-2 inhibitors and GLP-1RA. Computations were carried out using R statistical programming language and R package rstan.
Results (Data)
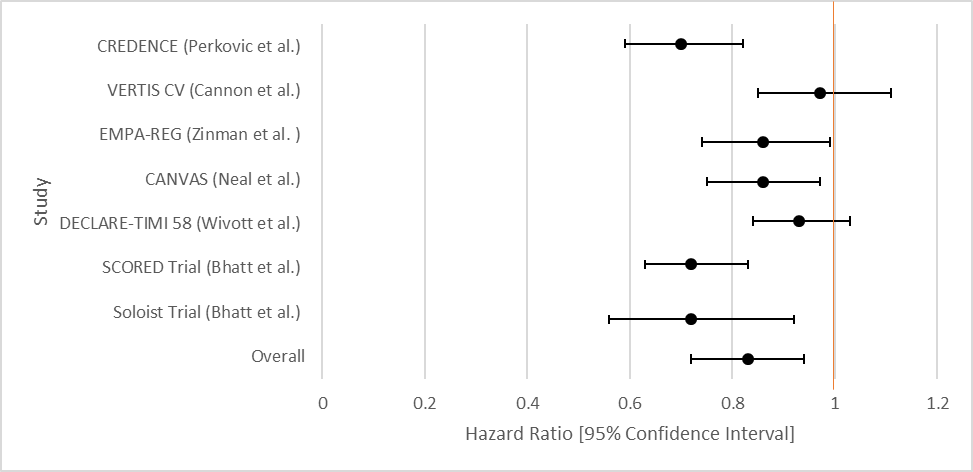
Major Adverse Cardiovascular Event (MACE)
The overall aggregate of the studies demonstrated statistical significance for both SGLT-2i and GLP-1RA in prevention of MACE. Both groups employed studies with large sample sizes. Even within individual studies, a majority of the studies that were included for each drug type demonstrated statistical significance with respect to MACE.
|
Author |
Study Population |
SGLT-2i Type |
HR [95% Confidence Interval] |
|
CREDENCE (Perkovic et al.) [9] |
4, 401 patients with T2DM and chronic kidney disease. |
Canagliflozin |
0.70[0.59-0.82] |
|
VERTIS CV (Cannon et al.) [10] |
8,246 randomly assigned patients with T2DM and atherosclerotic cardiovascular disease. |
Ertugliflozin |
0.97 [0.85-1.11] |
|
EMPA-REG (Zinman et al.) [11] |
7,020 patients with T2DM at high cardiovascular risk. |
Empagliflozin |
0.86 [0.74-0.99] |
|
CANVAS (Neal et al.) [12] |
10,142 participants with T2DM and high cardiovascular risk. |
Canagliflozin |
0.86 [0.75-0.97] |
|
DECLARE-TIMI 58 (Wivott et al.) [13] |
17,160 patients patients with T2DM who had or were at risk for atherosclerotic cardiovascular disease |
|
0.93 [0.84-1.03] |
|
SCORED Trial (Bhatt et al.) [14] |
10, 584 patients were randomized in a 1:1 fashion to either sotagliflozin 400 mg daily (n = 5,292) or placebo (n = 5,292). Sotagliflozin was started at 200 mg daily and increased to target dose if there were no unacceptable side effects. |
Sotagliflozin |
0.72[0.63-0.83] |
|
Soloist Trial (Bhatt et al.) [15] |
1,222 patients with T2DM who were recently hospitalized for worsening heart failure were randomly assigned to receive sotagliflozin or placebo. |
Sotaglifozin |
0.72[0.56-0.92] |
|
Overall Results |
0.83[0.72-0.94] |
||
|
p-value |
0.014 |
||
|
76.68 |
Table 1: Data Results of Studies Investigating the effect of SGLT-2i on Primary Cardiovascular Outcomes
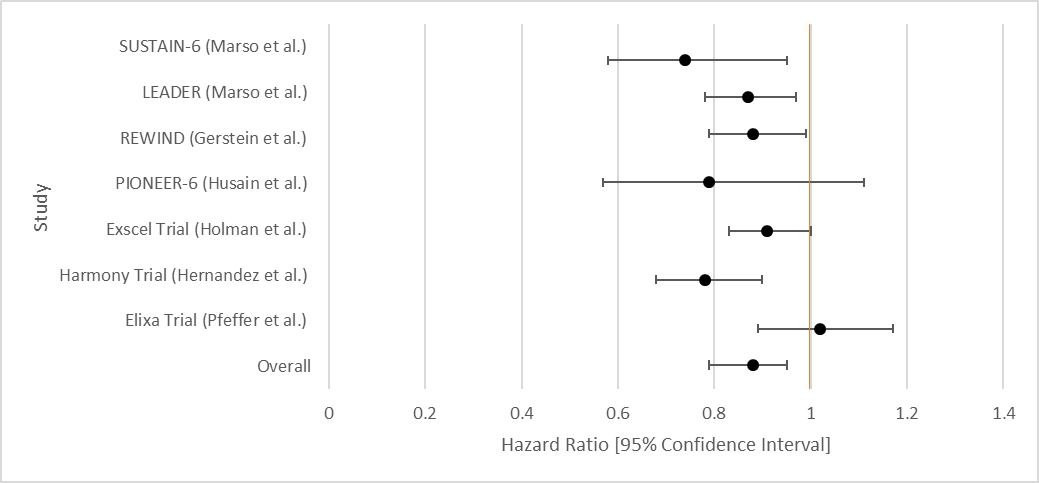
|
Author or Trial |
