Success of Vaginal Birth after Cesarean Section (VBAC) based on Previous Cesarean Delivery Indication in a Tertiary University Hospital: A Five Year Retrospective Study
Article Information
John Edward O Tanchuco, MD1,* and Chiaoling Sua Lao, MD1
1 Department of Obstetrics and Gynecology, University of the Philippines - Philippine General Hospital Taft Avenue, Ermita, Manila 1000
*Corresponding Author: John Edward O Tanchuco, MD, Department of Obstetrics and Gynecology, University of the Philippines – Philippine General Hospital, Philippines.
Received: 05 January 2023; Accepted: 12 January 2023; Published: 10 February 2023
Citation: John Edward O. Tanchuco, Chiaoling Sua Lao. Success of Vaginal Birth After Cesarean Section (VBAC) based on Previous Cesarean Delivery Indication in a Tertiary University Hospital: A Five Year Retrospective Study. Obstetrics and Gynecology Research. 6 (2023): 63-70
Share at FacebookAbstract
Objective:
This study aims to determine the success of vaginal birth after cesarean section (VBAC) based on previous cesarean delivery indication.
Design:
Retrospective cohort study
Setting:
University of the Philippines - Philippine General Hospital, Department of Obstetrics and Gynecology hospital masterlist data
Sample:
Gravidas with a previous cesarean section within a five year period (2015 - 2019) METHODS: Maternal demographics, obstetric characteristics on admission, perinatal morbidities and maternal morbidities were recorded. Data was analyzed using Student’s t-test for continuous variables, chi-square test to compare the distribution and Z-test was used to compare success rates.
Main outcome measures:
The main outcome measures are TOLAC rate, VBAC rate, factors which affect success of TOLAC and VBAC, and perinatal and maternal morbidities associated with successful and failed VBAC.
Results:
A total of 2485 patients were included. The overall TOLAC rate was 17% (95% CI: 15.6% - 18.6%) and the VBAC rate was 9.5% (95% CI: 8.3% - 10.7%). Patients with successful VBAC are younger, had less weight and body mass index, shorter interdelivery intervals, and admitted in active phase cervical dilatation. Previous cesarean section indication did not significantly affect VBAC success. Perinatal and maternal morbidities of successful and failed VBAC did not significantly differ from one another.
Conclusions:
This study provided local evidence and valuable perspective in success factors which influence our counselling and eventual management of patients with a previous cesarean section
Keywords
Trial of Labor after Cesarean; TOLAC; Vaginal Birth after Cesarean; VBAC; Cesarean section; Philippines
Trial of Labor after Cesarean articles Trial of Labor after Cesarean Research articles Trial of Labor after Cesarean review articles Trial of Labor after Cesarean PubMed articles Trial of Labor after Cesarean PubMed Central articles Trial of Labor after Cesarean 2023 articles Trial of Labor after Cesarean 2024 articles Trial of Labor after Cesarean Scopus articles Trial of Labor after Cesarean impact factor journals Trial of Labor after Cesarean Scopus journals Trial of Labor after Cesarean PubMed journals Trial of Labor after Cesarean medical journals Trial of Labor after Cesarean free journals Trial of Labor after Cesarean best journals Trial of Labor after Cesarean top journals Trial of Labor after Cesarean free medical journals Trial of Labor after Cesarean famous journals Trial of Labor after Cesarean Google Scholar indexed journals TOLAC articles TOLAC Research articles TOLAC review articles TOLAC PubMed articles TOLAC PubMed Central articles TOLAC 2023 articles TOLAC 2024 articles TOLAC Scopus articles TOLAC impact factor journals TOLAC Scopus journals TOLAC PubMed journals TOLAC medical journals TOLAC free journals TOLAC best journals TOLAC top journals TOLAC free medical journals TOLAC famous journals TOLAC Google Scholar indexed journals Vaginal Birth after Cesarean articles Vaginal Birth after Cesarean Research articles Vaginal Birth after Cesarean review articles Vaginal Birth after Cesarean PubMed articles Vaginal Birth after Cesarean PubMed Central articles Vaginal Birth after Cesarean 2023 articles Vaginal Birth after Cesarean 2024 articles Vaginal Birth after Cesarean Scopus articles Vaginal Birth after Cesarean impact factor journals Vaginal Birth after Cesarean Scopus journals Vaginal Birth after Cesarean PubMed journals Vaginal Birth after Cesarean medical journals Vaginal Birth after Cesarean free journals Vaginal Birth after Cesarean best journals Vaginal Birth after Cesarean top journals Vaginal Birth after Cesarean free medical journals Vaginal Birth after Cesarean famous journals Vaginal Birth after Cesarean Google Scholar indexed journals VBAC articles VBAC Research articles VBAC review articles VBAC PubMed articles VBAC PubMed Central articles VBAC 2023 articles VBAC 2024 articles VBAC Scopus articles VBAC impact factor journals VBAC Scopus journals VBAC PubMed journals VBAC medical journals VBAC free journals VBAC best journals VBAC top journals VBAC free medical journals VBAC famous journals VBAC Google Scholar indexed journals Cesarean section articles Cesarean section Research articles Cesarean section review articles Cesarean section PubMed articles Cesarean section PubMed Central articles Cesarean section 2023 articles Cesarean section 2024 articles Cesarean section Scopus articles Cesarean section impact factor journals Cesarean section Scopus journals Cesarean section PubMed journals Cesarean section medical journals Cesarean section free journals Cesarean section best journals Cesarean section top journals Cesarean section free medical journals Cesarean section famous journals Cesarean section Google Scholar indexed journals Obstetricians articles Obstetricians Research articles Obstetricians review articles Obstetricians PubMed articles Obstetricians PubMed Central articles Obstetricians 