Successful Conservative Treatment in a Rare Case of Type 2 Congenital Cervical Dysgenesis: Case Report and Systematic Literature Review
Article Information
Ursula Catena1,2, Ilaria Romito1,2*, Maria Cristina Moruzzi1,2, Ilaria De Blasis1,2,
Antonia Carla Testa1,2, Giovanni Scambia1,2
1Division of Gynecologic Oncology, Fondazione Policlinico Universitario Agostino Gemelli, Rome, Italy
2Catholic University of Sacred Heart, Rome, Italy
*Corresponding Author: Dr. Romito Ilaria, Division of Gynecologic Oncology, Fondazione Policlinico Universitario Agostino Gemelli, Catholic University of Sacred Heart, IRCCS, Rome 00168, Italy
Received: 12 April 2020; Accepted: 20 April 2020; Published: 29 April 2020
Citation:
Ursula Catena, Ilaria Romito, Maria Cristina Moruzzi, Ilaria De Blasis, Antonia Carla Testa, Giovanni Scambia. Successful Conservative Treatment in a Rare Case of Type 2 Congenital Cervical Dysgenesis: Case Report and Systematic Literature Review. Obstetrics and Gynecology Research 3 (2020): 119-131.
Share at FacebookAbstract
Objective: Providing a systematic review of type 2 cervical dysgenesis (CD) by taking into consideration an interesting and rare case of genital anomaly which was treated with the use of laparoscopic ultrasound guidance.
Materials and Methods: A research of MEDLINE, EMBASE, Web of Sciences, Scopus, ClinicalTrial.gov, OVID and Cochrane Library was done. We analysed all types of study including case reports. We identified articles published at the time we began our review up from inception to July 2019.
Results: Three hundred thirty-four articles were identified, three hundred fifteen other articles were excluded for various reasons. Overall, nineteen articles were incorporated for further assessment. Three surgical techniques were used to treat type 2 cervical dysgenesis: drilling and coring technique (CDT), utero-vaginal anastomosis (UVA) and hysterectomy (HRT) or hemi-hysterectomy (H-HRT). Recurrences (38%) were described only with CDT. Five successful pregnancies were reported with the same technique.
Conclusions: Type 2 cervical dysgenesis is a rare congenital malformation. Data about recurrence and pregnancy rate are too sparse to recommend one technique rather than another. As shown in our comprehensive review, ultrasound-guided laparoscopy could represent a valid new surgical treatment approach.
Keywords
CDT, UVA, Type 2 Cervical Dysgenesis
CDT articles CDT Research articles CDT review articles CDT PubMed articles CDT PubMed Central articles CDT 2023 articles CDT 2024 articles CDT Scopus articles CDT impact factor journals CDT Scopus journals CDT PubMed journals CDT medical journals CDT free journals CDT best journals CDT top journals CDT free medical journals CDT famous journals CDT Google Scholar indexed journals UVA articles UVA Research articles UVA review articles UVA PubMed articles UVA PubMed Central articles UVA 2023 articles UVA 2024 articles UVA Scopus articles UVA impact factor journals UVA Scopus journals UVA PubMed journals UVA medical journals UVA free journals UVA best journals UVA top journals UVA free medical journals UVA famous journals UVA Google Scholar indexed journals Type 2 Cervical Dysgenesis articles Type 2 Cervical Dysgenesis Research articles Type 2 Cervical Dysgenesis review articles Type 2 Cervical Dysgenesis PubMed articles Type 2 Cervical Dysgenesis PubMed Central articles Type 2 Cervical Dysgenesis 2023 articles Type 2 Cervical Dysgenesis 2024 articles Type 2 Cervical Dysgenesis Scopus articles Type 2 Cervical Dysgenesis impact factor journals Type 2 Cervical Dysgenesis Scopus journals Type 2 Cervical Dysgenesis PubMed journals Type 2 Cervical Dysgenesis medical journals Type 2 Cervical Dysgenesis free journals Type 2 Cervical Dysgenesis best journals Type 2 Cervical Dysgenesis top journals Type 2 Cervical Dysgenesis free medical journals Type 2 Cervical Dysgenesis famous journals Type 2 Cervical Dysgenesis Google Scholar indexed journals Cervical uterine articles Cervical uterine Research articles Cervical uterine review articles Cervical uterine PubMed articles Cervical uterine PubMed Central articles Cervical uterine 2023 articles Cervical uterine 2024 articles Cervical uterine Scopus articles Cervical uterine impact factor journals Cervical uterine Scopus journals Cervical uterine PubMed journals Cervical uterine medical journals Cervical uterine free journals Cervical uterine best journals Cervical uterine top journals Cervical uterine free medical journals Cervical uterine famous journals Cervical uterine Google Scholar indexed journals cervix articles cervix Research articles cervix review articles cervix PubMed articles cervix PubMed