Surgical Management of Solid Pseudopapillary Tumor of the Pancreas - An Observational Study
Article Information
Uddin MS1*, Sobhan SA2, Sakib A3
Department of Hepatobiliary, Pancreatic and Liver Transplantation Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
*Corresponding Author: Dr. Mohammed Saief Uddin, Department of Hepatobiliary, Pancreatic and Liver Transplantation Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Received: 20 May 2023; Accepted: 25 May 2023; Published: 07 June 2023
Citation: Surgical Management of Solid Pseudopapillary Tumor of the Pancreas - An Observational Study
Share at FacebookAbstract
Introduction: Solid pseudopapillary tumors (SPT) of the pancreas are rare neoplasms that predominantly affect young females. This study aimed to investigate the demographic characteristics, clinical presentations, tumor locations, surgical treatments, and outcomes in a cohort of patients with SPT in Bangladesh.
Methods: This retrospective observational study was conducted at the Department of Hepatobiliary, Pancreatic and Liver Transplantation Surgery, Bangabandhu Sheikh Mujib Medical University, Al-Manar Hospital Limited and Abeer General Hospital, Dhaka, Bangladesh. Hospital records of 36 patients with histopathologically confirmed SPT, aged between 18 and 49 years, were included for the study. Data on demographic characteristics, clinical presentations, tumor location, surgical treatment, and outcomes were collected and analyzed using SPSS software V.25.
Result: The majority of patients were in the 18-29 age range (66.67%) and female (86.11%). The most common clinical presentation was abdominal pain or discomfort (44.44%), followed by a palpable abdominal mass (25.00%). Notably, 30.56% of patients were asymptomatic. The most common tumor location was the tail of the pancreas (30.56%). Distal pancreatectomy with splenectomy was the most common surgical treatment (55.56%). Complete tumor resection was achieved in 94.44% of patients, with only 5.56% having residual tumor. Postoperative complications were reported in 13.89% of cases.
Conclusion: This study highlights the demographic and clinical characteristics of patients with SPT in Bangladesh, as well as the surgical management and outcomes. The findings are largely consistent with existing literature, emphasizing the importance of appropriate surgical management and postoperative care for patients with SPT. Further investigation into regional factors that may affect tumor location distribution is warranted.
Keywords
Tumor, Pancreas, Papillary, Pseudopapillary
Tumor articles; Pancreas articles; Papillary articles; Pseudopapillary articles
Tumor articles Tumor Research articles Tumor review articles Tumor PubMed articles Tumor PubMed Central articles Tumor 2023 articles Tumor 2024 articles Tumor Scopus articles Tumor impact factor journals Tumor Scopus journals Tumor PubMed journals Tumor medical journals Tumor free journals Tumor best journals Tumor top journals Tumor free medical journals Tumor famous journals Tumor Google Scholar indexed journals Pancreas articles Pancreas Research articles Pancreas review articles Pancreas PubMed articles Pancreas PubMed Central articles Pancreas 2023 articles Pancreas 2024 articles Pancreas Scopus articles Pancreas impact factor journals Pancreas Scopus journals Pancreas PubMed journals Pancreas medical journals Pancreas free journals Pancreas best journals Pancreas top journals Pancreas free medical journals Pancreas famous journals Pancreas Google Scholar indexed journals Papillary articles Papillary Research articles Papillary review articles Papillary PubMed articles Papillary PubMed Central articles Papillary 2023 articles Papillary 2024 articles Papillary Scopus articles Papillary impact factor journals Papillary Scopus journals Papillary PubMed journals Papillary medical journals Papillary free journals Papillary best journals Papillary top journals Papillary free medical journals Papillary famous journals Papillary Google Scholar indexed journals Pseudopapillary articles Pseudopapillary Research articles Pseudopapillary review articles Pseudopapillary PubMed articles Pseudopapillary PubMed Central articles Pseudopapillary 2023 articles Pseudopapillary 2024 articles Pseudopapillary Scopus articles Pseudopapillary impact factor journals Pseudopapillary Scopus journals Pseudopapillary PubMed journals Pseudopapillary medical journals Pseudopapillary free journals Pseudopapillary best journals Pseudopapillary top journals Pseudopapillary free medical journals Pseudopapillary famous journals Pseudopapillary Google Scholar indexed journals pancreatic neoplasm articles pancreatic neoplasm Research articles pancreatic neoplasm review articles pancreatic neoplasm PubMed articles pancreatic neoplasm PubMed Central articles pancreatic neoplasm 2023 articles pancreatic neoplasm 2024 articles pancreatic neoplasm Scopus articles pancreatic neoplasm impact factor journals pancreatic neoplasm Scopus journals pancreatic neoplasm PubMed journals pancreatic neoplasm medical journals pancreatic neoplasm free journals pancreatic neoplasm best journals pancreatic neoplasm top journals pancreatic neoplasm free medical journals pancreatic neoplasm famous journals pancreatic neoplasm Google Scholar indexed journals pancreatic trauma articles pancreatic trauma Research articles pancreatic trauma review articles pancreatic trauma PubMed articles pancreatic trauma PubMed Central articles pancreatic trauma 2023 articles pancreatic trauma 2024 articles