2023 articles Obstetricians 2024 articles Obstetricians Scopus articles Obstetricians impact factor journals Obstetricians Scopus journals Obstetricians PubMed journals Obstetricians medical journals Obstetricians free journals Obstetricians best journals Obstetricians top journals Obstetricians free medical journals Obstetricians famous journals Obstetricians Google Scholar indexed journals Gynecologists articles Gynecologists Research articles Gynecologists review articles Gynecologists PubMed articles Gynecologists PubMed Central articles Gynecologists 2023 articles Gynecologists 2024 articles Gynecologists Scopus articles Gynecologists impact factor journals Gynecologists Scopus journals Gynecologists PubMed journals Gynecologists medical journals Gynecologists free journals Gynecologists best journals Gynecologists top journals Gynecologists free medical journals Gynecologists famous journals Gynecologists Google Scholar indexed journals cesarean deliveries articles cesarean deliveries Research articles cesarean deliveries review articles cesarean deliveries PubMed articles cesarean deliveries PubMed Central articles cesarean deliveries 2023 articles cesarean deliveries 2024 articles cesarean deliveries Scopus articles cesarean deliveries impact factor journals cesarean deliveries Scopus journals cesarean deliveries PubMed journals cesarean deliveries medical journals cesarean deliveries free journals cesarean deliveries best journals cesarean deliveries top journals cesarean deliveries free medical journals cesarean deliveries famous journals cesarean deliveries Google Scholar indexed journals maternal articles maternal Research articles maternal review articles maternal PubMed articles maternal PubMed Central articles maternal 2023 articles maternal 2024 articles maternal Scopus articles maternal impact factor journals maternal Scopus journals maternal PubMed journals maternal medical journals maternal free journals maternal best journals maternal top journals maternal free medical journals maternal famous journals maternal Google Scholar indexed journals perinatal benefits articles perinatal benefits Research articles perinatal benefits review articles perinatal benefits PubMed articles perinatal benefits PubMed Central articles perinatal benefits 2023 articles perinatal benefits 2024 articles perinatal benefits Scopus articles perinatal benefits impact factor journals perinatal benefits Scopus journals perinatal benefits PubMed journals perinatal benefits medical journals perinatal benefits free journals perinatal benefits best journals perinatal benefits top journals perinatal benefits free medical journals perinatal benefits famous journals perinatal benefits Google Scholar indexed journals
Article Details
List of abbreviations
TOLAC – Trial of Labor after Cesarean; VBAC – Vaginal Birth after Cesarean;
ERCS – Emergency / Elective Repeat Cesarean Section
Introduction and Significance of the Study
Trial of labor after cesarean delivery (TOLAC) is defined by the American College of Obstetricians and Gynecologists (ACOG) as a “planned attempt to deliver vaginally by a woman who has had a previous cesarean delivery, regardless of the outcome.” This provides a possibility for women to achieve a successful vaginal birth after cesarean section (VBAC). TOLAC for a second delivery is a necessary option in developing countries to reduce the cost and morbidities associated with repeat cesarean deliveries. [1] Decreased maternal morbidity, decreased risk of complications in future pregnancies and a decrease in the overall cesarean delivery rate at the population level are all desirable outcomes associated with VBAC. [2]
However, VBAC remains to be a public health goal to reduce cesarean section rates. Cesarean sections have been continuously increasing over the past decades, with no significant maternal and perinatal benefits. [4, 26] In response, the World Health Organization has made recommendations on non-clinical interventions designed to reduce cesarean section rates with three targets of intervention: the woman (patient), the healthcare professional and health organizations, facilities, or systems. [26] While VBAC awareness is high in the local setting, it has yet to translate into the reduction of cesarean section rates in the Philippines. In the study of Magante et al in 2015 on VBAC practice in the Philippines, 75% of Filipino obstetricians practiced VBAC, mostly from university hospitals. Participants have scored higher on requirements of VBAC, qualifications of low-risk candidates, and associated complications. Practitioners emphasized its lower cost, shorter recovery time, and fewer long- term complications. They were more likely to do VBAC for a patient who comes in active labor. For non-practitioners of VBAC, the main cause was fear of associated complications. [17]
Cesarean sections have both short-term and long-term risks for both the mother and the child with significant healthcare costs. [26] VBAC impacts healthcare system financing by reducing healthcare costs per patient. A local cost-effectiveness study by Garcia-Tansengco in 2001 has shown a cost-effectiveness ratio for a trial of labor was PHP 10,225.97 per uterine rupture averted, while that for an elective repeat cesarean section was PHP 12,447.40 per uterine rupture averted. Although the cost difference is small (PHP 2,221.43), the incremental cost-effectiveness ratio per year could reach as high as PHP 1.2 million per uterine rupture averted. [10]
This study aims to determine the success of vaginal birth after cesarean section (VBAC) based on previous cesarean delivery Indication in Filipino gravidas in a tertiary university hospital as the basis to offer TOLAC and VBAC in women with a previous cesarean. Implications from this study aims to improve VBAC counselling in the antenatal visits and appropriately advise the likelihood of successful VBAC.
