Telemedicine-Guided Cardiopulmonary Resuscitation in A COVID-19 Patient Admitted to a Field Hospital
Article Information
Iuri R. Magalhaes MD, Tarso A. D. Accorsi MD, PhD*, Fernando G. Scarpanti MD, Karine De Amicis Lima MSc, PhD, Renata A. Morbeck MR, Carlos H. S. Pedrotti MD, Eduardo Cordioli MD
Telemedicine Department, Hospital Israelita Albert Einstein, Sao Paulo, Brazil
*Corresponding Author: Tarso A. D. Accorsi MD, PhD, Telemedicine Department, Hospital Israelita Albert Einstein, Sao Paulo, Brazil
Received: 21 July 2020; Accepted: 14 August 2020; Published: 02 December 2020
Citation: Iuri R. Magalhaes, Tarso A. D. Accorsi, Fernando G. Scarpanti, Karine De Amicis Lima, Renata A. Morbeck, Carlos H. S. Pedrotti, Eduardo Cordioli. Telemedicine-Guided Cardiopulmonary Resuscitation in A COVID-19 Patient Admitted to a Field Hospital. Archives of Clinical and Medical Case Reports 4 (2020): 1187-1193.
Share at FacebookAbstract
Introduction: Telemedicine offers instrumental support in the COVID-19 pandemic, helping restructure overloaded health systems. However, there exists a paucity of evidence regarding the feasibility and aid offered by telemedical consultation during life-threatening situations.
Narrative: This paper is a case report of a confirmed COVID-19 66-year-old female admitted to a field hospital who evolved with an unstable condition and suffered a cardiac arrest. All data were collected through a retrospective analysis of the medical records and relevant information is presented. General practitioners assisted the patient during cardiac arrest, helped remotely by a cardiologist, who orientated the ACLS (Advanced Cardiovascular Life Support) protocol review.
Discussion: A telemedicine-guided tension pneumothorax diagnosis was made, allowing timely drainage. The patient recovered through spontaneous circulation; post-cardiac arrest management was also remotely guided and there was progressive recovery. This case demonstrates that low-cost and easy-access specialist teleconsultation may be feasible and effective to improve protocol-adherence even in extreme situations and can be expanded in several scenarios.
Keywords
Case Reports; Life Support Care; Heart arrest; Coronavirus Infections
Case Reports articles; Life Support Care articles; Heart arrest articles; Coronavirus Infections articles
Case Reports articles Case Reports Research articles Case Reports review articles Case Reports PubMed articles Case Reports PubMed Central articles Case Reports 2023 articles Case Reports 2024 articles Case Reports Scopus articles Case Reports impact factor journals Case Reports Scopus journals Case Reports PubMed journals Case Reports medical journals Case Reports free journals Case Reports best journals Case Reports top journals Case Reports free medical journals Case Reports famous journals Case Reports Google Scholar indexed journals Life Support Care articles Life Support Care Research articles Life Support Care review articles Life Support Care PubMed articles Life Support Care PubMed Central articles Life Support Care 2023 articles Life Support Care 2024 articles Life Support Care Scopus articles Life Support Care impact factor journals Life Support Care Scopus journals Life Support Care PubMed journals Life Support Care medical journals Life Support Care free journals Life Support Care best journals Life Support Care top journals Life Support Care free medical journals Life Support Care famous journals Life Support Care Google Scholar indexed journals Heart arrest articles Heart arrest Research articles Heart arrest review articles Heart arrest PubMed articles Heart arrest PubMed Central articles Heart arrest 2023 articles Heart arrest 2024 articles Heart arrest Scopus articles Heart arrest impact factor journals Heart arrest Scopus journals Heart arrest PubMed journals Heart arrest medical journals Heart arrest free journals Heart arrest best journals Heart arrest top journals Heart arrest free medical journals Heart arrest famous journals Heart arrest Google Scholar indexed journals Coronavirus Infections articles Coronavirus Infections Research articles Coronavirus Infections review articles Coronavirus Infections PubMed articles Coronavirus Infections PubMed Central articles Coronavirus Infections 2023 articles Coronavirus Infections 2024 articles Coronavirus Infections