Central articles cervix 2023 articles cervix 2024 articles cervix Scopus articles cervix impact factor journals cervix Scopus journals cervix PubMed journals cervix medical journals cervix free journals cervix best journals cervix top journals cervix free medical journals cervix famous journals cervix Google Scholar indexed journals endocervical canal articles endocervical canal Research articles endocervical canal review articles endocervical canal PubMed articles endocervical canal PubMed Central articles endocervical canal 2023 articles endocervical canal 2024 articles endocervical canal Scopus articles endocervical canal impact factor journals endocervical canal Scopus journals endocervical canal PubMed journals endocervical canal medical journals endocervical canal free journals endocervical canal best journals endocervical canal top journals endocervical canal free medical journals endocervical canal famous journals endocervical canal Google Scholar indexed journals cervical fibrous articles cervical fibrous Research articles cervical fibrous review articles cervical fibrous PubMed articles cervical fibrous PubMed Central articles cervical fibrous 2023 articles cervical fibrous 2024 articles cervical fibrous Scopus articles cervical fibrous impact factor journals cervical fibrous Scopus journals cervical fibrous PubMed journals cervical fibrous medical journals cervical fibrous free journals cervical fibrous best journals cervical fibrous top journals cervical fibrous free medical journals cervical fibrous famous journals cervical fibrous Google Scholar indexed journals utero-vaginal articles utero-vaginal Research articles utero-vaginal review articles utero-vaginal PubMed articles utero-vaginal PubMed Central articles utero-vaginal 2023 articles utero-vaginal 2024 articles utero-vaginal Scopus articles utero-vaginal impact factor journals utero-vaginal Scopus journals utero-vaginal PubMed journals utero-vaginal medical journals utero-vaginal free journals utero-vaginal best journals utero-vaginal top journals utero-vaginal free medical journals utero-vaginal famous journals utero-vaginal Google Scholar indexed journals reproductive articles reproductive Research articles reproductive review articles reproductive PubMed articles reproductive PubMed Central articles reproductive 2023 articles reproductive 2024 articles reproductive Scopus articles reproductive impact factor journals reproductive Scopus journals reproductive PubMed journals reproductive medical journals reproductive free journals reproductive best journals reproductive top journals reproductive free medical journals reproductive famous journals reproductive Google Scholar indexed journals gynaecological articles gynaecological Research articles gynaecological review articles gynaecological PubMed articles gynaecological PubMed Central articles gynaecological 2023 articles gynaecological 2024 articles gynaecological Scopus articles gynaecological impact factor journals gynaecological Scopus journals gynaecological PubMed journals gynaecological medical journals gynaecological free journals gynaecological best journals gynaecological top journals gynaecological free medical journals gynaecological famous journals gynaecological Google Scholar indexed journals
Article Details
1. Introduction
Cervical uterine anomalies are among the rarest uterine congenital anomalies which can be observed in the absence of the cervical canal or concomitantly with its obstruction. Although the prevalence counts only accounts for 3% of all uterine malformations and for 0.1% of the overall population [1], it is relevant because it generally affects women during their childbearing age, impairing fertility [2]. In the new ESHRE/ESGE classification, cervical anomaly is classified into 5 groups or classes: C0 (normal cervix), C1 (septate cervix), C2 (double normal cervix), C3 (unilateral cervical aplasia), and C4 (cervical aplasia) [3]. In another type of classification [4], this condition is divided into 4 categories according to both the anatomical variants and the type of surgical treatment: type 1 cervical agenesis (CA) (characterized by the complete absence of the cervix and no endocervical canal); type 2 cervical dysgenesis (CD) (characterized by cervical obstruction with the cervix being well formed, but lacking an endocervical canal); type 3 cervical dysgenesis (characterized by cervical fibrous cord whose diameter as well as the stroma nature may vary); type 4 cervical dysgenesis (characterized by cervical fragmentation with separation of the segments) (Figure1) [5].
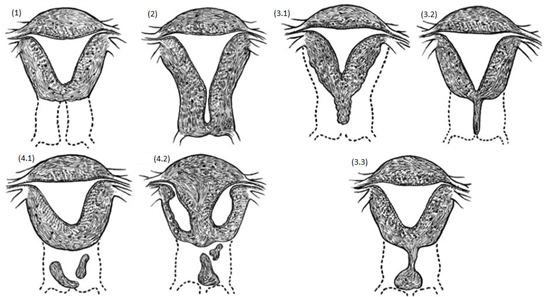
Figure 1: Cervical uterine anomalies [5].