Materials and Methods
Definition of Terms
Women who had cesarean sections for non-recurring indications such as fetal distress or malpresentation would either undergo successful vaginal birth after cesarean section (VBAC) or have an elective / emergency repeat cesarean section (ERCS) in the current pregnancy. Women with a prior cesarean who had TOLAC and gave birth vaginally will be recorded under successful VBAC, while those that resulted in to an elective / emergency repeat cesarean section will be coded under “failed” VBAC.
Study Population
This is a retrospective cohort study and utilized available masterlist data from the University of the Philippines - Philippine General Hospital, Department of Obstetrics and Gynecology archives from January 1, 2015, until December 31, 2019, which contain information on all births in the Philippine General Hospital for the five (5) year duration. All patients who underwent TOLAC from 2015-2019 who meet the inclusion criteria for TOLAC were included in the study, regardless of the age of gestation, route and neonatal outcomes upon delivery. Consent and motivation to undergo TOLAC was assumed in these patients. Information was confirmed via outpatient chart review for the selected sample. Those with incomplete masterlist data were excluded from this study.
Sample Size
There were 30,053 obstetric charity admissions from the year 2015-2019 based on the OB-GYN department’s annual statistics report. The sample size for frequency in a population was computed from OpenEpi, Version 3, open-source online calculator http://www.openepi.com/SampleSize/SSPropor.htm (accessed August 10, 2020). Assumed frequency of outcome factor in the population set at 50±5% with a 95% confidence level. The minimum sample size required for this study was 380 patients.
Data Collection
The master list contained the maternal demographics and obstetric characteristics on admission which include: age, height, weight, body mass index (BMI), gravity-parity score, estimated fetal weight, interdelivery interval, gestational age on admission, cervical dilatation on admission, and previous cesarean section indication, which were all recorded. The indication of the current cesarean section was recorded if failed VBAC / ERCS occurs. For any perinatal or maternal morbidities associated with both successful and failed VBAC, these were noted as well in the data collection. Perinatal morbidities include low first and/or fifth minute APGAR scores (<6) and admission to the neonatal intensive care unit. Maternal morbidities include uterine rupture, postpartum hemorrhage and peripartum hysterectomy.
Statistical Analysis
The data was analyzed using STATA version 14.1 (STATACorp LLC, October 2015, Texas). Numerical variables are presented as mean and standard deviation (±SD). The demographic and obstetric characteristics of the TOLAC and successful VBAC groups was compared using Student’s t-test for continuous variables and chi-square test was used to compare the distribution. Z-test was used to compare success rates. A 95% confidence interval (p-value < 0.05) was considered statistically significant.
Results
A total of 2972 patients successfully met the inclusion criteria for this retrospective cohort study. Of the 2972 patients, 2485 patients (83.61% of total eligible patients) were used in this study; 487 patients were excluded due to incomplete and / or inconsistent masterlist data from the UP-PGH Department of Obstetrics and Gynecology archives. Among the 2,485 Filipino gravidas included in this study, 424 patients underwent TOLAC and 235 patients had successful VBAC. (Table 1 and 2). The overall TOLAC rate in the tertiary university hospital is 17% (95% CI: 15.6% - 18.6%) and the VBAC rate is 9.5% (95% CI: 8.3% - 10.7%) Conversely, the failed VBAC / ERCS overall rate is 90.5% (95% CI: 89.3% - 91.7%).
