Septic Shock in Neonate: Clinical Profile and its Outcome
Article Information
A. Mannan1*, Mosammad Alpana Jahan2, Md. Arif Hossain3, Afroza Islam Shuma4, Sadeka Choudhury Moni5, Ismat Jahan6, Mohammad Kamrul Hassan Shabuj7, Mohammod Shahidullah8
1Professor, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
2Subject Matter Specialist, Regional Roaming Team (RRT) & Newborn Knowledge Cell (NKC), Department of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3Medical Officer, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
4Medical Officer (Neonatology), Upazila Health Complex, Singair, Manikganj, Bangladesh
5Associate Professor, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
6Assistant Professor, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
7Associate Professor, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
8Professor, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
*Corresponding Author: M. A. Mannan, Professor, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
Received: 01 March 2022; Accepted: 09 March 2022; Published: 24 March 2022
Citation:
M. A. Mannan, Mosammad Alpana Jahan, Md. Arif Hossain, Afroza Islam Shuma, Sadeka Choudhury Moni, Ismat Jahan, Mohammad Kamrul Hassan Shabuj, Mohammod Shahidullah. Septic Shock in Neonate: Clinical Profile and its Outcome. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 177-187.
Share at FacebookAbstract
Background: Sepsis is one of the leading causes of neonatal mortality worldwide. Shock is usually accompanied with sepsis. Documentation of presentations and causative organisms is crucial to manage the newborn with septic shock.
Objective: The objective of this study was to describe the clinical profile and outcome of newborns with septic shock.
Materials and methods: This retrospective study was conducted in the Department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh, from January 2019 to December 2020. A total of144 neonates with septic shock were included in this study. Hospitalized inborn and out born babies were enrolled. Baseline data of selected neonates were retrieved from the registry book. Time of onset of sepsis, presentation of shock with their management and hospital outcome were collected. Data were analyzed in SPSS version 20. Statistical analysis was performed to establish the relationship between neonatal variables and outcomes with septic shock.
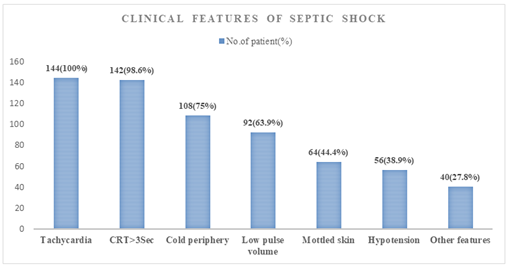
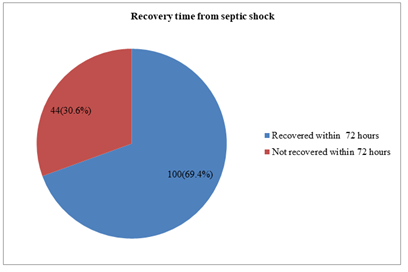
Results: Among 1086 admitted newborns, 536 (49.4%) developed sepsis, of which 144 (26.86%) newborns developed septic shock. The mean gestational age and birth weight were 34.32±2.88 wk and 1886.50±744.9g respectively. One hundred and eight newborns were premature and 90.3% developed sepsis at >72 hours of age. Newborns with septic shock were presented with tachycardia (100%), prolonged CRT (98.6%), cold peripheries (75%), low pulse volume (44.4%), and 38.9% newborns had low blood pressure. Culture-positive sepsis was 31.2% cases. One hundred newborns recovered from septic shock within 72 hours (69.4%) and 64.6% of newborns survived after septic shock. The predictors of outcome of mortality were male sex, age of onset of sepsis >72 hours, positive blood culture, mechanical ventilation and DIC. No variables were found significant in binary regressi
Keywords
Septic shock, Pathogens, Newborn, Outcome, Culture positive, Survivor
Article Details
1. Introduction
Every year, 130 million babies are born worldwide and 14 million newborns die within 28 days after birth [1]. Three-quarter of newborns died in the first week and more than a quarter died in the first 24 hours [2]. In developing countries, sepsis is probably responsible for 30-50% of the total neonatal deaths each year [3]. In Bangladesh, the neonatal mortality rate is 30 per 1,000 live births [4] and sepsis accounts for 20% of neonatal death in Bangladesh [5]. Shock is a common problem in the Neonatal Intensive Care Unit (NICU) and is defined as a condition in which there is decreased oxygenation to the tissue as a result of impaired circulation. Newborns with sepsis often develop septic shock. Premature low birth weight babies are most susceptible to develop shock. Approximately 20% of VLBW newborns admitted to the neonatal intensive care unit (NICU) developed hypotension within 24 hours of admission [6]. Although the true incidence is unknown, a recent retrospective cohort study conducted