Study Population |
GLP-1RA |
Hazard Ratio [95% Confidence Interval] |
|
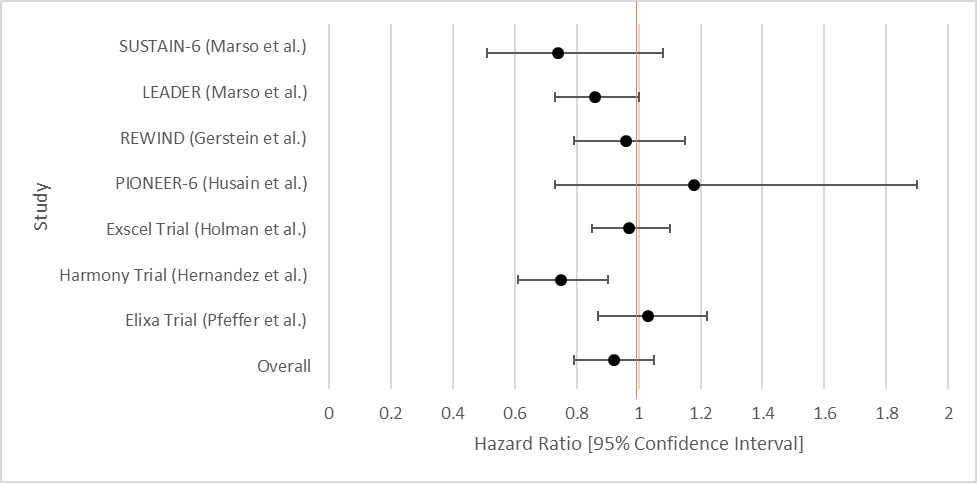
SUSTAIN-6 (Marso et al.) [16] |
3,297 patients with T2DM and glycated Hgb 7% or more. |
Semaglutide |
0.74[0.58-0.95] |
|
LEADER (Marso et al.) [17] |
9,340 patients were randomly assigned patients with T2DM and high cardiovascular risk to receive liraglutide or placebo. |
Liraglutide |
0.87(0.78-0.97) |
|
REWIND (Gerstein et al.) [18] |
9,901 patients at least 50 years with T2DM who had either a previous cardiovascular event or cardiovascular risk factors. |
Dulaglutide |
0.88 [0.79-0.99] |
|
PIONEER-6 (Husain et al.) [19] |
Total: 5,878 patients. 3,183 patients. The mean age of the patients was 66 years; 2695 patients (84.7%) were 50 years of age or older and had cardiovascular or chronic kidney disease. |
Semaglutide |
0.79 [0.57-1.11] |
|
Exscel Trial (Holman et al.) [20] |
14,752 patients with T2DM regardless of previous cardiovascular disease. |
Exenatide |
0.91 [0.83-1.00] |
|
Harmony Trial (Hernandez et al.) [21] |
Total: 9,463 patients. 4,731 patients were assigned to receive albiglutide and 4,732 patients to receive placebo. Patient ages were 40 years and older. Underlying conditions included T2DM and cardiovascular disease (at a 1:1 ratio). |
Albiglutide |
0.78 [0.68-0.90] |
|
Elixa Trial (Pfeffer et al.) [22] |
6,068 patients with T2DM who had had a myocardial infarction or who had been hospitalized for unstable angina within the previous 180 days to receive lixisenatide or placebo |
Lixisenatide |
1.02[0.89-1.17] |
|
Overall Results |
0.88[0.79-0.95] |
||
|
p-value |
0.012 |
||
|
72.44 |
Table 2: Data Results of Studies Investigating the effect of GLP-1RA on Primary Cardiovascular Outcomes
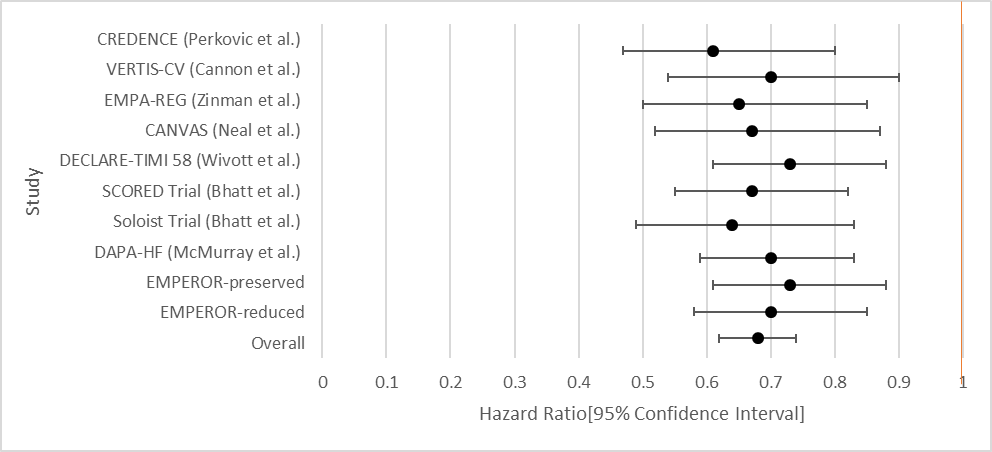
Heart Failure Hospitalizations
The overall aggregate of the studies demonstrated statistical significance for SGLT-2i. GLP-1RA did not demonstrate statistical significance. Within individual studies, all of the studies for SGLT-2i showed a statistically significant result. For GLP-1RA only one such study demonstrated a benefit.
