Syncope in Acute Pulmonary Embolism. Importance of Early Recognition of Recurrent Syncope as a Manifestation of Acute Bilateral Pulmonary Embolism
Article Information
Khalid Sawalha MD1*, Bryan Huang MD1, Shoaib Khan MD1, Naveed Younis MD2
1Division of Internal Medicine, White River Health System, Batesville, Arkansas, USA
2Division of Cardiology, White River Health Systems, Batesville, Arkansas, USA
*Corresponding Author: Khalid Sawalha, MD, Division of Internal Medicine, White River Health System, Batesville, Arkansas, USA
Received: 30 January 2021; Accepted: 16 February 2021; Published: 08 March 2021
Citation: Khalid Sawalha, Bryan Huang, Shoaib Khan, Naveed Younis. Syncope in Acute Pulmonary Embolism. Importance of Early Recognition of Recurrent Syncope as a Manifestation of Acute Bilateral Pulmonary Embolism. Archives of Clinical and Medical Case Reports 5 (2021): 256-260.
Share at FacebookAbstract
A 43-year-old female patient with past medical history of superficial DVTs, nicotine dependency, and morbid obesity presented with shortness of breath and syncope. She was found to be tachycardic with elevated D-Dimer. Emergent chest-CT was performed which revealed large bilateral pulmonary emboli. As her vitals were within normal limits at that time, there were no indications for tissue plasminogen activator. Later, patient started having fleeting episodes of bradycardia and hypotension with drop in systolic pressure over 40mmHg on slight movements. Being in a rural hospital with limited resources, the decision was made to transfer the patient. Following the transfer, the patient was pronounced deceased due to complications related to her condition. We report this case to emphasize the importance of early recognition and management with thrombolytic therapy or mechanical thrombectomy if contraindications exist in patients with recurrent syncope in a rural setting.
Keywords
Bilateral Pulmonary Embolism; Recurrent Syncope
Bilateral Pulmonary Embolism articles; Recurrent Syncope articles
Bilateral Pulmonary Embolism articles Bilateral Pulmonary Embolism Research articles Bilateral Pulmonary Embolism review articles Bilateral Pulmonary Embolism PubMed articles Bilateral Pulmonary Embolism PubMed Central articles Bilateral Pulmonary Embolism 2023 articles Bilateral Pulmonary Embolism 2024 articles Bilateral Pulmonary Embolism Scopus articles Bilateral Pulmonary Embolism impact factor journals Bilateral Pulmonary Embolism Scopus journals Bilateral Pulmonary Embolism PubMed journals Bilateral Pulmonary Embolism medical journals Bilateral Pulmonary Embolism free journals Bilateral Pulmonary Embolism best journals Bilateral Pulmonary Embolism top journals Bilateral Pulmonary Embolism free medical journals Bilateral Pulmonary Embolism famous journals Bilateral Pulmonary Embolism Google Scholar indexed journals Embolism articles Embolism Research articles Embolism review articles Embolism PubMed articles Embolism PubMed Central articles Embolism 2023 articles Embolism 2024 articles Embolism Scopus articles Embolism impact factor journals Embolism Scopus journals Embolism PubMed journals Embolism medical journals Embolism free journals Embolism best journals Embolism top journals Embolism free medical journals Embolism famous journals Embolism Google Scholar indexed journals Recurrent Syncope articles Recurrent Syncope Research articles Recurrent Syncope review articles Recurrent Syncope PubMed articles Recurrent Syncope PubMed Central articles Recurrent Syncope 2023 articles Recurrent Syncope 2024 articles Recurrent Syncope Scopus articles Recurrent Syncope impact factor journals Recurrent Syncope Scopus journals Recurrent Syncope PubMed journals Recurrent Syncope medical journals Recurrent Syncope free journals Recurrent Syncope best journals Recurrent Syncope top journals Recurrent Syncope free medical journals Recurrent Syncope famous journals Recurrent Syncope Google Scholar indexed journals Syncope articles Syncope Research articles Syncope review articles Syncope PubMed articles Syncope PubMed Central articles Syncope 2023 articles Syncope 2024 articles Syncope Scopus articles Syncope impact factor journals Syncope Scopus journals Syncope PubMed journals Syncope medical journals Syncope free journals