Right Ventricle Free Wall Strain to Detect Proximal Right Coronary Artery Lesion in Patients with Acute Inferior Myocardial Infarction
Article Information
Md. Owashak Faysal1*, Tuhin Haque2, Md. Mahbubur Rahman3, Rahatul Quadir4, Sharmin Ali5, Md. Rakibul Hasan6, Nurul Islam7, Md. Asifudduza8, Rezwana Rahman9
1Medical Officer, Department of Cardiology, National Institute of Cardiovascular Disease (NICVD), Dhaka, Bangladesh
2Professor of Cardiology Department, National Heart Foundation Hospital & Research Institute, Dhaka, Bangladesh
3Professor of Cardiology Department, National Institute of Cardiovascular Diseases(NICVD), Dhaka, Bangladesh
4Assistant Registrar, National Institute of Cardiovascular Diseases(NICVD), Dhaka, Bangladesh
5Medical Officer, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka, Bangladesh
6Junior Consultant, Department of Cardiology, Labaid Cardiac Hospital, Dhaka, Bangladesh
7Senior Medical Officer, Department of
Cardiology, National Heart Foundation Hospital & Research Institute, Dhaka, Bangladesh 8Junior Consultant, Department of Cardiology,
Labaid Cardiac Hospital, Dhaka, Bangladesh
9Resident, Department of Pediatric Hematology and Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
Corresponding author: Dr. Md. Owashak Faysal, Medical Officer, Department of Cardiology, National Institute of Cardiovascular Disease (NICVD), Dhaka, Bangladesh.
Received: May 06, 2023;Accepted: May 15, 2023;Published: July 07, 2023
Citation: Md. Owashak Faysal, Tuhin Haque, Rahatul Quadir, Sharmin Ali, Md. Rakibul Hasan, Nurul Islam, Md. Asifudduza, Rezwana Rahman. Right Ventricle Free Wall Strain to Detect Proximal Right Coronary Artery Lesion in Patients with Acute Inferior Myocardial Infarction. Cardiology and Cardiovascular Medicine . 7 (2023): 241-250.
Share at FacebookAbstract
Background: Prediction of the proximal right coronary artery lesion in the setting of acute inferior myocardial infarction is very crucial for the reduction of significant morbidity and mortality.
Objective: The objective of the study was to determine the validity of right ventricular free wall strain detected by spickle-tacking echocardiography for identifying proximal right coronary artery lesion in acute inferior myocardial infraction.
Methodology: This cross sectional observational study was carried out at the Department of Cardiology and the Department of Echocardiography of National Heart Foundation Hospital and Research Institute from March 2020 to February 2021. 80 patients with acute inferior MI were included in this study. Echocardiographic examination was done with the measurement of conventional parameters and strain analysis. Patients with RCA occluded proximal to right ventricular branch were assigned to group I and patients with RCA occluded distal to right ventricular branch were assigned to group II. Correlation was done with the echocardiographic and angiographic parameters.
Results: RV-FW strain was lower in group I patients compared to group II (-12.21±4.22 % vs -18.16±2.93 %). Based on ROC curves average RV- FW at a cut off value of ≥ -15.8 % predicted proximal RCA lesion with 83.0% sensitivity and 75.8% specificity which was much reliable than the sensitivity and specificity of other conventional parameters like FAC (44.7% and 39.4%), TAPSE (48.9% and 39.4%) and TDI-TV Sm (44.7% and 30.3%).
Conclusion: RV-FW strain at a cutoff value of ≥ -15.8 % is an independent predictor of the proximal RCA lesion in patients with acute inferior MI.
Keywords
Acute inferior myocardial infarction, Right coronary artery, Right ventricular free wall strain
Acute inferior myocardial infarction articles, Right coronary artery articles, Right ventricular free wall strain articles.
Article Details
Introduction
In worldwide coronary artery disease (CAD) is leading cause of mortality. The prevalence of CAD was first reported in 1976, which was 0.33% [1]. More than 17 million deaths globally each year that is 30% of all deaths, 80% of which occur in low-income and middle-income countries and this figure is expected to grow to 23.6 million by 2030. It alone caused 7 million deaths worldwide in 2010, an increase of 35% since 1990 [2]. Acute coronary syndrome (ACS) is a major cause of mortality in developing countries and is
responsible for a large number of hospitalizations annually [3]. ACS comprises non ST elevation ACS (NSTE-ACS), Unstable angina (UA) and ST elevation MI (STEMI) [4]. Inferior wall myocardial infarction (MI) occurs from a coronary artery occlusion with resultant decreased perfusion to that region of the myocardium. The inferior myocardium, is supplied by the right coronary artery in most patients. Because of left dominance, the left circumflex will supply the posterior descending coronary artery in about 6-10% of the population. The anterior wall of the heart inferior MIs have a better prognosis than those in other regions. About 40% of all MIs involve the inferior wall. The mortality rate of an inferior wall MI is less than 10% traditionally, However, several complicating factors that increase mortality, including right ventricular infarction, hypotension, bradycardia, heart block, and cardiogenic shock [5]. The RV is essentially supplied by the RCA in the case of right dominance in coronary circulation. The infundibulum is supplied by both RCA and LAD; anterior wall by the right ventricular branch of the RCA and LAD; inferior wall by the right ventricular branch and a small branch originating from the posterior descending artery and lateral wall by the RCA acute marginal artery. Dual blood supply to both anterior wall and infundibulum decreases the risk of ischemia. Whereas the inferior wall is the most susceptible to ischemia, lateral wall is also susceptible to moderate ischemia [6]. This sub-group of patients are associated with considerable immediate morbidity and mortality [7]. RV ischemia occurs in 50% of patients with inferior myocardial infarction, and may result in severe hemodynamic compromise associated with poor clinical outcome. RCA occlusion proximal to the RV branch results in RVFW dysfunction [8]. Patients with inferior MI, the presence of RVFW dysfunction was associated with a 2.6- times increased risk of mortality as well as statistically significant increases in secondary end points of