Suprapubic Tube Complications Using the Percutaneous Trochar Approach: A Case Series
Article Information
Cynthia Ong1, Minna Blottner1, Sarah C Krzastek1,2, Tyler J Roseman 1,2, Adam P Klausner 1,2*
1Virginia Commonwealth University School of Medicine, Division of Urology/Department of Surgery, Richmond, Virginia
2Central Virginia Veterans Affairs Health System, Division of Urology/Department of Surgery, Richmond, Virginia
*Corresponding Author: Adam P. Klausner, Division of Urology/Department of Surgery, Virginia Commonwealth University School of Medicine, PO BOX 980118, Richmond.
Received: 09 January 2023; Accepted: 20 January 2023; Published: 08 September 2023
Citation: Cynthia Ong, Minna Blottner, Sarah C Krzastek, Tyler J Roseman, Adam P Klausner. Suprapubic Tube Complications Using the Percutaneous Trochar Approach: A Case Series. Archives of Nephrology and Urology 6 (2023): 99-103.
Share at FacebookAbstract
Suprapubic Tube (SPT) catheters are common urinary diversion techniques for long term maintenance of bladder dysfunction. Multiple SPT placement techniques exist, including open, image-guided, or cystoscope-guided, using either a Seldinger or trochar approach. This case series includes six patients (3 males/3 females, average age = 58.2 years) with neurogenic bladder who underwent SPT placement via trochar technique with subsequent complications. Complications were graded using the Clavien-Dindo (CD) classification and included hematuria, catheter malposition or dislodgement, and organ perforation. Key potential risk factors include history of neurogenic bladder, previous chronic indwelling catheter, altered/abnormal urethral or bladder anatomy, concurrent anticoagulant use, obesity, and prior abdominal surgery. While SPT placement has utility in bladder management, placement with trochar techniques can lead to significant complications. Risk factors must be carefully considered in all patient candidates and alternative placement options via an open approach or with imaging guidance should be considered in select patients.
Keywords
Cystostomy, Suprapubic, Neurogenic Bladder,Complications, Peroperative
Cystostomy articles; Suprapubic articles; Neurogenic Bladder articles; Complications articles; Peroperative articles
Cystostomy articles Cystostomy Research articles Cystostomy review articles Cystostomy PubMed articles Cystostomy PubMed Central articles Cystostomy 2023 articles Cystostomy 2024 articles Cystostomy Scopus articles Cystostomy impact factor journals Cystostomy Scopus journals Cystostomy PubMed journals Cystostomy medical journals Cystostomy free journals Cystostomy best journals Cystostomy top journals Cystostomy free medical journals Cystostomy famous journals Cystostomy Google Scholar indexed journals Suprapubic articles Suprapubic Research articles Suprapubic review articles Suprapubic PubMed articles Suprapubic PubMed Central articles Suprapubic 2023 articles Suprapubic 2024 articles Suprapubic Scopus articles Suprapubic impact factor journals Suprapubic Scopus journals Suprapubic PubMed journals Suprapubic medical journals Suprapubic free journals Suprapubic best journals Suprapubic top journals Suprapubic free medical journals Suprapubic famous journals Suprapubic Google Scholar indexed journals Neurogenic Bladder articles Neurogenic Bladder Research articles Neurogenic Bladder review articles Neurogenic Bladder PubMed articles Neurogenic Bladder PubMed Central articles Neurogenic Bladder 2023 articles Neurogenic Bladder 2024 articles Neurogenic Bladder Scopus articles Neurogenic Bladder impact factor journals Neurogenic Bladder Scopus journals Neurogenic Bladder PubMed journals Neurogenic Bladder medical journals Neurogenic Bladder free journals Neurogenic Bladder best journals Neurogenic Bladder top journals Neurogenic Bladder free medical journals Neurogenic Bladder famous journals Neurogenic Bladder Google Scholar indexed journals Complications articles Complications Research articles Complications review articles Complications PubMed articles Complications PubMed Central articles Complications 2023 articles Complications 2024 articles Complications Scopus articles Complications impact factor journals Complications Scopus journals Complications PubMed journals Complications medical journals Complications free journals Complications best journals Complications top journals Complications free medical journals Complications famous journals Complications Google Scholar indexed journals Peroperative articles Peroperative Research articles Peroperative review articles Peroperative PubMed articles Peroperative PubMed Central