Role of Telemedicine and Impact of Covid 19 Pandemic on Diabetic Patients Management and Clinical Outcomes
Article Information
Abdulmajeed Alruwaitea1,2 , Abdulaziz Alalwan1,2, Yousef Alluhaymid1,2, Faisal Alrayes1,2 and Abdulaziz Aljohani1,2
1 Family Medicine Department, King Saud University Medical City, Riyadh, Saudi Arabia
2 Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
*Corresponding author: Abdulmajeed Alruwaitea. Family Medicine Department, King Saud University Medical City, Riyadh, Saudi Arabia. Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia.
Received: 15 July 2023; Accepted: 27 July 2023; Published: 05 August 2023
Citation: Abdulmajeed Alruwaitea, Abdulaziz Alalwan, Yousef Alluhaymid, Faisal Alrayes and Abdulaziz Aljohani. Role of telemedicine and Impact of COVID 19 pandemic on diabetic patients management and clinical outcomes. Archives of Clinical and Biomedical Research. 7 (2023): 475-488.
Share at FacebookAbstract
Background: Telemedicine has emerged as a valuable tool in managing chronic diseases like diabetes, especially during the COVID-19 pandemic. This study aims to evaluate the impact of telemedicine on diabetes management by assessing patient outcomes and healthcare accessibility.
Methods: A retrospective cohort study was undertaken at King Saud University Medical City (KSUMC) located in Riyadh, Saudi Arabia. Diabetic patient visits in Family Medicine clinics were documented and implemented in an Excel sheet by the quality team at the Family Medicine department. The study period extended from January to April 2023. Patients were divided into two groups based on their albumin/creatinine ratio (ACR). And the data included demographic information, HbA1c measurements, co-morbidities, documented telemedicine interactions, and other relevant variables before and after the Covid-19 lockdown. The data collection period spanned from January 2020 to December 2020.
Results: The sample comprised 121 diabetic patients, with 57% females and 43% males. The mean age was 60.68 years, and the majority (50.4%) were aged 61 years or older. During the pandemic, 81.8% of patients received telemedicine care. There were no significant differences in mean HbA1c, ACR, or BMI between the periods before and after the pandemic lockdown.
Conclusion: Telemedicine played a crucial role in managing diabetic patients during the COVID-19 pandemic. While telemedicine did not directly impact ACR, patients with high ACR demonstrated poorer glycemic control. These findings highlight the need for further research and improvement in optimizing telemedicine for diabetes management, with a focus on enhancing glycemic control and patient outcomes.
Keywords
Telemedicine; Diabetes; Covid-19; Hba1c; Albumin/ Creatinine Ratio.
Article Details
1. Introduction
Telemedicine refers to the utilization of technology and devices to remotely gather health-related information about patients, aiding in determining the necessity and urgency of medical intervention. It serves as both a screening and diagnostic tool and has gained significant recognition in recent literature, primarily due to the increased adoption and advancement of digital technologies such as smartphones and digital connectivity [1].
For several decades, telemedicine has been acknowledged as a valuable approach for enhancing access to healthcare services that may be challenging to obtain due to factors such as geographical location (rural or remote areas) or various barriers (frailty, transportation limitations, or physical and mental health conditions). Its significance lies in its ability to overcome these obstacles and ensure individuals receive the healthcare they need [2].
In the field of diabetology, the utilization of telemedicine has witnessed a significant rise in order to enhance healthcare accessibility and improve clinical outcomes for patients with diabetes. Just as various aspects of life have become automated and digitally addressed, routine medical care for chronic conditions will also follow suit [3].
The utilization of telemedicine has demonstrated notable improvements in the self-management processes and clinical outcomes for patients with diabetes. The use of mobile devices and apps offers numerous advantages for healthcare professionals (HCPs), particularly in terms of increased access to point-of-care tools. This accessibility has been shown to enhance clinical decision-making and ultimately lead to improved patient outcomes. Furthermore, telemedicine empowers patients to better manage their condition and effectively control their blood glucose levels [4].
Diabetes is a prevalent chronic disease affecting a significant number of individuals worldwide. It is also among the primary comorbidities in individuals who have succumbed to COVID-19 infection, second only to hypertension. Additionally, the risk of mortality in hospital settings due to COVID-19 appears to be 3.5 to 5 times higher in individuals with type 1 diabetes and twice as high in those with type 2 diabetes compared to non-diabetic patients [5].
The presence of diabetes, along with other comorbidities, substantially exacerbates the clinical status of individuals infected with COVID-19, elevating the risk of unfavorable outcomes, including mortality. However, it is important to note that having diabetes does not appear to increase the susceptibility to contracting the coronavirus [5]. Diabetic kidney disease affects around 40% of individuals with diabetes and is the primary cause of chronic kidney disease (CKD) on a global scale. Effective management of these conditions revolves around maintaining proper control over blood glucose levels and blood pressure [6].
As per the International Diabetes Federation Diabetes Atlas (2021), there are currently 537 million adults between the ages of 20 and 79 living with diabetes. It is projected that this number will increase by 46% between 2021 and 2045. Estimates suggest that by 2030, there will be approximately 643 million adults worldwide with diabetes, and by 2045, this number is expected to rise to 783 million [7].
In developing countries where telemedicine is not available, the absence of this essential tool poses challenges for individuals with diabetes and their healthcare providers, especially during pandemics. As the COVID-19 outbreak rapidly escalated, patients and healthcare professionals in many countries had to find temporary solutions for telecommunication. Despite the lack of telemedicine infrastructure in regions with a high prevalence of diabetes, such as the Middle East and South Asia, the widespread use of smartphones in these areas presents an opportunity to quickly implement a relatively simple telemedicine clinic. This approach can serve the purpose of maintaining communication during pandemics without imposing significant burdens on patients and healthcare systems, thereby leveraging existing technological resources effectively [8].
Telemedicine is crucial in managing diabetes, but challenges remain. This research aims to evaluate its impact, effectiveness, and accessibility in diabetes care. The study fills gaps in knowledge and guides healthcare professionals in optimizing telemedicine for better patient outcomes.
As a result of the COVID-19 pandemic, there has been a huge change in the healthcare system globally. One of these changes was the lockdowns of most Clinics and hospitals to prevent the spread of the virus and ensure the safety of the population, Patients are not allowed to visit the hospital until there is an emergency [9]. Consequently, the routine management of diabetic patients was affected during this lockdown period.