morbidity such as ventricular arrhythmias, high grade AV block, and mechanical complications [9]. The occlusion in the proximal segment of the right ventricular branch of the RCA causes ischemia in a larger area. On biventricular performance, the ischemic, dyskinetic RVFW exerts mechanically disadvantageous effects. Depressed RV systolic function leads to a decrease in trans-pulmonary delivery of LV preload, resulting in diminished cardiac output. The ischemic right ventricle is stiff, dilated, and volume dependent, resulting in pandiastolic RV dysfunction and septally-mediated alterations in LV compliance, which are exacerbated by elevated intrapericardial pressure [8]. The early recognition of RVMI in a patient with acute MI is of prime importance, not only for prognostication purposes, but also because it can guide specific therapy, including aggressive primary PCI, with particular attention to RV branch revascularization, in order to limit the deleterious effects of this diagnosis [10]. Echocardiography is a non-invasive and available method for RV function assessment [11]. Because of the complex anatomy, non-invasive evaluation of the right ventricular functions may be challenging. American Society of Echocardiography and the European Association of Cardiovascular Imaging recommended the use of at least one parameter of the following: FAC, TAPSE, tissue Doppler imaging derived tricuspid annular systolic motion and MPI, which is obtained from tricuspid annulus for the global evaluation of the right ventricular functions [12]. Echocardiography was conducted to evaluate the RV involvement and to predict the proximal RCA occlusion in patients with inferior MI [13]. TAPSE has been proposed as a simple and reproducible parameter for quantitative assessment of RV systolic function, TAPSE is a widely recognized, clinically useful and feasible marker of right ventricular systolic dysfunction [14]. TAPSE only provides a measure of tricuspid displacement and it reflects only isolated metrics of the RV that do not fully capture the complexity of RV adaptation. It represents longitudinal function of the RV but it assumes that the movement of the basal segments can be representative of the entire RV function and, moreover, it is an angle-dependent measure [15]. It is not able to highlight regional abnormalities [16]. The FAC is a two-dimensional measure of right ventricular global systolic function is calculated as the difference in end-diastolic area and end- systolic area divided by the end-diastolic area [17]. FAC provides information about RV global functions rather than the segmental analysis, it may be insufficient regarding the prediction of the RCA occlusion [18]. By means of measurement of myocardial velocities, TDI allows quantitative assessment of RV systolic and diastolic function. In When compared to healthy individuals and patients without RV involvement with inferior myocardial infarction and RV involvement, the tricuspid lateral annular systolic and early diastolic velocities were significantly reduced [19]. The most important limitations of TDI are angle-dependent and influenced by myocardial tethering [20]. During recent years, deformation imaging called myocardial mechanics, have emerged as valuable tools for more comprehensive and reliable assessment of myocardial function [21]. In recent years, the speckle-tracking echocardiography, which is not affected by the angle, has been used in the evaluation of the right or left ventricular functions in various disorders. Although the strain was mainly developed for the evaluation of the LV, several studies had demonstrated its advantages in the subtle RV assessment in disorders such as pulmonary arterial hypertension, MI and congenital heart diseases [22]. Speckle tracking echocardiography is a relatively new, angle and user-independent technique used for the evaluation of myocardial function. Speckle tracking appears to be highly reproducible and minimally affected by intra-observer and inter-observer variability [23]. Speckle tracking has recently been extended for the analysis of RV function. This technique provides an objective quantification of global and segmental RV longitudinal strain [24, 25]. Because of the complex shape of this chamber, RV as¬sessment by conventional 2- dimensional imaging is difficult. 2-D strain analysis is a technique which more accurately evaluates RV function and offers an estimation of segmental and global deformation also in the early stages of myocardial dysfunction [15]. Speckle- tracking based RV free wall strain and LV GLS were decreased in the patient group with proximal RCA lesion compared to those with distal RCA lesion. In addition, it was also demonstrated that diseased RV free wall strain could detect the presence of the proximal RCA lesion [26]. Right ventricular FW strain value was a predictor of the RCA proximal occlusion. As RV lateral wall is perfused by the right ventricular branch of the RCA, a larger infarction may develop in RV by occlusion proximal to this branch. It may cause more severe myocardial necrosis and fibrosis, which may lead to a decrease in RV myocardial deformation measured with the speckle-tracking method. RV strain had a sensitivity of 60.5% and a specificity of 87.5% to determine RV dysfunction, global RV function using mean RV strain was more effective to diagnose RV dysfunction than segmental parameters [27]. RV strain is an excellent predictor of outcome and accurate, highly-feasible, fast and reproducible echocardiographic technique that provides important information about RV mechanics [27] and compared to other indices of RV function, with MRI based RVEF measurements has significantly better correlation [28]. Few study reported that RV strain to be the best parameter to identify patients with Right ventricular systolic dysfunction with a worst prognosis [29]. In one study, decreased baseline RVGLS was associated with poor short-term and long-term prognosis independent of other parameters, RVFWS showed only a tendency for mortality prediction [30].
Objectives
General objective
To determine the validity of right ventricular free wall strain detected by spickle-tacking echocardiography for identifying proximal right coronary artery lesion in acute inferior myocardial infraction.