articles Peroperative 2023 articles Peroperative 2024 articles Peroperative Scopus articles Peroperative impact factor journals Peroperative Scopus journals Peroperative PubMed journals Peroperative medical journals Peroperative free journals Peroperative best journals Peroperative top journals Peroperative free medical journals Peroperative famous journals Peroperative Google Scholar indexed journals Suprapubic Tube articles Suprapubic Tube Research articles Suprapubic Tube review articles Suprapubic Tube PubMed articles Suprapubic Tube PubMed Central articles Suprapubic Tube 2023 articles Suprapubic Tube 2024 articles Suprapubic Tube Scopus articles Suprapubic Tube impact factor journals Suprapubic Tube Scopus journals Suprapubic Tube PubMed journals Suprapubic Tube medical journals Suprapubic Tube free journals Suprapubic Tube best journals Suprapubic Tube top journals Suprapubic Tube free medical journals Suprapubic Tube famous journals Suprapubic Tube Google Scholar indexed journals Clavien-Dindo articles Clavien-Dindo Research articles Clavien-Dindo review articles Clavien-Dindo PubMed articles Clavien-Dindo PubMed Central articles Clavien-Dindo 2023 articles Clavien-Dindo 2024 articles Clavien-Dindo Scopus articles Clavien-Dindo impact factor journals Clavien-Dindo Scopus journals Clavien-Dindo PubMed journals Clavien-Dindo medical journals Clavien-Dindo free journals Clavien-Dindo best journals Clavien-Dindo top journals Clavien-Dindo free medical journals Clavien-Dindo famous journals Clavien-Dindo Google Scholar indexed journals
Article Details
1. Introduction
Suprapubic Tube (SPT) catheters are a common urinary diversion technique, typically placed for long term maintenance of bladder dysfunction. SPTs are often preferred over indwelling urethral catheters because of decreased catheter-related discomfort and pain scores, and decreased risk of erosion with comparable levels of continence and infection.
Though considered relatively benign, SPT placement is known to be associated with numerous complications, including bleeding, surgical site infection, obstruction, and leakage. Early post-procedural complication rates can be as high as 52% within 90 days of placement, though many minor SPT complications can resolve spontaneously with conservative measures [1-5]. However, rare complications including bladder/bowel perforation or urosepsis can result in significant medical intervention requiring reoperation.
One of the more serious complications of SPT placement includes bowel perforation and injury to surrounding structures. Risk factors for this include prior abdominal surgery and prior radiation, but 8% of bowel perforations occurred in patients with no identifiable risk factors [6]. Overall, the mortality rate of the SPT procedure is 1.8% [6], so careful consideration and shared-decision making must take place before the procedure occurs.
While an SPT can be placed in an open fashion, percutaneous tube placement is less invasive and preferred if possible. Multiple percutaneous SPT techniques exist, including image and cystoscope guided or using either a Seldinger or a trochar approach. Our institution primarily utilizes the trochar technique, and the purpose of this paper is to characterize our complications associated with this approach in a case series.
2. Methods
Six patients who had significant complications requiring re-intervention were identified from Morbidity and Mortality conferences between 2020-2021 at two tertiary care medical centers which provide all adult in-patient and out-patient training for an accredited urology residency training program. All procedures were performed using a trochar technique as follows: The patient was placed in Trendelenburg position. An area approximately 2 cm above the pubic symphysis was identified and anesthetized [7,8]. A 5 cm spinal needle was then advanced to confirm return of urine either blindly or using cystoscopic or ultrasound guidance. A 1 cm incision was then created, and an SPT trochar from a commercially available kit (Utah Medical, Midvale, UT) was then advanced into the bladder. The trochar was then removed leaving a peal-away sheath. Once urine return or visual confirmation was confirmed, a 16Fr Foley was placed, the balloon was inflated, the sheath was removed, and the Foley was secured. As SPT placements are performed by multiple providers both on an elective and emergent basis, this study does not provide an exact rate of complications, although our estimation is approximately 5% [9]. Complications were graded using the Clavien-Dindo (CD) classification and presented as a case series.