Legend: (1) Cervical agenesis type 1; (2) Cervical dysgenesis type 2; (3) Cervical dysgenesis type 3; (4) Cervical dysgenesis type 4
The treatment remains controversial and depends on the symptoms as well as on the type of malformation. Particularly, for type 2 CD, three different surgical techniques have been proposed: first, coring and drilling technique (CDT), consisting in opening the cervical canal and draining the content; second, utero-vaginal anastomosis (UVA), consisting in the anastomosis of the section between the vagina and the endometrium; third, hysterectomy (HRT) or hemi-hysterectomy (H-HRT) [5]. Although the first two techniques try to restore and preserve the patient’s fertility, a consensus on which technique is the best has not yet been reached, also because of the rarity of the condition and the difficulties in RCT setting. Indeed, only case reports have been published until now, with a high rate of complications, recurrence of the symptoms after the first treatment, and often without any reference on the reproductive outcome [6-8]. In the last few decades, a new approach for the treatment of uterine pathologies has started to be used which consists in the use of a laparoscopic ultrasound probe (IUOS) to guide gynaecological conservative procedures. The probe, within the abdominal cavity, is in direct contact with the sections to be treated thus avoiding the potential source of interference as abdominal wall or vaginal wall [9]. This new innovative method was applied for endoscopic surgery in different conditions (myomas, uterine septum, cervical cancer) and seemed to be promising and accurate in the treatment of other gynaecological diseases [10, 11]. For this reason, it could be used for the treatment of cervical uterine anomalies where a more meticulous approach needs be employed [12]. Therefore, this systematic review sets out to analyse the efficacy and the fertility outcomes of different surgical techniques in the treatment of type 2 CD as well as to show the treatment of the rare type 2 CD case with the use of IUOS.
2. Case Report: CDT under Laparoscopic Ultrasound Guidance in a Patient with Bicorporeal Uterus and Type 2 Right Cervical Dysgenesis
We described a case of a 30-year-old nulligravida woman, with irregular menstrual cycles. She was referred to our gynaecological department for chronic pelvic pain and dysmenorrhea. The patient had a bicorporeal uterus with unilateral type 2 CD. Pre-operative ultrasonographic evaluation revealed a bicorporeal uterus, with double cervical canal, hematotrachelos content in the right cervical canal, consisting in an imperforated right cervix (Figure 2). Laparoscopy was performed in lithotomic position, after a 10-mm trocar insertion in the umbilicus. Two 5-mm ancillary trocars were introduced in the lower abdomen. Continuous CO2 pneumoperitoneum was induced keeping an intra-abdominal pressure below 12 mmHg. A 0° optic was introduced in the umbilical 10-mm trocar. Laparoscopy showed a IV stage endometriosis with nodules on the diaphragmatic peritoneum. In the pelvis, two hemi-uteruses were attached posteriorly to the rectum. The right ovary and fallopian tube were adherent and entrapped in a peritoneal pseudocyst. The pseudocyst contained fluid, which was removed. The right fallopian tube appeared swollen and hydropic and was therefore removed. A second 10mm-suprapubic trocar was positioned to enter with a Canon Aplio i800 ultrasound machine, and a laparoscopic probe covered with a sterile cover. The probe was inserted in the 10 mm suprapubic trocar, angled 90° and positioned in direct contact with the peritoneum between the bladder and the uterus (Figure 3). The surgeon used vaginoscopic approach, with a 5-mm diameter continuous-flow oval profile hysteroscope, a 30° fore-oblique telescope and a 5 Fr operating channel (Office Continuous Flow Operative Hysteroscopy ‘size 5’; Karl Storz, Tuttlingen, Germany). Saline solution (NaCl 0.9%) was used as a means of distension infused by way of an electronic irrigation and aspiration system (Endomat; Karl Storz, Tuttlingen, Germany). A stable intrauterine pressure of about 40 mmHg was obtained. The hysteroscopic view showed a single external cervical os with a regular cervix on the left side. A left hemi-cavity with a single fallopian tube ostium was found during the left cervical canal examination (Figure 4). The right external cervical os was not visible. Therefore, we used the laparoscopic ultrasound probe that revealed a right uterine cavity connected to a cervical canal filled with haemorrhagic material. The surgeon used a Collins speculum to open the walls of the vagina and the laparoscopic ultrasound guidance helped him to identify the right external cervical os. By vaginoscopic approach the surgeon used 5 Fr grasper forcep and scissors through the operating channel of the hysteroscope to open the external cervical os and to drain the hematotrachelos (Figure 5). The right uterine hemi-cavity was entered from this right cervical canal and a single tubal ostium was visualized (Figure 5). Cervical canal biopsy showed the presence of endocervical mucosa. No ectocervical mucosa was identified. A 10 Fr catheter was placed in the right hemi-cavity to keep the walls outstretched thus avoiding postoperative adhesions and possible right cervical canal reclosure. The Foley catheter was maintained inside the right hemi-cavity for 30 days. At day 31, during post-operative follow-up, transvaginal ultrasonographic evaluation revealed a bicorporeal uterus with double normal endometrial cavity and two normal cervical canals (Figure 6). After one month, hysteroscopy showed two normal cervical canals, both ending in a uterine hemi-cavity without postsurgical adhesions. In the following seven months, the patient had normal menstrual cycles without dysmenorrhea and chronic pelvic pain.