Specific objectives
- To assess right ventricular function by Tricuspid annular plane systolic excursion(TAPSE), fractional area changes(FAC) & TDI-TV Sm.
- To measure right ventricular free wall strain by speckle- tracking echocardiography in patient with acute inferior
- To identify proximal RCA lesion in acute inferior MI by coronary angiography.
- To estimate the sensitivity & specificity of RV-FW strain, TAPSE, FAC and TV-TDI Sm to detect proximal right coronary artery
Methodology
This was a cross sectional observational study. A total of 80 patients were included in this study, 47 in Group-I (Proximal RCA lesion) and 33 in Group-II (Distal RCA lesion) by using Purposive sampling method. The study conducted from March 2020 to February 2021 at the Department of Cardiology and the Department of Echocardiography of the National Heart Foundation Hospital and Research Institute, Mirpur, Dhaka. Bangladesh.
Inclusion criteria
- Age over 18 years
- Symptomatic with at least 1 mm ST-segment elevation in the inferior deviation of ECG
Exclusion criteria
- Patients, having a LCX dominance in the coronary anatomy
- cardiogenic shock and hemodynamic instability
- A previous history of coronary intervention and MI
- A lesion > 50% in LAD and LCX arteries
- Concomitant moderate to severe valvular pathology
- Atrial fibrillation
- Atrioventricular block and ventricular arrhythmias
- Active infection
- Hepatic and chronic renal failure
- Severe pulmonary disease
- Cor pulmonale
- Poor echo window
Study procedure
86 patients who were admit at National Heart Foundation Hospital & Research Institute, Dhaka for coronary angiography with acute inferior MI fulfilling the inclusion criteria was included in the study. Meticulous history was taken and detailed clinical examination was performed in each patient. Demographic data such as age, sex, height (cm), weight (Kg) was noted. Risk factors were recorded for all patients. Patients baseline 12 lead ECG was performed. Blood sample was taken for Troponin, Blood sugar, HbA1C, Serum creatinine, Serum electrolytes, fasting lipid profile. Echocardiography was done for all patients. Coronary angiography was done. After fulfilling the exclusion criteria 80 patients were selected. Patients were categorized into two groups according to RCA lesions, proximal or distal to the right ventricular branch.
Statistical analysis
All the statistical analyses were performed by using SPSS version 23.0 for Windows. Chi-Square test with Yates correction was used to analyze the categorical variables, shown with cross tabulation. Student t-test was used for continuous variables. Receiver operating characteristic (ROC) curves was generated to determine the cutoff value for the best sensitivity, specificity, negative and positive predictive values of RV-FW strain with regard to diagnosis of proximal coronary artery lesion. A model with a cutoff value of RV-FW strain above ≥-15.8% was considered as positive. Sensitivity and specificity of the TAPSE, FAC, TDI-TV Sm and RV-FW strain evaluation of proximal coronary artery lesion was calculated. P-value <0.05 was considered statistically significant.
Results
This cross-sectional observational study was conducted in the Department of Cardiology, National Heart Foundation Hospital and Research Institute, Mirpur, Dhaka, over one year from March 2020 to February 2021 to evaluate the right ventricular functions with speckle-tracking and conventional echocardiography in patients with acute inferior MI and investigate the correlation between the echocardiographic parameters and the prediction of the proximal RCA lesion. A total of 86 patients were selected among the patients admitted in the department of cardiology, National Heart Foundation Hospital and Research Institute with acute inferior MI, within the study period. Among them 80 patients were fulfilled the inclusion and exclusion criteria. The main objective of this study was to evaluate the right ventricular functions with speckle-tracking and conventional echocardiography in patients with acute inferior MI and investigate the correlation between the echocardiographic parameters and the prediction of the proximal RCA lesion. Coronary artery lesions were divided into two groups. Patients with RCA occlusion proximal to right ventricular branch were included in group I and patients with RCA occlusion distal to right ventricular branch were included in group II.
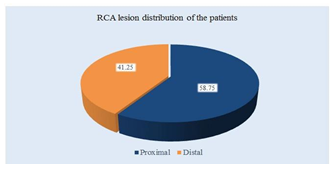
Table 1: RCA lesion by coronary angiography of the study patients (N=80)
|
Coronary angiography of RCA lesion |
n |
% |
|
Proximal |
47 |
58.75 |
|
Distal |
33 |
41.25 |
Among 80%, 47(58.75%) patients had proximal lesion and 33(41.25%) patients had distal lesion.
Table 2: Demographic variables of the study patients (N=80)
|
Demographic variables |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
||
|
n |
% |
n |
% |
||
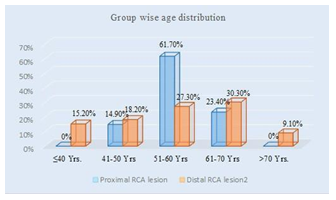
|
Age (years) |
|||||
|
≤40 yrs. |
0 |
0.0 |
5 |
15.2 |
0.948 |
|
41-50 yrs. |
7 |
14.9 |
6 |
18.2 |
|
|
51-60 yrs. |
29 |
61.7 |
9 |
27.3 |
|
|
61-70 yrs. |
11 |
23.4 |
10 |
30.3 |
|
|
>70 yrs. |
0 |
0.0 |
3 |
9.1 |
|
|
Mean ±SD |
56.3±6.1 |
56.1±12.0 |
|||
|
Range (min-max) |
42.0-69.0 |
30.0-72.0 |
|||
|
Sex |
|||||
|
Male |
45 |
95.7 |
32 |
97.0 |
0.632 |
|
Female |
2 |
4.3 |
1 |
3.0 |
|
|
Occupational status |
|||||
|
Service |
19 |
40.4 |
12 |
36.4 |
0.186 |
|
Business |
16 |
34.0 |
10 |
30.3 |
|
|
Farmer |
11 |
23.4 |
6 |
18.2 |
|
|
Others |
0 |
0.0 |
4 |
12.1 |
|
|
Housewife |
1 |
2.1 |
1 |
3.0 |
|
Table 2, showed that there was no significant difference between the two groups in regards to age. Male patients were predominant in both the groups. But gender distribution was similar between the groups. There is no significant difference between the two groups in respect of occupational status.