Syncope best journals Syncope top journals Syncope free medical journals Syncope famous journals Syncope Google Scholar indexed journals tissue articles tissue Research articles tissue review articles tissue PubMed articles tissue PubMed Central articles tissue 2023 articles tissue 2024 articles tissue Scopus articles tissue impact factor journals tissue Scopus journals tissue PubMed journals tissue medical journals tissue free journals tissue best journals tissue top journals tissue free medical journals tissue famous journals tissue Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Leukemia articles Leukemia Research articles Leukemia review articles Leukemia PubMed articles Leukemia PubMed Central articles Leukemia 2023 articles Leukemia 2024 articles Leukemia Scopus articles Leukemia impact factor journals Leukemia Scopus journals Leukemia PubMed journals Leukemia medical journals Leukemia free journals Leukemia best journals Leukemia top journals Leukemia free medical journals Leukemia famous journals Leukemia Google Scholar indexed journals thromboembolism articles thromboembolism Research articles thromboembolism review articles thromboembolism PubMed articles thromboembolism PubMed Central articles thromboembolism 2023 articles thromboembolism 2024 articles thromboembolism Scopus articles thromboembolism impact factor journals thromboembolism Scopus journals thromboembolism PubMed journals thromboembolism medical journals thromboembolism free journals thromboembolism best journals thromboembolism top journals thromboembolism free medical journals thromboembolism famous journals thromboembolism Google Scholar indexed journals
Article Details
1. Introduction
Acute pulmonary embolism (PE) is a form of venous thromboembolism (VTE) that is common and sometimes fatal. The clinical presentation of PE is variable and often nonspecific making the diagnosis challenging. Recurrent syncope is a rare presentation of pulmonary embolism that is estimated to occur in 10% of cases [1]. It can be associated with quick deterioration and poor prognosis. Early recognition of syncope as a mechanism of pulmonary embolism is crucial as the 30-day mortality is significantly higher in these patients [2]. Hence, intervention and early treatment are critical to reduce mortality. We present this case to emphasize the importance of early thrombolytic therapy in patients presenting with syncope-associated pulmonary embolism.
2. Case Presentation
A 43-year-old female initially presented to the emergency department with shortness of breath and syncope. She has a history of superficial DVTs, nicotine dependency, and morbid obesity. On presentation, she was alert and oriented with normal neurological findings. She had an elevated heart rate of over 120 with an oxygen saturation of 90% on 2L NC and was hemodynamically stable. Her labs were significant for leukocytosis, an elevated D-Dimer of 2.85 ug/mL, BNP 17400 pg/mL, and an initial troponin of 0.063ng/mL. An emergent chest-CT was performed which revealed large bilateral pulmonary emboli (Figure 1). The patient was subsequently started on full-dose Lovenox and sent to the progressive care unit for further evaluation and management. Overnight, the patient was noted to have an episode of syncope that was associated with cyanosis, tremors, and diaphoresis. At that time, her blood pressure was stable at 130/80 as she remained mildly lethargic. As the patient did not meet formal indications for systemic tissue plasminogen activator (tPA), she was immediately transferred to the ICU for further evaluation and closer monitoring of her symptoms. During the day, an echocardiogram was performed which revealed a severely dilated right atrium and ventricle with a right ventricular systolic pressure of 66.2 mmHg (Figure 2). The patient had fleeting episodes of bradycardia and hypotension with a noted drop of over 40 mmHg in her systolic pressure on slight movements. Given her rapid decompensation and being in rural setting with limited resources, the patient was immediately transferred to a facility capable of performing intervention catheter-directed thrombolysis for treatment. Following the transfer, the patient was pronounced deceased due to complications related to her condition.