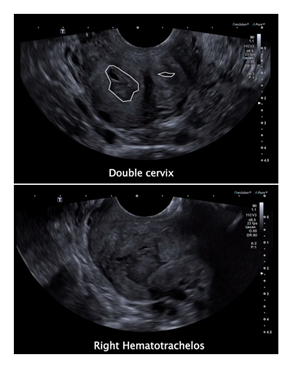
Figure 2: Double cervix (top) and right hematotrachelos (bottom).
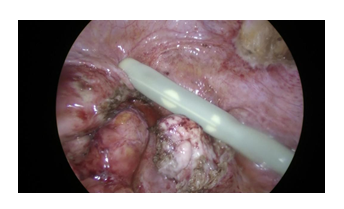
Figure 3: Laparoscopic ultrasound probe.
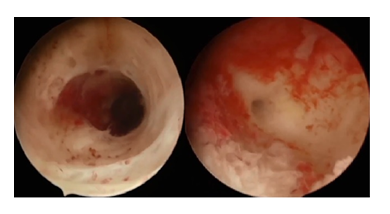
Figure 4: left cervical canal and left fallopian tube ostium.
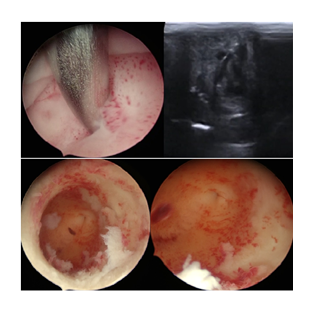
Figure 5: Opening of the right external cervical os with 5Fr grasper forcep (CDT) (top left); US view of the DTC (top right). Right cervical canal and right fallopian tube ostium after the drainage of the hematotrachelos (bottom) Blue arrow = grasper forcep into the uterine cavity.
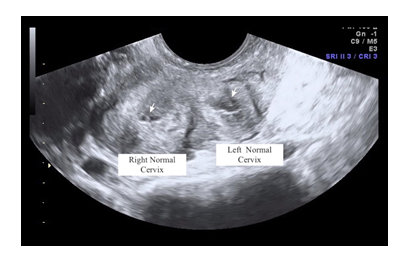
Figure 6: Bicorporeal uterus with double normal endometrial cavity.
3. Materials and Methods
The design of this systematic review of the literature was in accordance with the “PRISMA Guidelines” [13]. The clinical question for this review was developed based on the “PICOS format” [13]. Data were derived from researches published in MEDLINE, EMBASE, Web of Sciences, Scopus, ClinicalTrial.gov, OVID and Cochrane Library up from inception to July 2019, using a combination of the following Medical Subjects’Headings (MeSH): “cervical aplasia” or “cervical agenesis”, “cervical dysplasia” or “cervicaldysgenesis”, “uterine malformations” and “surgical treatment*”. Studies of patients with type 2 CD undergoing surgical treatment were taken into consideration. Case reports were included in the selection. Only articles published in English were included. To avoid duplication, studies describing the same study population were included only once. We examined these record titles and abstracts retrieved from the said researches. All full-text manuscript reference lists were analysed in order to find additional eligible studies. This process was carried out by 2 co-authors (UC, IR). The article selection process is shown in Figure 7.
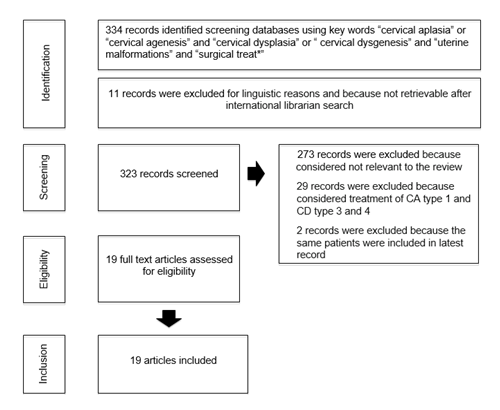
Figure 7: Study selection process.