|
Characteristics |
TOLAC (+) n=424 |
TOLAC (-) n=2,061 |
p-value |
|
Age (years) |
28.87 + 5.88 |
29.76 + 5.94 |
<.01* |
|
Maternal weight (kg) |
63.68 + 11.23 |
64.91 + 11.55 |
0.04* |
|
Maternal BMI (kg/m2) |
27.11 + 4.52 |
27.64 + 4.78 |
0.04* |
|
Fetal weight (g) |
2828.5 + 2777.5 |
2871.5 + 2848.6 |
0.13 |
|
Interdelivery interval (mos) |
51.24 + 35.40 |
56.54 + 39.34 |
0.01* |
|
Gestational age (mos) |
37.84 + 2.38 |
37.72 + 2.07 |
0.3 |
|
Admission cervical dilatation (cm) |
3.99 + 2.82 |
1.84 + 1.96 |
<0.01* |
|
Previous CS indication |
<0.01* |
||
|
Cephalopelvic / Fetopelvic Disproportion |
44 |
803 |
|
|
Non-reassuring Fetal Status |
130 |
398 |
|
|
Malpresentation |
167 |
362 |
|
|
Placenta Previa |
21 |
95 |
|
|
Deteriorating Maternal Status |
20 |
159 |
|
|
Repeat Cesarean Section / Scarred |
23 |
192 |
|
|
Twin Gestation |
3 |
12 |
|
|
Fetal Congenital Anomalies |
8 |
14 |
|
|
Failure of Induction |
5 |
12 |
|
|
Infectious causes |
0 |
7 |
|
|
Others |
3 |
6 |
Table 1: Demographic and obstetric characteristics of Filipino gravidas who underwent trial of labor after cesarean section (TOLAC) C (n=2,485)
|
Characteristics |
Successful VBAC n=235 |
Failed VBAC n=2,250 |
p- value |
|
Age (years) |
28.74 + 5.77 |
29.70 + 5.95 |
0.02* |
|
Maternal weight (kg) |
61.69 + 9.95 |
65.02 + 11.61 |
<0.01* |
|
Maternal BMI (kg/m2) |
26.27 + 4.24 |
27.68 + 4.77 |
<0.01* |
|
Fetal weight (g) |
2839.6 + 514.7 |
2866.8 + 532.9 |
0.46 |
|
Interdelivery interval (mos) |
47.20 + 31.62 |
56.51 + 39.31 |
<0.01* |
|
Gestational age (mos) |
38.00 + 2.66 |
37.71 + 2.06 |
0.05 |
|
Admission cervical dilatation (cm) |
5.20 + 2.61 |
1.89 + 2.00 |
<0.01* |
|
Previous CS indication |
<0.01* |
||
|
Cephalopelvic / Fetopelvic Disproportion |
23 |
824 |
|
|
Non-reassuring Fetal Status |
62 |
466 |
|
|
Malpresentation |
111 |
418 |
|
|
Placenta Previa |
15 |
101 |
|
|
Deteriorating Maternal Status |
14 |
165 |
|
|
Repeat Cesarean Section / Scarred |
3 |
212 |
|
|
Twin Gestation |
0 |
15 |
|
|
Fetal Congenital Anomalies |
4 |
18 |
|
|
Failure of Induction |
2 |
15 |
|
|
Infectious Causes |
0 |
7 |
|
|
Others |
1 |
8 |
Table 2:Demographic and obstetric characteristics of Filipino gravidas who underwent successful and failed vaginal birth after cesarean section (VBAC) (n=2,485)
Patients with successful VBAC are significantly younger, had less weight and body mass index, shorter interdelivery intervals, and admitted in active phase cervical dilatation, compared to those who had failed VBAC / underwent ERCS. Previous cesarean section indication was also significantly different between the two groups. Gestational age on delivery and estimated fetal weight did not seem to contribute to successful VBAC. These observations are consistent to those patients who decided to undergo TOLAC as well. (Table 3)
Taking all factors simultaneously, the adjusted analysis showed that only interdelivery interval, cervical dilatation at admission, and successful TOLAC significantly increased the likelihood of successful VBAC. Interdelivery interval was found to be a significant factor affecting the odds of successful VBAC, but the actual effect might not be clinically significant (adjusted OR=0.99, 95% CI=0.99-1.00). Maternal age, weight and body mass index were found to be independent predictors of successful VBAC in the pairwise unadjusted bivariate logistic regression analysis, but not in the adjusted analysis where all factors are taken simultaneously. Finally, fetal weight, gestational age and previous cesarean indication do not affect the odds of successful VBAC. (Table 3)
|
Factors |
Unadjusted Analysis |
Adjusted Analysis |
||
|
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
|
Maternal age (y) |
0.97 (0.95-0.99) |
0.01* |
1.01 (0.98-1.04) |
0.47 |
|
Maternal weight (kg) |
0.97 (0.96-0.99) |
<0.01* |
0.99 (0.96-1.02) |
0.68 |
|
Maternal BMI (kg/m2) |
0.93 (0.90-0.96) |
<0.01* |
0.96 (0.89-1.03) |
0.29 |
|
Fetal weight (g) |
1.00 (1.00-1.00) |
0.46 |
NS |
NS |
|
Interdelivery interval (m) |
0.99 (0.99-1.00) |
<0.01* |
0.99 (0.99-1.00) |
0.03* |
|
Gestational age (w) |
1.07 (1.00-1.16) |
0.05 |
NS |
NS |
|
Cervical dilatation at admission (cm) |
1.62 (1.52-1.70) |
<0.01* |
1.46 (1.37-1.55) |
<0.01* |
|
Previous CS Indication |
NS |
NS |
||
|
Cephalopelvic / Fetopelvic |
0.23 (0.03-1.94) |
0.18 |
||
|
Disproportion Non-reassuring Fetal |
1.06 (0.13-8.65) |
0.95 |
||
|
Malpresentation |
2.12 (0.26-17.16) |
0.48 |
||
|
Previa |
1.19 (0.14-10.18) |
0.88 |
||
|
Deteriorating Maternal Status |
0.68 (0.08-5.82) |
0.72 |
||
|
Repeat CS/ Scarred |
0.11 (0.01-1.21) |
0.07 |
||
|
Twin Gestation |
N/A |
|||
|
Fetal MCA |
1.78 (0.17-18.53) |
0.63 |
||
|
Failure of Induction |
0.50 (0.03-9.08) |
0.64 |
||
|
Infectious Cases |
N/A |
|||
|
Others |
N/A |
|||
|
Successful TOLAC |
18.12 (13.32-24.66) |
<0.01* |
10.88 (7.78-15.22) |
<0.01* |
Table 3: Factors associated with successful VBAC in Filipino gravidas (n=2,485)