3. Results / Case Presentations
A total of six patients were identified (3 males/3 females, average age = 58.2 years). All patients had neurogenic bladder dysfunction and chronic urinary retention. CD classifications were Grade I (N=2), II (N=2), III (N=1), and IV (N=1) (Table 1). Complications included gross hematuria (early and recurrent), catheter malposition (early and delayed), catheter dislodgement, and bladder perforation
Table 1: Complications and interventions.
|
Case |
Complication |
Intervention |
CD |
|
1 |
Early Hematuria |
Admission, CBI |
II |
|
2 |
Recurrent Hematuria |
Admission,CBI, transfusions |
II |
|
3 |
Early Malposition |
Return to OR for Replacement |
III |
|
4 |
Delayed Malposition |
SPT Removal |
I |
|
5 |
Dislodgement |
SPT Removal |
I |
|
6 |
Bladder Perforation |
Exploratory Laparotomy |
IV |
|
CD - Clavien-Dindo classification, SPT - Suprapubictube, CBI - continuous bladder irrigation, OR - Operating Room |
|||
Case 1: Early Hematuria
A 74-year-old male with a history of neurogenic bladder due to multiple sclerosis underwent urodynamics which demonstrated detrusor overactivity with impaired contractility and incomplete emptying. The patient elected to undergo SPT placement. Comorbidities included insulin-dependent diabetes and hypertension. The patient had no prior abdominal surgeries and was not on any anticoagulants. SPT placement was performed in the operating room without event, and the patient was discharged the same day. However, upon arrival at home, the patient noted absent SPT drainage and significant bleeding per urethra [10,11]. He presented to the emergency department with a drop in hemoglobin, and bedside catheter irrigation evacuated more than 50 mL of clot. Hematuria persisted, and he was admitted on continuous bladder irrigation. After 24 hours, urine remained clear, continuous irrigation was discontinued, and the hemoglobin level stabilized. The patient was discharged home without any further issues. This patient was given a Grade II CD classification.
Case 2: Recurrent Hematuria
A 67-year-old male with a history of neurogenic bladder secondary to incomplete C4 tetraplegia following a motor vehicle accident was previously maintained on timed voiding and the use of condom catheters. Urodynamics demonstrated a large bladder capacity with poor compliance, high detrusor pressure, and bladder outlet obstruction likely due to detrusor sphincter dyssynergia [12]. Given worsening incontinence and steadily rising creatinine, the patient elected SPT placement. Comorbidities included chronic kidney disease, diabetes, hypertension, peripheral vascular disease, and cerebrovascular accident. The patient had no prior abdominal surgeries but was maintained on anticoagulation. He was taken to the OR (after appropriate discontinuation of anticoagulation) for successful SPT placement and discharged home the same day with instruction to resume anticoagulation after 24 hours. The patient returned to the ED nine days later for gross hematuria with SPT blockage. A new concurrent urethral catheter was placed, and the patient was admitted for continuous bladder irrigation (with anticoagulation held). However, the patient developed multiple episodes of recurrent bleeding and ultimately required transfusion with a total of four units of packed red blood cells [13]. Hematuria resolved, continuous irrigation was eventually discontinued, and the patient was subsequently discharged home with removal of the urethral catheter and maintenance of the SPT for drainage. Over the next 6 months, the patient had two additional episodes of recurrent hematuria requiring emergency department visits with one additional transfusion of a single unit of blood, but not requiring in-patient admission or surgical intervention. This patient was given a Grade II CD classification.