|
Author |
Study Population |
SGLT-2i Type |
Hazard Ratio [95% Confidence Interval] |
|
CREDENCE (Perkovic et al.) [9] |
4,401 patients with T2DM and chronic kidney disease (CKD). |
Canagliflozin |
0.61[0.47-0.80] |
|
VERTIS-CV (Cannon et al.) [10] |
8,246 patients with T2DM and atherosclerotic cardiovascular disease. |
Ertugliflozin |
0.70 [0.54-0.90] |
|
EMPA-REG (Zinman et al.) [11]
|
7,020 patients with T2DM at high cardiovascular risk. |
Empagliflozin |
0.65 [0.5-0.85] |
|
CANVAS (Neal et al.) [12] |
10,142 participants with T2DM and high cardiovascular risk. Participants in each trial were randomly assigned to receive canagliflozin or placebo. |
Canagliflozin |
0.67[0.52-0.87] |
|
DECLARE-TIMI 58 (Wivott et al.) [13] |
17,160 patients with T2DM and had multiple risk factors for atherosclerotic cardiovascular disease or had established atherosclerotic cardiovascular disease. |
Dapagliflozin |
0.73[0.61-0.88] |
|
SCORED Trial (Bhatt et al.) [14] |
10, 584 patients were randomized in a 1:1 fashion to either sotagliflozin 400 mg daily (n = 5,292) or placebo (n = 5,292). Sotagliflozin was started at 200 mg daily and increased to target dose if there were no unacceptable side effects. |
Sotagliflozin |
0.67[0.55-0.82] |
|
Soloist Trial (Bhatt et al.) [15] |
1,222 patients with T2DM who were recently hospitalized for worsening heart failure were randomly assigned to receive sotagliflozin or placebo. |
Sotaglifozin |
0.64[0.49-0.83] |
|
DAPA-HF (McMurray et al.) [23] |
4,744 patients with New York Heart Association class II, III, or IV heart failure and an ejection fraction of 40% or less to receive either dapagliflozin (at a dose of 10 mg once daily) or placebo. |
Dapagliflozin |
0.70[0.59-0.83] |
|
Emperor-Preserved (Anker et al.) [24] |
5,988 patients with class II-IV heart failure and an ejection fraction of more than 40% to receive empagliflozin or placebo. |
Empagliflozin |
0.73[0.61-0.88] |
|
Emperor-Reduced (Packer et al.) [25] |
3,730 patients with class II, III, or IV heart failure and an ejection fraction of 40% or less to receive empagliflozin (10 mg once daily) or placebo |
Empaglifozin |
0.70[0.58-0.85] |
|
Overall Results |
0.69[0.64-0.74] |
||
|
p-value |
<0.001 |
||
|
25.81 |
Table 3: Data Results of Studies Investigating the effect of SGLT-2i on HF Hospitalizations
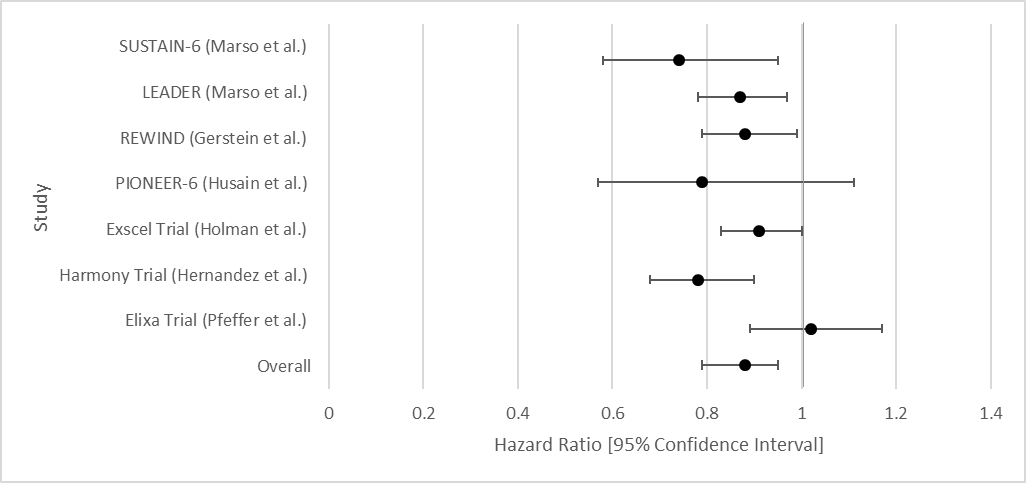
|
Author or Trial |
Study Population |
GLP-1RA |
Hazard Ratio [95% Confidence Interval] |
|
SUSTAIN-6 (Marso et al.) [16] |
3,297 patients with T2DM and glycated Hgb 7% or more. |
Semaglutide |
1.11 [0.77-1.61] |
|
LEADER (Marso et al.) [17] |
9,340 patients randomized who had T2DM. |
