Successful Resolution of Subfoveal Hemorrhage with Subretinal delivery of Aflibercept in AMD and Idiopathic Polypoidal Choroidal Vasculopathy- A Case Series
Article Information
Kinza T. Ahmad MD, Suzie A. Gasparian MD, K.V. Chalam MD, PhD*
Department of Ophthalmology, Loma Linda University, Loma Linda, California, USA
*Corresponding Author: K.V. Chalam, MD, PhD, Department of Ophthalmology, Loma Linda University College of Medicine, 11370 Anderson St., Suite 1800, Loma Linda, CA 92354, USA
Received: 11 October 2023; Accepted: 23 November 2023; Published: 22 December 2023
Citation: Kinza T. Ahmad, Suzie A. Gasparian, K.V. Chalam. Successful Resolution of Subfoveal Hemorrhage with Subretinal delivery of Aflibercept in AMD and Idiopathic Polypoidal Choroidal Vasculopathy- A Case Series. Archives of Clinical and Medical Case Reports. 7 (2023): 428-432.
Share at FacebookAbstract
Introduction: Submacular hemorrhage due to IPCV is visually debilitating for patients and different methods are utilized in management of this sight-threatening complication with limited success. In this expanded case series, we describe the visual outcomes of submacular hemorrhage secondary to IPCV treated with subretinal delivery of aflibercept during pars plana vitrectomy (PPV).
Methods: In this retrospective review, we report the clinical, surgical, and multimodal imaging data of four eyes of four patients who underwent surgery for submacular hemorrhage due to IPCV at Loma Linda University Hospital. Each eye underwent standard 23-gauge PPV and subretinal delivery of 2 mg aflibercept with a 25 g/42 g cannula coupled to the viscous fluid control unit of a standard vitrectomy system. Results: All patients had resolution of the submacular hemorrhage with improvement in visual acuity.
Conclusion: Our series describes a group of cases with successful resolution of subfoveal hemorrhage and improvement in VA using a novel technique of subretinal aflibercept delivery for the treatment of subretinal bleeding in IPCV.
Keywords
Idiopathic Polypoidal Choroidal Vasculopathy (IPCV); Aflibercept; subretinal hemorrhage; subretinal injection
Idiopathic Polypoidal Choroidal Vasculopathy (IPCV) articles; Aflibercept articles; subretinal hemorrhage articles; subretinal injection articles
Article Details
1. Introduction
Idiopathic polypoidal choroidal vasculopathy (IPCV) is a disease of the choroidal vasculature that often leads to an exudative and hemorrhagic macular degeneration secondary to dysfunctional poylps [1]. It is a distinct entity from age-related macular degeneration and is one of the leading causes of subretinal hemorrhage [2]. Submacular hemorrhage due to IPCV is visually debilitating for patients and different methods are utilized in management of this sight-threatening complication with limited success. Previous studies have reported pneumatic displacement [3], pneumatic displacement with intravitreal tissue plasminogen activator (TPA) [4], pars plana vitrectomy (PPV) with subretinal TPA and air [5], PPV with subretinal TPA and gas [6], and PPV with subretinal bevacizumab+TPA and gas [7], all with varying success rates. Recently, we described a novel technique of subretinal delivery of aflibercept during parsplana vitrectomy for the treatment of submacular hemorrhage in IPCV [8].
In this case series, we report successful surgical outcomes after subretinal delivery of aflibercept in 4 patients (4 eyes) with IPCV and validate the safety and efficacy of this technique for the treatment of submacular hemorrhage.
2. Case Presentations
This was a retrospective review of the clinical, surgical, and imaging data of four eyes of four patients who underwent surgery for submacular hemorrhage due to IPCV at Loma Linda University Hospital. Each eye underwent standard 23-gauge PPV, and 2 mg of aflibercept was delivered into the subretinal space using a 25 g/42 g cannula coupled to the viscous fluid control unit of a standard vitrectomy system. The details of the surgical technique utilized for these 4 cases have been described previously [8]. All vitrectomies were performed by a single surgeon (KVC). The eyes were evaluated at various time points using multimodal imaging (optical coherence tomography [OCT] and retinal angiography).