Scopus articles Coronavirus Infections impact factor journals Coronavirus Infections Scopus journals Coronavirus Infections PubMed journals Coronavirus Infections medical journals Coronavirus Infections free journals Coronavirus Infections best journals Coronavirus Infections top journals Coronavirus Infections free medical journals Coronavirus Infections famous journals Coronavirus Infections Google Scholar indexed journals Cardiovascular articles Cardiovascular Research articles Cardiovascular review articles Cardiovascular PubMed articles Cardiovascular PubMed Central articles Cardiovascular 2023 articles Cardiovascular 2024 articles Cardiovascular Scopus articles Cardiovascular impact factor journals Cardiovascular Scopus journals Cardiovascular PubMed journals Cardiovascular medical journals Cardiovascular free journals Cardiovascular best journals Cardiovascular top journals Cardiovascular free medical journals Cardiovascular famous journals Cardiovascular Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals SARS-COV-2 articles SARS-COV-2 Research articles SARS-COV-2 review articles SARS-COV-2 PubMed articles SARS-COV-2 PubMed Central articles SARS-COV-2 2023 articles SARS-COV-2 2024 articles SARS-COV-2 Scopus articles SARS-COV-2 impact factor journals SARS-COV-2 Scopus journals SARS-COV-2 PubMed journals SARS-COV-2 medical journals SARS-COV-2 free journals SARS-COV-2 best journals SARS-COV-2 top journals SARS-COV-2 free medical journals SARS-COV-2 famous journals SARS-COV-2 Google Scholar indexed journals enterectomy articles enterectomy Research articles enterectomy review articles enterectomy PubMed articles enterectomy PubMed Central articles enterectomy 2023 articles enterectomy 2024 articles enterectomy Scopus articles enterectomy impact factor journals enterectomy Scopus journals enterectomy PubMed journals enterectomy medical journals enterectomy free journals enterectomy best journals enterectomy top journals enterectomy free medical journals enterectomy famous journals enterectomy Google Scholar indexed journals
Article Details
Abbreviations:
ACLS- Advanced Cardiovascular Life Support; CPR- Cardiopulmonary Resuscitation; PEA- Pulseless Electrical Activity; ROSC- Return of Spontaneous Circulation
1. Introduction
The SARS-COV-2 pandemic exposed the fragility of global health systems, and a lack of resources to meet progressive patients’ demand [1,2]. Field hospitals have been established to support the overloaded system, and the medical staff is predominantly composed of volunteer general practitioners [3]. COVID-19 in the severe form presents acute respiratory distress syndrome and other possible complications, such as thromboembolic events, acute kidney injury, liver damage, shock and severe arrhythmias [4, 5]. Cardiac arrest may occur in multiple situations and may challenge professionals who are not used to dealing with critically ill patients [6]. In this complex context, telemedicine holds the potential to excel. Teleconsultation is an efficient method to increase access to specialists and decision support, but the feasibility in life-threatening situations is not sufficiently studied [7].
This is an in-edit case report of telemedicine-guided cardiopulmonary resuscitation in a COVID-19 patient at a field hospital. The local institutional Ethics Committee approved this report. The patient was admitted to Pacaembu Pandemic Field Hospital (Sao Paulo, Brazil) with access to the emergency telemedicine service of Hospital Israelita Albert Einstein (Sao Paulo, Brazil) through a portable system.
Narrative
During the COVID-19 pandemic, a female 66-year-old patient, without known comorbidities, presented cough, myalgia, fatigue and mild dyspnea. On the fifth day of symptoms, due to progressive dyspnea, she sought care for the first time at the emergency department. On admission, she was conscious, normotensive, with pulmonary crackles and desaturation. COVID-19 pneumonia was hypothesized and standard tests were conducted. Initial treatment included ceftriaxone, azithromycin, oseltamivir and supplemental oxygen therapy with an O2 nasal catheter. Immediately after stabilization, she was referred to a field hospital. COVID-19 was confirmed by PCR; the lab tests did not indicate a high-risk profile and only antimicrobials and clinical support were maintained.