Liraglutide |
0.87 [0.73-1.05] |
|
REWIND (Gerstein et al.) [18] |
9,901 patients at least 50 years with T2DM who had either a previous cardiovascular event or cardiovascular risk factors. |
Dulaglutide |
0.93[0.77-1.12] |
|
PIONEER-6 (Husain et al.) [19] |
Total: 5,878 patients. 3,183 patients. The mean age of the patients was 66 years; 2695 patients (84.7%) were 50 years of age or older and had cardiovascular or chronic kidney disease. |
Semaglutide |
0.86 [ 0.48-1.55] |
|
Exscel Trial (Holman et al.) [20] |
14,752 patients with T2DM regardless of previous cardiovascular disease. |
Exenatide |
0.94 [0.70-1.13] |
|
Harmony Trial (Hernandez et al.) [21] |
Total: 9,463 patients. 4,731 patients were assigned to receive albiglutide and 4,732 patients to receive placebo. Patient ages were 40 years and older. Underlying conditions included T2DM and cardiovascular disease (at a 1:1 ratio). |
Albiglutide |
0.71 [0.53-0.94] |
|
Elixa Trial (Pfeffer et al.) [22] |
6,068 patients with T2DM who had had a MI or who had been hospitalized for unstable angina within the previous 180 days to receive lixisenatide or placebo. |
Lixisenatide |
0.96[0.75-1.23] |
|
Overall Results |
0.90[0.79-1.04] |
||
|
p-value |
0.122 |
||
|
48.64 |
Table 4: Data Results of Studies Investigating the effect of GLP-1RA on HF Hospitalizations
Atrial Fibrillation
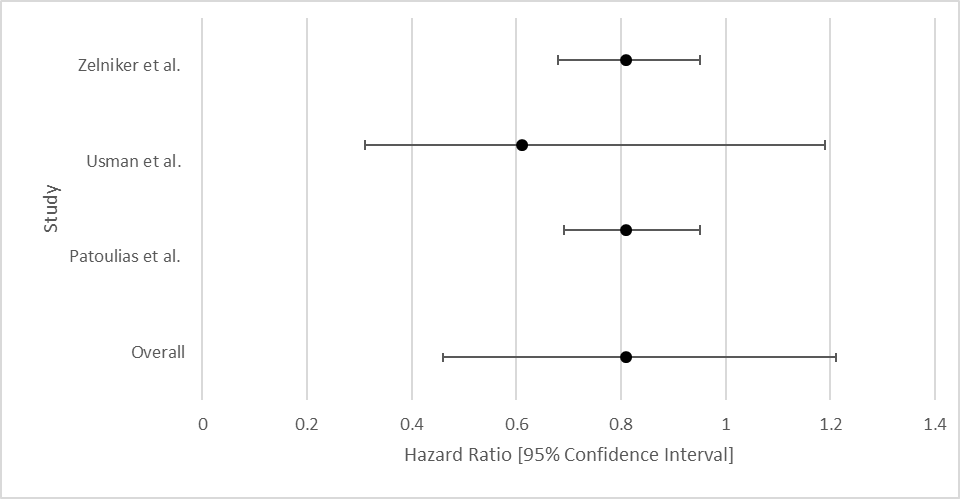
The overall aggregate of studies showed no statistically significant benefit for SGLT-2i in preventing AF. Individually, 2/3 of the studies did show benefit. Data for GLP-1RA were limited.
|
Author |
Study Population |
SGLT-2i Type |
Hazard Ratio [95% Confidence Interval] |
|
Zelniker et al. [26] |
17, 160 patients with T2DM and multiple risk factors for atherosclerotic cardiovascular disease. |
Dapagliflozin |
0.81 [0.68-0.95] |
|
Usman et al. [27] |
35 randomized controlled trials with a total of 34,987 patients with T2DM. |
Unspecified SGLT-2 |
0.61[0.31-1.19] |
|
Patoulias et al. [28] |
Patients with T2DM and Cardiac Risk Factors |
SGLT-2 inhibitors (unspecified) |
0.81[0.69-0.95] |
|
Overall Results |
0.81[0.46-1.24] |
||
|
p-value |
0.144 |
||
|
92.47 |
Table 5: Data Results of Studies Investigating the effect of SGLT-2i on Atrial Fibrillation
Stroke
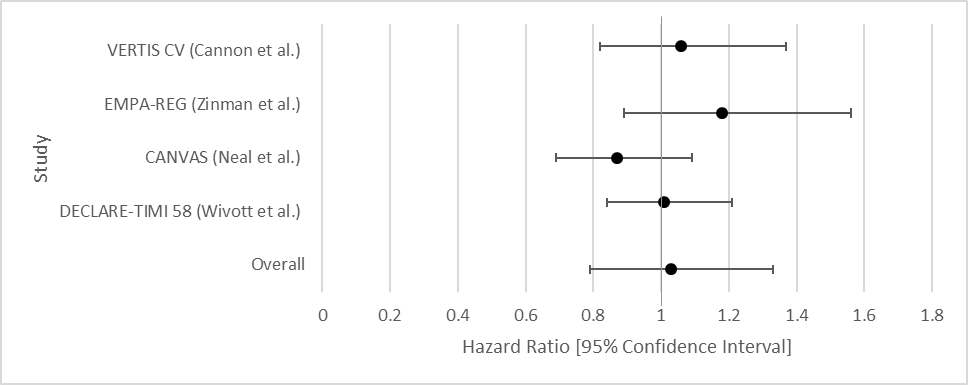
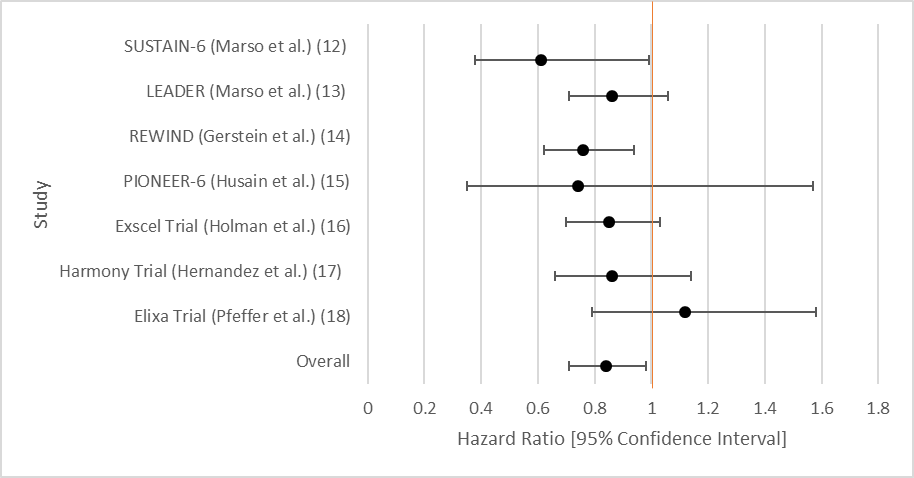
The overall aggregate of studies for GLP-1RA demonstrated statistically significant benefit in preventing stroke, but not SGLT-2 inhibitors. Individually, three of the studies for GLP-1RA showed benefit with respect to stroke reduction while none of the studies for SGLT-2i demonstrated statistical significance.
