Spinal Anesthesia in a Healthy Parturient Causing Suspicious Bullous Skin Lesions: A Case Report
Article Information
Cynthia Karam1†, Roland Kaddoum2†, Nancy Abou Nafeh3, Carine Zeeni4, Fatima Msheik El-Khoury5, Amro Khalili6*
1Cynthia Karam, MD, Assistant Professor, Department of Anesthesiology and Pain Medicine, American University of Beirut Medical Center, Beirut, Lebanon
2Roland Kaddoum, MD, Associate Professor, Department of Anesthesiology and Pain Medicine, American University of Beirut Medical Center, Beirut, Lebanon
3Nancy Abou Nafeh, MD, Clinical Instructor of Anesthesiology, Department of Anesthesiology and Pain Medicine, American University of Beirut Medical Center, Beirut, Lebanon
4Carine Zeeni, MD, Associate Professor, Department of Anesthesiology and Pain Medicine, American University of Beirut Medical Center, Beirut, Lebanon
5Fatima Msheik El-Khoury, MBA, PhD, Clinical Instructor of Anesthesiology, Department of Anesthesiology and Pain Medicine, American University of Beirut Medical Center, Beirut, Lebanon
6Amro Khalili, MD, Clinical Instructor of Anesthesiology, Department of Anesthesiology and Pain Medicine, American University of Beirut Medical Center, Beirut, Lebanon
†Cynthia Karam and Roland Kaddoum equally contributed to the case report as first authors
*Corresponding Author: Amro Khalili, MD, Clinical Instructor of Anesthesiology, Department of Anesthesiology and Pain Medicine, B-floor, American University of Beirut Medical Center (AUBMC), American University of Beirut (AUB), Hamra, Beirut, Lebanon.
Received: 19 May 2023; Accepted: 30 May 2023; Published: 12 June 2023
Citation: Cynthia Karam, Roland Kaddoum, Nancy Abou Nafeh, Carine Zeeni, Fatima Msheik El-Khoury, Amro Khalili. Spinal Anesthesia in a Healthy Parturient Causing Suspicious Bullous Skin Lesions: A Case Report. Archives of Clinical and Medical Case Reports. 7 (2023): 257-260.
Share at FacebookAbstract
We present a case of suspicious bullous skin lesions after spinal anesthesia in a previously healthy parturient presenting at term for an elective secondary cesarean section. On day 1 post-partum, pruritic red fluid-filled clustered bullae highly resembling those of bullous pemphigoid were noted around the spinal anesthesia injection site.
Fusidic acid/betamethasone skin cream was prescribed by a dermatologist for twice-daily application. The bullae decreased in size gradually and became crusted 1 week post-partum with mild residual pruritus. At 6 weeks post-partum, the bullae completely disappeared without a scar. Checking the site of neuraxial blockade on the first day postoperatively allowed early detection of such unique skin lesions.