Two days following admission, the patient remained at the same clinical status on stable oxygen therapy; however, C-reactive protein was still high and biomarkers such as D-dimer and troponin were high (200 mg/L and 337 pg/mL, respectively). Other tests and ECG showed no relevant alterations. The diagnostic suggestion was COVID-19-induced cardiac injury, without clinical or ECG criteria for acute coronary syndrome.
The next day, eighty days after symptoms onset, the patient presented severe respiratory distress and hypotensive septic shock requiring orotracheal intubation and mechanical ventilation. A non-ultrasound-guided central line in the left internal jugular vein was provided for vasoactive drugs’ administration and step-up antibiotics (piperacillin and tazobactan plus teicoplanin). Suddenly, a few hours later, the patient presented cardiopulmonary arrest in pulseless electrical activity (PEA), which was promptly recognized by the nurse assistants. Cardiopulmonary resuscitation (CPR) was immediately started by the local team and cardiologic manual device teleconsultation was accessed by a standby nurse technician following the orders of the leader rescuer. Initially, clinical judgment was evolution of COVID-related hypoxemia and presumed poor prognosis despite resuscitation. The remote cardiologist, after a brief observation of the scenario, first guided the improvement of the efficiency of chest compressions and defined the role of each rescuer. There was a better adaptation to the standard ACLS protocol: adequate compressions and ventilation, proper and timely use of adrenaline and, without specific interventions, the return of spontaneous circulation (ROSC) occurred 14 minutes after collapse, approximately two minutes after the start of the video call. ECG was performed immediately after ROSC and showed sinus rhythm, intermittent first-degree AV-block, right branch block, isolated and paired ventricular extrasystoles and fusion beats.
Local general practitioners suspected acute myocardial infarction and queried about the possibility of fibrinolysis. The cardiologist had remote access to the patient’s medical records details, both clinical evolution and laboratory tests. The ECGs and other image exams were viewed via videocall. The brief data evaluation did not point to evidence for acute ischemic disease, implying the need for an expansion of the investigation. Elevated platon troponin was associated with previous myocardial injury and STEMI was not observed. The interactive discussion did not indicate fibrinolysis. During teleconsulting, the patient had a second episode of cardiac arrest in PEA rhythm. The local team restarted the resuscitation maneuvers with telemedicine monitoring. The remote cardiologist emphasized the need to review possible causes of cardiac arrest according to the protocol established by the Advanced Cardiovascular Life Support (ACLS) (“5H/5T”).
The most common causes of cardiac arrest were considered, including hypoxemia, coronary thrombosis, pulmonary embolism, electrolyte disturbances and pneumothorax. Hypoxemia was ruled out due to adequate saturation performed before cardiac arrest. Myocardial infarction wasn’t the most probable cause since troponin levels were stable, with an absence of acute ischemic changes in ECG. Electrolytes such as potassium and arterial blood gases were observed to be normal. Pneumothorax was suggested as the main hypothesis after a new non ultrasound-guided central line in the jugular vein. A new clinical and lung point-of-care ultrasound assessment was requested. Thus, the non-checked chest radiography performed minutes before cardiac arrest was evaluated (Figure 1). The presence of pneumothorax in the left lung was identified, with a deviation of the mediastinum to the right side and lowering the left cupula of the diaphragm. The right lung showed COVID-19 alterations. Cardiac arrest diagnosis was done, and a potentially reversible cause was in progress: tension pneumothorax. High-quality CPR has been performed and one dose of epinephrine administered. Thoracic drainage was performed with pleural puncture, and the patient returned to spontaneous circulation after 2 minutes.