over a period of 6 years found the incidence rate of septic shock 2.2 per 1,000 admissions per year. Septic shock associated with mortality was about 71% with very low birth weight newborn [7]. Some inflammatory cytokines, including IL1β, IL6, IL8, and TNFα, are elevated in septic shock [8]. The action of the inflammatory mediator results in damage to the capillary wall with loss of vascular tone, which results in dilation and reduced systemic vascular resistance with increased systemic blood flow and low to normal blood pressure. In the early stages of shock, heart rate increases as compensatory mechanism, the skin is supplied with sufficient blood and is warm (warm shock).In the later stages of shock, myocardial contraction decreases, vasocon-striction, decreased systemic blood flow, decreased pulse rate, cold peripheries and capillary refill time became prolonged (cold shock) [9]. Early diagnosis, timely administration of appropriate antibiotics and appropriate supportive care are important for improving survival and reducing long-term sequelae [10]. In a population-based study conducted by Watson and colleagues, the mortality rate was 10.3% in neonates with severe sepsis [11]. There are various predictors to assess the mortality by septic shock such as refractory shock, acute renal failure, neutropenia, increased prothrombin time, excessive bleeding, metabolic acidosis, and hypothermia [12, 13]. Septic shock is associated with high mortality and morbidity in neonates but very few data are available in Bangladesh. The objective of this study was to describe the clinical features and outcomes in neonates with septic shock.
2. Materials and Methods
This retrospective study was conducted in the department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), from January 2019 to December 2020. History about demographics and socioeconomic information, date of admission, mode and place of delivery, gestational age, birth weight, maternal history of PROM, antenatal corticosteroid, antibiotics used were collected from registry book. Clinical findings of neonates included signs and symptoms of septic shock like: mottled skin, temperature instability, pallor, capillary refilling time >3 sec, tachycardia, low volume pulses, cold peripheries and low blood pressure etc all data were also collected from case record form.
Sepsis was defined as clinical syndrome of systemic illness accompanied by bacteremia occurring in the first month of life [14]. Septic shock is a condition of inadequate tissue perfusion secondary to cardiovascular dysfunction occurring in the course of suspected or certain systemic infection, requiring fluid resuscitation or inotropic support [15, 16]. All patients were investigated and managed as per standard of institutional protocol for septic shock. All infants were evaluated for sepsis including septic screening, blood culture and CSF culture when indicated. The management includes appropriate appropriate fluid resuscitation, use of inotropes, empirical antibiotics and blood component transfusion. All these information’s along with duration of NICU stay, complications like AKI,DIC, discharge/death was recorded. The final outcome was considered as “survivor” and “non-survivor” from NICU. Data were analyzed using the statistical package for social sciences (SPSS) version 20. Quantitative data was expressed as mean ± SD and categorical data was presented as proportion. All quantitative variables were compared by unpaired t-test; categorical variables were compared by Chi-square test. P- < 0.05 was considered as statistically significant. Regression analysis was performed to see relationship between the predictive factors with survivor/non-survivors.
3. Results
During the study period total no of admitted neonates were 1086. Among them, 536 newborns developed sepsis, resulting in a rate of 49.4%. Newborns who developed multiple septic episodes, single episode was taken as septic event. Total 144 (26.86%) newborns developed septic shock during the study period. Among them mean gestational age and mean birth weight was 34.32 ± 2.88 wk and 1886.50 ± 744.94 g respectively. Among the admitted neonates, ninety-six cases (66.7%) were inborn. One hundred and eight neonates (75%) were born premature. About 90.3% newborn developed sepsis >72 hours of age. The profile of antenatal factors showed that 16.7% mothers had PROM and 26.4% took antenatal antibiotics (Table 1).