Keywords
Bullous Dermatoses; Bullous Pemphigoid; Contact Dermatitis Bullous Variants; Spinal Anesthesia
Bullous Dermatoses articles; Bullous Pemphigoid articles; Contact Dermatitis Bullous Variants articles; Spinal Anesthesia articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Bullous Dermatoses articles Bullous Dermatoses Research articles Bullous Dermatoses review articles Bullous Dermatoses PubMed articles Bullous Dermatoses PubMed Central articles Bullous Dermatoses 2023 articles Bullous Dermatoses 2024 articles Bullous Dermatoses Scopus articles Bullous Dermatoses impact factor journals Bullous Dermatoses Scopus journals Bullous Dermatoses PubMed journals Bullous Dermatoses medical journals Bullous Dermatoses free journals Bullous Dermatoses best journals Bullous Dermatoses top journals Bullous Dermatoses free medical journals Bullous Dermatoses famous journals Bullous Dermatoses Google Scholar indexed journals Bullous Pemphigoid articles Bullous Pemphigoid Research articles Bullous Pemphigoid review articles Bullous Pemphigoid PubMed articles Bullous Pemphigoid PubMed Central articles Bullous Pemphigoid 2023 articles Bullous Pemphigoid 2024 articles Bullous Pemphigoid Scopus articles Bullous Pemphigoid impact factor journals Bullous Pemphigoid Scopus journals Bullous Pemphigoid PubMed journals Bullous Pemphigoid medical journals Bullous Pemphigoid free journals Bullous Pemphigoid best journals Bullous Pemphigoid top journals Bullous Pemphigoid free medical journals Bullous Pemphigoid famous journals Bullous Pemphigoid Google Scholar indexed journals Survey articles Survey Research articles Survey review articles Survey PubMed articles Survey PubMed Central articles Survey 2023 articles Survey 2024 articles Survey Scopus articles Survey impact factor journals Survey Scopus journals Survey PubMed journals Survey medical journals Survey free journals Survey best journals Survey top journals Survey free medical journals Survey famous journals Survey Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Dermatitis Bullous Variants articles Dermatitis Bullous Variants Research articles Dermatitis Bullous Variants review articles Dermatitis Bullous Variants PubMed articles Dermatitis Bullous Variants PubMed Central articles Dermatitis Bullous Variants 2023 articles Dermatitis Bullous Variants 2024 articles Dermatitis Bullous Variants Scopus articles Dermatitis Bullous Variants impact factor journals Dermatitis Bullous Variants Scopus journals Dermatitis Bullous Variants PubMed journals Dermatitis Bullous Variants medical journals Dermatitis Bullous Variants free journals Dermatitis Bullous Variants best journals Dermatitis Bullous Variants top journals Dermatitis Bullous Variants free medical journals Dermatitis Bullous Variants famous journals Dermatitis Bullous Variants Google Scholar indexed journals Prussian Blue Administration articles Prussian Blue Administration Research articles Prussian Blue Administration review articles Prussian Blue Administration PubMed articles Prussian Blue Administration PubMed Central articles Prussian Blue Administration 2023 articles Prussian Blue Administration 2024 articles Prussian Blue Administration Scopus articles Prussian Blue Administration impact factor journals Prussian Blue Administration Scopus journals Prussian Blue Administration PubMed journals Prussian Blue Administration medical journals Prussian Blue Administration free journals Prussian Blue Administration best journals Prussian Blue Administration top journals Prussian Blue Administration free medical journals Prussian Blue Administration famous journals Prussian Blue Administration Google Scholar indexed journals Spinal Anesthesia articles Spinal Anesthesia Research articles Spinal Anesthesia review articles Spinal Anesthesia PubMed articles Spinal Anesthesia PubMed Central articles Spinal Anesthesia 2023 articles Spinal Anesthesia 2024 articles Spinal Anesthesia Scopus articles Spinal Anesthesia impact factor journals Spinal Anesthesia Scopus journals Spinal Anesthesia PubMed journals Spinal Anesthesia medical journals Spinal Anesthesia free journals Spinal Anesthesia best journals Spinal Anesthesia top journals Spinal Anesthesia free medical journals Spinal Anesthesia famous journals Spinal Anesthesia Google Scholar indexed journals
Article Details
List of Abbreviations:
Th2: T-Helper 2
1. Introduction
During pregnancy, bullae can occur secondary to either common skin disorders or specific dermatoses of pregnancy. A heterogenous group of pregnancy or postpartum related dermatoses include, however is not limited to, pemphigoid gestationis, polymorphic
eruption of pregnancy, dermatitis herpetiformis, erythema multiforme, and allergic contact dermatitis among others.
An accurate understanding of these conditions allows for proper management and follow-up of the patient. Some conditions have been associated with adverse obstetric outcomes, such as increased risk of prematurity and small-for-gestational-age babies seen in fetuses born to patients with pemphigoid gestationis, putting emphasis on the importance of making the correct diagnosis [1].