pancreatic trauma Scopus articles pancreatic trauma impact factor journals pancreatic trauma Scopus journals pancreatic trauma PubMed journals pancreatic trauma medical journals pancreatic trauma free journals pancreatic trauma best journals pancreatic trauma top journals pancreatic trauma free medical journals pancreatic trauma famous journals pancreatic trauma Google Scholar indexed journals histopathological diagnoses articles histopathological diagnoses Research articles histopathological diagnoses review articles histopathological diagnoses PubMed articles histopathological diagnoses PubMed Central articles histopathological diagnoses 2023 articles histopathological diagnoses 2024 articles histopathological diagnoses Scopus articles histopathological diagnoses impact factor journals histopathological diagnoses Scopus journals histopathological diagnoses PubMed journals histopathological diagnoses medical journals histopathological diagnoses free journals histopathological diagnoses best journals histopathological diagnoses top journals histopathological diagnoses free medical journals histopathological diagnoses famous journals histopathological diagnoses Google Scholar indexed journals Jaundice articles Jaundice Research articles Jaundice review articles Jaundice PubMed articles Jaundice PubMed Central articles Jaundice 2023 articles Jaundice 2024 articles Jaundice Scopus articles Jaundice impact factor journals Jaundice Scopus journals Jaundice PubMed journals Jaundice medical journals Jaundice free journals Jaundice best journals Jaundice top journals Jaundice free medical journals Jaundice famous journals Jaundice Google Scholar indexed journals Palpable abdominal mass articles Palpable abdominal mass Research articles Palpable abdominal mass review articles Palpable abdominal mass PubMed articles Palpable abdominal mass PubMed Central articles Palpable abdominal mass 2023 articles Palpable abdominal mass 2024 articles Palpable abdominal mass Scopus articles Palpable abdominal mass impact factor journals Palpable abdominal mass Scopus journals Palpable abdominal mass PubMed journals Palpable abdominal mass medical journals Palpable abdominal mass free journals Palpable abdominal mass best journals Palpable abdominal mass top journals Palpable abdominal mass free medical journals Palpable abdominal mass famous journals Palpable abdominal mass Google Scholar indexed journals
Article Details
Introduction
Solid pseudopapillary tumor (SPT) of the pancreas, also known as solid pseudopapillary neoplasm, is a rare and enigmatic pancreatic neoplasm, accounting for approximately 1-2% of all pancreatic tumors [1]. This tumor predominantly affects young women, with a female-to-male ratio of approximately 10:1 [2]. Although the etiology of SPT remains unknown, studies have suggested the involvement of genetic mutations, such as CTNNB1 gene, which encodes the beta-catenin protein [3,4]. Globally, the incidence of SPT has been reported to be increasing, possibly due to the advancements in diagnostic imaging techniques and increased awareness among clinicians [5]. In Bangladesh, the prevalence of SPT is scarce, with only a few case reports published in the literature [6]. However, with a population of over 160 million, the burden of pancreatic tumors in Bangladesh cannot be underestimated. Risk factors and comorbidities associated with SPT have not been well-established, given the rarity of this tumor. Nonetheless, studies have demonstrated a possible association between the development of SPT and a history of pancreatitis or pancreatic trauma [7,8]. Further investigations are required to elucidate potential risk factors that could be contributing to the development of SPT in the Bangladeshi population. SPTs are generally considered to have a low malignant potential, with most cases exhibiting indolent behavior and favorable prognosis [9]. However, metastatic disease and local invasion can occur in a minority of patients, leading to increased morbidity and mortality. The 5-year survival rate for SPT patients is reported to be as high as 97%, with most deaths attributed to tumor recurrence or metastasis [10]. The cornerstone of SPT management is surgical resection, which offers the best chance for long-term survival [11]. The surgical approach depends on the tumor's location, size, and extent of invasion. Complete surgical resection, either by pancreatoduodenectomy or distal pancreatectomy, is the treatment of choice, and it is associated with excellent long-term outcomes [12,13]. However, in cases of unresectable or metastatic disease, chemotherapy and radiation therapy may be employed as palliative measures [14]. In Bangladesh, the healthcare system faces significant challenges, including limited resources, inadequate infrastructure, and a shortage of skilled healthcare professionals [15]. (Anwar et al., 2009). As a result, the management of rare and complex diseases like SPT may be compromised. This observational study aims to investigate the surgical management of SPT in Bangladesh, its efficacy, and its impact on patient outcomes. By examining the surgical management of SPT in Bangladesh, this study will contribute valuable insights to the existing literature and help to identify potential areas for improvement in the diagnosis and treatment of this rare pancreatic tumor. Ultimately, this research may lead to better understanding, improved management strategies, and enhanced patient outcomes for those affected by SPT in Bangladesh and beyond.