4. Results
Our electronic database search revealed 334 articles, 11 of which were excluded for linguistic reasons or because they were not easy to find after international librarian search. Three hundred and twenty-three full text articles were examined, 273 were excluded because they were, all considered, not relevant for the review, 29 records were excluded because they considered treatment of type 1, 3 and 4 cervical dysgenesis; two records were excluded because the same patients had been included in the latest records. Overall, 19 articles were selected for further assessment with a total of 68 patients. The patients’average age was 16.51 years ± 4.21 years (mean ± standard deviation) (range 10-28).The indication for the surgery was primary amenorrhea for patients with single cervix (C4) (40%) and dysmenorrhea or chronic pelvic pain for patients with double cervix (C3) (16.2%). Thirty patients (43.8%) had unknown treatment indication. All the cases were treated by using one of the three available techniques: drilling and coring technique (CDT), utero-vaginal anastomosis (UVA) and hysterectomy (HRT) or hemi-hysterectomy (H-HRT). In 29 (43%) out of 68 cases, the treatment technique was not described and in one (1.5%) patient the surgery was not performed. Twenty-one patients (55%) underwent CDT; 12 women (32%) underwent UVA and only 5 patients (13%) were treated directly with HRT or H-HRT (table 1).
Among the 38 patients who had undergone conservative surgery, follow-up data were available only for 9 (43%) patients in the CDT group and for 12 (100%) patients in the UVA group (table 2). Follow-up was 36 ± 43 months and 8 ± 50 months (median ± standard deviation) in the CDT and UVA technique, respectively. In few cases (14%) the CDT procedure was repeated due to symptoms’ reappearance [14-16] and in 38% of the patients an hemi-hysterectomy was performed as either a secondary or third procedure. Two cases of severe sepsis were also described, one of which required drainage of the pelvic abscess, intestinal resection and temporary sigmoid colostomy [17]. None of the 12 patients treated with UVA had a restenosis. Five successful pregnancies had been previously reported (Table 3). The CDT was the only procedure for which successful delivery was reported. Two pregnancies were spontaneous [18]. One patient became pregnant after a second IVF cycle with zygote Intrafallopian Transfer (ZIFT) [19] and another patient after an IVF with transmyometrial embryo transfer [20]. No complications were reported during pregnancies except for 1 case of severe pre-eclampsia at 31 weeks of gestation that was solved by performing a caesarean section. After UVA procedure, only one woman had a pregnancy with IVF that ended up with miscarriage [21].
|
Year |
Author |
Type of study |
N° |
ESGE/ESHRE |
Surgical Treatment |
|
1900 |
Ludwig [s] |
Case report |
1 |
C4 |
C |
|
1939 |
Duyzings [6] |
Case report |
1 |
C4 |
C |
|
1961 |
Zarou [6] |
Case report |
1 |
C4 |
C |
|
1963 |
Williams [s] |
Case report |
1 |
C4 |
C |
|
1979 |
Dillon [27] |
Case report |
1 |
C4 |
T- TAH |
|
1984 |
Garat [29] |
Case report |
1 |
C4 |
C |
|
1984 |
Ragni [s] |
Case report |
1 |
C4 |
C |
|
1989 |
Jacob and Griffin [22] |
Case report |
2 |
C4 |
2 C |
|
1990 |
Thijssen [19] |
Case report |
1 |
C4 |
C |
|
1990 |
Hampton [18] |
Case report |
1 |
C4, V4 |
C |
|
1999 |
Hovsepian [23] |
Case report |
1 |
U0,C4,V0 |
C |
|
1999 |
Antilla [20] |
Case report |
1 |
C4 |
C |
|
2010 |
Saleh [14] |
Case report |
1 |
U3b, C3, V0 |
C |
|
2010 |
Rock JA [24] |
Case report |
6 |
C4 |
4 C, graft |
|
2 T- TAH |
|||||
|
2013 |
Wang [7] |
Case report |
3 |
U3b, C3, V0 |
2 TU-TAH |
|
2013 |
Fedele [8] |
Case report |
4 |
U3b, C3, V0 |
NR |
|
2014 |
Ding [26] |
Case report |
6 |
4 U0, C4, V4 |
UVA, graft |
|
1 U0, C4, V0 |
|||||
|
1 U4, C4, V4 |
|||||
|
2014 |
Sabdia [15] |
Case report |
1 |
U3b, C3, V2 |
C, VS |
|
2016 |
Kimble [17] |
Case report |
2 |
U0, C4, V3 |
2 C, VS |
|
2016 |
Song [21] |
Case report |
30 |
NS |
5 UVA |
|
2017 |
Dohbit [30] |
Case report |
1 |
U3b, C3, V0 |
UVA |
|
2017 |
Kapczuk [16] |
Case report |
1 |
U3b, C3, V0 |
C |
|
Total |
68 |
Legend: NR = not reported; N°= number of patients; [s]=Quoted from Jacob and Griffin (1989); NS= not sure, this clinical article described a group of 96 patients with cervical agenesis. Only 30 patients had cervical obstruction; T-TAH: total laparotomic abdominal hysterectomy; TU-TAH: unilateral laparotomic abdominal hysterectomy; C = Drilling or coring technique or uterovaginal canalization; UVA = utero-vaginal anastomosis; VS = vaginal septotomy
Table 1: Sistematic literature review about cases of type 2 cervical dysgenesis (cervical obstruction).