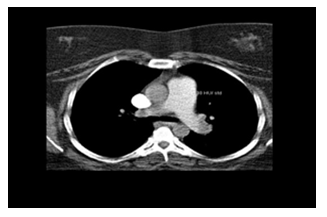
Figure 1: Chest CT revealing bilateral pulmonary embolism in a patient presenting with acute syncope.
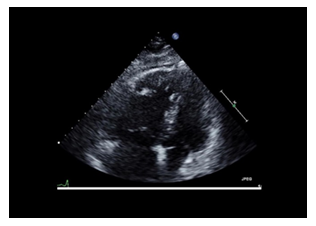
Figure 2: Transthoracic echocardiogram in a patient with acute bilateral pulmonary embolism showing McConnell sign.
3. Discussion
Pulmonary embolus (PE) refers to the obstruction of the pulmonary artery or one of its branches by material such as thrombus, tumor, air, or fat that originated elsewhere in the body. It can be acute, subacute and chronic based on the timeline of its presentation. It is also classified based on the presence or absence of hemodynamic stability, which is associated with right ventricular strain which is also called massive or high-risk PE. PE has a wide variety of presenting features, ranging from no symptoms to shock or sudden death. The most common presenting symptom is dyspnea followed by pleuritic chest pain, cough, and symptoms of deep venous thrombosis such as lower extremity pain, swelling and tenderness. Hemoptysis is an unusual presenting symptom. Rarely do patients present with shock, arrhythmia, or syncope. Diagnosis usually starts with a high index of clinical suspicion along with elevated D-Dimer and imaging includes computed tomographic pulmonary angiography and less commonly, ventilation perfusion scanning or other imaging modalities. For patients who are hemodynamically unstable and in whom definitive imaging is unsafe, bedside echocardiography or venous compression ultrasound may be used to obtain a presumptive diagnosis of PE to justify the administration of potentially life-saving therapies such as TPA.
In this case, the patient presented to a rural hospital with syncope with subsequent testing showing large bilateral pulmonary embolism. Hence, she was started on full dose Lovenox. Despite having normal vital signs and being on anticoagulation, she deteriorated overnight with recurrent episodes of syncope and hypotension manifested by drops in systolic blood pressure to more than 40 mmhg. Due to limited abilities in a rural setting, the decision was made to transfer to a facility capable of catheter directed thrombolysis. Unfortunately, following her transfer she was pronounced dead. Therefore, the distinction between hemodynamically stable and unstable PE is important because patients with hemodynamically unstable PE are more likely to die from obstructive shock as a result of severe right ventricular failure. Syncope associated pulmonary embolism can be fatal and attributed to rapidly decreasing cardiac output if not treated emergently.
4. Conclusion
Syncope-associated pulmonary embolism is a medical emergency that can be associated with poor prognosis and rapid decompensation. With a 90-day mortality rate of 17.4% [3] pulmonary embolism requires heightened clinical suspicion and immediate therapy to prevent fatal pulmonary and cardiac complications. While current guidelines indicate that systemic and catheter-directed thrombolysis are reserved for those with hemodynamic instability, those presenting with recurrent syncope may predict rapid decompensation and may also benefit from early thrombolytic therapy or mechanical thrombectomy if contraindications exist.
Acknowledgement
None.
Summary Conflict of Interest Statements
The Authors have no conflicts of interest to report.
Funding Information
This Manuscript received no fund.
Informed Consent
Verbal Consent was obtained directly from the patient prior to her transfer.
Ethics Approval
Our institution does not require ethical approval for reporting individual cases or case series.
References
- Demircan A, Aygencel G, Keles A, et al. Pulmonary embolism presenting as syncope: a case report. J Med Case Rep 3 (2009): 7440.
- Roncon L, Zuin M, Casazza F, et al. Impact of syncope and pre-syncope on short-term mortality in patients with acute pulmonary embolism. Eur J Intern Med 54 (2018): 27-33.
- Altinsoy B, Erboy F, Tanriverdi H, et al. Syncope as a presentation of acute pulmonary embolism. Therapeutics and clinical risk management 12 (2016): 1023-1028.