Many of the first challenges for diabetes care throughout the COVID-19 pandemic may be restricted access to health care, health education, routine laboratory investigations, and medications; this might have worsened due to the lockdown period [11].
These changes in the healthcare system arrived in Saudi Arabia, after detecting the first case of COVID-19 on March 2, 2020, basic precaution like hand wash, hand sanitizers, and mask in addition to total and partial lockdowns were implemented to prevent the spread out of the virus [10]. This stimulates most of the health sectors in different countries to implement alternative and effective strategies to overcome this challenge and to provide timely and effective care to such patients [11]. Some of these ideal ways and strategies include electronic health (eHealth), telehealth, and/or telemedicine platforms [12]. Previous studies documented the advantages of using these technologies strategies in pandemic and epidemic situations [13] . These strategies are playing a potential role to enhance the research of epidemiological, control of disease, and management of clinical cases [15,16].
According to the World Health Organization (WHO), eHealth means the use of data and communications technologies to support the health and their related fields such as health-care services, health surveillance, health literature, and health education and research [12]. Thus, eHealth includes all sorts of data and communication technology, such as websites and apps for health promotion, assessment, screening, and therapists’ video-chat sessions [17]. eHealth has many advantages, especially in epidemic and pandemic situations like lowering prices and replacing face-to-face healthcare contacts and communications [17].
On the other hand, telehealth refers to the use of electronic information and telecommunications technologies to support advanced health-related education, health administration, and public health [12]. however, the main role of Telehealth is to support long-distance clinical health care throughout reducing the time consumed by providing communication between patients and healthcare staff [18]. This process is done by using new telecommunications tools such as webcams, Videoconferencing, and similar television systems [19].
There are several advantages of using telehealth technology; it can reduce the use of resources in health centers, enhance access to care, and minimize the risk of direct transmission of the infective agent from person to person (Charles 2000). Recently, Telehealth can become a necessary need for the overall population, health care staff, and COVID-19 patients, particularly when people are in quarantine, enabling patients in real-time through contact with a health care staff for recommendations on their health issues [19].
In Saudi Arabia, several hospitals and health centers advocated the utilization of telemedicine to ensure that diabetic patients receive the required health care in a very timely and effective manner. However, the impact of such efforts has not been not well developed in Saudi Arabia, and the need to improve the clinical approach such as telehealth e-health is necessary [21] Hence, this study tends to undertake and determine the effect of the total and partial lockdowns of hospitals in Saudi Arabia on clinical outcomes in diabetic patients. Moreover, The most important goal of this study is to highlight the important innovative clinical approach such as telehealth and e-health which is not well developed in Saudi Arabia but highly needed as such diabetic patients need continuous management.
[22]. carried out research to examine diabetes nurses’ thoughts on the COVID-19 pandemic’s effects on diabetics and diabetes services in Europe. Using an electronic questionnaire that was disseminated through networks of diabetic nurses, they conducted a cross-sectional study of diabetes nurses from all around Europe. The survey, which was distributed from early June to July 2020, was created to provide a qualitative view on how the COVID-19 situation was affecting individuals with diabetes and services in various countries around Europe. The survey was carried out in 27 nations with diverse demographics, healthcare systems, and financial capabilities. Diabetes nurses from the participating nations were the participants. Overall, the results indicate that the pandemic has had a detrimental effect on the risks to the physical and mental health of persons with diabetes, as seen by reported increases in acute diabetic episodes, new diagnoses, anxiety, diabetes distress, and depression. Finally, as the COVID-19 situation worsens, we urgently need to make changes to the healthcare delivery systems to lessen the pandemic’s effects on people with diabetes [22].
Researchers [23] studied how the COVID-19 shutdown affected patients with type 1 diabetes (T1D) and type 2 diabetes’ ability to regulate their blood sugar levels. Studies published up through April 2021 were extensively searched in the databases for publications in English and German. They looked at a total of 1823 T2D patients and 2881 T1D individuals. In 72% of T1D investigations, glycemic results showed a clear, substantial improvement. Due to the “lockdown effect,” meta-analysis showed a mean difference in HbA1c of 0.05% and in time in range (TIR) of + 3.75%. The results for T2D patients clearly differ from those for T1D patients; the reviewed studies often demonstrate a decline in the patients’ weight/BMI and glycemic levels as a result of the lockdown period. In conclusion, additional research from various areas are required to determine the lockdown’s true effects on patients with T1D and T2D on a greater scale [23].
In research published in 2021, [24]. looked at how type 1 diabetes patients’ lifestyle and metabolic parameters were affected by the acute coronavirus infection. In this retrospective cohort research, T1D patients who visited the KPUM’s Department of Endocrinology and Metabolism between April 16 and May 1, 2020, were given a questionnaire. According to the results, during the COVID-19 pandemic, patients with T1D reported higher stress levels and lower exercise volumes. Additionally, individuals with T1D experienced worse HbA1c changes throughout the pandemic year compared to changes for the previous three months during the pre-pandemic year. The COVID-19 pandemic did not, however, cause a change in body weight. As a result, more focus should be placed on stress and lifestyle factor management in T1D patients in order to prevent deterioration of their glycemic control due to the ongoing pandemic [24].
The management of chronic patients in primary healthcare was the subject of research of Stachteas in 2022 to determine how the COVID-19 pandemic affected this management. Boolean operators were used to search the PubMed and Google Scholar databases until April 2021. After some consideration, the studies that were pertinent to the subject were included. The raised blood glucose levels (59.4% of participants) and increased variability (31.2%) compared to the pre-pandemic period were two of the primary documented consequences of the COVID-19 pandemic, according to a large study of diabetic patients in Brazil. Similar findings were obtained in large multicenter retrospective observational studies from the US and Korea with DM, which showed that social isolation policies had a negative impact on patients’ glycemic management and significantly raised HbA1c levels. Finally, robust and empowered primary and community health care is crucial if health systems are to be resilient to health crises of this severity [25].
[26] conducted study to compile information from the literature on the effects of telemedicine on the monitoring of diabetes patients during the pandemic and its role in the treatment of diabetic patients in the future. The available research indicates that, when compared to conventional treatment, the use of TM is associated with significant improvements in HbA1c for patients with type 1 and type 2 diabetes as well as patient-reported satisfaction. Since the proportion of TM visits was less than 1% before to the pandemic and increased to an average of 95.2% by April 2020, it is clear that the pandemic showed the necessity for increased usage of TM for the monitoring of patients with either T1D or T2D. Patients receiving TM treatment saw a mean decrease in HbA1c levels of 1.82%, compared to a mean decrease of 1.54% for patients receiving standard care. The management of patients with T1D and T2D, pregnant women with diabetes, and newly diagnosed cases of diabetes during the COVID-19 period in primary and secondary care has swiftly come to recognize TM as an indispensable and effective tool [26].
