Severe Atypical Presentation of Uveitis Associated with Tubulointerstitial Nephritis
Article Information
Christina L. Kong1, Betul Bayraktutar2, Ralitsa Loewen1, Elizabeth Conner2, Eduardo V. Zambrano3, Lama Khatib2, Marie-Hélène Errera*, 1, 2
1University of Pittsburgh Medical Center, Department of Ophthalmology, Pittsburgh, Pennsylvania, USA
2Children’s Hospital of Pittsburgh, Department of Ophthalmology, Pittsburgh, Pennsylvania, USA
3University of Pittsburgh Medical Center, Department of Pathology, Pittsburgh, Pennsylvania, USA
*Corresponding author: Marie-Hélène Errera, University of Pittsburgh Medical Center, Department of Ophthalmology, Pittsburgh, Pennsylvania, USA
Received: 26 October 2022; Accepted: 02 November 2022; Published: 18 November 2022
Citation:
Christina L. Kong, Betul Bayraktutar, Ralitsa Loewen, Elizabeth Conner, Eduardo V. Zambrano, Lama Khatib, Marie-Hélène Errera. Severe Atypical Presentation of Uveitis Associated with Tubulointerstitial Nephritis. Journal of Ophthalmology and Research 5 (2022): 147-149.
Share at FacebookAbstract
Although tubulointerstitial nephritis with uveitis (TINU) is a rare disorder that represents only 1-2% of all uveitis cases in tertiary care settings, it remains a common diagnosis among children and adolescents [1, 2]. Among young individuals with uveitis, up to one-third may have TINU [1, 3]. The condition most often presents as an acute, bilateral, non-granulomatous anterior uveitis [4, 5]. However, TINU may present with findings beyond the anterior segment [1, 6, 7]. In this report, we present an example of such a case.
Keywords
TINU, PPV, tubulointerstitial
Article Details
1. Introduction
Although tubulointerstitial nephritis with uveitis (TINU) is a rare disorder that represents only 1-2% of all uveitis cases in tertiary care settings, it remains a common diagnosis among children and adolescents [1, 2]. Among young individuals with uveitis, up to one-third may have TINU [1, 3]. The condition most often presents as an acute, bilateral, non-granulomatous anterior uveitis [4, 5]. However, TINU may present with findings beyond the anterior segment [1, 6, 7]. In this report, we present an example of such a case.
2. Case Report
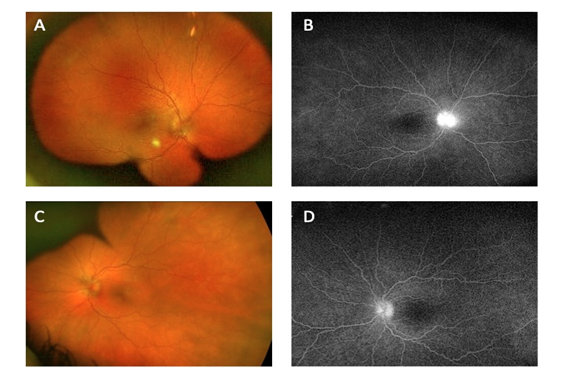
A 12-year-old otherwise healthy girl presented to our center as an urgent referral due to concern for active bilateral non-granulomatous anterior uveitis and bilateral Frisen grade 3 [8] optic disc edema. Her symptoms had started two months prior. She had been treated with prednisolone acetate drops with escalation to difluprednate drops without any significant improvement. She and her family denied any preceding symptoms including headache, fever, chills, joint pains, and rashes. On her initial evaluation, her best-corrected visual acuity was 20/25 in both eyes. Her clinical examination demonstrated 4+ cells in the anterior chamber with bilateral posterior synechiae and 360° blurring of the optic disc margin. Retina fluorescein angiography revealed dye leakage from both optic discs without retinal vessel leakage (Fig. 1).