2.1 Case 1
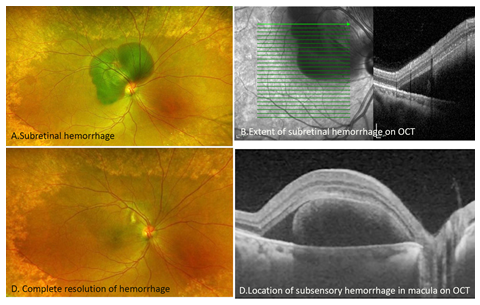
A 55 -year-old Hispanic woman presented to the medical retina clinic with a 5-day history of decreased vision in the right eye and an accompanying headache. At initial presentation, her best-corrected visual acuity (BCVA) was 20/200 in the right eye and 20/25 in the left eye. Fundus examination revealed submacular hemorrhage splitting fixation with an umbo of subretinal fluid (SRF) in the right eye (Figure 1a). OCT showed a submacular hemorrhage with a double hump sign associated with multilocular PED (Figure 1b, d). The FA/ICG of the right eye showed blockage in the superior macula and peripapillary area, corresponding to subretinal hemorrhage. The left eye showed a branching vascular network (BVN) in the nasal macula, without focal plaques or hot spots, and no polyps. The patient underwent 23-gauge PPV with a subretinal injection of 2 mg aflibercept. At the 1 month visit there was complete resolution of the hemorrhage with residual exudation in the area of the prior hemorrhage (Figure 1c, d). Fifteen months after surgery, BCVA improved to 20/50.
Figure 1: Preoperative color fundus photograph (A) and OCT imaging (B and D) showing subretinal hemorrhage splitting fixation with a notched PED and double hump sign characteristic of IPCV. (C) Color fundus photograph of the right eye 6 months postoperatively showing the resolution of the subretinal hemorrhage.
2.2 Case 2
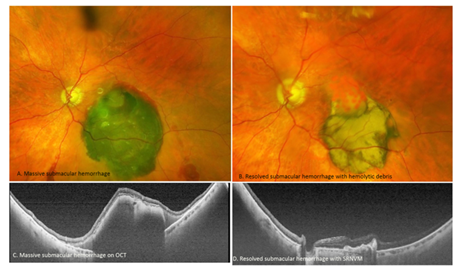
A 79-year-old white man presented to the medical retina clinic with a sudden decrease in vision in his left eye three weeks prior to presentation. On examination, the BCVA was 20/20 in the right eye and 20/400 in the left eye. Anterior segment evaluation revealed PCIOL in both eyes. On fundus examination, a few hard and soft drusen without pigment or atrophy were noted in OD, and a large submacular hemorrhage extending beneath the inferotemporal arcade was noted in OS (Figure 2a). OCT revealed a few drusen and an ERM in the right eye, with submacular and sub-RPE hemorrhages in the left eye (Figure 2c). The patient underwent 23-gauge PPV with a subretinal injection of 2 mg aflibercept the following day. At the 1-month postoperative visit, color fundus photographs showed improvement in the submacular hemorrhage, with settling of dehemoglobinized blood inferiorly in the left eye, and BCVA improved to 20/60 (Figure 2b, d).
Figure 2: (A) Color fundus photograph of the left eye preoperatively demonstrating a large submacular hemorrhage extending inferiorly. (C) Corresponding OCT showing a notched PED with submacular hemorrhage characteristic of IPCV. (B) Postoperative color fundus photograph showing the resolution of the submacular hemorrhage. (D) Corresponding postoperative OCT image showing subretinal hyperreflective material and collapsed PED.
2.3 Case 3
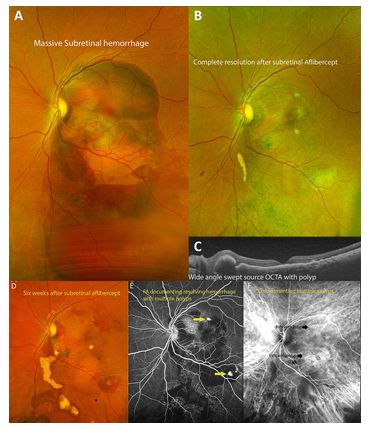
A 55-year-old Caucasian male with presented with a sudden loss of vision in his left eye. On examination, his best-corrected visual acuity (BCVA) was 20/30 in the right eye (OD) and CF at six feet in the left eye (OS). Anterior segment examination revealed significant nuclear sclerotic cataracts in both eyes. On fundus examination, the right eye was unremarkable, whereas the left eye had a submacular hemorrhage spanning both arcades with small polypoidal lesions in the macula (Figure 3A). Fluorescein angiography (FA) and indocyanine green angiography (ICGA) findings were consistent with the diagnosis of submacular hemorrhage secondary to IPCV (Figure 3B, 3C). The patient underwent a 23-gauge PPV with a subretinal injection of 2 mg aflibercept 6 days later. His vision improved to 20/200 one day after surgery and 20/60 at 90 days, with successful resolution of the submacular hemorrhage.