Case 3: Early Malposition
A 57-year-old male with a history of hepatitis C, alcoholic liver cirrhosis, chronic obstructive pulmonary disease and hypertension presented to the emergency department with 12 hours of urinary retention and abdominal discomfort. Despite numerous catheterization attempts by the on-call urology team as well as attempts at cystoscopic bladder access, the bladder could not be decompressed. At this point, the patient underwent an emergent bedside SPT placement. The patient was admitted to the medical service for observation and subsequently underwent a CT scan for continued abdominal discomfort which confirmed malposition of the SPT in the peritoneal cavity (Figure 1). The patient was then taken to the OR urgently where a urethral false passage was identified cystoscopically. A new 16Fr council tip catheter was inserted into the bladder, and the mispositioned SPT was removed [14]. The patient was admitted to the intensive care unit for hypotension. However, over the course of a two-week hospitalization, the patient’s encephalopathy progressed due to decompensated liver failure, and he was placed on palliative care and expired. This patient was given a Grade III CD classification.
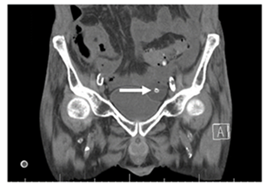
Figure 1: CT image demonstrating malpositioned suprapubic catheter (arrow) in the peritoneal cavity.
Case 4: Delayed Malposition
A 48-year-old female with a history of neurogenic bladder secondary to multiple sclerosis/neuromyelitis was managed with a chronic indwelling Foley. Previous urodynamics demonstrated detrusor acontractility. Cystoscopy noted Foley-induced erosion of the urethra and urethral meatus. Due to increasing leakage, she elected for SPT placement [15]. Comorbidities included diabetes, hypertension, deep vein thrombosis, and pulmonary embolism. Prior abdominal surgeries included only a tubal ligation. Medications were significant for chronic anticoagulant usage. The patient was stable in the recovery unit and was discharged home. She had her first SPT change performed in the out-patient clinic at six weeks and then monthly thereafter. However, after her third exchange, the patient presented to the emergency department with a severe epigastric pain and minimal SPT urine output. CT scan demonstrated the suprapubic catheter misplaced and lodged within the mesentery of the small bowel (Figure 2). The SPT was removed at bedside, and she was admitted to the hospital for IV antibiotics for an associated UTI and subsequently discharged on PO antibiotics. She then underwent subsequently underwent creation of an obstructing pubovaginal sling to help manage the erosion as well as replacement of the SPT. This patient was given a Grade I CD classification.
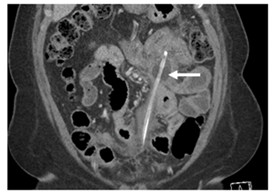
Figure 2: CT image demonstrating malpositioned suprapubic catheter (arrow) in the peritoneal cavity.
CASE 5: Dislodgement
A 65-year-old female with a history of neurogenic bladder following pontine cerebrovascular accident with residual right sided limb weakness was previously managed with a chronic indwelling Foley catheter. Urodynamics demonstrated low bladder capacity with detrusor overactivity incontinence and incomplete bladder emptying. Comorbidities include diabetes, pulmonary embolism, hypertension, and chronic kidney disease. The pahhhhhhtient had no prior abdominal surgeries but was on chronic anticoagulation therapy. The patient was taken to the operating room for SPT placement without difficulty and subsequently discharged the same day [16,17]. The patient returned to office after six weeks for her first SPT exchange without issue. However, one week later, she presented to the emergency department with complaints of clogging of the suprapubic catheter. A 22 Fr SPT was ultimately placed over wire with clear yellow urine output noted. Then, 4 days later, the patient again returned to the emergency department with decreased SPT drainage. A Foley was placed temporarily to provide relief. However, attempts to reestablish the SPT tract were unsuccessful, despite use of a wire and ultrasound guidance. Thus, SPT was removed, and the patient was sent home with a Foley catheter. This patient was given a Grade I CD classification.
Case 6: Bladder Perforation
A 38-year-old female with a history of neurogenic bladder due to C2-C3 incomplete tetraplegia following a gunshot wound was previously managed with a chronic indwelling Foley. SPT placement was recommended due to worsening leakage from bladder neck erosion. Comorbidities included diabetes and hypertension. The patient had no prior abdominal surgeries and was not on any anticoagulants. She was taken to the operating room for SPT placement. Upon insertion of the cystoscope, she was noted to have a patulous urethra and required manual compression of the anterior vaginal wall to achieve bladder distension. Shortly after arrival to the recovery unit, the patient became acutely hypotensive and tachycardic. Ultrasound confirmed significant intra-abdominal fluid, and, due to concerns for intraabdominal bleeding, she was taken back to the operating room for an emergent exploratory laparotomy where the patient had more than 2L of blood evacuated from the peritoneal cavity. The source of bleeding was identified as a perforation in the posterior bladder, which was controlled using absorbable suture. The patient required monitoring in the intensive care unit and continues to have a functioning SPT. This patient was given a Grade IV CD classification.