In a paper published in 2021, [27]. explored several strategies for restructuring and revolutionising diabetes outpatient treatment while also providing an overview of current telemedicine diabetes care applications. They said that individuals with diabetes, particularly those with poor glycemic control, have been recognised as a risk group that requires extra protection against viral illnesses such the seasonal flu and COVID19. Diabetes telemedicine adoption is hampered by a number of factors, including a lack of technical expertise and specialised training, a lack of standards, uncertainty about the technology’s effectiveness and success rate, and changing practitioner/patient relationships. All of these factors have an adverse effect on telemedicine adoption among practitioners. It was indicated that automated mobile transmission or a real-time feedback modality increased the efficiency of these interventions when used telemedical lifestyle modification methods demonstrated small decreases in HbA1c ( 0.3%) and weight ( 0.6 kg). Finally, more research based on randomized controlled trials is required to establish the validity and acceptability of telediabetology [27].
2. Research Methodology
This paper describes a retrospective cohort study conducted at King Saud University Medical City (KSUMC), a tertiary academic center located in Riyadh, Kingdom of Saudi Arabia. The study focuses on diabetic patients who visited the Family Medicine clinics. Patient visits were documented and recorded in an Excel sheet by the quality team at the Family Medicine department in KSUMC. Due to the Covid-19 pandemic, the clinics were closed in March 2020, and care was transitioned to telemedicine until October 2020. The diabetic patients were divided into two groups based on their albumin/creatinine ratio: normal and abnormal and the study was conducted from January to April 2023.
The target population for this study includes all diabetic patients who visited the Family Medicine clinics. The sample size for the cohort study was determined using a sample size formula. The ratio of patients with a positive albumin/creatinine ratio to those with a negative ratio was set at 3:1. For example, if there were 100 patients with a positive ratio, the group with a negative ratio would consist of 300 patients.
Inclusion Criteria the study included type 2 diabetes mellitus patients visiting the University Family Medicine clinic at King Saud University Medical City (KSUMC) while exclusion Criteria were non-diabetic patients, type 1 DM and other types of diabetes were excluded from the study.
The study variables include the albumin/creatinine ratio and HbA1c measurements of the patients before and after the Covid-19 lockdown. Patient data was treated with strict confidentiality and was not accessible to any third party. The study did not include patient names.
The data for this study was collected from the medical records of patients at the Family Medicine department in KSUMC. The data included demographic information, HbA1c measurements, co-morbidities, documented telemedicine interactions, and other relevant variables before and after the Covid-19 lockdown. The data collection period spanned from January 2020 to December 2020.
If data or questionnaires from other authors were used in this study, copyright permission was obtained or the data was sourced from open access materials. Proof of correspondence with the original author(s) was submitted.
3. Results
3.1 Statistical Data Analysis
The mean and standard deviation were used to describe the continuous measured variables and the frequencies and percentages were used to describe the categorical variables . The Kolmogrove-Smirnov statistical normality test and the histograms were used to assess the statistical normality assumptions for metric variables . The patients mean measured repeated parameters and outcomes ( before pandemic and after pandemic) were compared for statistically significant differences using the Non-Parameric Wilcoxon's signed Rank test and the Repeated measured categorical variables were also assessed for statistically significant changes across time using the Non-Parametric Cochran's Q chi-squared test. The independent samples t-test was used to assess the statistical significance of mean differences on metric variables between the levels of binary factors . The Pearson's correlations test was used to assess the correlations between metric measured variables . In order to account for the effect of time factor ( before vs post pandemic lockwon) into the multivariable analysis the data was restructured into a wide dataset with a matrix size equal to 121X2 repeated measuers = 242 data records . The restructured data was subjected to the Multivariable Binary Logistic Regression Analysis (MBLR) under the Generalized Linear Mixed models accounting for all the relevant predictor variables in the analysis. The associations between predictor variables with the analysed outcomes in the Logistic Regression analysis was expressed as Multivariable adjusted Odds Ratios (OR) with their associated 95% confidence intervals . The SPSS IBM statistical computing program version 21 was used for the statistical data analysis and the alpha significance value was considered at 0.050 level.
Table 1: Descriptive analysis of the patients sociodemographic characteristics and measured clinical outcomes and telemedicine.
|
Column1 |
Frequency |
Percentage |
|
Sex |
||
|
Female |
69 |
57 |
|
Male |
52 |
43 |
|
Age ( years), mean (SD) |
60.68 (10.50) |
|
|
Age group |
||
|
35-40 years |
5 |
4.1 |
|
41-50 years |
11 |
9.1 |
|
51-60 years |
44 |
36.4 |
|
>=61 years |
61 |
50.4 |
|
Received telemedicine care during the pandemic |
||
|
No |
22 |
18.2 |
|
Yes |
99 |
81.8 |
|
History of Hypertension requiring treatment |
||
|
No |
31 |
25.6 |
|
Yes |
90 |
74.4 |
|
Receives ARB/ACE treatment agents? |
||
|
No |
34 |
28.1 |
|
Yes |
87 |
71.9 |
|
Diagnosed with High serum Albumin:Creatinine Ratio (ACR>30 mg/gm) |
||
|
A:C ratio <30 mg/mmol |
91 |
76 |
|
A:C ratio >=30 mg/mmol |
30 |
24 |
The medical records of one hundred and twenty one diabetic patients were reviewed retrospectively and data was compiled on their glycemic control and the Albumin-Creatinine Ratio (ACR) during two different time points ( before and post the COVID lockdown . The resulted descriptive analysis for the patients sociodemographic characteristics are shown in the table-1. Most of the patients 57% were diabetic female patients and the remainder 43% of them were males . The mean ±SD age for the sample of patients was equal to 60.68 ±10.50 years , however 4.1% of the patients were aged between 35-40 years, another 9.1% of them were aged between 41-50 years and 36.4% of them were aged between 51-60 years but most of them 50.4% were aged >=61 years . Most of the patients in the sample 81.8% had received a tele-medicine follow up care during the lockdown period while they stayed at their homes , Also, the resulted findings showed that most of the patients 74.4% were priori diagnosed with Hypertension that required treatment , and 71.9% were treated with either an ARB /ACE inhibitor medications . Less than the third (30%) of the patients were found to have high serum Albumin:Creatinine Ratio >=30 mg/gm during the study period and the remainder 70% of the patients had ACR within expected bounds.