Table 3: Clinical profile of the study patients (N=80)
|
Clinical profile |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
||
|
Radiation of chest pain |
|||||
|
Back |
3 |
6.4 |
4 |
12.1 |
0.684 |
|
Both arm |
10 |
21.3 |
9 |
27.3 |
|
|
Left arm |
14 |
29.8 |
9 |
27.3 |
|
|
No radiation |
20 |
42.6 |
11 |
33.3 |
|
|
Duration of chest pain (hours) |
14.1±9.5 |
14.3±14.1 |
0.956 |
||
|
Pulse (beats/ min) |
75.4±11.2 |
68.4±8.0 |
0.003 |
||
|
SBP (mmHg) |
114.3±18.0 |
114.2±13.5 |
0.997 |
||
|
DBP (mmHg) |
72.1±10.6 |
77.0±11.6 |
0.057 |
||
Table 3 showed that 14(29.8%) patients had chest pain radiates to left arm in group I and 9(27.3%) in group II. Mean duration of chest pain was found 14.1±9.5 hours in group I and 14.3±14.1 hours in group II. Patients in group I were hemodynamically more unstable than those in group II as evidenced by increased mean pulse (75.4±11.2 vs 68.4±8.0 beats/min).
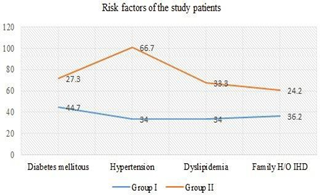
Table 5: Risk factors of the study patients (N=80)
|
Risk factors |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
||
|
Diabetes mellitus |
21 |
44.7 |
9 |
27.3 |
0.113 |
|
Hypertension |
16 |
34.0 |
22 |
66.7 |
0.004 |
|
Dyslipidemia |
16 |
34.0 |
11 |
33.3 |
0.947 |
|
Family H/O IHD |
17 |
36.2 |
8 |
24.2 |
0.257 |
|
Smoking status |
|||||
|
Smoker |
29 |
61.7 |
14 |
42.4 |
0.215 |
|
Ex-smoker |
2 |
4.3 |
3 |
9.1 |
|
|
Non smoker |
16 |
34.0 |
16 |
48.5 |
|
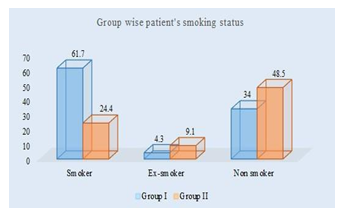
Table 5 showed that 16(34.0%) patients had hypertension in group I and 22(66.7%) in group II, which was statistically significant but others co-morbidities were not statistically significant between two groups.
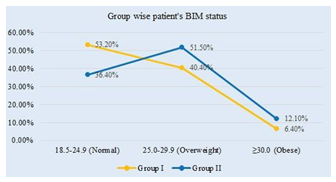
|
BMI (kg/m2) |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
||
|
18.5-24.9 (Normal) |
25 |
53.2 |
12 |
36.4 |
|
|
25.0-29.9 (Overweight) |
19 |
40.4 |
17 |
51.5 |
|
|
≥30.0 (Obese) |
3 |
6.4 |
4 |
12.1 |
|
|
Mean ±SD |
25.3±2.7 |
26.5±3.6 |
0.110 |
||
|
Range (min-max) |
20.8-32.0 |
18.8-32.0 |
|||
Table 4: BMI of the study patients (N=80)
Table 4 showed that mean BMI was 25.3±2.7 kg/m2 in group I and 26.5±3.6 kg/m2 in group II. The difference was not statistically significant between two groups.
|
FAC (%) |
|||||
|
Low (<30% Male; <35% Female) |
18 |
38.3 |
7 |
21.2 |
0.100 |
|
Normal (≥30% Male; ≥35% Female) |
29 |
61.7 |
26 |
78.8 |
|
|
Mean ±SD |
35.2±20.8 |
42.3±15.4 |
|||
|
Range (min-max) |
1.0-145.7 |
8.5-75.4 |
|||
|
TV annular Sm (cm/s) |
|||||
|
Low (<10 cm/s) |
10 |
21.3 |
3 |
9.1 |
0.004 |
|
Normal (≥10 cm/s) |
37 |
78.7 |
30 |
90.9 |
|
|
Mean ±SD |
11.1±2.4 |
12.7±2.2 |
|||
|
Range (min-max) |
6.4-16.0 |
7.0-16.0 |
|||
Table 6: Lipid profile of the study patients (N=80)
|
Lipid profile |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
|
Mean ±SD |
Mean ±SD |
||
|
Total cholesterol (mg/dl) |
194.1±34.2 |
187.7±32.4 |
0.407 |
|
TG (mg/dl) |
198.9±37.0 |
193.5±36.4 |
0.517 |
|
LDL (mg/dl) |
107.1±17.7 |
106.6±16.9 |
0.889 |
|
HDL (mg/dl) |
44.0±4.9 |
44.1±3.8 |
0.945 |
Table 6 showed that total cholesterol, TG, LDL and HDL were not statistically significant (p>0.05) between two groups.
