Single Coronary Artery Anomaly: Case Report
Article Information
Firas Ajam1*, Ndausung Udongwo2, Vandan Upadhyaya2, Bharath Sathya1, Daniel Kiss1
1Department of Cardiology, Jersey Shore University Medical Center, New Jersey, United States
2Department of Internal Medicine, Jersey Shore University Medical Center, New Jersey, United States
*Corresponding Author: Firas Ajam, Department of Cardiology, Jersey Shore University Medical Center, 1945 Route 33, Neptune, NJ 07712, USA
Received: 23 March 2021; Accepted: 31 March 2021; Published: 30 April 2021
Citation: Firas Ajam, Ndausung Udongwo, Vandan Upadhyaya, Bharath Sathya, Daniel Kiss. Single Coronary Artery Anomaly: Case Report. Cardiology and Cardiovascular Medicine 5 (2021): 272-276.
Share at FacebookAbstract
Single coronary anomaly is a rare congenital coronary artery disease where only one coronary artery arises from the aortic trunk, it could be an isolated finding or as part of other congenital cardiac diseases. We sought to present a patient with anginal symptoms was found to have single coronary artery.
Keywords
Absent right coronary artery, Ischemic heart disease, Congenital heart disease
Absent right coronary artery articles; Ischemic heart disease articles; Congenital heart disease articles
Article Details
1. Introduction
Single coronary artery anomaly is a rare congenital coronary artery disease, found as an isolated anomaly in approximately (0.024%-0.044%) [1]. The first case was reported by Thebesius in 1761 [2]. The first angiographic classification was proposed by Lipton et al in 1979, and modified in 1990 [1, 3].
2. Case Presentation
A 55-year-old male with a history of hypertension, hyperlipidemia, pulmonary embolism, former smoker for 12 years, and history of supraventricular tachycardia, who was sent for an elective cardiac catheterization. He’s been having recurrent episodes of retrosternal chest pain, lasting 10-15 minutes, exertional, relieved with rest, associated with shortness of breath, and no palpitations. Family history was remarkable for coronary artery disease. Patient denied any cough, fever or recent trauma. Home medications: metoprolol succinate (50mg daily) and aspirin (81mg daily). Vital signs: BP 168/96 mmHg, HR 70 bpm, temp 97 F. Physical examination was within normal limits. Electrocardiogram (EKG): normal sinus rhythm with a rate of 60 bpm, no ischmic changnes. Computed Tomography Cornoary Angiography showed non-obstructive calcified plaque in the mid left anterior descending artery (LAD) (coronary artery calcium score of 25.6 agatston units), the left circumflex artery (LCx) extending into the right coronary artery (RCA) territory and terminating near the right sinus of Valsalva, the RCA origin was unclear, with an absent ostium and proximal segment (Figure 1). Coronary angiography was recommended to evaluate if the patient had a dominant left circumflex artery (LCx), and an obstructed proximal RCA or an anomaly.
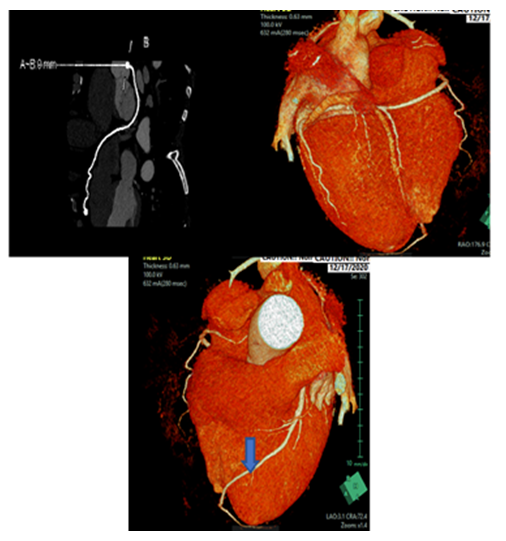
Figure 1: (A) CT Coronary Angiography showing the course of Left Circumflex (LCX) Artery; (B) CTA coronary reconstruction showing the course of Left Circumflex Artery; (C) CTA coronary reconstruction showing the course of the Left Anterior Descending (LAD) Artery.
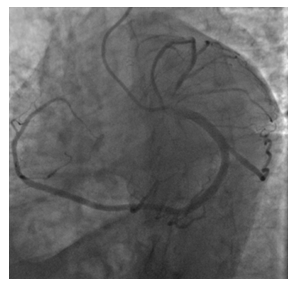
Figure 2: Left Anterior Oblique (LAO) coronary angiography showing the course of Left Circumflex artery (LCX).
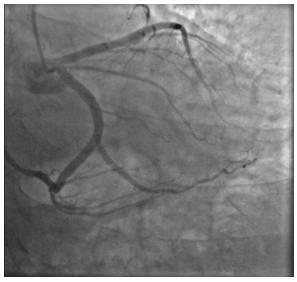
Figure 3: Right Anterior Oblique (RAO) coronary angiography of the LAD and LCX arteries.