Figure 1 showing the clinical features that are encountered during the time of septic shock. All neonates were presented with features of tachycardia, 98.6% with prolonged capillary refill time. About 75% had features of cold periphery followed by low pulse volume and mottled skin. Hypotension was observed in 38.9% cases. After diagnosis, all infants received treatment of shock according to institutional protocol. All patients received intravenous fluid boluses. The inotropic agents given to all patients were dopamine alone or in combination with other inotropes. Dopamine alone was given in less frequencies (26.88% vs 27.45%) compared to combination of inotropes (73.11% vs 72.54%) in the survivor and non-survivor groups respectively. Epinephrine or nor-epinephrine was given more in non-survivor group (27.1%). Hydrocortisone was also given more in non-survivor group (16%) compare to survivor group (3.8%).
Figure 2 showing the duration of recovery form septic shock. About 69.4% neonates recovered from septic shock within 72 hours with appropriate treatment, whereas 30.6% required prolonged time. Table 3 showing outcomes of neonate with septic shock. Fifty-one infants (35.4%) died during hospital stay after the onset of septic shock. In table 4, culture positive Sepsis was 45 out of 144 patients (31.2%). Among the culture positive cases, 21 were in survivor group and 24 neonates in non-survivor group; (p-.002). Univariate analysis of factors associated with mortality among neonates with septic shock showed that male sex, age of onset of sepsis >72 hours, culture positive sepsis, mechanical ventilator support and DIC were significantly related with mortality. No significant difference was found between survivors and non-survivor group for gestational age, birth weight, place of birth, maternal ACS therapy, small for gestational age, and AKI (Table 5). Logistic regression analysis was performed to find association between outcomes (survivor/non-survivor) and neonatal variables such as male sex, age of onset of sepsis >72 hours, mechanical ventilator support, disseminated intravascular coagulation and culture positive sepsis-all these variables did not show significant association (p- > 0.05) between septic shock and clinical outcome (Table 6).
|
Variables |
No. (%) |
|
Gestational age(weeks), Mean ± SD |
34.32 ± 2.88 |
|
Birth weight (gm), Mean ± SD |
1886.50 ± 744.94 |
|
Gender |
|
|
Male |
92 (63.9) |
|
Female |
52 (36.1) |
|
Place of birth |
|
|
Inborn |
96 (66.7) |
|
Outborn |
48 (33.3) |
|
Mode of delivery |
|
|
LUCS |
114 (79.2) |
|
NVD |
30 (20.8) |
|
Classification of newborn |
|
|
Preterm |
108 (75) |
|
Term |
36 (25) |
|
SGA |
21 (14.6) |
|
Age at the onset of sepsis |
|
|
≤72 hours |
14 (9.7) |
|
>72hours |
130 (90.3) |
|
PROM |
24 (16.7) |
|
Antenatal steroid therapy |
|
|
Complete |
63 (43.7) |
|
Incomplete |
29 (20.1) |
|
No |
16 (11.1) |
|
Antenatal antibiotics for maternal infection |
38 (26.4) |
|
Hospital stays (days), Mean ± SD |
11.9 ± 7.66 |
Quantitative data are presented as mean ± SD and Qualitative data as the number and percentage .PROM-Premature rupture of membrane, SGA-Small for gestational age, LUCS-Lower uterine cesarean section, NVD-normal vaginal delivery.
Table 1: Baseline characteristics of neonates (n=144).
|
Therapeutic Interventions |
Survivors (93) |
Non-survivors (51) |
|
Fluid therapy |
93 (100%) |
51 (100%) |
|
Dopamine only |
25 (26.88%) |
14 (27.45%) |
|
Dopamine+Dobutamine |
68 (73.11%) |
37 (72.54%) |
|
Epinephrine or Nor-epinephrine |
9 (12.0%) |
13 (27.1%) |
|
Hydrocortisone |
3 (3.8%) |
8 (16%) |
Categorical data are presented as number and percentage (%).
Table 2: Therapeutic Interventions implemented for septic shock (n=144).
|
Outcome |
No |
Frequency (%) |
|
Survivors |
93 |
64.6 |
|
Non-survivors |
51 |
35.4 |
Categorical data are presented as number and percentage (%).