|
Author |
Study Population |
SGLT-2i Type |
Hazard Ratio [95% Confidence Interval] |
|
VERTIS CV (Cannon et al.) [10] |
8,246 randomly assigned patients with T2DM and atherosclerotic cardiovascular disease. |
Ertugliflozin |
1.06[0.82-1.37] |
|
EMPA-REG (Zinman et al.) [11] |
7, 028 patients with T2DM. |
Empagliflozin |
Fatal or Nonfatal Stroke: 1.18[0.89-1.56] |
|
CANVAS (Neal et al.) [12] |
9,734 participants with T2DM. |
Canagliflozin |
0.87 [0.69-1.09] |
|
DECLARE-TIMI 58 (Wivott et al.) [13] |
17,160 patients with T2DM and had multiple risk factors for atherosclerotic cardiovascular disease or had established atherosclerotic cardiovascular disease |
Dapagliflozin |
1.01[0.84-1.21] |
|
Overall Results |
|
1.03[0.79-1.33] |
|
|
p-value |
|
0.869 |
|
|
|
81.43 |
Table 6: Data Results of Studies Investigating the effect of SGLT-2i on Stroke
|
Author or Trial |
Study Population |
GLP-1RA |
Hazard Ratio [95% Confidence Interval] |
|
SUSTAIN-6 (Marso et al.) [16] |
Randomized, double-blind, placebo-controlled, parallel-group trial; 3,297 patients with T2DM and glycated Hgb 7% or more. Patients were randomized in a 1:1:1:1 ratio to receive either 0.5 mg or 1.0 mg of once-weekly subcutaneous semaglutide or volume-matched placebo. |
Semaglutide |
0.61[0.38-0.99] |
|
LEADER (Marso et al.) [17]
|
9,340 patients randomized who had T2DM (glycated hemoglobin of 7% or higher, N=4,668 liraglutide group, N=4,672 placebo group |
Liraglutide |
0.86 [0.71-1.06] |
|
REWIND (Gerstein et al.) [18] |
9,901 patients at least 50 years with T2DM who had either a previous cardiovascular event or cardiovascular risk factors. |
Dulaglutide |
0.76[0.62-0.94] |
|
PIONEER-6 (Husain et al.) [19] |
3, 183 patients. The mean age of the patients was 66 years; 2695 patients (84.7%) were 50 years of age or older and had cardiovascular or chronic kidney |
Semaglutide |
0.74 [0.35-1.57] |
|
Exscel Trial (Holman et al.) [20] |
14,752 patients with T2DM regardless of previous cardiovascular disease. |
Exenatide |
Total Stroke: 0.85 [0.70-1.03] |
|
Harmony Trial (Hernandez et al.) [21] |
4,731 patients were assigned to receive albiglutide and 4,732 patients to receive placebo. Patient ages were 40 years and older. Underlying conditions included T2DM and cardiovascular disease (at a 1:1 ratio). |
Albiglutide |
0.86 [0.66-1.14] |
|
Elixa Trial (Pfeffer et al.) [22] |
6,068 patients with T2DM who had had a myocardial infarction or who had been hospitalized for unstable angina within the previous 180 days to receive lixisenatide or placebo. |
Lixisenatide |
1.12[0.79-1.58] |
|
Overall Results |
0.84[0.71-0.97] |
||
|
p-value |
0.029 |
||
|
53.91 |
Table 7: Data Results of Studies Investigating the effect of GLP-1RA on Stroke
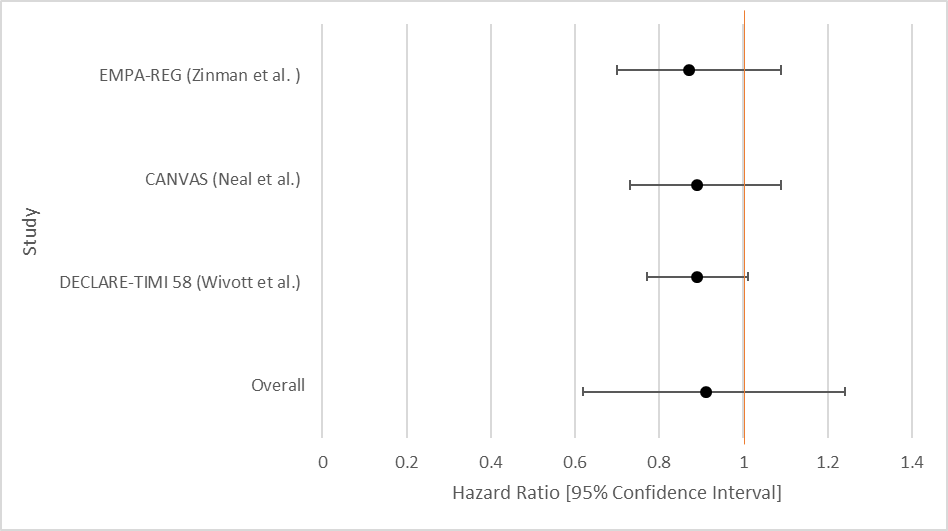
Myocardial Infarction
No statistically significant benefit for either SGLT-2i or GLP-1RA. Individually, none of the studies demonstrated statistical significance for SGLT-2i while only one of the studies for GLP-1RA demonstrated statistical significance.