Although pregnancy induces an immunosuppressive state, a prevalent T-helper 2 (Th2) cellular profile can lead to an aggravation of bullous pemphigoid especially during the first and second trimesters. However, in the third trimester, the clinical picture can improve due to increased production of endogenous corticosteroids by the chorion [2]. We did an up-to-date review of all previous cases in the field trying to find a relationship between bullous pemphigoid-like lesions, pregnancy, and regional or neuraxial anesthesia, but we didn’t find such similar case presentations.
2. Case Presentation
A 31-year-old female, gravida 2, para 1, with a second pregnancy complicated by gestational hypertension and polyhydramnios, presented at 37 weeks and 3 days of gestational age for an elective secondary cesarean section. She was previously healthy with no known allergies and no reported personal or family history of dermatologic or autoimmune diseases.
Due to her obstetric history of gestational hypertension in the prior pregnancy, she was maintained throughout the current pregnancy on oral aspirin, 100 mg once daily, which was discontinued at 36 weeks of gestational age. She presented to the delivery suite on her scheduled day and received the usual preoperative anesthesia assessment and obstetric care. She was consented for spinal anesthesia. In the operating room and under sterile technique, scrubbing and draping of her back was done with 2% chlorhexidine gluconate (CHG) / 70% isopropyl alcohol (IPA) swabs and sterile drapes, respectively. Afterwards, the skin was infiltrated with 4 mL of 1% lidocaine. Then, using a 25-G Whitacre spinal needle, 12.5 mg of hyperbaric bupivacaine, 12.5 mcg of fentanyl, and 0.1 mg of intrathecal morphine were injected intrathecally, after CSF aspiration, at the level of L3-L4 intervertebral space at a needle depth of 5 cm, without inflicted skin trauma. The skin at the puncture site was then covered by a sterile latex-free transparent film dressing (3M Tegaderm TM Film). A spinal level was confirmed at the T6 dermatome. The patient tolerated the cesarean delivery very well. She left the operating room in a stable condition. Following two hours of close postoperative observation in the delivery suite, the patient was safely transferred to the postpartum ward.
On day 1 post-partum and upon general assessment by the nurse in charge, pruritic red fluid-filled clustered bullae, highly resembling those of bullous pemphigoid, were noted at the area around the spinal anesthesia injection site (Figure 1). Upon further assessment by the medical team, no similar or other skin lesions were noted on the rest of her body. She remained afebrile with stable vital signs. She denied other associated symptoms such as pain, burning sensation, or tenderness upon palpation of her skin lesions. Her serum white blood cell (WBC) count increased from a preoperative value of 10,400/μL to 16,300/μL, consistent with normal post-partum laboratory findings.

Figure 1: Spinal anesthesia injection site at day 1 post-partum.
On day 2 post-partum, no major changes occurred in her skin lesions except for a mild increase in their size. Upon consultation, the dermatologist initially described bullous pemphigoid-like lesions based on their clinical appearance, and thus requested skin biopsy and serologic tests for a definitive diagnosis. The patient refused to do so due to her fear that a skin biopsy, tissue cultivation, or further needle pricks for serologic tests might cause the eruption of more of her pruritic bullae. An infectious cause of her lesions was also suspected. Herpes Zoster was low on the differential due to the non-painful nature and the non-dermatomal distribution of her lesions. The possibility of a rare local injection site skin reaction to lidocaine infiltration or a contact dermatitis bullous variant was also low on the differential since the patient already had received a lidocaine skin infiltration at the dorsum of her hand during the insertion of her peripheral intravenous catheter, which was covered by the same sterile latex-free transparent film dressing (3M Tegaderm TM Film), and no such skin lesions were noticed. Also, no such skin lesions were noticed 3 years ago at the spinal anesthesia injection site after her first cesarean delivery.