Table 3: Outcome of neonates with septic shock (n=144).
|
Blood culture |
No (%) |
Survivors(n=93) |
Non-survivors(n=51) |
p-value |
|
Culture positive Culture negative |
45 (31.2%) 99 (68.8%) |
21(22.6) 72(77.4) |
24(47.1) 27(52.9) |
.002 |
Chi-square test for categorical data. P < 0.05 considered as significant.
Table 4: Frequency of positive blood culture in neonates with septic shock (n=144).
|
Variables |
Survivors(n=93) |
Non-survivors(n=51) |
p-value |
|
Gestational age(weeks) |
|||
|
<34 |
68(73.1) |
40(78.4) |
0.481 |
|
>34 |
25(26.9) |
11(21.6) |
|
|
Birth weight (gm) |
|||
|
<1500gm |
40(43.0) |
20(39.2) |
0.659 |
|
> 1500gm |
53(57.0) |
31(60.8) |
|
|
Gender |
|||
|
Male- |
53(57.0) |
39(76.5) |
0.02 |
|
Female |
40(43.0) |
12(23.5) |
|
|
Place of birth |
|||
|
Inborn- |
65(69,9) |
31(60.8) |
0.267 |
|
Outborn- |
28(30.1) |
20(39.2) |
|
|
Small for gestational age- |
10(11.0) |
11(21.6) |
0.088 |
|
Antenatal steroid therapy |
24(25.8) |
14(27.5) |
0.83 |
|
Age at the onset of sepsis |
|||
|
≤72 hr |
5(5.37) |
9(17.64) |
0.017 |
|
>72hr |
88(94.62) |
42(82.35) |
|
|
Culture positive sepsis |
21 (22.6) |
24(47.1) |
0.002 |
|
Required>72hoursfrom recovery of shock |
28(30.10) |
16(31.37) |
0.875 |
|
Mechanical ventilator support |
14(15.05) |
15(29.41) |
0.04 |
|
AKI |
8(8.60) |
8(15.68) |
0.269 |
|
DIC |
12(12.90) |
18(35.29) |
0.002 |
Chi-square test for categorical data. P - < 0.05 w considered as significant. AKI-acute kidney injury, DIC-disseminated intravascular coagulation.
Table 5: Univariate analysis of risk factors associated with mortality among neonates with septic shock (n=144).
|
Predictors |
Mortality |
||
|
OR |
(95% CI) |
p-value |
|
|
Male Gender |
0 .388 |
.061-2.459 |
0.315 |
|
Age of onset of sepsis>72hours |
0.278 |
.015-5.302 |
0.395 |
|
Culture positive sepsis |
0.438 |
.088-2.187 |
0.314 |
|
Mechanical ventilator support |
0.933 |
.825-1.055 |
0.27 |
|
Disseminated intravascular coagulation |
0 .520 |
.119-2.270 |
0.384 |
Statistical test by binary logistic regression
Table 6: Logistic regression analysis of risk factors associated with mortality among neonates with septic shock.
4. Discussion
Sepsis is one of the major causes of neonatal morbidity and mortality in Bangladesh. Septic shock is frequently associated with neonatal sepsis, but very few data is available. Thus, this study was conducted to find out the clinical pattern and outcome among neonates with septic shock. Department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), conducted this retrospective study over a period of two years. During the study period, total study sample was 144 who developed septic shock during their course of hospital stay. Mean gestational age and birth weight was 34.32 ± 2.88 wk and 1886.50±744.94 g respectively. Sujana et al found similar gestational age and birth weight in their study. They found gestational age and birth weight 35.78 ± 3.00weeks and 1.95 ± 0.65g respectively [17]. Two-third of admitted neonate was inborn and 75% were preterm neonates in our study. This institute prefers inborn admission more, thus the percentage of inborn was more. About 43.7% of cases received a complete dose of antenatal corticosteroids. The age of onset of sepsis >72 hours was in 90.3% cases. Sharma et al [18] found LONS in 43.68% cases. Yadav NS found 71.2%sepsis at age more than 3 days [19].