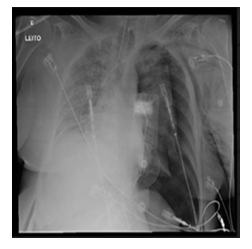
Figure 1: Chest radiography minutes before first cardiac arrest; left pneumothorax and mediastinal deviation.
The cardiologist oriented to perform a point-of-care echocardiogram. The left ventricle had diffuse hypokinesis. There were no changes in the right ventricle or evidence of pulmonary embolism. Another ECG was performed (Figure 2) which indicated second-degree AV-block and right bundle block without ischemic alterations.
’
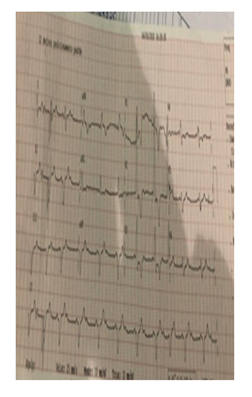
Figure 2: ECG after reversal of second cardiac arrest. Shared via application (WhatsApp) during video call.
The local team followed teleconsultation and management of vasoactive drug dosages, and optimal mechanical ventilation was performed in addition to the joint interpretation of new lab tests. After a brief period of stabilization, the telemedicine consultation concluded and step-by-step guidance was given. The patient remained hospitalized for 7 more days, with progressive recovery and uneventful hospital course.
3. Discussion
Cardiorespiratory arrest is a critical event, prevalent in unstable patients and associated with high morbidity and mortality. Despite standardized treatment, even in certified teams, it is a situation that can create physical and emotional stress that can occur with less adherence to the resuscitation protocol. Low confidence in the self-reporting rescue team during CPR is common, and there is evidence of confidence increase after frequent exposure to this situation. Less experienced doctors have lower confidence and more concern about making mistakes in those moments. Telemedicine allows remote training of the team, facilitating remote consultations with more experienced doctors [6].
The SARS-COV-2 pandemic has created immense stress and rearrangement to the healthcare system worldwide.1 Highly skilled health professionals, used to providing outpatient care, have been relocated for helping in the crescent demand on critically ill SARS-COV-2 patients. Similarly, less experienced professionals are exposed to unexpected contexts. In Brazil, the Education Ministry authorized the untimely graduation of students of Medical, Nursery, Pharmacy and Physiotherapy Faculties for helping to care for these patients [7]. In this setting, public initiatives have built field hospitals, aiming to assist the incoming demand and heterogeneous groups of health professionals are now acting on field [2]. Initially, at these locations, the patient profiles are of low-level complexity. However, clinical deterioration often occurs, such as sepsis, acute myocardial infarction, pulmonary embolism or cardiac arrest [3, 8].
In this case report, an elderly patient without comorbidities was admitted to a pandemic field hospital to support treatment. Unfortunately, she presented complications related to the SARS-COV-2 infection. This patient had high inflammatory markers, elevated troponin and D-dimer, in accordance with the literature definition of high-risk patients [9]. She presented clinical deterioration on the eighth day of symptoms, requiring vasoactive drugs and invasive ventilation, and deteriorating to cardiac arrest. The remote cardiologist, more experienced and qualified in ACLS, was decisive in the steps undertaken. Research suggests that most doctors and nurses are in favor of incorporating a remote medical consultant as a “co-pilot” in the context of a CPR. Being out of the CPR scenario can be an advantage to adding diagnostic possibilities and review protocols [10]. Emergency situations, such as cardiac arrest, are challenging for communication via telemedicine but has proven feasible. A pilot study proposed to monitor the quality of communication between a local doctor and a remote doctor evidenced that video call contact is possible even in critical situations such as sepsis and post-cardiac arrest care. Additionally, the use of video facilitates the understanding of the local team and improves the quality of CPR [11]. In this case report, the video call contact was determinant for the positive outcome.