Table 7: Biochemical parameters of the study patients (N=80)
|
Investigations |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
|
Mean ±SD |
Mean ±SD |
||
|
H e a m o g l o b i n (mg/dl) |
12.4±1.8 |
12.5±1.4 |
0.773 |
|
Random blood sugar (mmol/L) |
10.3±3.7 |
8.8±2.4 |
0.043 |
|
Serum creatinine (mg/dl) |
1.4±0.6 |
1.2±0.2 |
0.001 |
Table 7 showed biochemical parameters of the study patients. There was a significant (p<0.05) difference observed for random blood sugar which was higher in group I than group II (10.3±3.7 vs 8.8±2.4 mmol/L). The mean serum creatinine was significantly higher in group I than group II (1.4±0.6 vs 1.2±0.2 mg/dl).
Table 8: LVEF of the study patients (N=80)
|
Investigations |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
|
Mean ±SD |
Mean ±SD |
||
|
LVEF (%) |
44.6±6.2 |
45.8±5.4 |
0.379 |
|
Range (min-max) |
35.0-55.0 |
37.0-55.0 |
|
Table 8 showed that mean LVEF was 44.6±6.2 percent in group I and 45.8±5.4 percent in group II. The difference was not statistically significant (p>0.05) between two groups.
Table 9: 2-D & M-Mood echocardiographic parameters of the study patients (N=80)
|
Echocardiography- 2D |
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
||
|
n |
% |
n |
% |
||
|
TAPSE |
|||||
|
Low (<16 mm) |
18 |
38.3 |
8 |
24.2 |
0.089 |
|
Normal (≥16 mm) |
29 |
61.7 |
25 |
75.8 |
|
|
Mean ±SD |
15.9±3.3 |
17.1±3.0 |
|||
|
Range (min-max) |
8.0-20.0 |
12.0-24.4 |
|||
Table 9 showed that mean TAPSE was 15.9±3.3 mm in group I and 17.1±3.0 mm in group II. The mean FAC was 35.2±20.8 percent in group I and 42.3±15.4 percent in group II. The differences were not statistically significant between the two groups. The mean TV annular Sm was higher in group II patients compared to group I (11.1±2.4 cm/s vs 12.7±2.2 cm/s), which was statistically significant between the two groups.
Table 10: RV free wall strain (RV-FW strain) of the study patients (N=80)
|
Group I (Proximal RCA lesion) (n=47) |
Group II (Distal RCA lesion) (n=33) |
P value |
|||
|
Mean ±SD |
Mean ±SD |
||||
|
RV-FW strain (%) |
-12.21±4.22 |
-18.16±2.93 |
0.001 |
||
|
Range (min-max) |
-24.33 |
-(-3.00) |
-21.66 |
-(-12.13) |
|
Table 10 showed that mean RV-FW strain was lower in group I patients compared to group II (-12.21±4.22 percent vs -18.16±2.93 percent), which was statistically significant between the two groups.
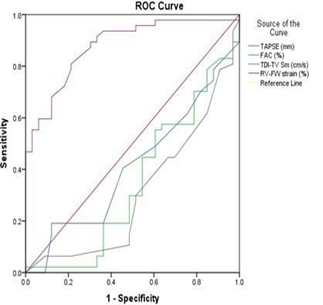
ROC curves for prediction of proximal coronary artery lesion is depicted in table XVII. Based on the ROC curves RV-FW strain had the best area under curve 0.878. ROC curves were constructed using TAPSE, FAC, TDI-TV Sm and RV-FW strain of the patients with proximal coronary artery lesion, which gave a RV-FW strain cut off value of (≥-15.8 percent) as the value with a best combination of sensitivity and specificity for proximal coronary artery lesion. At this cut-off value the sensitivity and specificity of RV-FW strain in diagnosing for proximal coronary artery lesion were found to be 83.0% and 75.8%, respectively. At this cut-off value the sensitivity and specificity of TAPSE in diagnosing proximal coronary artery lesion were found to be 48.9% and 39.4%, respectively. At this cut- off value the sensitivity and specificity of FAC in diagnosing proximal coronary artery lesion were found to be 44.7% and 39.4%, respectively. At this cut-off value the sensitivity and specificity of TDI-TV Sm in diagnosing proximal coronary artery lesion were found to be 44.7% and 30.3%, respectively.