Previous cesarean indication was not a significant variable in the adjusted analysis affecting VBAC success, but is crucial in counselling patients contemplating TOLAC and VBAC. Comparing patients offered TOLAC and those with successful VBAC, the success rates were significantly different for the following previous cesarean section indications (in decreasing frequency): (1) malpresentation (66.47%), (2) cephalopelvic / fetopelvic
disproportion (52.27%), (3) non-reassuring fetal status (47.69%), and (4) scarred uterus (13.04%). This suggests that a trial of labor and vaginal birth may be offered with some measure of success in patients with these previous cesarean section indications. (Table 4)
|
TOLAC |
Successful VBAC (+) |
p-value |
|
|
Cephalopelvic / Fetopelvic Disproportion |
44 |
23 |
<0.01* |
|
Non-reassuring Fetal Status |
130 |
62 |
<0.01* |
|
Malpresentation |
167 |
111 |
<0.01* |
|
Placenta Previa |
21 |
15 |
0.32 |
|
Deteriorating Maternal Status |
20 |
14 |
0.3 |
|
Repeat Cesarean Section / Scarred |
23 |
3 |
<0.01* |
|
Twin Gestation |
3 |
0 |
0.08 |
|
Fetal Congenital Anomalies |
8 |
4 |
0.25 |
|
Failure of Induction |
5 |
2 |
0.26 |
|
Infectious Causes |
0 |
0 |
- |
|
Others |
3 |
1 |
0.32 |
Table 4: TOLAC and VBAC success rates of Filipino gravidas according to previous cesarean section indication (n=2,485)
Neonatal outcomes (APGAR 1st and 5th minute scores, admission to the neonatal ICU) and maternal adverse outcomes (uterine rupture, postpartum hemorrhage, peripartum hysterectomy) of successful and failed VBAC were not significantly different from one another. No significant additional morbidity is incurred in choosing one delivery route over another. (Table 5)
|
Outcomes |
Successful |
Failed VBAC |
p-value |
|
APGAR score (1st minute) |
8.80 + .97 |
8.83 + .87 |
0.62 |
|
APGAR score (5th minute) |
8.93 + .52 |
8.93 + .52 |
0.98 |
|
Neonatal ICU admission |
284 |
20 |
0.07 |
|
Uterine rupture |
0 |
2 |
0.65 |
|
Postpartum Hemorrhage |
0 |
0 |
N/A |
|
Peripartum Hysterectomy |
0 |
6 |
0.43 |
Table 5: Maternal and perinatal outcomes of successful and failed VBAC in Filipino gravidas (n=2,485)
Discussion
TOLAC and VBAC are routinely offered to all patients in the Philippine General Hospital during their prenatal consult at the outpatient department. Filipina women consulting in the Philippine General Hospital outpatient clinic with a singleton pregnancy, in cephalic presentation and one previous lower segment cesarean section for non-recurrent cause (fetal distress, placenta previa, post-term pregnancy, failed induction of labor, malpresentation, and malposition) are inclusion criteria for a trial of labor. Women with previous upper segment cesarean, previous myomectomy or uterine surgery, placenta previa, twin gestation, severe medical disorders, intrauterine growth restriction, estimated fetal weight greater than 3.5 kg, and post-term pregnancy (≥42 weeks) are advised against trial of labor. Unless one mode of delivery is indicated over another, women may be offered a choice between an elective repeat cesarean section (ERCS) or vaginal birth after cesarean section (VBAC) which can be discussed as early as the first antenatal visit. [8]
The VBAC rate is dependent on the number of women with a prior cesarean attempting TOLAC, and the success rates among women with TOLAC. [4] Successful TOLAC leading to VBAC has a rate between 60-80% according to American College of Obstetricians and Gynecologists. (2) In the Royal College of Obstetrics and Gynecology (RCOG) guidelines, the success rate of planned VBAC is specified at 72-75%. [21] A cross-sectional study in Iran has reported a VBAC success rate as high as 91%. [20] In a retrospective review in Taiwan, 26.35% choose TOLAC with an 84.93% VBAC success rate. [25] In a retrospective cohort in a tertiary teaching hospital in Thailand, 355/592 (60%) had a successful VBAC and 237/592 (40%) had a failed TOLAC. [24] Finally, a local Philippine study by Malla and Co in 2015 has shown a VBAC success rate of 85.4% in a tertiary hospital in Manila. Failed TOLAC resulting in emergency repeat cesarean section amounted to 14.6% of patients, with fetal distress as the most common indication. [18] In our retrospective cohort, 17% (95% CI: 15.6% - 18.6%) had a TOLAC and only 9.5% (95% CI: 8.3% - 10.7%) having successful VBAC, which reflects a 55.88% VBAC success rate for those who decided to undergo TOLAC. The failed VBAC / ERCS overall rate is quite high in our retrospective cohort at 90.5% (95% CI: 89.3% - 91.7%). The success rate of our cohort is less than the average 60-80% prescribed by ACOG. There is a need to offer more TOLAC in our obstetric patients and identify factors that will increase the VBAC success rate. [11] Several retrospective cohorts have been done in various institutions with fairly similar results but evidence is still conflicting as to what factors / determinants constitute VBAC success. [1,5,6,8, 16,24]. The oldest local Philippine data published is the prospective study of Arandia et al which has shown that at the obstetric outpatient service of a tertiary institution, 58 patients met the