|
Year |
Author |
N° patients |
Follow-Up (Yes/months/NR) |
Recurrence (Yes/No) |
Surgical Secondary Treatment |
|
|
1900 |
Ludwig [s] |
1 |
NR |
NR |
NR |
|
|
1939 |
Duyzings [6] |
1 |
NR |
NR |
NR |
|
|
1961 |
Zarou [6] |
1 |
43 |
No |
No |
|
|
1963 |
Williams [s] |
1 |
Yes |
No |
No |
|
|
1979 |
Dillon [27] |
1 |
Yes |
No |
No |
|
|
1984 |
Garat [29] |
1 |
18 |
No |
No |
|
|
1984 |
Ragni [s] |
1 |
Yes |
Yes |
T-TAH |
|
|
1989 |
Jacob and Griffin [22] |
2 |
Yes |
Yes |
T-TAH |
|
|
1990 |
Thijssen [19] |
1 |
132 |
No |
No |
|
|
1990 |
Hampton [18] |
1 |
84 |
No |
No |
|
|
1999 |
Hovsepian [23] |
1 |
6 |
No |
No |
|
|
1999 |
Antilla [20] |
1 |
60 |
Yes |
No |
|
|
2010 |
Saleh [14] |
1 |
Yes |
Yes |
TU-TAH |
|
|
2010 |
Rock JA [24] |
6 |
Yes |
No |
No |
|
|
2013 |
Wang [7] |
3 |
NR |
NR |
NR |
|
|
2013 |
Fedele [8] |
4 |
NR |
NR |
NR |
|
|
2014 |
Ding [26] |
6 |
8 |
No |
No |
|
|
2014 |
Sabdia [15] |
1 |
Yes |
Yes |
SU-TAH |
|
|
2016 |
Kimble [17] |
2 |
6,36 |
Yes, I, MODS |
1 T-TAH |
|
|
1 (note) |
||||||
|
2016 |
Song [21] |
30 |
36,60,84,84,168 |
No |
No |
|
|
2017 |
Dohbit [30] |
1 |
6 |
No |
No |
|
|
2017 |
Kapczuk [16] |
1 |
1 |
Yes |
TU-TAH |
|
|
|
Total |
21 |
||||
Legend: NR = not reported; N°= number of patients; [s]=Quoted from Jacob and Griffin (1989); T-TAH: total laparotomic abdominal hysterectomy, TU-TAH: unilateral laparotomic abdominal; hysterectomy, SU-TAH: unilateral laparoscopic abdominal hysterectomy; I= infection, MODS = Multiple Organ Dysfunction Syndrome; (note) = LPT: Drainage of pelvic abscess, sigmoide colostomy (Hartmann) after 3 month hysterectomy and closure of Hartmann colostomy
Table 2: Follow-up and recurrence.
|
References |
Type of surgery |
Age of surgery (years) |
Complication surgery |
Assisted medical procreation |
Delivery (week) |
|
Zarou [6] |
Cervical drilling |
18 |
No |
No |
Cs at term |
|
Hampton [18] |
Cervical drilling |
11 |
No |
No |
Cs at 38w |
|
Thijssen [19] |
Cervical drilling |
15 |
No |
IVF-ZIFT |
Cs at term |
|
Antilla [20] |
Cervical drilling |
24 |
No |
IVF-transmyometrial ET |
Cs at 32 w |
|
Rock JA [24] |
Cervical drilling, skin graft |
/ |
/ |
/ |
Cs at 34 w |
Legend: ZIFT = zygote intra-Fallopian transfer; IVF = in-vitro fertilization; ET = embryo transfer; Cs = cesarean section
Table 3: Summary of the cases with type 2 cervical dysgenesis (cervical obstruction) and successful pregnancy.