Table 11: Distribution of the study patients according to in-hospital outcome. (N=100)
|
Cut of value |
Sensitivity |
Specificity |
Area under the ROC curve |
95% Confidence interval (CI) |
||
|
Lower bound |
Upper bound |
|||||
|
TAPSE (mm) |
<16.0 |
48.9 |
39.4 |
0.413 |
0.287 |
0.539 |
|
FAC (%) |
<37.0 |
44.7 |
39.4 |
0.350 |
0.225 |
0.476 |
|
TDI-TV Sm (cm/s) |
<11.5 |
44.7 |
30.3 |
0.311 |
0.192 |
0.430 |
|
RV-FW strain (%) |
≥-15.8 |
83.0 |
75.8 |
0.878 |
0.804 |
0.953 |
Discussion
The main finding of this study is that, among 80 patients, 47(58.75%) patients had proximal RCA lesion (group I) and 33(41.25%) patients had distal RCA lesion (group II). The RV-FW strain was found lower in group I patients compared to group II (-12.21±4.22 % vs -18.16±2.93 %), which was statistically significant between the two groups. Gecmen et al. (2018) [31] reported RV-FW strain (-11.56±2.8% vs. -16.17±4.2%, was also significantly lower in group 1 compared to group 2. The finding of RV scar and stunning which were demonstrated with the cardiac MRI compared to the findings of a study conducted with the speckle-tracking echocardiography. Regarding the results of this study, RV peak longitudinal strain value was superior over TAPSE and TDI in showing the scar [32]. In a study [26] focused on patients with the stable coronary disease, who were treated because of RCA lesions, it was shown that speckle-tracking based RV free strain. With proximal RCA lesion compared to those with distal RCA lesion LV GLS were decreased in the patient group. Furthermore, it was also demonstrated that RV free strain had a predictive value for the presence of the RCA proximal lesion. Chang et al. (2014) [26] observed the mean RVLS-FW was found -16.04±5.4% in proximal RCA lesion and -21.18±4.6% in distal RCA lesion. The difference was statistically significant between two groups. The different sensitivity & specificity with different cut of value of strain by different study may be due to use of different echo machine, patient’s population also different. In this study we have observed on the ROC curves RV-FW strain had area under curve 0.878. ROC was constructed by using RV-FW strain, which gave a cut off value ≥-15.8%, with 83.0% sensitivity and 75.8% specificity for prediction of proximal coronary artery lesion. Gecmen et al. (2018) [31] revealed the ROC analysis, RV-FW strain >-14.75% predicted proximal RCA occlusion with 83% sensitivity and 61% specificity. Roshdy et al. (2018) [33] had a cutoff value of ≥-19.7% for RV average FWLS had a sensitivity of 91.7% and specificity of 70.5% for diagnosis of proximal significant RCA stenosis. Gecmen et al. (2018) [31] reported 41 patients, who were included in Group 1 had an RCA occlusion proximal to right ventricular branch and the remaining 36 patients, who were included in Group 2 had an RCA occlusion distal to right ventricular branch. Chang et al. (2014) [26] reported 87(61.2%) patients had proximal RCA lesion and 55(38.8%) had distal RCA lesion. Roshdy et al. (2017) [33] observed that 34 patients had proximal RCA stenosis and 20 had without proximal RCA stenosis. In present study, RV-FW strain evaluation for inferior myocardial infarction,39 true positive cases, 8 false positive cases,8 false negative cases and 25 true negative cases were identified by proximal coronary artery lesion. The current study showed that there was no significant difference in age between the two groups with and without the proximal RCA. The mean age 56.3±6.1 was in proximal RCA group and 56.1±12.0 years in distal RCA group. Similar observation was found by Gecmen et al (2018) [31], which showed the mean age of the patients was 58.2±11.6 years in group 1 and 59.8±9.25 years in group 2 with no statistically significant difference between two groups. Chang et al. (2014) [26] reported the mean age was 63.67±11.47 years were entered for analysis. Roshdy et al. (2017) [33] observed the mean age of 58.9±8.4 years in group A and 59 ± 8.4 years in group B. This study showed that male patients were predominant in both the groups. But gender distribution was similar between the groups. Gecmen et al. (2018) [31] observed 35(85.0%) patients were males in group 1 and 27(75.0%) in group 2. Between two groups, the difference was not statistically significant. Chang et al. (2014) [26] and Roshdy et.al., (2017) [33] had also found no statistically significant difference between the two groups. In this present study, the mean BMI was found 25.3±2.7 kg/m2 in group I and 26.5±3.6 kg/m2 in group II. Between two groups, the difference was not statistically significant. Chang et al. (2014) [26] also found there was no statistically significant difference between groups with BMI. Finding of Gecmen et al. (2018) [31] is also in agreement with our observation. The current study showed that 16(34.0%) patients had hypertension in group I and 22(66.7%) in group Which was statistically significant but others co- morbidities were not statistically significant between two groups. This may be due to high prevalence of HTN in our group II patients. Chang et al. (2014) [26] observed diabetes mellitus, hypertension and hyperlipidemia were not statistically significant between two groups. Roshdy, et al. (2018) [33] also observed type 2 diabetes mellitus, hypertension and Family H/O CAD were not statistically significant between groups. Gecmen et al. (2018) [31] reported 26 of the patients (63.4%) had diabetes mellitus in group 1 and 18(50.0%) in group 2. The difference was not statistically significant between two groups. This study showed that total cholesterol, TG, LDL and HDL were not statistically significant between two groups. Gecmen et al. (2018) [31] reported the mean LDL was found 116.2±38.4 mg/dl in group 1 and 124.3±39.6 mg/dl in group II. The difference was not statistically significant between two groups. Chang et al. (2014) [26] also observed no statistically significant difference between two groups. This study showed that 29(61.7%) patients was found smoker in group I and 14(42.4%) in group II. The difference was not statistically significant of two groups. Chang et al. (2014) [26] reported 16(18.4%) patients were smoker in RCA positive and 7(12.7%) in RCA negative. The difference was not statistically significant among two groups. Roshdy et al. (2018) [33] observed 18(75%) patients were smoker in group I and 23(52.3%) in group II with no statistically significant difference. In this study we have observed patients in group I were hemodynamically more unstable than those in group II as evidenced by increased mean pulse. Gecmen et al. (2018) [31] reported systolic and diastolic blood pressure values and heart rate values of the patients were 143.5±26.8, 81.4±13.5 mmHg and 78.8±15.4 bpm. The mean systolic, diastolic blood pressure, heart rate and door