criteria for TOLAC, 32 (55%) underwent TOLAC, and 28 (87%) achieved VBAC. There was no maternal mortality or perinatal mortality attributed to VBAC with fewer postpartum complications and shorter hospital stays. [3] In the most recent meta-analysis by Wu et. al in 2019, factors associated with statistically significant likelihood of successful VBAC were: previous vaginal birth before cesarean section, previous VBAC, Bishop score at admission before delivery, fetal malpresentation as the indication for previous cesarean section, and white race [27]. These findings are similarly reflected in the retrospective cohort study, as cervical dilatation and fetal malpresentation were included as the factors increasing the likelihood of successful VBAC. On the other hand, factors decreasing likelihood of VBAC were: age, body mass index, diabetes, hypertensive disorders complicating pregnancy, macrosomia, labor induction, Black race (compared to white), Asian race (compared to white), Latina race (compared to white), and indications of previous cesarean section including cephalopelvic disproportion, dystocia and failed induction. [27] In contrast to our retrospective cohort, age and body mass index were significant factors in promoting VBAC success in the unadjusted analysis. In terms of cesarean section indication, cephalopelvic disproportion was considered to increase likelihood of VBAC success. Finally, maternal medical comorbidities were excluded from this study. Finally, factors that do not increase or decrease likelihood of VBAC success are: smoking, interdelivery interval, gestational age, epidural anesthesia, and indications of cesarean section including fetal distress, hypertensive disorders complicating pregnancy, and suspected macrosomia. [27] In our retrospective cohort, interdelivery interval was a factor identified in VBAC success and fetal distress confers significant likelihood of VBAC success. Identification of factors constituting VBAC success allows opportunity to select patients for VBAC and provides clinical evidence to the obstetrician for prenatal VBAC counselling, avoiding elective / emergency repeat cesarean section and its associated risks.
Factors associated with VBAC rates can be broadly categorized into four main groups: socioeconomic determinants of health, demographic and medical factors impacting pregnancy and birth, behavioral factors, and geographic access. These predictors at the population level are useful for developing appropriate national guidelines which can then be individualized at the patient-provider level. [4] Historical factors (such as a history of vaginal birth or indications of the previous cesarean section such as cephalopelvic disproportion or failed induction) can help identify VBAC candidates even if some of the conditions might not be present in the current pregnancy. [27] Previous indications of cesarean delivery and labor characteristics are also important determinants of VBAC success however, the evidence is conflicting. [15] Brill and Windrim state that non-recurrent indications for previous cesarean section is associated with a higher successful VBAC rate ~ 81% (132/163) than recurrent indications, such as cephalopelvic disproportion, which had a 77% (84/109) VBAC success rate [6] Landon et al has stated that there is an independent effect of previous cesarean indication of subsequent labor success rates, with the highest success rate (84%) reported for malpresentation. [15] In a retrospective cohort study in China, 84.0% (1686/2006) of women who planned for TOLAC had VBAC. Indications for repeat cesarean sections were maternal request and/or from their family members (44.4%), fetal distress (19.7%), abnormal stage of labor (18.4%), failed induction of labor (10.9%), and others (6.6%). [16]
The ACOG Practice Guidelines in 2010 state that VBAC success rates according to a prior indication of CS are as follows: 75% (malpresentation), 60% (fetal distress), and 54% (failure to progress or cephalopelvic disproportion). (25) In the recent metanalysis of Wu et al (2019), fetal malpresentation as the indication for previous cesarean section was associated with VBAC success while cephalopelvic disproportion, dystocia and failed induction as the indications for previous cesarean section were associated with failed VBAC. Indications for previous cesarean section such as fetal distress, hypertensive disorders, and suspected fetal macrosomia did not affect VBAC success rates. [27] In our adjusted analysis of our retrospective cohort, the previous cesarean section was not determined to be a significant factor affecting VBAC success. In our cohort, when we compared those who underwent TOLAC and those with successful VBAC, the following previous cesarean indications had statistically significant success rates (1) malpresentation (66.47%), (2) cephalopelvic / fetopelvic disproportion (52.27%), (3) non-reassuring fetal status (47.69%), and (4) scarred uterus (13.04%). These findings support the findings found in the recent literature.