Table 2: Bivariate comparison between patients with normal versus high ACR index
|
Negative AC ratio= low or normal |
Positive AC ratio=High |
|||||||
|
n=91 |
n=30 |
test statistic |
p-value |
|||||
|
Sex |
||||||||
|
Female |
56 (61.5) |
13 (43.3) |
χ2(1)=3.051 |
0.081 |
||||
|
Male |
35 (38.5) |
17 (56.7) |
||||||
|
Age ( years), mean (SD) |
60.12 (10.60) |
62.37 (10.12) |
t=1.02/df=119 |
0.311 |
||||
|
Received telemedicine care during the pandemic |
||||||||
|
No |
16 (17.6) |
6 (20) |
χ2(1)=0.10 |
0.755 |
||||
|
Yes |
75 (82.4) |
24 (80) |
||||||
|
History of Hypertension requiring treatment |
||||||||
|
No |
27 (29.7) |
4 (13.3) |
χ2(1)=3.20 |
0.075 |
||||
|
Yes |
64 (70.3) |
26 (86.7) |
||||||
|
Receives ARB/ACE treatment agents? |
||||||||
|
No |
28 (30.8) |
6 (20) |
χ2(1)=1.295 |
0.255 |
||||
|
Yes |
63 (69.2) |
24 (80) |
||||||
|
Glycated Hemoglobin Hba1c level before shutdown |
7.71 (1.55) |
8.37 (1.81) |
t=1.94/df=119 |
0.055 |
||||
|
High HBA1C index >7.5% before shutdown |
||||||||
|
No |
52 (57.1) |
13 (43.3) |
χ2(1)=1.73 |
0.188 |
||||
|
Yes |
39 (42.9) |
17 (56.7) |
||||||
|
Glycated Hemoglobin Hba1c level after shutdown |
7.80 (1.66) |
8.5 (1.52) |
t=2.04/df=119 |
0.043 |
||||
|
High HBA1C index >7.5% after shutdown |
||||||||
|
No |
50 (54.9) |
9 (30) |
χ2(1)=5.62 |
0.018 |
||||
|
Yes |
41 (45.1) |
21 (70) |
||||||
|
BEFORE -Body Mass Index (BMI) score, mean (SD) |
32.10 (6.17) |
33.19 (7.57) |
t=0.70/df=119 |
0.484 |
||||
The bivariate comparison analysis findings between patients with Normal Versus abnormally high ACR ratio are shown in the table-3 and the resulted findings showed that the patients age and sex did not correlate significantly with their risk of having high serum ACR score above normal thresholds, however male patients were found slightly more inclined to have high ACR compared to females but the difference between the two genders on their abnormal ACR state was insignificant statistically , p-value=0.081 according to the chi-squared test of association. Also, the resulted findings from the bivariate analysis showed that the patients care via telemedicine did not correlate significantly with their risk of High ACR state , p-value=0.755, but hypertensive patients were found to be slightly though not significantly statistically more inclined to have high ACR score, p-value=0.075 according to the chi-squared test of independence . The patients treatment with ACE/ARB agents did not converge significantly on their ACR state.
According to an Independent sample's t-test, the patients with high ACR (>=30 mg/gm) measured slightly higher mean glycated hemoglobin before the pandemic ( M=8.37) compared to patients with normal/low ACR ( Mean Hba1c=7.71) , the difference between the two groups was not significantly statistically nevertheless, p-value=0.055. The patients risk of having poor glycemic control ( having hba1c>=7.5% ) before the pandemic did not correlate significantly however with their risk of having high ACR levels, p-value=0.188 . But, the patients with high ACR ratio measured a significantly higher mean Glycated hemoglobin hba1c score ( M=8.50) post the lockdown compared to those patients who had normal/low ACR ( M=7.80) on average according to an independent samples t-test, p-value=0.043 . Also, a chi-squared test of association showed that the patients with abnormally high hba1c >=7.5% were found to be significantly more predicted to have high ACR score well above 30 mg/gm compared to patients with hba1c of less than 7.5% , p-value=0.018 . The patients mean body mass index did not differ significantly between the patients with normal or high ACR ratio neither before the lockdown or post the lockdown.
Table 3: Descriptive bivariate analysis of the measured diabetic control and clinical outcomes throughout the study period-before and after the lockdown . N=121
|
Before pandemic |
During/After pandemic |
test statisitc |
p-value |
||
|
Glycated Hemoglobin Hba1c level before |
7.87 (1.63) |
7.79 (1.66) |
Z=1.39 |
0.165 |
wilcoxon's signed rank |
|
High HBA1C index >7.5% |
|||||
|
No |
65 (53.7) |
59 (48.8) |
χ2 (1)=1.79 |
0.18 |
cochran q |
|
Yes |
56 (46.3) |
62 (51.2) |
|||
|
Albumin: Creatinine (ACR) Ratio level |
124.36 (601.40) |
93.31 (310.21) |
Z=1.16 |
0.248 |
wilcoxon's signed rank |
|
ACR ratio Level |
|||||
|
A:C ratio <30 mg/mmol |
91 (76) |
91 (76) |
χ2 (1)<0.0001 |
1 |
cochran q |
|
A:C ratio >=30 mg/mmol |
30 (24) |
30 (24) |
|||
|
Body Mass Index (BMI) score, mean (SD) |
32.55 (6.19) |
32.30 (6.41) |
Z=1.95,df=106 |
0.057 |
wilcoxon's signed rank |
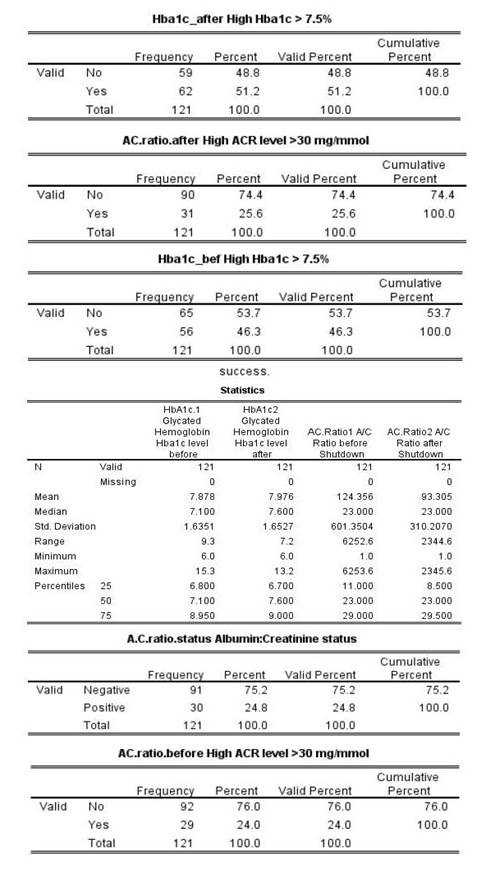
To assess the statistical significance of the change of patients measured glycemic control index and their ACR from before to after the lockdown the bivariate analysis methods were used to compare these score between the two time points. The resulted findings from the analysis, table-3, showed there was no statistically significant difference between the patients measured serum glycated hemoglobin (hba1c) index before and after the lockdown according to the Non-parametric Wilcoxon's signed rank paired samples test, p-value=0.165 . Also, the patients risk of having hba1c above 7.5% did not differ significantly between the two periods of time according to the Cochran's Q chi-squared test, p-value=0.180 . Also, the analysis yielded findings showed that there has been no significant change in patients mean measured ACR from before to post lockdown periods , p-value=0.248 . Indeed the patients with high ACR level continued to have abnormally high ACR ratio during the two time periods which are at least 6 months apart, p-value =1, according to Cochran's Q chi-squared test , therefore the patients with high ACR level before the lockdown also measured abnormally high ACR during the lockdown . The patients mean measured BMI score also did not differ significantly between before and after the pandemic lockdown periods , p-value=0.057.