to reperfusion were not statistically significant between two groups. Chang et al. (2014) [26] reported there is no statistically significant difference of meal pulse and mean blood pressure between the two groups. In this study, regarding the distribution of patients according to biochemical parameters, we found there was a significant difference of random blood sugar which was higher in group I than group II. The mean serum creatinine was significantly higher in group I than group II but other investigations were not statistically significant between the two groups. Gecmen et al. (2018) [31] reported the mean serum creatinine was found 0.88±0.22 mg/dl in group 1 and 0.85±0.22 mg/dl in group 2. The median glucose was found 140 mg/dl in group 1 and 141.5 mg/dl in group 2. The difference was not statistically significant between two groups. Chang et al. (2014) [26] had not found any statistically significant difference of serum creatinine between two groups. This study showed that mean LVEF was found 44.6±6.2 percent in group I and 45.8±5.4 percent in group II. The difference was not statistically significant between two groups. Gecmen et al. (2018) [31] and Chang et al. (2014) [26] also didn’t observed any statistically significant difference of LVEF between two groups. Present study showed that mean TAPSE was found 15.9±3.3 mm in group I and 17.1±3.0 mm in group II. The mean FAC was found 35.2±20.8 percent in group I and 42.3±15.4 percent in group II. The difference was not statistically significant between the two groups. Gecmen et al. (2018) [31] reported the mean RV TAPSE and FAC were significantly higher in group I compared to group II. But as FAC provides information only about RV global functions rather than the segmental analysis, that may be insufficient regarding the prediction of the RCA occlusion. Chang et al. (2014) [26] observed the mean TAPSE was found 1.85±0.5 cm and 2.01±0.46 cm and RV FAC was found 68.65±13.0 percent and 71.21±14.41% in proximal RCA lesion and distal RCA lesion respectively. The difference was not statistically significant between two groups. Some earlier studies had shown good correlation of TAPSE and RV FAC with ECG evidence of RV infarction, but the number of patients was less and there was no angiographic correlation. TAPSE also has some limitations like, its measurement is restricted to longitudinal function of RV free wall and functional status of LV may have an influence on it. In current study that mean TDI-TV Sm was found higher in group II patients compared to group I (11.1±2.4 cm/s vs 12.7±2.2 cm/s), which was statistically significant between the two groups. In comparison with Gecmen et al. (2018) [31] showed TDI-TV Sm was also significantly higher in group 1 compared to group II. This study showed that sensitivity of TAPSE was 48.9% and specificity was 39.4%. The sensitivity of FAC was 44.7 % and specificity 39.4%. The sensitivity and specificity of TDI-TV Sm was 44.7% and 30.3% respectively. In comparison with these parameters, the sensitivity of RV-FW strain was 83.0%and specificity was 75.8%. The sensitivity and specificity of RV FW strain is much reliable than the conventional echocardiographic parameters. Gecmen et al. (2018) [31] also reported that the Right ventricular free wall strain may show a subclinical RV dysfunction in patients with proximal lesion of RCA without impairing the right ventricular systolic functions such as TAPSE, FAC, TDI-TV Sm. The Roshdy et al. (2018) [33] and some other studies are near to our results, whereas others are concordent to some degree. Previous studies showed the correlation between the angiographic evidence of proximal RCA lesion in acute inferior MI with different echocardiographic parameters. The present study reveals that, decrease RV-FW strain is an important predictor of proximal RCA lesion in acute inferior MI patients which has a high sensitivity and specificity than other conventional echocardiographic parameters. Early prediction of proximal RCA lesion can facilitate the early effective management of these group of population and can reduce the morbidity and mortality.
Conclusion
Decreased RV-FW strain is a predictor of the presence of proximal RCA in patients with acute inferior MI. It can impair without any impairment of other parameters. The decreased RV-FW strain might be associated with morbidity and mortality in this patient group.
Limitations of the Study
This is a single-center study and non-randomized sampling was done instead of random sampling. Therefore, the results of the study may not reflect the exact picture of the country. Only patients with good image quality were included in this study, because the image quality is the basic requirement for strain assessment. Lack of prognostic information due to lack of follow-up.
Recommendations
RVFW Strain measurement using 2D speckle-tracking echocardiography can be used to detect proximal right coronary artery lesion in acute inferior MI patients and can help in early assessment and effective management to reduce significant morbidity and mortality in these patients group. Further studies with larger number of enrolled subjects and randomized trials are needed for detailed evaluation of this issue. Long term follows up is also recommended.
Ethical Issue
The study was approved by the Institutional Review Board on National Heart Foundation Hospital & Research Institute, Dhaka, Bangladesh.
References
- Malik Congenital and acquired heart diseases (a survey of 7062 persons) Bangladesh Med Res Counc Bull 2 (1976): 115-119.
- Rahman MS, Malik F, Ahmed N, Badiuzzaman M, Ahmed MN, et In-hospital outcome of Non ST Elevated Myocardial Infarction (NSTEMI) in National Heart Foundation Hospital & Research Institute, Dhaka. JNHFB 6 (2017): 33-37.
- Murray CJ, Lopez Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 349 (1997): 1269-1276.
- Daga LC, Kaul U, Mansoor A. Approach to STEMI and J Assoc Physicians India 59 (2011): 19-25.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372 (2021):
- Rallidis LS, Makavos G, Nihoyannopoulos Right ventricular involvement in coronary artery disease: role of echocardiography for diagnosis and prognosis. Journal of the American Society of Echocardiography 27 (2014): 223-229.
- Shah PK, Maddahi J, Berman DS, Pichler M, Swan Scintigraphically detected predominant right ventricular dysfunction in acute myocardial infarction: clinical and hemodynamic correlates and implications for therapy and prognosis. Journal of the American College of Cardiology 6 (1985): 1264-1272.
- Goldstein JA. Pathophysiology and management of right heart J Am Coll Cardiol 40 (2002): 841-853.
- Hamon M, Agostini D, Le Page O, Riddell JW, Hamon
- Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: meta- analysis. Critical care medicine 36 (2008): 2023-2033.