The benefits of VBAC compared to ERCS include avoidance of major abdominal surgery, less blood transfusion and lower rates of postpartum hemorrhage, bowel-bladder injury, peripartum hysterectomy, thromboembolism, postpartum infection, and an overall shorter recovery period. (2) Significant differences in neonatal intensive care unit admission and neonatal resuscitation (6.8% vs. 57.1% p = 0.002), birthweight upon delivery (2940±768 grams vs. 3764±254 grams p < 0.007), and successful breastfeeding (95.8% vs. 42.9% p = 0.002) was observed when comparing women who underwent VBAC versus ERCS in a cohort in Iran. [20] In contrast, when high-risk women with comorbidities were compared to low-risk women who underwent TOLAC and successful VBAC, there were no significant differences in maternal and neonatal morbidities such as blood transfusion, uterine rupture, unplanned hysterectomy, or admission to the intensive care unit. [22] Similar to our retrospective cohort, no significant neonatal and maternal morbidities were identified when comparing route of delivery (VBAC and ERCS) regardless of maternal condition. This contrasts the American College of Obstetricians and Gynecologists (ACOG) advise which cautioned that maternal and neonatal morbidities are increased in failed TOLAC that led to ERCS compared to VBAC. (2) Therefore, careful selection of women most likely to achieve VBAC could prevent maternal- neonatal complications associated with elective / emergency repeat cesarean delivery [22]
Many investigators have attempted to use scoring systems to predict the odds of successful VBAC but have not been widely validated across populations and have not been shown to improve patient outcomes. [2,11] The Royal College of Obstetricians and Gynecologists (RCOG) has recommended the Implementation of a VBAC versus ERCS checklist or clinical pathway to facilitate best practices in antenatal counseling, shared decision-making, and documentation. (21) Such checklists may be crafted based on local population-based evidence and recent available evidence. Demographic and maternal characteristics, prior patient experiences and psyche, and physician counseling all play a role in decision making regarding the route of delivery of patients with a previous cesarean section.
[19]There is no definite “decision discriminatory point” set when to choose one route over another in eligible individuals but those with at least 60-70% probability of undergoing successful TOLAC and VBAC experience more or less the same possible maternal-fetal morbidities as those who undergo repeat elective or emergency cesarean section. [2]
Conclusion
Better identification of women with the highest risk of failure of VBAC must be screened during the prenatal visits to provide appropriate advise and expectation management. [15] The discrepancy between the patient perspective and the clinical information from the provider requires careful consideration to ensure that shared decision making on the likelihood of successful VBAC is consistent with the values and preferences of the individual patient and supported by the best current evidence. [13,14] A balance of least risk and most possible benefit should be acceptable to both the patient and the obstetrician, in consideration of possible future pregnancies. [2] The findings of the cohort study may be utilized in the antenatal counselling of patients desiring TOLAC and VBAC. This study provides local evidence and valuable perspective in success factors which influence our counselling and eventual management of patients with a previous cesarean section.
Author Contribution
The entire content of this manuscript and the approval of this submission is accepted to be the responsibility of all of the authors.
Disclosure of Conflict of Interest
The author declares no conflict of interest.
Ethical approval
The conducted research is not related to either human or animals use.
Acknowledgements
I offer my sincerest acknowledgment to Ms. Katrina Sanchez, my research assistant from the UP-PGH Department of Obstetrics and Gynecology and Mr. Dan Louie Renz P. Tating, MS (cand), RN of Nightingale Research Solutions for the statistical analysis and guidance in this research paper
References
- Abdelazim, I A, Elbiaa, A A M, Al-Kadi, M, Yehia, A H, Nusair, B M S, & Faza, M A. Maternal and obstetrical factors associated with a successful trial of vaginal birth after cesarean section. Journal of the Turkish German Gynecological Association, (2014); 15(4); 245–249.
- ACOG Practice Bulletin No. 205. (2019) Obstetrics & Gynecology, 133(2); e110– e127.
- Arandia R F, Vergara M M, & Ragasa, L R.The outcome of the planned trial of labor following one previous low transverse cesarean section: A six-month experience. Philippine Journal of Obstetrics and Gynecology, (1991); 15(4), 235-242.
- Attanasio L B, & Paterno M T. Correlates of Trial of Labor and Vaginal Birth After Cesarean in the United States. Journal of Women’s Health (2019).
- Birara M, Gebrehiwot Y. Factors associated with the success of vaginal birth after one caesarean section (VBAC) at three teaching hospitals in Addis Ababa, Ethiopia: a case-control study. BMC Pregnancy Childbirth 13, 31(2013).
- Brill Y, & Windrim R. Vaginal Birth After Caesarean Section: Review of Antenatal Predictors of Success. Journal of Obstetrics and Gynaecology Canada, (2003); 25(4), 275–286.
- Davidson C, Bellows P, Shah U, et al., Outcomes associated with a trial of labor after cesarean in women with one versus two prior cesarean deliveries after a change in clinical practice. guidelines in an academic hospital. The Journal of Maternal-Fetal & Neonatal Medicine, (2018); 1–121.
- Fitzpatrick K E, Kurinczuk J J, Bhattacharya S, Quigley M A. Planned mode of delivery after previous cesarean section and short-term maternal and perinatal outcomes: A population-based record linkage cohort study in Scotland. PLoS Med. 2019;16(9):e1002913.
- Fox N S, Namath A G, Ali M, et al., Vaginal birth after cesarean delivery for arrest of descent. The Journal of Maternal-Fetal & Neonatal Medicine, (2018); 1–5.