|
Hba1c |
AC Ratio |
BMI |
Age |
|
|
Mean Serum Glycated Hemoglobin Hba1c Level. |
1 |
|||
|
Serum mean Albumin: Creatinine Ratio |
.003 |
1 |
||
|
Mean Body Mass Index (BMI) level |
-.098 |
-.068 |
1 |
|
|
Age In years |
-.266** |
.221* |
-.029 |
1 |
|
**. Correlation is significant at the 0.01 level (2-tailed). *. Correlation is significant at the 0.05 level (2-tailed). Table 4 : Bivariate correlations between the diabetic patients measured outcomes at baseline(before pandemic), n=121. |
||||
The bivariate Pearson's correlations test findings, table-4, showed that the patients mean serum Hba1c score did Not correlate significantly with their mean measured ACR ratio score before the pandemic, p-value>0.050 . However, the patients age had correlated significantly but Negatively with their mean measured serum hba1c scorem r=-0.266, p-value<0.010, older patients measured significantly lower serum hba1c score on average . But, according to the Pearson's correlations test the patients age had correlated positively and significantly with their mean measured serum ACR score, older patients tended to measured significantly higher mean serum ACR score in general , r=0.221, p-value<0.050.
Table 5: Multivariable Binary Logistic Regression Analysis of the patients odds of having high A/C ratio (>=30 mg/gm) during the study period.
|
Multivariable adjusted Odds Ratio (OR) |
95% C.I.for OR |
p-value |
||
|
Lower |
Upper |
|||
|
Sex=Male |
3.571 |
1.811 |
7.043 |
<0.001 |
|
Age in yers |
1.024 |
.990 |
1.060 |
.164 |
|
Received telemedicine care=yes |
1.039 |
.463 |
2.333 |
.926 |
|
ACE/ARB inhibitors intake= yes |
2.787 |
.736 |
10.552 |
.131 |
|
Positive history of hypertention |
.807 |
.191 |
3.417 |
.771 |
|
Time=During shutdown |
1.037 |
.555 |
1.939 |
.909 |
|
Mean Glycated Hemoglobin (hba1c) score |
1.267 |
1.048 |
1.533 |
.015 |
|
Body Mass Index (BMI) Score |
1.060 |
1.005 |
1.118 |
.033 |
|
Constant |
0.0005 |
<0.001 |
||
|
Dependent variable =High ACR index>30 mg/gm throghout the study time (No/Yes) . |
||||
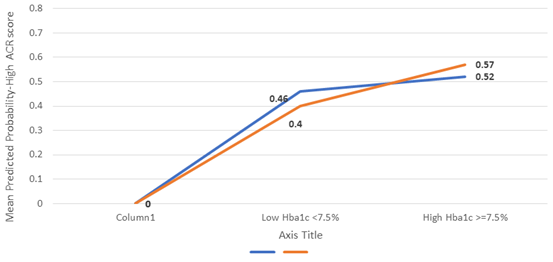
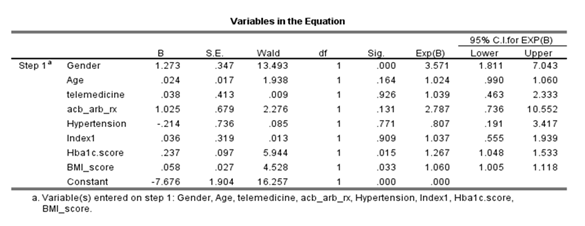
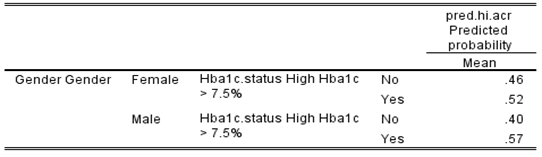
To assess the impact of patients glycemic control and the effect of telemedicine on the patients odds of having abnormally high ACR ratio the Multivariable Binary Logistic Regression Analysis (MLBR) was used to regress the patients odds of having abnormally high ACR ratio against their sociodemographic factors, telemedicine care, serum hba1c score comorbodity and ACR ratio . The resulted findings , table6, showed that male patients were found to be significantly more predicted to have abnormally high ACR ratio ( 3.571 times more ) compared to female patients on average, p-value<0.001 . The patients age ( in years) and their care with telemedicine and receiving ACE/ARB medications did not correlated significantly with their odds of having abnormally high ACR ratio throughout the study time ( before and after lockdown) . Also, the patients history of hypertension did not correlate significantly with odds of having abnormally high ACR ratio, p-value=0.771, and their odds of having abnormally high ACR ratio did not differ significantly between the two time points ( before vs after the lockdown) , p-value=0.909 . But , the patients mean measured serum glycated hemoglobin ( hba1c) index score had correlated significantly and positively with their odds of having abnormally high ACR ratio, for each additional one percent rise in the patients measured serum hba1c score their mean predicted odds of having abnormally high ACR score (>=30 mg/gm) tended to rise significantly by a factor equal to 1.267 times higher or 26.7% times higher on average, p-value= 0.015 , higher serum hba1c predicted higher odds of having abnormally high ACR ratio as such , note figure -A it is clear from the illustration that patients with higher hba1c above normal acceptable levels measured significantly higher mean predicted probability of having high ACR score for both genders, but males indeed exceeded females with respect to their probability of having high ACR with high Hba1c compared to females , an interaction effect between patients sex and their serum hba1c score and / state was tested in the iterative competing analysis models and it was found to be statistically non-significant as such the interaction effect was dismissed from the analysis model . Not only that but also the patients mean Body Mass Index ( BMI) score had correlated positively and significantly with their odds of having abnormally high ACR ratio, for each additional one percent rise in the patients mean BMI score the patients predicted odds of having abnormally high ACR tended to rise by a factor equal to 1.06 times higher or 6% times higher on average , p-value=0.033.