Methods
This retrospective observational study was conducted at the Department of Department of Hepatobiliary, Pancreatic and Liver Transplantation Surgery of the Bangabandhu Sheikh Mujib Medical University, Al-Manar Hospital Limited and Abeer General Hospital, Dhaka, Bangladesh. The study duration was 7 years, from January 2016 to December 2022. During this period, hospital records of a total of 36 patients with solid pseudopapillary tumors (SPT) of the pancreas were included for the study following inclusion and exclusion criteria. Patients aged between 18 and 49 years, with a histopathologically confirmed diagnosis of SPT, were included in the study. The exclusion criteria comprised patients with other histopathological diagnoses, those who had received prior treatment for SPT, and patients with incomplete medical records. Data on demographic characteristics, clinical presentations, tumor location, surgical treatment, and outcomes were collected from patient records and analyzed. The results were then compared with existing literature to identify trends and discrepancies in the presentation, management, and outcomes of SPT. All collected data was analyzed using SPSS software V.25, and presented in tabular format.
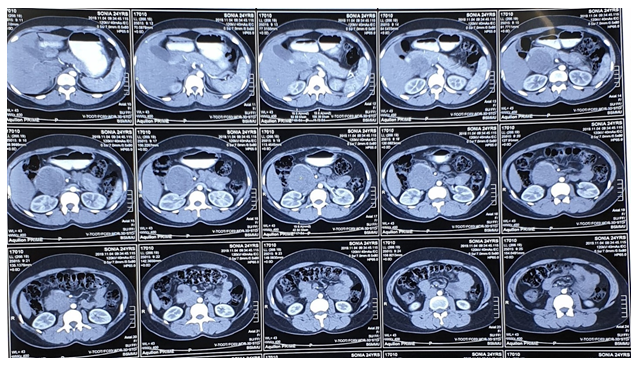
Figure 1: CT scan of a Solid Pseudopapillary Tumor
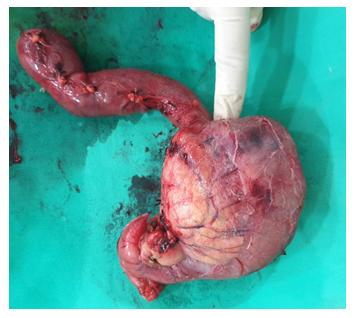
Figure 2: Specimen of a solid pseudopapillary tumor
|
Variables |
Frequency |
Percentage |
|
Age Range |
||
|
18-29 |
24 |
66.67% |
|
30-39 |
8 |
22.22% |
|
40-49 |
4 |
11.11% |
|
Gender |
||
|
Male |
5 |
13.89% |
|
Female |
31 |
86.11% |
Table 1: Distribution of participants by demographic characteristics (N = 36)
A total of 36 patients with solid pseudopapillary tumors (SPT) of the pancreas were included, with the majority (66.67%) falling in the 18-29 age range, followed by 22.22% in the 30-39 age range, and 11.11% in the 40-49 age range.