- Kakouros N, Cokkinos Right ventricular myocardial infarction: pathophysiology, diagnosis, and management. Postgraduate medical journal 86 (2010): 719-728.
- William V, El Kilany W. Assessment of right ventricular function by echocardiography in patients with chronic heart failure. The Egyptian Heart Journal 70 (2018): 173-
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European Heart Journal-Cardiovascular Imaging 16 (2015): 233-271.
- El Sebaie MH, El Khateeb Right ventricular echocardiographic parameters for prediction of proximal right coronary artery lesion in patients with inferior wall myocardial infarction. Journal of the Saudi Heart Association 28 (2016): 73-80.
- Kjaergaard J, Iversen KK, Akkan D, Møller JE, Køber LV, et Predictors of right ventricular function as measured by tricuspid annular plane systolic excursion in heart failure. Cardiovascular ultrasound 7 (2009): 1-7.
- Iacoviello M, Monitillo F, Citarelli G, Leone M, Grande D, et Right ventriculo-arterial coupling assessed by two-dimensional strain: A new parameter of right ventricular function independently associated with prognosis in chronic heart failure patients. International journal of cardiology 241 (2017): 318-321.
- Focardi M, Cameli M, Carbone SF, Massoni A, De Vito R, et al. Traditional and innovative echocardiographic parameters for the analysis of right ventricular performance in comparison with cardiac magnetic European Heart Journal-Cardiovascular Imaging 16 (2015): 47-52.
- Michael SL, Merlo CL, Basch CE, Wentzel KR, Wechsler
- Critical connections: health and academics. J Sch Health 85 (2015): 740-58.
- Lemarié J, Huttin O, Girerd N, Mandry D, Juillière Y, et Usefulness of speckle-trackingimagingforrightventricular assessment after acute myocardial infarction: a magnetic resonance imaging/echocardiographic comparison within the relation between aldosterone and cardiac remodeling after myocardial infarction study. Journal of the American Society of Echocardiography, 28 (2015): 818-827.
- Bleeker GB, Steendijk P, Holman ER, Yu CM, Breithardt OA, et Assessing right ventricular function: the role of echocardiography and complementary technologies. Heart 92 (2006): i19-i26.
- Matteo Cameli MD, Stefania Sparla MD, Maurizio Losito MD, Francesca M Righini MD, Daniele Menci MD, et Correlation of left atrial strain and Doppler measurements with invasive measurement of left ventricular end diastolic pressure in patients stratified for different values of ejaction fraction First published (2015).
- Dandel M, Lehmkuhl H, Knosalla C, Suramelashvili N, Hetzer Strain and strain rate imaging by echocardiography-basic concepts and clinical applicability. Current cardiology reviews 5 (2009): 133- 148.
- Mondillo S, Galderisi M, Mele D, Cameli M, Lomoriello VS, et Speckle-tracking echocardiography: a new technique for assessing myocardial function. Journal of Ultrasound in Medicine 30 (2011): 71-83.
- Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, et Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. Journal of the American Society of Echocardiography 23 (2010): 351-369.
- Cameli M, Righini FM, Lisi M, Mondillo Right ventricular strain as a novel approach to analyze right ventricular performance in patients with heart failure. Heart failure reviews 19 (2014): 603-610.
- Muraru D, Onciul S, Peluso D, Soriani N, Cucchini U, et al. Sex-and method-specific reference values for right ventricular strain by 2-dimensional speckle-tracking Circulation: Cardiovascular Imaging 9 (2016): e003866.
- Chang WT, Tsai WC, Liu YW, Lee CH, Liu PY, et al. Changes in right ventricular free wall strain in patients with coronary artery disease involving the right coronary artery. Journal of the American Society of Echocardiography 27 (2014): 230-238.
- Tadic M, Pieske-Kraigher E, Cuspidi C, Morris DA, Burkhardt F, et Right ventricular strain in heart failure: Clinical perspective. Archives of cardiovascular diseases 110 (2017): 562-571.
- Leong DP, Grover S, Molaee P, Chakrabarty A, Shirazi M, et Nonvolumetric echocardiographic indices of right ventricular systolic function: validation with cardiovascular magnetic resonance and relationship with functional capacity. Echocardiography 29 (2012): 455-463.
- Mouton S, Ridon H, Fertin M, Pentiah AD, Goémine C, et 2D-speckle tracking right ventricular strain to assess right ventricular systolic function in systolic heart failure. Analysis of the right ventricular free and posterolateral walls. International journal of cardiology 245 (2017): 190-195.
- Nagy VK, Széplaki G, Apor A, Kutyifa V, Kovács A, et Role of right ventricular global longitudinal strain in predicting early and long-term mortality in cardiac resynchronization therapy patients. PloS one 10 (2015): e0143907.
- Gecmen C, Candan O, Kahyaoglu M, Kalayci A, Cakmak EO, et Echocardiographic assessment of right ventricle free wall strain for prediction of right coronary artery proximal lesion in patients with inferior myocardial infarction. The international journal of cardiovascular imaging 34 (2018): 1109-1116.
- Hutyra M, Skála T, Horák D, Köcher M, Tüdös Z, et al. Echocardiographic assessment of global longitudinal right ventricular function in patients with an acute inferior ST elevation myocardial infarction and proximal right coronary artery occlusion. The international journal of cardiovascular imaging 31 (2015): 497-507.
- Roshdy HS, El-Dosouky II, Soliman High-risk inferior myocardial infarction: Can speckle tracking predict proximal right coronary lesions. Clinical cardiology 41 (2018): 104-110.