|
Multivariable adjusted Odds Ratio (OR) |
95% C.I.for OR |
p-value |
|||
|
Lower |
Upper |
||||
|
Gender=Male |
.813 |
.453 |
1.460 |
.488 |
|
|
Age-years |
.956 |
.927 |
.986 |
.004 |
|
|
Body Mass Index score |
.992 |
.946 |
1.039 |
.723 |
|
|
Hypertension=yes |
.587 |
.186 |
1.853 |
.364 |
|
|
ACE/ARB inhibitors intake= yes |
1.954 |
.694 |
5.503 |
.205 |
|
|
Received telemedicine care during pandemic=yes |
1.909 |
.904 |
4.031 |
.090 |
|
|
Time=Post-Pandemic |
1.238 |
.718 |
2.135 |
.442 |
|
|
A/C ratio status=Higher than Normal >30 mg/mmol |
3.358 |
1.528 |
7.379 |
.003 |
|
|
Constant |
6.463 |
.157 |
|||
|
Dependent variable =Dichotomized Repeated measures of HBA1C index>7.5 throghout the study time (No/Yes) |
|||||
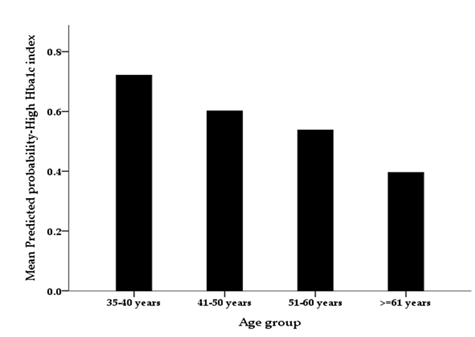
Table 6: To assess the statistical significance of the predictors that may help explain the patients glycemic control the Multivariable Binary Logistic Regression Analysis was also applied to patients odds of having poor glycemic control ( i.e., having hba1c score <7.5% versus hba1c>=7.5%) . The resulted findings from the multivariable analysis , table6, showed that the patients sex did not correlate significantly with their odds of having high hba1c score (>=7.5%), p-value=0.488 . However, the patients age (years) had correlated significantly but negatively with their odds of having poor glycemic control , for each additional year rise in the patients age their mean predicted odds of having poorer glycemic control ( i.e. having hba1c>=7.5%) declined by a factor equal to to 4.5% times less on average, p-value=0.004, see the figure-B . The patients measured other factors ( BMI score, History of hypertension, being treatmed with ACE/ARB agents) did not correlate significantly with their odds of having poorer glycemic control, but patients who received telemedicine care were found to be slightly more inclined to have poorer glycemic control compared to patients who had not received a tele-medicine care on average, the difference between them was not statistically significant however, p-value=0.090 . The patients odds of having poor glycemic control did not differ significantly between before and after the pandemic lockdown periods , p-value=0.442, according to the multivariable adjusted findings, but the analysis findings showed that the patients with higher than normal serum ACR index ( ACR>=30 mg/gm) were found to be significantly more predicted (3.358 times more ) to have poor glycemic control compared to patients with normal or low serum albumin-creatinine ACR ratio on average, p-value=0.003, the patients with higher ACR were significantly more inclined to poor glycemic control as such.
|
Column1 |
Female |
Male |
|
Low Hba1c <7.5% |
0.46 |
0.4 |
|
High Hba1c >=7.5% |
0.52 |
0.57 |
4. Discussion
The COVID-19 pandemic had presented significant challenges for the management of diabetic patients, with restrictions and lockdown measures limiting access to essential healthcare services and medications [9,11]. In response to these challenges, telehealth and eHealth platforms had emerged as promising solutions to ensure the timely and effective delivery of care to individuals with diabetes [11,12].
Telemedicine has proven to be invaluable during the COVID-19 era, benefiting patients with diabetes in primary and secondary care. It has been particularly useful for managing various types of diabetes, including T1D, T2D, gestational diabetes, and new cases. TM not only reduces the risk of COVID-19 infection but also improves glycemic control and alleviates diabetes distress [26].
Over the past two years, telemedicine has experienced significant growth in various medical fields, including diabetes care, thanks to the integration of new technological tools for data collection, transfer, and analysis. However, the widespread adoption of telemedicine has been hindered by several barriers, such as the absence of clear guidelines for data management and privacy, insufficient reimbursement policies, limited access to diabetes technologies, and the need for both patients and healthcare providers to become familiar with diverse digital tools [28].
This discussion aimed to provide a comprehensive analysis of the impact of the COVID-19 pandemic on diabetic patient outcomes and the utilization of telemedicine. It would draw on existing literature and statistical data analysis to shed light on the current state of affairs and identify areas for future research and improvement.
The present study analyzed a dataset comprising 121 diabetic patients to investigate the effects of the pandemic on patient outcomes and the adoption of telemedicine. The sample population consisted of 57% female and 43% male participants, with a mean age of 60.68 years. This demographic profile aligned with previous research indicating a higher prevalence of diabetes among women and the influence of age as a risk factor for diabetes and its complications [29].
The study revealed that 81.8% of the patients received telemedicine care during the pandemic, reflecting the widespread acceptance and utilization of telehealth technologies as an alternative means of providing healthcare services in times of restricted in-person care. This finding supported the recommendations for the use of telemedicine in ensuring the delivery of essential healthcare to diabetic patients in Saudi Arabia [21].
Interestingly, no significant differences were observed in the albumin/creatinine ratio (ACR) based on sex, age, receipt of telemedicine care, or treatment with ACE/ARB. However, male patients exhibited significantly higher odds of having a high ACR compared to female patients. This suggested a potential gender disparity in the development or progression of renal complications in diabetic individuals.