5. Discussion
CD is among the rarest Mullerian anomalies. Type 2 CD often occurs in a young population for whom fertility is a major concern. Conservative surgical techniques, described in literature, are CDT and UVA. We used CDT in a case of type 2 CD ultrasound-guided laparoscopy for the first time. In literature, the first surgical technique described to treat type 2 CD is the coring and drilling technique. The principle of the surgery consists in cervical canal opening with various instruments and drainage of the content. The connection between the cervix and the vagina can be done with a vaginal approach, through the external cervical os [6] or, with a laparotomic approach, forcing a trocar down through the cervix into the vagina [22]. After creating the connection, some authors prefer to use a Foley catheter to stent the neo-cervical canal to avoid post-surgical stenosis [23].
Another option is to sew a full-thickness skin graft around the Foley catheter to speed the process of epithelialization and to reduce the chances of endometritis [24]. The uterovaginal anastomosis (UVA) consists in the anastomosis between the vagina and the endometrium. It is a very ancient technique, considering that 5 cases of type 2 CD were described between 1938 and 1958 [25]. All authors performed an incision in the peritoneum between the bladder and the uterus and/or between the uterus and the rectum, proceeding with the incision ofthe cervix and introducing a Foley catheter. The last part of the technique consists in suturing the endometrium to the vagina. To reduce the risk of stenosis it is possible to use [21] a biological mesh or a partial vaginal epithelium. Other surgeons have explored the use of a cellular porcine small intestinal submucosa graft for cervicovaginal reconstruction [26].
The demolitive treatment consists in hysterectomy or hemi-hysterectomy. This possibility is generally reserved to patients with bicorporeal uterus [7] or to patients without pregnancy desire [24, 27]. It is also employed in case of repeated failures of the conservative treatment or in case of complications after surgery (infections or cervical restenosis) [14-17]. The risk of recurrence is associated with fertility-sparing surgery. In our series, none of the patients treated with UVA had a restenosis but median follow-up compared with the CDT group’s follow-up was too short. No conclusion can be drawn and any impact on recurrence due to different conservative treatment would require a rather large series with a longer follow-up. Pregnancies are reported only in the CDT group. In this case, too, the series is too short to carry out a methodological analysis based on the results.
6. Strengths of the Study
This paper is the first systematic review specifically focused on the surgical treatment of type 2 cervical dysgenesis. The use of the laparoscopic probe in cervical uterine anomalies will enable further research in this field.
7. Study Limitations
Although we performed a systematic and comprehensive review, RCTs are lacking in our paper. Most papers are case reports,which does not allow for a methodological analysis of the results.
8. Conclusion
Standard treatment of type 2 CD has not yet been established due to its rarity. The conservative technique should be recommended, especially for young women. There is no evidence that one technique is better than the others in terms of recurrence and fertility outcome. RCT with larger sample size are needed. Hysterectomy should be recommended if canalization procedures fail or in the absence of pregnancy desire [28]. While waiting for larger case studies to have comparable results about surgical outcomes and fertility, we proposed intraoperative laparoscopic ultrasound guidance as an innovative approach, albeit just in one case, to be used in complex female genital malformation.
Acknowledgements
Nothing to declare
Disclosure
Nothing to declare
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Grimbizis GF, Camus M, Tarlatzis BC, et al. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update7 (2001): 161-174.
- Fujimoto VY, Miller JH, Klein NA, et al.Congenital cervical atresia: report of seven cases and review of the literature. Am J Obstet Gynecol 177 (1997): 1419-1425.
- Grimbizis GF, Gordts S, Di Spiezio Sardo A, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod 28 (2013): 2032-2044.
- Rock J A, Carpenter S E, Wheeless, et al. The clinical management of maldevelopment of the uterine cervix. Journal of Pelvic Surgery 1 (1995): 129-133.
- Roberts CP, Rock JA. Surgical methods in the treatment of congenital anomalies of the uterine. Curr Opin Obstet Gynecol 23 (2011): 251-257.
- Zarou Gs, Acken HS, Brevetti RC. Surgical management of congenital atresia of the cervix. Case report and review of the literature. Am J Obstet Gynecol 82 (1961): 923-928.
- Wang S, Lang JH, Zhu L, et al. Duplicated uterus and hemivaginal or hemicervical atresia with ipsilateral renal agenesis: an institutional clinical series of 52 cases. Eur J Obstet Gynecol Reprod Biol 170 (2013): 507-511.