|
Author |
Study Population |
SGLT-2i Type |
Hazard Ratio [95% Confidence Interval] |
|
EMPA-REG (Zinman et al. ) [11]
|
7, 028 patients with T2DM |
Empagliflozin |
0.87 [0.70-1.09] |
|
CANVAS (Neal et al.) [12] |
9,734 participants with T2DM |
Canagliflozin |
0.89 [0.73-1.09] |
|
DECLARE-TIMI 58 (Wivott et al.) [13] |
17,160 patients with T2DM and had multiple risk factors for atherosclerotic cardiovascular disease or had established atherosclerotic cardiovascular disease. |
Dapagliflozin |
0.89 [0.77-1.01] |
|
Overall Results |
0.90[0.65-1.21] |
||
|
p-value |
0.213 |
||
|
90 |
Table 8: Data Results of Studies Investigating the effect of SGLT-2i on Myocardial Infarction
|
Author or Trial |
Study Population |
GLP-1RA |
Hazard Ratio [95% Confidence Interval] |
|
Marso et al. [16] |
3,297 patients with T2DM and glycated Hgb 7% or more. |
Semaglutide |
Nonfatal: 0.74 [0.51-1.08] |
|
Marso et al. [17] |
9,340 patients randomized who had T2DM |
Liraglutide |
0.86 [0.73-1.00] |
|
REWIND (Gerstein et al.) [18] |
Randomized, double-blind, placebo-controlled trial. 9,901 Men and women aged at least 50 years with T2DM who had either a previous cardiovascular event or cardiovascular risk factors were randomly assigned (1:1) to either weekly subcutaneous injection of dulaglutide (1.5 mg) or placebo. |
Dulaglutide |
0.96[0.79-1.15] |
|
PIONEER-6 (Husain et al.) [19] |
3183 patients were randomly assigned to receive oral semaglutide or placebo. The mean age of the patients was 66 years; 2695 patients (84.7%) were 50 years of age or older and had cardiovascular or chronic kidney disease. |
Semaglutide |
1.18 [0.73-1.90] |
|
Exscel Trial (Holman et al.) [20] |
14,752 patients with T2DM were randomly assigned, with or without previous cardiovascular disease, to receive subcutaneous injections of extended-release exenatide at a dose of 2 mg or matching placebo once weekly. Patients were followed for a median of 3.2 years (interquartile range, 2.2 to 4.4). |
Exenatide |
0.97 [0.85-1.10] |
|
Harmony Trial (Hernandez et al.) [21] |
Total: 9,463 patients. Double-blind, randomized, placebo-controlled trial: 4731 patients were assigned to receive albiglutide and 4732 patients to receive placebo; patient ages 40 years and older with T2DM and cardiovascular disease (at a 1:1 ratio) to groups that either received a subcutaneous injection of albiglutide (30-50 mg, based on glycemic response and tolerability) or of a matched volume of placebo once a week, in addition to their standard care. |
Albiglutide |
0.75 [0.61-0.90] |
|
Elixa Trial (Pfeffer et al.) [22] |
6,068 patients with T2DM who had had a myocardial infarction or who had been hospitalized for unstable angina within the previous 180 days to receive lixisenatide or placebo |
Lixisenatide |
1.03[0.87-1.22] |
|
Overall Results |
0.92 [0.79- 1.05] |
||
|
p-value |
0.147 |
||
|
70.08 |
Table 9: Data Results of Studies Investigating the effect of GLP-1RA on Myocardial Infarction
Heart Failure Symptoms
|
Author |
Study Population |
SGLT-2i Type |
Change in HF symptoms |
|
Ingelheim et al. [29] |
315 participants with T2DM |
Empagliflozin |
Exercise Capacity score was 299.5 for placebo vs 297.0 for Empagliflozin group |
|
Abraham et al. [30] |
HF patients with and without T2DM |
Empagliflozin |
+2.7% in 6MWTD (Dyspnea Score) |
|
Nunez et al. [31] |
Nineteen patients with T2DM and symptomatic HF |
Empagliflozin |
+11.1% in peak VO21 |
Table 10: Data Results of Studies Investigating the effect of SGLT-2i on HF Symptoms
Discussion
This meta-analysis of the current landmark trial data regarding the utility of SGLT-2i and GLP-1RA explored the efficacy of both anti-hyperglycemic medications in reduction of cardiovascular conditions and symptoms while also exploring differences between the two medication classes. Our findings are consistent with other published studies and confirm the various cardioprotective effects of these medications. Moreover, in this analysis we studied varying efficacies of different medications in either of the drug class in preventing MACE (major adverse cardiovascular events), heart failure hospitalizations, atrial fibrillation, stroke, and myocardial infarction. Additionally, this analysis studied the ability of both medications in either drug class in improving heart failure symptoms.
This study had two major findings: both medication classes help prevent major cardiovascular events (MACE) and that patient underlying conditions should not necessarily guide which class of medication to choose.
Regarding MACE, analysis of the above trials of SGLT-2i and GLP-1RA clearly demonstrated that both anti-hyperglycemics had a statistically significant reduction in the incidence of major adverse cardiovascular events. A similar magnitude of reduction in MACE has been noticed in previously published studies comparing the two drug class32. This shows that these medications can be of major benefit to patients at risk of major cardiovascular events. Cardiac events are among the leading causes of death. As a result, these results mean that these classes of medications can be among the leading agents in prevention of death overall.