Fusidic acid/betamethasone skin cream was prescribed by the dermatologist for a twice-daily application with close follow-up. The patient was discharged home on day 3 post-partum to continue fusidic acid/betamethasone skin cream application for a total of 10 days. After one week, follow up examination showed that her bullae decreased in size and became crusted with mild residual pruritus. Two weeks later, the patient reported sloughing of her bullae with no pruritus. However, a persistent brownish skin discoloration at the bullae site was noticed (Figure 2). Six weeks post-partum, her skin lesions completely disappeared with no persistent scarring.
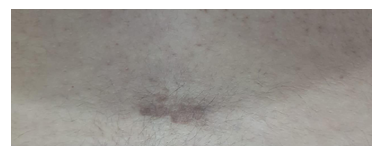
Figure 2: Spinal anesthesia injection site at 2 weeks post-partum.
3. Discussion and Conclusions
Bullous pemphigoid is an acquired, chronic, blistering, autoimmune, subepidermal bullous disease in which autoantibodies are directed against components of the basement membrane zone of the skin [2]. It is characterized by formation of bullae on the skin and mucous membranes. The pathogenesis involves migration of inflammatory cells into the subepithelial tissues due to activation of complements caused by antigen-antibody reaction. The incidence of bullous pemphigoid is 6-7 cases per million population per year in the western world. It usually involves elderly more than 60 years of age and is rare in children, although childhood bullous pemphigoid has been described [3]. One of the variants of the disease is cicatricial pemphigoid, which commonly involves mucous membranes of the oropharynx, conjunctiva, nasopharynx, larynx, esophagus, genitalia, and anus. Bullous eruptions are usually followed by scarring [4].
The clinical course of the disease is one of exacerbations and remissions. The diagnosis is based on clinical presentation, histopathological analysis, direct and indirect immunofluorescence microscopy on perilesional skin, analysis of staining patterns, and characterization of circulating autoantibodies [5]. There have been several reports of its association with other autoimmune skin bullous diseases like pemphigus, pemphigoid, epidermolysis bullosa acquisita, dermatitis herpetiformis (Duhring disease), linear immunoglobulin-A disease, and multiple autoimmune syndrome [6]. The relationship between bullous pemphigoid and malignancy is a matter of debate.
Despite several published case reports, there is no definite association. Ogawa et al., found a significantly higher incidence of malignancy in bullous pemphigoid patients in Japan [7]. Other authors from other countries in Asia have also reported a higher incidence of malignancy in these patients [8], however other studies done on Caucasian patients have failed to prove any statistically significant association. Treatment is with corticosteroids, immunosuppressive agents, and occasionally antibiotics if an associated secondary bacterial infection develops [9].
There are no definite recommendations for either general or neuraxial anesthesia in bullous pemphigoid patients. Use of neuraxial anesthesia in these patients is controversial, the reason being that blister formation can occur at the site of needle insertion. In case of epidural anesthesia, fixation of the epidural catheter on the skin may be difficult. However, neuraxial and regional anesthesia have been described for surgeries in these patients, as it avoids general anesthesia and airway instrumentation [10, 11]. The use of adhesive tape to secure the epidural catheter to an area of skin should be avoided. Spinal anesthesia has been described for cesarean sections while avoiding local anesthetic skin infiltration at the site of spinal needle insertion because of the risk of bullae formation and skin sloughing [12]. In case of spinal needle insertion, an area devoid of skin lesions should be chosen. Also, skin infection at the site of local anesthetic injection is possible, which may lead to subsequent sepsis.
A choice of an area devoid of skin lesions is thus recommended and considered safe for performing spinal anesthesia [12]. Several published case reports showed that a single shot spinal anesthetic is safe for cesarean sections, however general anesthesia is not contraindicated if the oral mucosa is not involved with bullae [12]. Neuraxial opioids, especially intrathecal morphine, are preferably avoided in these patients as they are associated with pruritus [13]. Much is yet to be determined in terms of the association between spinal anesthesia, pregnancy, and bullous skin diseases. Our patient did not have any personal or family history of dermatologic or autoimmune diseases. She had previously received spinal anesthesia with lidocaine skin infiltration during her first cesarean section without such unique complication. Still, there is the possibility of a very rare local injection site skin reaction to lidocaine infiltration or a contact dermatitis bullous variant developing for the first time in our patient. One limitation to all these postulations is the lack of diagnostic skin biopsy, tissue cultivation, or serologic tests for circulating autoantibodies confirming the diagnosis of bullous dermatoses.