4. Discussion
Our case series of complications associated with SPT placement via the trochar approach identified several categories including hematuria, catheter malposition, catheter dislodgement, and organ perforation. In addition, several patients required antibiotics for associated UTIs. Key potential risk factors include neurogenic bladder status (seen in all patients) as well as urethral erosion in women which can prevent adequate distention of the bladder at the time of SPT placement. In addition, severe hematuria was seen in association with chronic anticoagulation, and malposition was seen in a patient with cirrhosis and abdominal ascites. Finally, the risk of complications appears to increase in the setting of altered/abnormal urethral anatomy in the setting of obesity or prior abdominal surgery.
Consistent with our series, previous studies show that the timing of complications can vary widely from the immediate postoperative period to months after initial SPT placement. Looking specifically at more severe complications, one patient in our study had a perforated bladder and subsequent hemoperitoneum that required an exploratory-laparotomy, consistent with a known risk of bladder injury. While none of our patients experienced injury to bowel, bowel perforation is also a significant, known complication of SPT placement. One case report found a perforated ileum eight months after initial SPT placement. Another case report described post-op feculent drainage and peritonitis two months after a first SPT exchange in a patient with a history of abdominal surgery. Given rare but serious complication risks, this routine urologic procedure is associated with a mortality rate of 1.8% [6].
Review of these cases identified additional risk factors that may increase risk of complications including history of chronic indwelling catheters, abnormal urethral anatomy, and concurrent anticoagulation. Longstanding Foley catheters pose a unique complication to SPT placement as chronic indwelling catheters can alter urethral anatomy [4]. Subsequent urethral erosion can make it difficult to fully distend the bladder, impeding visualization of placement, which may pose increased risks of bladder perforation as seen in Case 6. Abnormal urethral anatomy may also pose increased difficulty of catheter placement, increasing risk of catheter malposition and the need for removal and replacement, as seen in Case 3. Finally, concurrent anticoagulation use can result in significant hematuria which may require blood transfusions, as evidenced by Case 2.
This study only includes our institution-specific experiences utilizing the trochar SPT placement kit. Other percutaneous techniques, such as the Seldinger technique, were not analyzed. One study of SPT placements found more minor complications associated with the Seldinger technique, but after regression analysis they found that catheter insertion technique, size, and type were not predictors of complications. Based on our series, we now routinely infiltrate the SPT tract with hemostatic agents to provide tamponade and limit bleeding. Further review and comparison of complications associated with percutaneous SPT placement via the Seldinger method is warranted. Additionally, image-guidance including ultrasound or interventional radiology assistance may be necessary in more complex cases of difficult SPT placements.
Despite complications, suprapubic tubes can be significantly beneficial in the management of chronic urinary retention, with improved overall quality of life and patient satisfaction. In one randomized control trial, patients receiving SPT had significantly less postoperative pain compared to those with transurethral catheters following a robot-assisted radical prostatectomy. Another study comparing long term outcomes of SPT demonstrated a 72% satisfaction rate and 89% preference over transurethral catheters [9].
While this study is limited by the small sample size and lack a clear complication rate or comparison to other percutaneous approaches, it provides insight into risk factors of an important and common urologic procedure.
Conclusion
In conclusion, while SPT placement has utility in bladder management, percutaneous placement using a trochar can lead to significant complications and risks factors for complications including altered anatomy, prior surgery, ascites, and anticoagulation use must be carefully considered in all patient candidates. In addition, where possible, alternative placement options with imaging guidance should be considered in select patients.
Acknowledgements
There is no funding associated with the current study.