- Fedele L, Motta F, Frontino G, et al. Double uterus with obstructed hemivagina and ipsilateral renal agenesis: pelvic anatomic variants in 87 cases. Hum Reprod 28 (2013): 1580-1583.
- Hao Y, Li SJ, Zheng P, et al. Intraoperative ultrasound-assisted enucleation of residual fibroids following laparoscopic myomectomy. Clin Chim Acta 495 (2019): 652-655.
- Cheung TH, Lo KW, Yim SF, et al. Clinical use of laparoscopic ultrasonography in detecting nodal metastasis in advanced-stage cervical carcinoma. Int J Gynaecol Obstet 112 (2011): 154-158.
- Mascilini F, Quagliozzi L, Moro F, et al. Role of Intraoperative Ultrasound to Extend the Application of Minimally Invasive Surgery for Treatment of Recurrent Gynecologic Cancer. J Minim Invasive Gynecol 25 (2018): 848-854.
- Letterie GS, Marshall L. Evaluation of real-time imaging using a laparoscopic ultrasound probe during operative endoscopic procedures. Ultrasound Obstet Gynecol 16 (2000): 63-67.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8 (2010): 336-341.
- Saleh M, Badawy SZ. Unilateral non-communicating cervical atresia in a patient with uterus didelphys and unilateral renal agenesis. J Pediatr Adolesc Gynecol 23 (2010): e137-e140.
- Sabdia S, Sutton B, Kimble RM. The obstructed hemivagina, ipsilateral renal anomaly, and uterine didelphys triad and the subsequent manifestation of cervical aplasia. J Pediatr Adolesc Gynecol 27 (2014): 375-378.
- Kapczuk K, Friebe Z, Iwaniec K, et al. Obstructive Mullerian Anomalies in Menstruating. J Pediatr Adolesc Gynecol 31 (2018): 252-257.
- Kimble R, Molloy G, Sutton B. Partial Cervical Agenesis and Complete Vaginal Atresia. J Pediatr Adolesc Gynecol 29 (2016): e43-e47.
- Hampton HL, Meeks GR, Bates GW, et al. Pregnancy after successful vaginoplasty and cervical stenting for partial atresia of the cervix. Obstet Gynecol 76 (1990): 900-901.
- Thijssen RF, Hollanders JM, Willemsen WN, et al. Successful pregnancy after ZIFT in a patient with congenital cervical atresia. Obstet Gynecol 76 (1990): 902-904.
- Anttila L, Penttilä TA, Suikkari AM. Successful pregnancy after in-vitro fertilization and transmyometrial embryo transfer in a patient with congenital atresia of cervix: case report. Hum Reprod 14 (1999): 1647-1649.
- Song X, Zhu L, Ding J, et al. Clinical characteristics of congenital cervical atresia and associated endometriosis among 96 patients. Int J Gynaecol Obstet 134 (2016): 252-255.
- Jacob JH, Griffin WT. Surgical reconstruction of the congenitally atretic cervix: two cases. Obstet Gynecol Surv 44 (1989): 556-569.
- Hovsepian DM, Auyeung A, Ratts VS. A combined surgical and radiologic technique for creating a functional neo-endocervical canal in a case of partial congenital cervical atresia. Fertil Steril 71 (1999): 158-162.
- Rock JA, Roberts CP, Jones HW Jr. Congenital anomalies of the uterine cervix: lessons from 30 cases managed clinically by a common protocol. Fertil Steril 94 (2010): 1858-1863.
- Rotter CW. Surgical correction of congenital atresia of the cervix. Am. J. Obst e ginec 76 (1958): 643.
- Ding JX, Chen XJ, Zhang XY, et al. Acellular porcine small intestinal submucosa graft for cervicovaginal reconstruction in eight patients with malformation of the uterine cervix. Hum Reprod 29 (2014): 677-682.
- Dillon WP, Mudaliar NA, Wingate MB. Congenital atresia of the cervix. Obstet Gynecol 54 (1979): 126-129.
- Alessandro Bulfoni, Francesca Motta, Giada Frontino, et al. Mayer-Rokitansky-Kuster-Hauser syndrome: associated anomalies in a cohort of 77 patients. Italian Journal of Gynaecology & Obstetrics 31 (2019): 1.
- Garat JM, Martinez E, Aragona F, et al. Cervical uterine atresia with hematometra: a rare cause of urinary retention in a girl. J Urol 132 (1984): 772-773.
- Dohbit JS, Meka E, Tochie JN, et al. A case report of bicornis bicollis uterus with unilateral cervical atresia: an unusual aetiology of chronic debilitating pelvic pain in a Cameroonian teenager. BMC Womens Health 17 (2017): 39.