|
Clinical Presentation |
Frequency |
Percentage |
|
Abdominal pain or discomfort |
16 |
44.44% |
|
Palpable abdominal mass |
9 |
25.00% |
|
Jaundice |
7 |
19.44% |
|
Weight loss |
5 |
13.89% |
|
Asymptomatic |
11 |
30.56% |
Table 2: Distribution of participants by clinical presentations (N = 36)
Abdominal pain or discomfort was the most common symptom (44.44%), followed by a palpable abdominal mass (25.00%), Jaundice (19.44%), and weight loss (13.89%). Notably, 30.56% of patients were asymptomatic, emphasizing the varied clinical manifestations of SPT.
|
Tumor Location |
Frequency |
Percentage |
|
Head |
9 |
25.00% |
|
Uncinated process |
2 |
5.56% |
|
Body |
5 |
13.89% |
|
Tail |
11 |
30.56% |
|
Body and tail |
9 |
25.00% |
Table 3: Distribution of participants by location of tumor (N = 36)
The most common location of the tumor was the tail (30.56%), followed by the head (25.00%) and the body and tail combined (25.00%). Tumors located in the body and the uncinated process represented 13.89% and 5.56% of cases, respectively.
|
Surgical Treatment |
Frequency |
Percentage |
|
Distal pancreatectomy with splenectomy |
20 |
55.56% |
|
Distal pancreatectomy with spleen preservation |
4 |
11.11% |
|
Pancreatoduodenectomy |
9 |
25.00% |
|
Central pancreatectomy |
2 |
5.56% |
|
Laparoscopy with tumor biopsy |
1 |
2.78% |
Table 4: Distribution of participants by type of Surgical treatment (N = 36)
The majority underwent distal pancreatectomy with splenectomy (55.56%), while 11.11% had distal pancreatectomy with spleen preservation. Pancreatoduodenectomy was performed in 25.00% of cases, and central pancreatectomy and laparoscopy with tumor biopsy each accounted for 5.56% & 2.78% respectively of the surgical treatments.
|
Outcome |
Frequency |
Percentage |
|
Complete Tumor Resection |
34 |
94.44% |
|
Residual Tumor |
2 |
5.56% |
|
Post-Operative complications |
5 |
13.89% |
Table 5: Distribution of participants by treatment outcome (N = 36)
The majority of participants, 94.44%, achieved complete tumor resection, indicating successful treatment. Only 5.56% of participants had residual tumor, indicating a need for further treatment. Additionally, 13.89% of participants experienced post-operative complications, highlighting the importance of careful monitoring and management of patients after surgery.
Discussion
In the present study, 36 patients with solid pseudopapillary tumors (SPT) of the pancreas were included, showing a higher prevalence among younger individuals, with 66.67% aged 18-29 years, followed by 22.22% aged 30-39 years, and 11.11% aged 40-49 years. This finding aligns with the existing literature, which indicates that SPT predominantly affects younger individuals [2]. The age distribution observed in this study is also consistent with the findings of Papavramidis and Papavramidis, who reported a similar pattern in their review of 718 cases [1]. Regarding the clinical presentation, abdominal pain or discomfort was the most common symptom (44.44%), followed by a palpable abdominal mass (25.00%), jaundice (19.44%), and weight loss (13.89%). Interestingly, 30.56% of patients were asymptomatic, emphasizing the varied clinical manifestations of SPT. These findings are in line with those reported by Law et al., who conducted a systematic review and found that the majority of patients with SPT presented with abdominal pain or discomfort, followed by a palpable mass, and a significant proportion were asymptomatic [10]. The most common location of the tumor was the tail (30.56%), followed by the head (25.00%) and the body and tail combined (25.00%). Tumors located in the body and the uncinated process represented 13.89% and 5.56% of cases, respectively. The tumor location distribution is somewhat different from the results reported by Yu et al. (2010), who found that the majority of tumors were located in the head of the pancreas [2]. The discrepancies in tumor location distribution may be attributed to differences in sample sizes, patient populations, or regional factors that warrant further investigation. The majority of participants underwent distal pancreatectomy with splenectomy (55.56%), while 11.11% had distal pancreatectomy with spleen preservation. Pancreatoduodenectomy was performed in 25% of cases, and central pancreatectomy and laparoscopy with tumor biopsy each accounted for 5.56% & 2.78% respectively of the surgical treatments. The surgical approach used in the current study is consistent with recommendations in the literature for managing SPT [3]. In terms of surgical outcomes, 94.44% of participants achieved complete tumor resection, indicating successful treatment. This high success rate is consistent with the findings of Estrella et al., who reported a similarly high rate of complete tumor resection in their study. Only 5.56% of participants had residual tumor, indicating a need for further treatment [9]. Additionally, 13.89% of participants experienced post-operative complications, highlighting the importance of careful monitoring and management of patients after surgery. The complication rate observed in this study is comparable to the rates reported by Castro et al., who found that SPT patients experienced a similar range of postoperative complications [16]. In conclusion, the present study's findings are largely consistent with the existing literature on the clinical presentation, tumor location, surgical management, and outcomes of SPT. The discrepancies in tumor location distribution may be attributed to differences in sample sizes, patient populations, or regional factors that warrant further investigation. The high success rate of complete tumor resection and comparable postoperative complication rates underscore the importance of appropriate surgical management and postoperative care for patients with SPT.