- Garcia-Tansengco, M. Effective repeat cesarean section versus trial of labor after a previous cesarean section: A cost-effectiveness analysis. Philippine Journal of Obstetrics and Gynecology, (2001); 25(1); 1-8.
- Grisaru-Granovsky S, Bas-Lando M, Drukker L, et al., Epidural analgesia at the trial of labor after cesarean (TOLAC): a significant adjunct to successful vaginal birth after cesarean (VBAC). Journal of perinatal medicine, (2018); 46(3); 261–269.
- Guise J M, Denman M A, Emeis C, et al., Vaginal Birth After Cesarean. Obstetrics & Gynecology, (2010); 115(6); 1267–1278.
- Jessica Dy, Sheri De Meester, Hayley Lipworth, Jon Barrett, No. 382-Trial of Labour After Caesarean, Journal of Obstetrics and Gynecology Canada, Volume 41, Issue 7, 2019.
- Kaimal A J, Grobman W A, Bryant A, et al., The association of patient preferences and attitudes with the trial of labor after cesarean. Journal of Perinatology (2019).
- Landon M B, Leindecker S, Spong C Y, et al., The MFMU Cesarean Registry: factors affecting the success of trial of labor after previous cesarean delivery. American Journal of Obstetrics and Gynecology, (2005); 193(3); 1016–1023.
- Li Y X, Bai Z, Long, D J, et al., Predicting the success of vaginal birth after caesarean delivery: a retrospective cohort study in China. BMJ Open, 9(5), e027807 (2019).
- Magante C V.A questionnaire-based cross-sectional study obstetricians' knowledge, attitudes, and practices of vaginal birth after cesarean (VBAC) in the Philippines. The Health Sciences Journal, (2015); 4(1); 1-9
- Malla A P, and J.T. Co. Maternal and neonatal outcomes associated with a trial of labor after prior cesarean delivery in a tertiary hospital: A retrospective study. Department of Obstetrics-Gynecology - Jose R. Reyes Memorial Medical Center (2015).
- Metz T D, Stoddard G J, Henry E, et al., How do good candidates for a trial of labor after cesarean (TOLAC) who undergo elective repeat cesarean differ from those who choose TOLAC?. American Journal of Obstetrics and Gynecology, (2013); 208(6), 458.e1–458.e4586.
- Mirteymouri M, Ayati S, Pourali L, Mahmoodinia M, Mahmoodinia M. Evaluation of Maternal-Neonatal Outcomes in Vaginal Birth After Cesarean Delivery Referred to Maternity of Academic Hospitals. J Family Reprod Health. 2016; 10(4): 206-210.
- RCOG: Birth after Previous Caesarean Birth (Green-top Guideline No. 45). Green-top Guideline No 45 October 2015.
- Regan J, Keup C, Wolfe K, et al., Vaginal birth after cesarean success in high-risk women: a population-based study. Journal of Perinatology, (2014); 35(4), 252–257.
- Shipp T O, Zelop C M, Repke J T, e t al: Interdelivery interval and risk of symptomatic uterine rupture. Obstet Gynecol (2001); 97; 1-75.
- Thapsamuthdechakorn A, Sekararithi R, Tongsong T. Factors Associated with Successful Trial of Labor after Cesarean Section: A Retrospective Cohort Study. Journal of Pregnancy, 2018; 1-5.
- Tsai H T, & Wu, C H. (2017). Vaginal birth after cesarean section—The world trend and local experience in Taiwan. Taiwanese Journal of Obstetrics and Gynecology, 56(1), 41–45.
- World Health Organization (WHO) recommendations non-clinical interventions to reduce unnecessary cesarean sections. Geneva: World Health Organization; 2018. License: CC BY-NC-SA 3.0 IGO.
- Wu Y, Kataria Y, Wang, Z, et al., Factors associated with successful vaginal birth after a cesarean section: a systematic review and meta- analysis. BMC Pregnancy and Childbirth, (2019); 19(1).
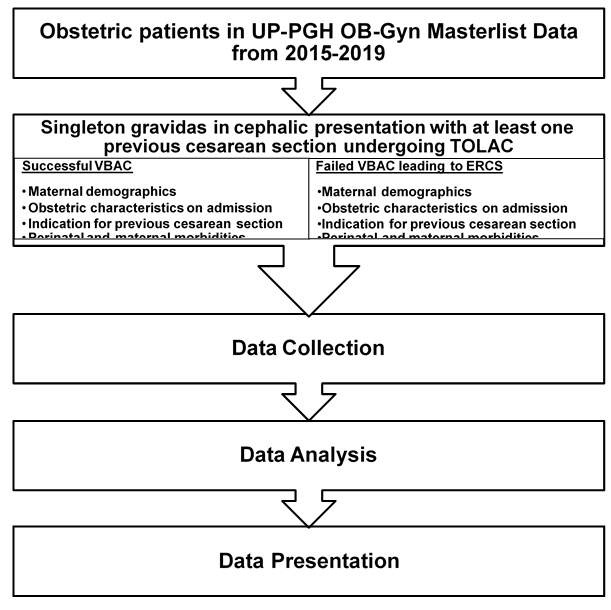
Figure 1: Workflow Process of the Study