Our study finding is higher than those studies. Clinical features of septic shock were cold periphery, mottled skin, low pulse volume, tachycardia and prolonged CRT present in all patients in our study. Hypotension was reported in a smaller percentage because it was a late presentation of shock. The compensation mechanisms appear in the early stages of shock to maintain important organ function. This compensated phase is characterized by activation of neurohumoral factors, redistribution of blood flow to "vital" organs, including brain, heart, adrenal glands. Thus, heart rate and cardiac contractility increases which maintains blood pressure in range. During uncompensated Phase, these mechanisms fail, leading to hypotension, poor perfusion and worsening lactic acidosis due to anaerobic tissue metabolism. Without effective treatment, the shock can quickly move to an irreversible stage leading to organ failure and eventually death [20]. In this study about 69.45% neonates recovered from septic shock within 72 hours of treatment. Blood culture remains the gold standard for confirming sepsis. In this study culture positive sepsis was about 31.2% cases. Similarly, Sharma et al found culture-positivity rate 37.63% [18] while in Shah AJ et al, [21] found culture positive sepsis in 31.75%, Bhattacharjee et al, [22] found 32% and West BA et al, [23] found 41.6% had positive blood culture in their study. Awad HA et al, [24] found32.25% culture-positive and among them late onset sepsis was found in 64.6%. We found survivor rate about 64.6%. Similar findings were found in a study conducted by Wale A et al. In their study, they included 211 neonates with sepsis admitted at the NICU, where they found 67.8% has good outcomes and 32.2% had a poor outcome [25]. Kermorvant-Duchemin E et al found 40% mortality rate in their study [7]. The predictors of the outcome of mortality were male sex, age of onset of sepsis >72 hours, positive blood culture, mechanical ventilator support and DIC. These factors were significantly related with mortality in this study. The sex of the newborn was significantly associated with neonatal sepsis.
One study found that male sex were 3.7 times more likely to develop neonatal sepsis than their counterparts [26]. This finding is consistent with a study done in Australia. The risk of neonatal sepsis has been reported to be three-fold higher in male newborns compared to female newborns. However, the etiology of gender differences in the disease remains relatively uncertain and can be multifactorial as genetic, immunological, and hormonal effects play important roles [27]. Late onset sepsis was found significantly associated with poor outcomes in this study in univariate analysis. The experience of the NICHD Neonatal Research Network shows late onset sepsis is a major issue and affects 25% of infants with very low birth weight (VLBW) in the neonatal intensive care unit (NICU). Late onset Gram-negative sepsis (LONS) and meningitis are considered to be the leading cause of neonatal morbidity and mortality [28]. In a study, hospital-acquired LOS was significantly associated with mechanical ventilation, and death (p< 0.01) and catecholamine support (OR = 3.2) were associated with death in hospital-acquired LOS [29].
5. Conclusion
In this study, 26.86% (144/536) septic neonates developed septic shock in the course of NICU stay. The common presentation of shock in newborns were tachycardia, prolonged CRT, cold peripheries, low pulse volume and mottled skin; the incidence of hypotension was 38.9%. Neonatal death after the onset of septic shock was 35.4%. Early recognition and prompt management can improve the survival of neonates.
Limitations
This study has some limitations, because of its retrospective design, we were unable to retrieve complete information for all cases of Shock.
References
- Kayom VO, Mugalu J, Kakuru A, et al. Burden and factors associated with clinical neonatal sepsis in urban Uganda: a community cohort study. BMC 18 (2018): 1-8.
- Jehan I, Harris H, Salat S, et al. Neonatal mortality, risk factors, and causes: a prospective population-based cohort study in urban Pakistan. Bull World Heal Organ 87 (2009): 130-138.
- Aijaz N, Huda N, Kausar S. Disease burden of NICU, at a tertiary care hospital, Karachi. Journal of the Dow University of Health Sciences (JDUHS) 6 (2012): 32-35.
- NIPORT I. Bangladesh Demographic and Health Survey 2017–18: Key Indicators (2019).
- Maternal WH. Child Epidemiology Estimation Group Child Causes of Death 2000–2017. WHO: Geneva, Switzerland (2018).
- Halkar M. Approach to Shock and Hypotension in Neonates. PERINATO-LOGY 16 (2015).
- Kermorvant-Duchemin E, Laborie S, Rabilloud M, et al. Outcome and prognostic factors in neonates with septic shock. Pediatric Critical Care Medicine 9 (2008): 186-191.