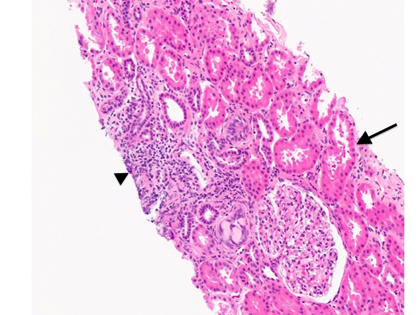
The diagnostic work-up included a normal complete blood count, a normal creatinine of 0.48 mg/dL (glomerular filtration rate = 138 ml/minute per 1.73 m2) and no protein or blood on urinalysis. Her beta-2-microglobulin level was elevated to 2,275 mcg/g (normal range < 132 mcg/g). She was therefore referred to the nephrology service and underwent a renal biopsy that demonstrated tubulointerstitial nephritis and mild tubular interstitial edema (Fig. 2). Given her constellation of symptoms, she was diagnosed with TINU and treated with intravenous methylprednisolone for 3 days due to the presence of disc edema and potential vascular occlusion.
On discharge, she was prescribed a regimen of oral prednisone 0.2 mg/kg twice a day, oral methotrexate 15 mg once a week, and subcutaneous adalimumab 40 mg once every 2 weeks. Her topical regimen was topical steroids and cycloplegic agents. At last follow-up at 3 months, the anterior uveitis was quiet and the papillitis had resolved with improvement in her beta-2-microglobulin level to 185 mcg/g. She remained on systemic immune modulatory therapy as well as a slow oral prednisone taper due to an increase in beta-2-microglobulin to 225 mcg/g during an attempt at a more rapid taper.
3. Discussion
In 1975, Dobrin et al. first described TINU as a disease that causes both interstitial nephritis and primarily a bilateral anterior uveitis [4]. In the initial criteria for TINU established by Mandeville et al. in 2001, TINU is categorized as “Definite”, “Probable”, and “Possible” based on the presentation of anterior uveitis as well pathologic and laboratory findings [5]. Since then, a total of almost 600 cases of TINU have been described in the literature [9]. This has helped clarify previously established understandings of this disease entity including its ocular findings.
While there is no known racial or ethnic predisposition, TINU does remain a more common diagnosis among individuals younger than 20 years old. For instance, Mackensen et al. found that TINU was nearly seven times more common in children and adolescents with a median age at diagnosis of 15 years old [1]. In most cases, TINU presents as an acute, bilateral, non-granulomatous anterior uveitis; however, recent studies have shown that TINU can also present with a myriad of findings in the posterior segment. In a review of 133 cases, Mandeville et al. found that 20% of patients with known ocular complications of TINU had optic disc edema [5, 10-16].
A recent retrospective study found posterior segment findings in 65% of 17 patients diagnosed with TINU. Among them, 41% had disc edema similar to the patient presented in this report, 24% had macular edema, and 12% had retinal vasculitis [6]. The case we describe here of optic disc edema in the setting of anterior uveitis serves as a reminder of the limitations of the initial diagnostic criteria for TINU and emphasizes the importance of keeping a broad differential diagnosis when uveitis patients present with posterior segment findings.
In the work-up for our patient, beta-2-microglobulin remained a key diagnostic marker. She presented with a normal creatinine without evidence of proteinuria or hematuria on urinalysis. Her elevated beta-2-microglobulin helped clarify her diagnosis and the renal biopsy provided definitive evidence. An elevated beta-2-microglobulin in combination with an elevated creatinine has a positive predictive value (PPV) of 100% for definite and probable TINU. An elevated beta-2-microglobulin alone has a PPV of 88% and negative predictive value of 97% [17]. This serum marker has also been shown to have a direct correlation with uveitis activity. One study found that beta-2-microglobulin has a stronger correlation with the degree of anterior chamber cell than creatinine does [18]. Though TINU is predominantly associated with anterior uveitis, posterior pole findings can be found and may be more common than previously thought. In such cases, it remains important to have a high degree of clinical suspicion for TINU and to utilize tests such as beta-2-microglobulin to help establish the diagnosis.