Moreover, the analysis demonstrated a significant increase in mean glycated hemoglobin (HbA1c) levels among patients with a high ACR after the pandemic compared to those with a normal ACR. This finding implies that the COVID-19 lockdown may have negatively affected glycemic control in diabetic patients with renal dysfunction. Previous research had highlighted the adverse effects of social isolation and limited access to healthcare on glycemic management in diabetic individuals [25]. While the utilization of telemedicine during the pandemic might have mitigated some of these negative effects, as evidenced by the high proportion of patients receiving telemedicine care, further investigation was necessary to assess the effectiveness of telemedicine in improving glycemic control and patient satisfaction in the specific context of Saudi Arabia.
Furthermore, the analysis examined the changes in measured outcomes before and after the pandemic lockdown. Surprisingly, no significant differences were found in mean HbA1c, ACR, or BMI between these time periods. This suggested that the COVID-19 pandemic and associated lockdown measures did not have a substantial impact on these parameters in the studied diabetic population. However, it was important to acknowledge that the analysis was limited to a specific dataset of 121 patients and might not fully represent the broader population of diabetic individuals.
The bivariate correlations at baseline showed no significant association between mean HbA1c and mean ACR levels. However, age exhibited a negative correlation with HbA1c levels, indicating that older patients had lower HbA1c levels, which was a positive finding in terms of glycemic control. Conversely, age correlated positively with ACR levels, suggesting that older patients had higher ACR levels, indicating a higher prevalence of renal complications in this population. These correlations highlighted f age as a potential risk factor for both glycemic control and renal function in diabetic patients.
Limitations of this study included the small sample size and the retrospective nature of the analysis, which might limit the generalizability of the findings. Additionally, the dataset relied on recorded information and might have been subject to errors or missing data. Future research should consider larger sample sizes, diverse populations, and prospective study designs to provide more robust evidence and address the limitations of the current analysis.
The findings of this study have important implications for future research in the field of telemedicine and diabetes management. Further investigation is needed to explore the long-term effects of telemedicine on glycemic control, patient satisfaction, and healthcare accessibility. Additionally, studies should focus on optimizing telemedicine platforms and interventions to enhance the overall management and outcomes of diabetic patients.
Based on this study, the following recommendations are suggested for future research and clinical practice:
- Further research should be conducted to evaluate the long-term effects of telemedicine on glycemic control, patient adherence to treatment plans, and overall healthcare outcomes in diabetic patients. Longitudinal studies with larger sample sizes and diverse populations would provide more robust evidence in this regard.
- Healthcare providers should be trained and educated on the effective utilization of telemedicine platforms for diabetes management. This includes the proper use of digital tools, communication strategies, and the integration of telemedicine into routine clinical practice.
- Strategies should be developed to address the gender disparity observed in the development or progression of renal complications among diabetic patients. Future studies should explore the underlying factors contributing to this disparity and develop targeted interventions to improve outcomes in both male and female patients.
- Efforts should be made to optimize telemedicine platforms and interventions to ensure equitable access to healthcare services for all diabetic patients, including those in rural or remote areas. This may involve addressing technological barriers, improving digital literacy, and ensuring the availability of telemedicine services in underserved communities.
- Collaboration between healthcare providers, policymakers, and technology experts is essential to develop comprehensive telemedicine guidelines and policies for diabetes management. These guidelines should address issues such as privacy and security, reimbursement mechanisms, and standards for telemedicine platforms.
- Patient education and empowerment should be emphasized in telemedicine interventions. Providing patients with the necessary knowledge and skills to actively participate in their own care, such as self-monitoring of blood glucose and medication management, can contribute to improved outcomes and self-management.
- Continued monitoring and evaluation of telemedicine programs are necessary to assess their effectiveness, identify areas for improvement, and ensure quality care delivery. Regular feedback from patients and healthcare providers can help refine telemedicine interventions and address any barriers or challenges encountered.
- By implementing these recommendations, healthcare systems can harness the potential of telemedicine to enhance diabetes management, improve patient outcomes, and increase access to quality care.
Author contributions
We would like to express our gratitude to all the participants who took part in this study and made this research possible. We also extend our appreciation to the healthcare professionals and staff at King Saud University Medical City for their support and assistance throughout the data collection process. Their contributions are greatly acknowledged.
Conflicts of interest
We declare that there are no conflicts of interest related to this research. We have no financial or personal relationships that could influence or bias the findings and interpretations presented in this study. Our objective is to provide unbiased and objective information to contribute to the scientific knowledge and understanding of telemedicine in diabetes management.
Conclusion
In conclusion, the present study contributes to the existing body of knowledge by providing insights into the impact of the COVID-19 pandemic on diabetic patient outcomes and the utilization of telemedicine. The findings underscore the importance of telehealth technologies in ensuring the continuity of care for diabetic patients during periods of restricted access to traditional healthcare services. The identified factors such as gender, glycemic control, and BMI can guide clinicians and researchers in tailoring interventions to mitigate the risk of renal complications in diabetic patients. However, further research is necessary to evaluate the effectiveness and long-term impact of telemedicine in the Saudi Arabian context and to explore additional factors that may influence patient outcomes.
References
- Galiero R, Pafundi P C, Nevola R, et al. The importance of telemedicine during covid-19 pandemic: a focus on diabetic retinopathy. Journal of Diabetes Research (2020): 1-8.
- Russo GT, Andreozzi F, Calabrese M, et al. Role of telemedicine during COVID-19 pandemic in type 2 diabetes outpatients: The AMD annals initiative. Diabetes Research and Clinical Practice 194 (2022): 110158.
- Borries TM, Dunbar A, Bhukhen A, et al. The impact of telemedicine on patient self-management processes and clinical outcomes for patients with Types I or II Diabetes Mellitus in the United States: A scoping review. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 13 (2019): 1353-1357.
- Dhediya R, Chadha M, Bhattacharya AD, et al. Role of Telemedicine in Diabetes Management. Journal of Diabetes Science and Technology (2022): 193229682210811.
- De Kreutzenberg SV. (2022). Telemedicine for the Clinical Management of Diabetes; Implications and Considerations After COVID-19 Experience. High Blood Pressure & Cardiovascular Prevention 29 (2022): 319-326.
- Wang H, Yuan X, Wang J, et al. Telemedicine maybe an effective solution for management of chronic disease during the COVID-19 epidemic. Primary Health Care Research & Development, 22 (2021): 48.