- Lynch S K, Mullett M D, Graeber J E, et al. A comparison of albumin-bolus therapy versus normal saline-bolus therapy for hypotension in neonates. Journal of Perinatology 28 (2008): 29-33.
- Jones J G, Smith S L. Shock in the critically ill neonate. The Journal of perinatal & neonatal nursing 23 (2009): 346-354.
- Klinger G, Levy I, Sirota L, et al. Israel Neonatal Network. Outcome of early-onset sepsis in a national cohort of very low birth weight infants,’ Pediatrics 125 (2010): e736-e740.
- Watson RS, Carcillo JA, Linde-Zwirble WT, et al. The epidemiology of severe sepsis in children in the United States. Am J Respir CritCare Med 167 (2003): 695-701
- Bhutta ZA, Yusuf K. Neonatal sepsis in Karachi: factors determining outcome and mortality. J Trop Pediatr 43 (1997): 65-70.
- Pierro A. Metabolism and nutritional support in the surgical neonate. J Pediatr Surg 37 (2002): 811-822.
- Gomella TL, Cunningham MD, Eyal FG, et al. Neonatology: management, procedures, on-call problems, diseases, and drugs. New York: McGraw-Hill Education Medical (2013).
- Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatric critical care medicine 6 (2005): 2-8.
- Haque KN. Understanding and optimizing outcome in neonates with sepsis and septic shock. InIntensive Care Medicine (2007): 55-68.
- Sujana CS, Meshram RJ, Lakhkar BB. Clinical profile and short-term outcomes in neonates with septic shock. International Journal of Contemporary Pediatrics Sujana CS et al. Int J ContempPediatr 6 (2019): 1456-1460.
- Sharma CM, Agrawal RP, Sharan H, et al. Neonatal sepsis: bacteria & their susceptibility pattern towards antibiotics in neonatal intensive care unit. Journal of clinical and diagnostic research: JCDR 7 (2013): 2511.
- Yadav NS, Sharma S, Chaudhary DK, et al. Bacteriological profile of neonatal sepsis and antibiotic susceptibility pattern of isolates admitted at Kanti Children’s Hospital, Kathmandu, Nepal. BMC research notes 11 (2018): 1-6.
- Noori S, Friedlich PS, Seri I. Pathophysiology of shock in the fetus and neonate. In: Polin RA, FoxWW, Abman SH, editors. Fetal and neonatal physiology. 4th ed. Philadelphia: Elsevier Saunders (2011): 853-863.
- Shah AJ, Mulla SA, Revdiwala SB. Neonatal sepsis: High antibiotic resistance of the bacterial pathogens in a neonatal intensive care unit of a tertiary care hospital. J Clin Neonatol 1 (2012): 72-75.
- Bhattacharjee A, Sen MR, Prakash P, et al. Increased prevalence of extended spectrum β – Lactamase producers in neonatal septicemic cases at tertiary referral hospital. Indian J Med Microbiol 26 (2008): 356- 360
- West BA, Peterside O. Sensitivity pattern among bacterial isolates in neonatal septicaemia in Port Harcourt. Annals of clinical microbiology and antimicrobials 11 (2012): 1-6.
- Awad HA, Mohamed MH, Badran NF, et al. Multidrug-resistant organisms in neonatal sepsis in two tertiary neonatal ICUs, Egypt. Journal of the Egyptian Public Health Association 91 (2016): 31-38.
- Wale A, Chelkeba L, Wobie Y, et al. Treatment Outcome and Associated Factors of Neonatal Sepsis at MizanTepi University Teaching Hospital, South West Ethiopia: A Prospective Observational Study. Pediatric Health, Medicine and Therapeutics 12 (2021): 467.
- Neonatal Sepsis and Its Associated Factors Among Neonates Admitted to Neonatal Intensive Care Units in Primary Hospitals in Central Gondar Zone, Northwest Ethiopia (2019).
- Driscoll DNO, Mcgovern M, Greene CM, et al. Gender disparities in preterm neonatal outcomes. Found Acta Pædiatrica 107 (2018): 1494–1499.
- Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 110 (2002): 285- 291.
- Berardi A, Sforza F, Baroni L, et al. Epidemiology and complications of late-onset sepsis: an Italian area-based study. PloS one 14 (2019): e0225407.