Limitations of the study
The study was conducted in a three hospital with a small sample size. So, the results may not represent the whole community.
Conclusion
In conclusion, the present study's findings are largely consistent with the existing literature on the clinical presentation, tumor location, surgical management, and outcomes of SPT. The discrepancies in tumor location distribution may be attributed to differences in sample sizes, patient populations, or regional factors that warrant further investigation. The high success rate of complete tumor resection and comparable postoperative complication rates underscore the importance of appropriate surgical management and postoperative care for patients with SPT.
Funding
No funding sources
Conflict of interest: None declared
References
- Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg 200 (2005): 965-972.
- Yu PF, Hu ZH, Wang XB, et al. Solid pseudopapillary tumor of the pancreas: A review of 553 cases in Chinese literature. World J Gastroenterol 16 (2010): 1209-1214.
- Gao H, Yang J, Pan W, et al. Iron Overload and the Risk of Diabetes in the General Population: Results of the Chinese Health and Nutrition Survey Cohort Study. Diabetes Metab J 46 (2022): 307-318.
- Zhu Y, Xu H, Chen H, et al. Proteomic Analysis of Solid Pseudopapillary Tumor of the Pancreas Reveals Dysfunction of the Endoplasmic Reticulum Protein Processing Pathway*. Molecular & Cellular Proteomics 13 (2014): 2593-2603.
- Vassos N, Agaimy A, Klein P, et al. Solid-pseudopapillary neoplasm (SPN) of the pancreas: case series and literature review on an enigmatic entity. Int J Clin Exp Pathol 6 (2013): 1051-1059.
- Chowdhury MM, Ullah AA, Karim R, et al. Solid Pseudopapillary Tumor of the Pancreas: A Case Report. Mymensingh Med J 28 (2019): 479-483.
- Lahiri R, Bhattacharya S. Pancreatic trauma. Ann R Coll Surg Engl 95 (2013): 241-245.
- Walker AE. The Adult Pancreas in Trauma and Disease. Acad Forensic Pathol 8 (2018): 192-218.
- Estrella JS, Li L, Rashid A, et al. Solid pseudopapillary neoplasm of the pancreas: clinicopathologic and survival analyses of 64 cases from a single institution. Am J Surg Pathol 38 (2014): 147-157.
- Law JK, Ahmed A, Singh VK, et al. A systematic review of solid-pseudopapillary neoplasms: are these rare lesions? Pancreas 43 (2014): 331-337.
- Machado MCC, Machado MAC, Bacchella T, et al. Solid pseudopapillary neoplasm of the pancreas: distinct patterns of onset, diagnosis, and prognosis for male versus female patients. Surgery 143 (2008): 29-34.
- Bachmann J, Michalski CW, Martignoni ME, et al. Pancreatic resection for pancreatic cancer. HPB (Oxford) 8 (2006): 346-351.
- Kim CB, Ahmed S, Hsueh EC. Current surgical management of pancreatic cancer. J Gastrointest Oncol 2 (2011): 126-135.
- Sperti C, Berselli M, Pasquali C, et al. Aggressive behaviour of solid-pseudopapillary tumor of the pancreas in adults: A case report and review of the literature. World J Gastroenterol 14 (2008): 960-965.
- Islam A, Biswas T. Health System in Bangladesh: Challenges and Opportunities. American Journal of Health Research 2 (2014): 366.
- De Castro SMM, Singhal D, Aronson DC, et al. Management of Solid-pseudopapillary Neoplasms of the Pancreas: a Comparison with Standard Pancreatic Neoplasms. World J Surg 31 (2007): 1130-1135.