The leader of a resuscitation team is responsible for conducting and reviewing protocols and requesting interventions. These functions do not require physical contact with the patient. It is not utopian to say that the role of the leader can be performed by a remote doctor [12]. In addition to the telemedicine physician being able to act as a “co-pilot” in a CPR, other technological tools can improve the quality of the provided assistance. A study in a simulation center showed an improvement in the quality of cardiac compressions of health professionals who were trained and received performance feedback via telemedicine [13]. Other devices for measuring the quality of CPR maneuvers can provide real-time feedback necessary to increase the number of effective compressions. The use of telemedicine and technological tools contribute to monitoring and improving the quality of CPR [14]. In the case reported, it was necessary to integrate more than one application to obtain patient data. The ECG, despite being shown by video call, was only completely analyzed when shared via a mobile phone application. It should be noted that efforts need to be made to optimize the quality of the interface and share patient data between the telemedicine physician and the local doctor [15].
Cardiology teleconsultation during cardiac arrest is feasible and may improve outcomes through better adherence to the ACLS protocol. Telemedicine is a low-cost easily usable tool supporting better prognosis of life-threatening situations, especially in situations incurring high costs for the healthcare system, such as the COVID-19 pandemic.
Financial Support
There was no funding source for this work.
Conflicts of Interest
The authors declare they have no conflicts of interest related to the present manuscript.
Authors’ Contributions
Iuri R. Magalhaes, Tarso A. D. Accorsi: Conception, planning, analysis and interpretation of data; Iuri R. Magalhaes, Fernando G. Scarpanti: Data collection; Carlos H. S. Pedrotti, Tarso A. D. Accorsi: Writing of the article or its critical intellectual review; Tarso A. D. Accorsi; Karine De Amicis Lima; Eduardo Cordioli: Responsibility for final approval for publication
References
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed 91 (2020): 157-160.
- Portal da Prefeitura Municipal de São Paulo - Secretaria Especial de Comunicação. Hospital de Campanha do Pacaembu começa a funcionar na próxima semana (2020).
- Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382 (2020): 1708-1720.
- Andersen LW, Holmberg MJ, Berg KM, et al. In-hospital cardiac arrest: A review. JAMA 321 (2019): 1200-1210.
- Kuehn BM. Telemedicine helps cardiologists extend their reach. Circulation 134 (2016): 1189-1191.
- Peltan ID, Poll J, Sorensen J, et al. Clinician perspectives regarding in-hospital cardiac arrest resuscitation: A multicenter survey. Crit Care Med 47 (2019): e190-e197.
- Portal do Ministério da Educação. MEC autoriza formatura antecipada de estudantes de Medicina, Enfermagem, Farmácia e Fisioterapia (2020).
- Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol 75 (2020): 2352-2371.
- Guzik TJ, Mohiddin SA, Dimarco A, et al. COVID-19 and the cardiovascular system: Implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020 cvaa106 (2020).
- Honarmand K, Mepham C, Ainsworth C, et al. Adherence to advanced cardiovascular life support (ACLS) guidelines during in-hospital cardiac arrest is associated with improved outcomes. Resuscitation 129 (2018): 76-81.
- Johnsen E, Bolle SR. To see or not to see--better dispatcher-assisted CPR with video-calls? A qualitative study based on simulated trials. Resuscitation 78 (2008): 320-326.
- Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132 (2015): S444-64.
- Wiech P, Salacinska I, Muster M, et al. Use of selected telemedicine tools in monitoring quality of in-hospital cardiopulmonary resuscitation: A prospective observational pilot simulation study. Med Sci Monit 25 (2019): 2520-2526.
- Lin YY, Chiang WC, Hsieh MJ, et al. Quality of audio-assisted versus video-assisted dispatcher-instructed bystander cardiopulmonary resuscitation (): A systematic review and meta-analysis. Resuscitation 123 (2018): 77-85.
- Giordano V, Koch H, Godoy-Santos A, et al. WhatsApp messenger as an adjunctive tool for telemedicine: An overview. Interact J Med Res 6 (2017): e11.