Figure 3: (A) Fundus photograph at the initial visit demonstrating a large dense subretinal hemorrhage extending from the superior macula beyond the inferior arcade. (B) Fundus photograph 6 months after pars plana vitrectomy with delivery of subretinal aflibercept demonstrating resolution of the submacular hemorrhage. (C) Swept-source OCT of the macula demonstrating a near-normal macular contour with small polyps, pigment epithelial detachment (PEDs), and slight atrophy of the outer retinal layers.
2.4 Case 4
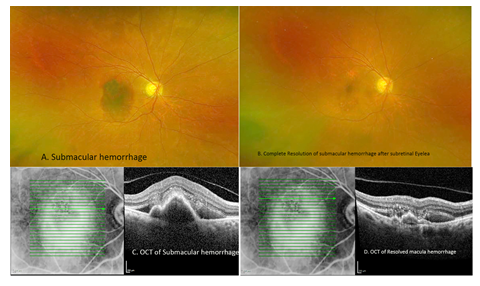
A 79-year-old Hispanic woman presented to the ER with a 4 days of decreased vision in the right eye. On examination, her BCVA was CF at six feet in the right eye and 20/100 in the left eye. Anterior segment evaluation revealed a 1+ nuclear sclerotic cataract (NSC) in both the eyes. Fundus examination revealed a subretinal hemorrhage (Figure 4A) of approximately 2-disc diameters in size with scant exudates in the right eye; the left eye was within normal limits. OCT revealed submacular hemorrhage in the right eye and VMT (Figure 4C) with associated macular edema in the left eye. The patient underwent 23-gauge PPV with a subretinal injection of 2 mg aflibercept on the same day. At the 1-month postoperative visit, color fundus photography showed improvement in submacular hemorrhage with settling of blood inferiorly in the right eye, and BCVA was CF in two feet. At the 6 months visit she had nearly complete resolution of the hemorrhage (Figure 4B), with improvement in BCVA to 20/80. OCT demonstrated subfoveal PED associated with subretinal fluid and VMT (Figure 4D).
Figure 4: (A) Color fundus photograph of the left eye preoperatively demonstrating a large submacular hemorrhage extending inferiorly. (C) Corresponding OCT showing a notched PED with submacular hemorrhage characteristic of IPCV. (B) Postoperative color fundus photograph showing the resolution of the submacular hemorrhage. (D) Corresponding postoperative OCT image showing subretinal hyperreflective material and collapsed PED.
3. Discussion
Idiopathic polypoidal choroidal vasculopathy (IPCV), a disease of the choroidal vasculature, often leads to submacular exudation and hemorrhage, secondary to dysfunctional polyps with increased VEGF levels [9,11]. Submacular hemorrhage and associated hemoglobin breakdown products are extremely toxic to photoreceptors and often lead to permanent loss of vision (if not removed immediately) [9]. Multiple modalities (PPV with TPA, pneumatic displacement) attempt to displace the liquefied blood products (either through dilution or lysis of clot) away from the fovea to prevent toxicity to photoreceptors in the fovea.
Intravitreal Aflibercept (VEGF-TRAP EYE, Eylea™; Regeneron Pharmaceuticals, Tarrytown, NY, USA), a soluble fusion protein (155KD) is superior to bevacizumab for the treatment of submacular hemorrhage associated with IPCV [10]. However intravitreal aflibercept is often ineffective in submacular hemorrhage, as the internal limiting membrane prevents rapid penetration of aflibercept into the subretinal space due to its molecular size. Larger antibodies (115 kDA; ~5nm) were unable to cross the ILM, while smaller Fab fragments of 48 kDA (~2.5 nm) easily diffused into subretinal space [12,13]; Aflibercept was not detected in subretinal space after intravitreal administration in a monkey study [14].
In this series, we delivered aflibercept directly into the subretinal space during vitrectomy in a controlled fashion using a viscous fluid control system (used in gene therapy). We hypothesized that the direct delivery of medication into the subretinal space (dual effect of inhibiting VEGF-induced choroidal exudation and physically limiting the duration of hemorrhagic products in contact with the photoreceptors through dilution) resulted in the rapid resolution of hemorrhage and recovery of vision in our subjects. No intra- or post-operative complications were noted in the selected group of patients.