Conflict of interest
The authors report no conflicts of interest related to the current study
References
- Krane Louis Spencer, Bhandari Mahendra, Peabody James O, Menon Mani. Impact of percutaneous suprapubic tube drainage on patient discomfort after radical prostatectomy. European urology. 56 (2009): 325-330.
- Morgan Monica S C, Ozayar Asim, Friedlander Justin I, Shakir Nabeel, Antonelli Jodi A et al. An assessment of patient comfort and morbidity after robot-assisted radical prostatectomy with suprapubic tube versus urethral catheter drainage. Journal of Endourology. 30 (2016): 300-305.
- Galfano Antonio, Secco Silvia, Panarello Daniele, Barbieri Michele, Di Trapani Dario et al. Pain and discomfort after Retzius-sparing robot-assisted radical prostatectomy: a comparative study between suprapubic cystostomy and urethral catheter as urinary drainage. Minerva Urology Nephrology. 71 (2019): 381-385.
- Katsumi H K, Kalisaart J F, Ronningen L D, Hovey R M. Urethral versus suprapubic catheter: choosing the best bladder management for male spinal cord injury patients with indwelling catheters. Spinal Cord. 48 (2010): 325-329.
- Rabinowitz Matthew J, Haney Nora M, Myers Amanda A, Dora Chandler D, Pavlovich Christian P. Urinary outcomes after MRI-guided whole-gland transurethral ultrasound ablation for prostate cancer: comparison of suprapubic tube to indwelling urethral catheter. Journal of Endourology, online. 2022.
- Tompkins Andrew J, Travis Michelle, Wayne Reed E, Lasser Michael, Ellsworth Pamela. Decreasing suprapubic tube-related injuries: results of case series and comprehensive literature review. Urol Nursing. 34 (2014): 9-17
- Ginger Van Anh T, Miller Jane L, Yang Claire C. Bladder neck closure and surapubic tube placement in a debilitated patient population. Neurourology Urodynamics. 29 (2010): 382-386.
- Sorokin Igor, De Elise. Options for independent bladder management in patients with spinal cord injury and hand function in prohibiting intermittent catheterization. Neurourology Urodynamics. 34 (2015): 167-176.
- Dindo Daniel, Demartines Nicolas, Clavien Pierre-Alain. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240 (2004): 205-213.
- Ahluwalia RS, Johal N, Kouriefs C, Kooiman G, Montgomery Bruce SI et al. The surgical risk of suprapubic catheter insertion and long-term sequelae. Ann R Coll Surg Engl. 88 (2006): 210-213.
- Parry Neil G, Rozycki Grace S, Feliciano David V, Tremblay Lorraine N, Cava Raymond A, et al. Traumatic rupture of the urinary bladder: is the suprapubic tube necessary? J Trauma. 54 (2004): 431-436.
- Hall S, Ahmed S, Reid S, Thiruchelvam N, Sahai A, et al. A national UK audit of suprapubic catheter insertion practice and rate of bowel injury with comparison to a systematic review and meta-analysis of available research. Neurourology Urodynamics. 38 (2019): 2194-2199.
- Mongiu Anne K, Helfand Brain T, Kielb Stephanie J. Small bowel perforation during suprapubic tube exchange. Canadian Journal of Urology. 16 (2009): 4519-4521.
- Ahmed Shwan J, Mehta Ajay, Rimington Peter. Delayed bowel perforation following suprapubic catheter insertion. BMC Urol. 4 (2004):16.
- Cronin Carmel G, Prakash Priyanka, Gervais Debra A, Hahn Peter F, Arellano Ronald, et al. Imaging-guided suprapubic bladder tube insertion: experience in the care of 549 patients. AJR. 196 (2011): 182-188.
- Mond D J, Lee W J. Fluoroscopically guided suprapubic cystostomy in complex urologic cases. J Vasc Interv Radiol. 5 (1994): 911-914.
- Harke Nina, Godes Michael, Habibzada Jawid, Urbanova Katarina, Wagner Christian, Zecha Henrik, et al. Postoperative patient comfort in suprapbuic drainage versus transurethral catheterization following robot-assisted radical prostatectomy: a prospective randomized clinical trial. World Journal of Urology. 35 (2017): 389-394.