In our opinion, it would be wise for all anesthesiologists to check the site of neuraxial block on the first day postoperatively, before discharging the patient. This can allow the early detection of such unique skin lesions, be it self-limiting or serious.
If a parturient patient presents with similar skin lesions after spinal anesthesia and has no known dermatologic or autoimmune diseases, we suggest expectant management of her skin lesions with close observation of any new onset signs and symptoms.
Declarations
Ethics Approval and Consent to Participate
The American University of Beirut Medical Center (AUBMC) Institutional Review Board (IRB) does not require its approval for the involvement of human participants in the publication of case reports.
Consent for Publication
Written informed consent was obtained from the patient for the publication of this case report.
Availability of Data and Materials
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Funding
None.
Authors' Contributions
Cynthia Karam and Roland Kaddoum have equal contribution to the case report as first authors in discussing and interpreting the case, drafting, and approving the final version of the manuscript.
Nancy Abou Nafeh, Carine Zeeni, and Fatima Msheik El-Khoury contributed to interpreting the case, drafting, and approving the final version of the manuscript. Amro Khalili contributed to discussing and interpreting the case, drafting, and approving the final version of the manuscript.
All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
References
- Shornick JK, Black MM. Fetal risks in herpes gestationis. J Am Acad Dermatol 26 (1992): 63-68.
- Kasperkiewiez M, Zilikens D. The pathophysiology of bullous pemphigoid. Clin Rev Allergy Immunol 33 (2007): 67-77.
- Wu KG, Chou CS, Hsu CL, et al. Childhood Bullous Pemphigoid: A Case Report and Literature Review. J Clin Exp Dermatol Res S6 (2013): 010.
- Fleming TE, Korman NJ. Cicatrical pemphigoid. J Am Acad Dermatol 43 (2000): 571-594.
- Di Zenzo G, Della Torre R, Zambruno G, Borradori L. Bullous pemphigoid: from the clinic to the bench. Clin Dermatol 30 (2012): 3-16.
- Ljubojevic S, Lipozencic J. Autoimmune bullous diseases associations. Clin Dermatol 30 (2012): 17-33.
- Ogawa H, Sakuma M, Morioka S, et al. The incidence of internal malignancies in pemphigus and bullous pemphigoid in Japan. J Dermatol Sci 9 (1995): 136-141.
- Fernandes J, Barad P, Shukla P. Association of Bullous Pemphigoid with Malignancy: A Myth or Reality? Indian J Dermatol 59 (2014): 390-393.
- Wojnarowska F, Kirtschig G, Highet AS, et al. British Association of Dermatologists. Guidelines for the management of bullous pemphigoid. Br J Dermatol 147 (2002): 214-221.
- Berryhi U RE. Skin and bone disorders. In: Katz J, Benumof J, Kadis LB, editors. Anesthesia and Uncommon Diseases, 3rd ed. Philadelphia: WB Saunders Co (1990): 668-672.
- Lavie CJ, Thomas MA, Fondak AA. The perioperative management of the patient with pemphigus vulgaris and villous adenoma. Cutis 34 (1984): 180-182.
- Abouleish EI, Elias MA, Lopez M, et al. Spinal anesthesia for cesarean section in a case of pemphigus foliaceous. Anesth Analg 84 (1997): 449-450.
- Mahajan R, Grover VK. Neuraxial opioids and Koebner phenomenon: Implications for anesthesiologists. Anesthesiology 99 (2003): 229-230.