Regarding individual effects, SGLT-2i and GLP-1RA do not appear to have much in the way of preventing individual conditions, with the exception of SGLT-2i with respect to Heart Failure and GLP-1RA with respect to stroke. Furthermore, this means that with regards to atrial fibrillation, stroke, and myocardial infarction, there is no demonstrated improvement in either class of medication.
This suggests that individual conditions should not be the primary focus of these medications. Preventing overall cardiovascular outcomes should be the primary focus of prescribing either SLGT-2 inhibitors or GLP-1RA. If a patient has either heart failure or pre-disposition to stroke, it may be then wise to prescribe SGLT-2i or GLP-1RA agonists, respectively. It also means that more studies on alternative agents in preventing atrial fibrillation, stroke, or myocardial infarction must be purused.
On the topic of heart failure hospitalizations, there was a striking difference noticed in terms of heart failure hospitalization rates with use of SGLT-2i compared with GLP-1RA agonists. This is consistent with results from a large population-based analysis by Patorno et al. in which the initiation of SGLT-2i versus GLP-1RA therapy was associated with an approximately 30% reduction in the risk for the primary HHF outcome in all included patients, regardless of the presence or absence of cardiovascular disease at baseline33. This finding is also consistent with the effects of SGLT2 inhibitors on heart failure hospitalizations in cardiovascular outcome trials and in other real-world comparisons to other antidiabetic drugs34.
Multiple mechanisms have been proposed for cardioprotective effects of SGLT-2i, while mechanism for the cardioprotective effects of GLP-1RA is still relatively unknown. Lopaschuk and Verma proposed that SGLT-2i increase diuresis, decrease blood pressure, and decrease sympathetic response35. This may translate into reduced cardiac afterload and improved ventricular-atrial coupling, possibly explaining why SGLT-2i perform better in reducing heart failure hospitalizations and improving heart failure symptoms 34. Cox et al. demonstrated that GLP-1RA reduce the blood sugar levels and indirectly reduce inflammation or atherosclerotic plaque formation36. Given that atherosclerotic plaque formation and rupture are among the foundational causes of strokes, this can be hypothesized to explain a reduction in stroke events seen in patients on GLP-1RA agnostic therapy.
This meta-analysis includes a diverse number of studies and presents a holistic picture of how SGLT-2i and GLP-1RA perform in the general cardiovascular risk population. This study may be particularly useful for clinicians needing to decide appropriate treatment regimens for patients with diabetes and concurrent cardiovascular symptoms. However, this study still has certain limitations. First, the availability of data on GLP-1RA were limited compared to the data available on SGLT-2 inhibitors, making some comparison computations heterogeneous. Second, the current study suffers from the inherent limitation of meta-analysis that can arise as the positive results might be published more easily than the negative results. Thirdly, there could be other confounding variables present with regards to test subjects. Dietary habits, lifestyle differences, and inherent genetic differences all are factors that are difficult to control for in an randomized controlled trial. Consequently, it is difficult to say that the treatment alone accounts for differences present between treatment and placebo groups. Additionally, the number of trials included in SGLT2 inhibitors treatment and GLP-1RA treatment might not be comparable. Therefore, more complete data must be available in order to create a more thorough meta-analysis.
Conclusions
The data of this meta-analysis suggests that both SGLT-2iand GLP-1RA are important considerations in the medication repertoire for physicians treating patients with diabetes, heart failure, those at risk for a major cardiovascular event, or a combination of these conditions. These meta-analyses demonstrate that both SGLT-2iand GLP-1RA provide statistically significant benefits in a diverse array of cardiovascular conditions. Both classes of anti-hyperglycemics provide protection against major cardiovascular events. With regard to specific conditions, SGLT-2i demonstrate greater benefit in patients with heart failure, while GLP-1RA demonstrate greater benefit in patients at risk for a stroke.
Statements and Declarations
Declarations
Ethics approval and consent to participate:
Not applicable
Consent for Publication
Not Applicable
Availability of Data and Materials
All data generated or analyzed during this study are included in this published article.
Competing Interests
The authors declare that they have no competing interests.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Authors’ Contributions
- AJ obtained, analyzed, and interpreted the data. AJ participated in the statistical analysis. AJ was a major contributor to writing the manuscript.
- KH obtained, analyzed, and interpreted the data. KH participated in the statistical analysis. KH was a major contributor to writing the manuscript.
- TA obtained, analyzed, and interpreted the data. TA participated in the statistical analysis. TA was a major contributor to writing the manuscript.
- LLN obtained, analyzed, and interpreted the data. LLN participated in the statistical analysis. LLN was a major contributor to writing the manuscript.
- TK obtained, analyzed, and interpreted the data. TK participated in the statistical analysis. TK was a major contributor to writing the manuscript.
- All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
References
- Vallon V. The mechanisms and therapeutic potential of SGLT2 inhibitors in diabetes mellitus. Annu Rev Med 66 (2014): 255-270.
- Drucker DJ. Mechanisms of Action and Therapeutic Application of Glucagon-like Peptide-1. Cell Metab 27 (2018):740-756.
- S. Food and Drug Administration (2020) FDA approves new treatment for a type of heart failure [Press release]. https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-type-heart-failure. Date Accessed: 01 April 2023
- FDA grants dulaglutide CV indication for diabetes with or without established CVD. [Press release]. https://www.healio.com/news/endocrinology/20200224/fda-grants-dulaglutide-cv-indication-for-diabetes-with-or-without-established-cvd. Date Accessed: 01 April 2023
- Galman A, Carlin JB, Stern H, Dunson D, Vehtari A, Rubin D (2014). Bayesian Data Anal. Third Edition. Boca Raton, FL: Chapman; Hall/CRC Press, pp 372.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clinl Trials 7 (1986): 177-188.