In conclusion, subretinal delivery of aflibercept is a safe and effective strategy for treating submacular hemorrhage with good clinical results (improved visual acuity and resolution of hemorrhage).
Presentations: Presented as a poster at the American Society of Retina Specialist, July 2022.
Conflict of Interest: No conflicting relationships exist for any author. The authors alone are responsible for the content and writing of this manuscript.
Data Availability: All data generated or analyzed during this study are included in this published article.
Funding:
This research received no external funding.
IRB Statement: The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Loma Linda University (protocol code 5220227 and date of approval 7/11/2022).
Informed Consent: Informed consent for publication was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare that they have no competing interests. None of the authors has any conflicts of interest to disclose.
Authors’ Contributions:
Kinza T. Ahmad and Kakarla V. Chalam wrote and edited the manuscript. Suzie A. Gasparian helped collect and evaluate the data. Kakarla Chalam is the attending physician and performed all operative procedures and clinical examinations.
Acknowledgments:
We acknowledge Loma Linda University Eye Institute.
References
- Yannuzzi LA, Sorenson J, Spaide RF, Lipson B. Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina 32 (2012): 1-8.
- Stanescu-Segall D, Balta F, Jackson TL. Submacular hemorrhage in neovascular age-related macular degeneration: A synthesis of the literature. Survey of Ophthalmology 61 (2016): 18-32.
- Gopalakrishan M, Giridhar A, Bhat S, Saikumar SJ, Elias A. Pneumatic displacement of submacular hemorrhage: safety, efficacy, and patient selection. Retina27 (2007): 329-334.
- Fujikawa M, Sawada O, Miyake T, et al. Comparison of pneumatic displacement for submacular hemorrhages with gas alone and gas plus tissue plasminogen activator. Retina33 (2013): 1908-1914.
- Sandhu SS, Manvikar S, Steel DH. Displacement of submacular hemorrhage associated with age-related macular degeneration using vitrectomy and submacular tPA injection followed by intravitreal ranibizumab. Clinical Ophthalmology (2010): 637.
- Hillenkamp J, Surguch V, Framme C, et al. Management of submacular hemorrhage with intravitreal versus subretinal injection of recombinant tissue plasminogen activator. Graefe’s Archive for Clinical and Experimental Ophthalmology 248 (2009): 5-11.
- Treumer F, Roider J, Hillenkamp J. Long-term outcome of subretinal coapplication of rtPA and bevacizumab followed by repeated intravitreal anti-VEGF injections for neovascular AMD with submacular haemorrhage. British Journal of Ophthalmology 96 (2011): 708-713.
- Chalam KV, Gasparian S. Successful delivery of subretinal aflibercept (new surgical technique) for the treatment of submacular hemorrhage in idiopathic polypoidal choroidal vasculopathy. Journal of Surgical Case Reports 2021 (2021).
- Glatt H, Machemer R. Experimental Subretinal Hemorrhage in Rabbits. American Journal of Ophthalmology94 (1982): 762-773.
- Lee WK, Iida T, Ogura Y, et al. Efficacy and Safety of Intravitreal Aflibercept for Polypoidal Choroidal Vasculopathy in the PLANET Study. JAMA Ophthalmology 136 (2018): 786.
- Park DH, Kim IT. Polymorphisms in the VEGF-A in polypoidal choroidal vasculopathy in a Korean population. Japanese Journal of Ophthalmology 56 (2012): 145-151.
- Mordenti J, Cuthbertson RA, Ferrara N, et al. Comparisons of the Intraocular Tissue Distribution, Pharmacokinetics, and Safety of 125I-Labeled Full-Length and Fab Antibodies in Rhesus Monkeys Following Intravitreal Administration. Toxicologic Pathology 27 (1999): 536-544.
- Peynshaert K, Devoldere J, Minnaert AK, De Smedt SC, Remaut K. Morphology and Composition of the Inner Limiting Membrane: Species-Specific Variations and Relevance toward Drug Delivery Research. Current Eye Research 44 (2019): 465-475.
- Julien S, Biesemeier A, Taubitz T.Different effects of intravitreally injected ranibizumab and aflibercept on retinal and choroidal tissues of monkey eyes. Br J Ophthalmology 98 (2014): 813-825.