Conflicts of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
This work was supported by NIH CORE Grant P30 EY08098 to the Department of Ophthalmology of the Eye and Ear Foundation of Pittsburgh and by an unrestricted grant from Research to Prevent Blindness, New York, New York
References
- MacKensen F, Billing H. Tubulointerstitial nephritis and uveitis syndrome. Curr Opin Ophthalmol 20 (2009): 525-531.
- Kump LI, Cervantes-Castañeda RA, Androudi SN, Foster CS. Analysis of pediatric uveitis cases at a tertiary referral center. Ophthalmology 112 (2005): 1287-1292.
- Rosenbaum JT. Bilateral anterior uveitis and interstitial nephritis. Am J Ophthalmol 105 (1988): 534-537.
- Dobrin RS, Vernier RL, Fish AJ. Acute eosinophilic interstitial nephritis and renal failure with bone marrow-lymph node granulomas and anterior uveitis. A new syndrome. Am J Med 59 (1975): 325-333.
- Mandeville JTH, Levinson RD, Holland GN. The Tubulointerstitial Nephritis and Uveitis Syndrome. Surv Ophthalmol 46 (2001): 195-208.
- Koreishi AF, Zhou M, Goldstein DA. Tubulointerstitial Nephritis and Uveitis Syndrome: Characterization of Clinical Features 29 (2020): 1312-1317.
- Nagashima T, Ishihara M, Shibuya E, Nakamura S, Mizuki N. Three cases of tubulointerstitial nephritis and uveitis syndrome with different clinical manifestations. Int Ophthalmol 37 (2017): 753-759.
- Frisen L. Swelling of the optic nerve head: a staging scheme. J Neurol Neurosurg Psychiatry 45 (1982): 13.
- Petek T, Frelih M, Marcun Varda N. Tubulointerstitial nephritis and uveitis syndrome in an adolescent female: a case report. J Med Case Rep 15 (2021): 1-17.
- Sherman MD, Own KH. Interstitial nephritis and uveitis syndrome presenting with bilateral optic disk edema. Am J Ophthalmol 127 (1999): 609-610.
- Waeben M, Boven K, D’Heer B, Tassignon MJ. Tubulo-interstitial nephritis-uveitis (TINU)-syndrome with posterior uveitis. Bull Soc Belge Ophtalmol 261 (1996): 73-76.
- van Leusen R, Assmann KJ. Acute tubulo-interstitial nephritis with uveitis and favourable outcome after five months of continuous ambulatory peritoneal dialysis (CAPD). Neth J Med 33 (1988): 133-139.
- Turut P, Bego B, Lelievre G, Malthieu D, Carouge J. [The TINU (tubulo-interstitial nephritis-uveitis) syndrome. Apropos of a case]. Bull Soc Ophtalmol Fr 87 (1987): 1153-1155.
- Mouillon M, Cras-Bonsey A, Romanet JP, et al. [Acute interstitial tubulopathy and uveitis. "Tubulo-interstitial nephritis and uveitis syndrome]. Ophtalmologie 1 (2): 289-291.
- Manjón MT, Sánchez-Bursón J, Montero R, Pérez-Requena J, Alonso M, Marenco JL. Two cases of acute tubulointerstitial nephritis associated with panuveitis (TINU syndrome). J Rheumatol 26 (1999): 234-236.
- Derzko-Dzulynsky L, Rabinovitch T. Tubulointerstitial nephritis and uveitis with bilateral multifocal choroiditis. Am J Ophthalmol 129 (2000): 807-809.
- Hettinga YM, Scheerlinck LME, Lilien MR, Rothova A, De Boer JH. The Value of Measuring Urinary β2-Microglobulin and Serum Creatinine for Detecting Tubulointerstitial Nephritis and Uveitis Syndrome in Young Patients with Uveitis. JAMA Ophthalmol 133 (2015): 140-145.
- Provencher LM, Fairbanks AM, Abramoff MD, Syed NA. Urinary β2-microglobulin and disease activity in patients with tubulointerstitial nephritis and uveitis syndrome. J Ophthalmic Inflamm Infect 8 (2018).