- De Bragança P, Alberto C, Stern JM. Evidence and Credibility: Full Bayesian Significance Test for Precise Hypotheses. Entropy 1 (1999): 99-110.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 21 (2022): 1539-1558.
- Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink, et al. CREDENCE Trial Investigators Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N Engl J Med 380 (2019): 2295-2306.
- Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, VERTIS CV Investigators, et al. Ertugliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 383 (2020):1425-1435.
- Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med 373 (2015): 2117-2128.
- Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med 377 (2017): 644-657.
- Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 380 (2019): 347-357.
- Bhatt DL, Szarek M, Pitt B, Cannon C P, Leiter LA, McGuire DK, et al. Sotagliflozin in Patients with Diabetes and Chronic Kidney Disease. N Engl J Med 384 (2021): 129-139.
- Bhatt DL, Szarek M, Steg PG, Cannon CP, Leiter LA, et al. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. N Engl J Med 384 (2021): 117-128.
- Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 375 (2016): 1834-1844.
- Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 375 (2016): 311-322.
- Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet 394 (2019): 121-130.
- Husain M, Birkenfeld AL, Donsmark M, Dungan K, Eliaschewitz FG, et al. Oral Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 381 (2019): 841-851.
- Holman RR, Bethel MA, Mentz RJ, Thompson VP, Lokhnygina Y, et al. Effects of Once-Weekly Exenatide on Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 377 (2017): 1228-1239.
- Hernandez AF, Green JB, Janmohamed S, D'Agostino RB Sr, Granger CB, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet 392 (2018): 1519-1529.
- Pfeffer M, Claggett B, Diaz R, Dickstein K, Gerstein H, Kober L, Lawson F, Ping L, Wei X, Lewis E, Maggioni A, McMurray, J (2015) Lixisenatide In Patients with Type 2 Diabetes and Acute Coronary Syndrome. N Engl J Med 373: 2247-2257.
- McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med 381 (2019): 1995-2008.
- Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med 385 (2019): 1451-1461.
- Packer M, Anker SD, Butler J, Filippatos G, Pocock SJ, et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N Engl J Med 383 (2020): 1413-1424.
- Zelniker TA, Bonaca MP, Furtado RHM, Mosenzon O, Kuder JF, et al. Effect of Dapagliflozin on Atrial Fibrillation in Patients With Type 2 Diabetes Mellitus: Insights From the DECLARE-TIMI 58 Trial. Circulation 141 (2020): 1227-1234.
- Usman MS, Siddiqi TJ, Memon MM, Khan MS, Rawasia WF, Talha Ayub M, Sreenivasan J, Golzar, Y. Sodium-glucose co-transporter 2 inhibitors and cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol 25 (2018): 495-502.
- Patoulias D, Toumpourleka M, Papadopoulos C, Doumas M. Meta-analysis evaluating the risk of atrial fibrillation with newer antidiabetics across the cardiovascular and renal outcome trials. Am J Cardiol 139 (2021): 139-141.
- Ingelheim B (2020) This Study Tests Emagliflozin in Patients with Chronic Heart Failure with Preserved Ecjection Fraction (HFpEF). The Study Looks at How Far Patients Can Walk in 6 Minutes and at Their Heart Failure Symptoms. Retrieved from: https://clinicaltrials.gov/ct2/show/NCT03448406. Date Accessed: 01 April 2023
- Abraham WT, Lindenfeld J, Ponikowski P, Agostoni P, Butler J, Desai AS, et al. Effect of empagliflozin on exercise ability and symptoms in heart failure patients with reduced and preserved ejection fraction, with and without type 2 diabetes. Eur Heart J 42 (2021): 700-710.
- Núñez J, Palau P, Domínguez E, Mollar A, Núñez E, Ramón JM, Miñana G, Santas E, Fácila L, Górriz JL, Sanchis J, Bayés-Genís A. Early effects of empagliflozin on exercise tolerance in patients with heart failure: A pilot study. Clin Cardiol 41 (2018): 476-480.
- Giugliano D, Scappaticcio L, Longo M, Bellastella G, Esposito K. GLP-1RA receptor agonists vs. SGLT-2 inhibitors: the gap seems to be leveling off. diabetol 20 (2021): 205.
- Patorno E, Htoo PT, Glynn RJ, Schneeweiss S, Wexler DJ, et al. Sodium-Glucose Cotransporter-2 Inhibitors Versus Glucagon-like Peptide-1 Receptor Agonists and the Risk for Cardiovascular Outcomes in Routine Care Patients With Diabetes Across Categories of Cardiovascular Disease. Ann Intern Med 174 (2021): 1528-1541.
- Patorno E, Goldfine AB, Schneeweiss S, Everett BM, Glynn RJ, Liu J, Kim SC. Cardiovascular outcomes associated with canagliflozin versus other non-gliflozin antidiabetic drugs: population based cohort study. BMJ 360 (2018): 119.
- Lopaschuk GD, Verma S. Mechanisms of Cardiovascular Benefits of Sodium Glucose Co-Transporter 2 (SGLT2) Inhibitors: A State-of-the-Art Review. J Am Coll Cardiol. Basic to translational science 5 (2020): 632-644.
- Cox E, Alicic R, Neumiller J, Tuttle K. Clinical Evidence and Proposed Mechanisms for Cardiovascular and Kidney Benefits from Glucagon-like Peptide-1 Receptor Agonists. US Endocrinol 16 (2020): 80-87.