Cardiac catheterization revealed the left coronary artery originating from the left ostium giving rise to the left anterior descending (LAD) and Left Circumflex (LCx) arteries. LCx gives rise to four obtuse mariginals (OMs) and continues in the atrioventricular (AV) groove and supplies the right coronary territory, giving off the posterior descending artery (PDA) and several acute marginals, several attempts were made to visualize the RCA and was deemed to be absent (Figures 2, 3). Overall, there were no hemodynamically significant coronary artery obstructions, only very mild coronary disease. The patient was managed medically and discharged in stable condition, and was scheduled for outpatient follow up.
3. Discussion
The incidence of SCA according to Lipton et al was 0.024% and according to Yamanaka and Hobbs was 0.044%. A retrospective analysis by Desmet et al. showed low incidence of associated congenital heart disease and suggested no association brtween SCA and certain other diseases [4]. In a study of 142 patients with an SCA and associated congenital heart disease, in 49% SCA arose from the right sinus of Valsalva (SoV), and 45% arose from the left SoV. Major congenital cardiac anomalies were reported in 41%, the most common anomalies were transposition of the great vessels, coronary artery fistula, improper division of the truncus arteriosus, tetralogy of Fallot and bicuspid aortic valve.
Lipton’s classification considers the beginning of the ostium from the sinus of Valsalva, anatomical path of the vessel, and the sequence of the transverse trunk. Alphabets R or L are used to identify the ostial origin of the vessel, roman numerals I, II, or III are used to represent the anatomical distribution of the vessel, and letters A, B, P, S, and C are used to outline the progression of the vessel with respect to the pulmonary artery and the aorta. The majority of patients are asymptomatic. However, around 15% might have ischemic heart disease directly triggered by the atypical anatomy of the arteries and not by coronary artery disease. Ischemic symptoms might range from exertional angina to sudden death in rare types.
Impaired myocardial perfusion can be related to anatomical malformations, including the acute angle take-off of the anomalous vessel, with a tapered slit-like orifice that breakdowns in a valve-like manner, thereby limiting the blood flow. Other anatomical structures responsible for ischemia are the proximal intramural course of the anomalous vessel, which is squeezed within the aortic wall, and the compression of the anomalous vessel along its path between the aorta and the pulmonary artery during exercise as both vessels get larger [5, 6]. Taylor et al observed the records of 242 deceased patients with remote congenital coronary anomalies and found that one-third of the patients had sudden cardiac death, and half of these were exercise-related deaths, with younger patients were obsereved to die suddenly during physical exertion (Taylor AJ, Rogan KM). Moreover, Basso et al. claim that (59%) of patients with SCA, died under the age of 30 years of age, mainly during exercise [6].
Coronary angiography is the gold standard to diagnose, assess and classify coronary anomalies, echocardiography can be used to detect any other associated structural heart diseases. Cardiovascular magnetic resonance (CMR) is an alternative, non-invasive tool, with the advantages of no radiation exposure, no body habitus limitations, and instantaneous assessment of cardiovascular structure and perfusion, it aslo provides high spatial and temporal resolutions [7]. Percutaneous Coronary Intervention (PCI) considered the gold starndartd for treatement, the abnormal source and path of coronary arteries might be challenging and could lead to complications in cannulation of the coronary ostium as well as technical difficulties in catheter support during
PCI [8, 9].
4. Conclusion
Single coronary anomaly is a rare congenital disease with wide variety of symptoms, ranging from anginal symptoms to sudden cardiac death. Multi-disciplinary approach should be used in evaluating those patients. Further studies are recommended to help in earlier diagnosis and management.
Funding
No funding or sponsorship was received for publication of this article.
Authorship
All named authors take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
References
- Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn 21 (1990): 28-40.
- Thebesius A. Dissertatio Medica de Circulo Sanguinis in Cordo. Ludg Batav, JA Langerak (1716).
- Halpenn IC, Penny JL, Kennedy RJ. Single coronary artery: Antemortem diagnosis in a patient with congestive heart failure. Am J Cardiol 19 (1967): 424-427.
- Desmet W, Vanhaecke J, Vrolix M, Van de Werf F, Piessens J, et al. Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J 13 (1992): 1637-1640.
- Angelini P. Coronary artery anomalies-current clinical issues: Definitions, classification, incidence, clinical relevance, and treatment guidelines. Tex Heart Inst J 29 (2002): 271-278.
- Basso C, Maron BJ, Corrado D, Thiene G. Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J A Coll Cardiol 35 (2000): 1493-1501.
- Rudan D, Todorovic N, Starcevic B, Raguz M, Bergovec M. Percutaneous coronary intervention of an anomalous right coronary artery originating from the left coronary artery. Wien Klin Wochenschr 122 (2010): 508-510.
- Çallskan M, Çiftçi Ö, Güllü H, Alpaslan M. Anomalous right coronary artery from the left sinus of Valsalva presenting a challenge for percutaneous coronary intervention. Turk Kardiyol Dern Ars 37 (2009): 44-47.
- Kafkas N, Triantafyllou K, Babalis D. An isolated single LI type coronary artery with severe LAD lesions treated by transradial PCI. J Invasive Cardiol 23 (2011): E216-E218.