- Kusuma CF, Aristawidya L, Susanti CP, et al. A review of the effectiveness of telemedicine in glycemic control in diabetes mellitus patients. Medicine 101 (2022): 32028.
- Al-Sofiani ME, Alyusuf EY, Alharthi S, et al. Rapid Implementation of a Diabetes Telemedicine Clinic During the Coronavirus Disease 2019 Outbreak: Our Protocol, Experience, and Satisfaction Reports in Saudi Arabia. Journal of Diabetes Science and Technology (2020): 193229682094709.
- Nachimuthu S, R Vijayalakshmi, M Sudha, et al. Coping with diabetes during the COVID e 19 lockdown in India: Results of an online pilot survey. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 14 (2020): 579-582.
- Tourkmani AM, ALHarbi TJ, Bin Rsheed AM, et al. (2020) The impact of telemedicine on patients with uncontrolled type 2 diabetes mellitus during the COVID-19 pandemic in Saudi Arabia: Findings and implications. Journal of Telemedicine and Telecare 29 (2023): 390-398.
- Ghosh A, Gupta R, Misra AJD. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab Syndr 14 (2020): 273-276.
- Bitar H and Alismail S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: A rapid systematic review. DIGITAL HEALTH 7 (2021): 1-19.
- Lurie N and Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med 178 (2018): 745-746.
- Hollander JE and Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med 382 (2020): 1679-1681.
- Smith AC, Thomas E, Snoswell CL, et al. (2019) Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 26 (2020): 309-313.
- Zhou X, Snoswell CL, Harding LE, et al. (2020) The role of Telehealth in reducing the mental health burden from COVID-19. Telemed E Health 26 (2020): 377-379.
- Stevens WJM, van der Sande R, Beijer LJ, et al. scoping review on adverse effects. J Med Internet Res 21 (2019): 10736.
- Jahanshir A, Karimialavijeh E, Sheikh H, et al. Smartphones and medical applications in the emergency department daily practice. Emergency 5 (2017): 14.
- Monaghesh E and Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20 (2020):1193.
- Charles BL. Telemedicine can lower costs and improve access. Healthc Financ Manage 54 (2000): 66.
- Tourkmani AM, ALHarbi TJ, Bin Rsheed AM, et al. The impact of telemedicine on patients with uncontrolled type 2 diabetes mellitus during the COVID-19 pandemic in Saudi Arabia: Findings and implications. Journal of Telemedicine and Telecare 29 (2023): 390-398.
- Forde R, Arente L, Ausili D, et al. The impact of the COVID?19 pandemic on people with diabetes and diabetes services: A pan?European survey of diabetes specialist nurses undertaken by the Foundation of European Nurses in Diabetes survey consortium. Diabetic Medicine, 38 (2020): 14498.
- Eberle C & Stichling S. Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: a systematic review. Diabetology & Metabolic Syndrome 13 (2021): 95.
- Hosomi Y, Munekawa C, Hashimoto Y, et al. The effect of COVID-19 pandemic on the lifestyle and glycemic control in patients with type 1 diabetes: a retrospective cohort study. Diabetology International 13 (2021): 85-90.
- Stachteas P. The impact of the COVID-19 pandemic on the management of patients with chronic diseases in Primary Health Care 216 (2022): 445-448.
- Papazafiropoulou A. (2022). Telemedicine and diabetes during the COVID-19 era. Archives of Medical Science – Atherosclerotic Diseases 7 (2022): 131-135.
- Aberer F, Hochfellner DA & Mader JK. (2021). Application of Telemedicine in Diabetes Care: The Time is Now. Diabetes Therapy, 12 (2021): 629-639.
- Giani E, Dovc K, Dos Santos TJ, et al. Telemedicine and COVID ?19 pandemic: The perfect storm to mark a change in diabetes care. Results from a world?wide cross?sectional web?based survey. Pediatric Diabetes, 22(2021), 1115-1119.
- Zhang H, Ni J, Yu C, et al. Sex-Based Differences in Diabetes Prevalence and Risk Factors: A Population-Based Cross-Sectional Study Among Low-Income Adults in China. Frontiers in Endocrinology 10 (2019): 658.
- Camargo, L.M.A., Silva, R.P.M. and de Oliveira Meneguetti, D.U., 2019. Research methodology topics: Cohort studies or prospective and retrospective cohort studies. Journal of Human Growth and Development, 29(3), pp.433-436.
- Bikbov B, Purcell CA, Levey AS, et al. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The lancet 395 (2020): 709-733.
- Brough HA, Kalayci O, Sediva A, et al. Managing childhood allergies and immunodeficiencies during respiratory virus epidemics – the 2020 COVID-19 pandemic: a statement from the EAACI-section on pediatrics. Pediatr Allergy Immunol 31 (2020): 442-448.
- Deng SQ and Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med 9 (2020): 575.
- Gupta R, Hussain A, Misra AJD. Diabetes and COVID-19: Evidence, current status and unanswered research questions. Eur J Clin Nutr 74 (2020): 864-870.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet 395 (2020): 497-506.
- Jiang F, Deng L, Zhang L, et al. Review of the clinical characteristics of coronavirus disease 2019 (COVID-19). J Gen Intern Med 35 (2020): 1545-1549.
- Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19—studies needed. N Engl J Med 382 (2020): 1194-1196.
- Mousa D, Helal I, Alhejaili F, et al. Sun-137 prevalence of chronic kidney disease markers in Saudi Arabia: population based pilot study. Kidney International Reports 5 (2020): 258.
- van der Hoek L, Pyrc K, Jebbink MF, et al. Identification of a new human coronavirus. Nat Med 10 (2004): 368-373.
- Wu Z and McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323 (2020): 1239-1242.
- Jun Min. “Managing cardiovascular risk in people with chronic kidney disease: a review of the evidence from randomized controlled trials.” Therapeutic advances in chronic disease 2,4 (2011): 265-278.
- Alguwaihes AM, Al-Sofiani ME, Megdad M, et al. Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a single-centre retrospective study. Cardiovascular Diabetology, 19 (2020): 1-12.
- Bain SC, Czernichow S, Bøgelund M, Costs of COVID-19 pandemic associated with diabetes in Europe: a health care cost model. Current Medical Research and Opinion, 37 (2020): 27-36.
- Hafidh K, Abbas S, Khan A, et al. The Clinical Characteristics and Outcomes of COVID-19 Infections in Patients with Diabetes at a Tertiary Care Center in the UAE. Dubai Diabetes and Endocrinology Journal, 26 (2020): 158-163.