Retained Pessary Erosion into the Bladder and the Importance of a Reliable Patient Tracking Method
Article Information
Laena Hines, Jeanne O’Brien*, Divya Ajay
University of Rochester Medical Center, Department of Urology, NY, USA
*Corresponding author: Jeanne O’Brien, Department of Urology, University of Rochester Medical Center, 601 Elmwood Ave, Rochester, NY 14642, USA
Received: 27 October 2021; Accepted: 08 November 2021; Published: 29 November 2021
Citation:
Laena Hines, Jeanne O’Brien, Divya Ajay. Retained Pessary Erosion into the Bladder and the Importance of a Reliable Patient Tracking Method. Journal of Women’s Health and Development 4 (2021): 173-177.
Share at FacebookAbstract
Pessary use in the elderly population is a reasonable and well-utilized option for managing symptomatic pelvic organ prolapse and stress urinary incontinence (SUI). However, pessary use has risks to consider in patients that may be lost to follow up. We present the case of an 89-year-old woman with dementia, uterine prolapse managed with Gellhorn pessary, and recurrent UTIs who was found to have an eroded pessary in her bladder. We review pessary use for pelvic organ prolapse and SUI and associated risks, recurrent urinary tract infection guidelines, the continued importance of physical exam, and we propose a database to ensure proper follow up for pessary patients.
Keywords
Pessary, Dementia, Recurrent UTIs, Bladder erosion, Pelvic exam
Pessary articles Pessary Research articles Pessary review articles Pessary PubMed articles Pessary PubMed Central articles Pessary 2023 articles Pessary 2024 articles Pessary Scopus articles Pessary impact factor journals Pessary Scopus journals Pessary PubMed journals Pessary medical journals Pessary free journals Pessary best journals Pessary top journals Pessary free medical journals Pessary famous journals Pessary Google Scholar indexed journals Dementia articles Dementia Research articles Dementia review articles Dementia PubMed articles Dementia PubMed Central articles Dementia 2023 articles Dementia 2024 articles Dementia Scopus articles Dementia impact factor journals Dementia Scopus journals Dementia PubMed journals Dementia medical journals Dementia free journals Dementia best journals Dementia top journals Dementia free medical journals Dementia famous journals Dementia Google Scholar indexed journals Recurrent UTIs articles Recurrent UTIs Research articles Recurrent UTIs review articles Recurrent UTIs PubMed articles Recurrent UTIs PubMed Central articles Recurrent UTIs 2023 articles Recurrent UTIs 2024 articles Recurrent UTIs Scopus articles Recurrent UTIs impact factor journals Recurrent UTIs Scopus journals Recurrent UTIs PubMed journals Recurrent UTIs medical journals Recurrent UTIs free journals Recurrent UTIs best journals Recurrent UTIs top journals Recurrent UTIs free medical journals Recurrent UTIs famous journals Recurrent UTIs Google Scholar indexed journals Bladder erosion articles Bladder erosion Research articles Bladder erosion review articles Bladder erosion PubMed articles Bladder erosion PubMed Central articles Bladder erosion 2023 articles Bladder erosion 2024 articles Bladder erosion Scopus articles Bladder erosion impact factor journals Bladder erosion Scopus journals Bladder erosion PubMed journals Bladder erosion medical journals Bladder erosion free journals Bladder erosion best journals Bladder erosion top journals Bladder erosion free medical journals Bladder erosion famous journals Bladder erosion Google Scholar indexed journals Pelvic exam articles Pelvic exam Research articles Pelvic exam review articles Pelvic exam PubMed articles Pelvic exam PubMed Central articles Pelvic exam 2023 articles Pelvic exam 2024 articles Pelvic exam Scopus articles Pelvic exam impact factor journals Pelvic exam Scopus journals Pelvic exam PubMed journals Pelvic exam medical journals Pelvic exam free journals Pelvic exam best journals Pelvic exam top journals Pelvic exam free medical journals Pelvic exam famous journals Pelvic exam Google Scholar indexed journals pelvic organá articles pelvic organá Research articles pelvic organá review articles pelvic organá PubMed articles pelvic organá PubMed Central articles pelvic organá 2023 articles pelvic organá 2024 articles pelvic organá Scopus articles pelvic organá impact factor journals pelvic organá Scopus journals pelvic organá PubMed journals pelvic organá medical journals pelvic organá free journals pelvic organá best journals pelvic organá top journals pelvic organá free medical journals pelvic organá famous journals pelvic organá Google Scholar indexed journals intra-vesical pessary articles intra-vesical pessary Research articles intra-vesical pessary review articles intra-vesical pessary PubMed articles intra-vesical pessary PubMed Central articles intra-vesical pessary 2023 articles intra-vesical pessary 2024 articles intra-vesical pessary Scopus articles intra-vesical pessary impact factor journals intra-vesical pessary Scopus journals intra-vesical pessary PubMed journals intra-vesical pessary medical journals intra-vesical pessary free journals intra-vesical pessary best journals intra-vesical pessary top journals intra-vesical pessary free medical journals intra-vesical pessary famous journals intra-vesical pessary Google Scholar indexed journals dementia articles dementia Research articles dementia review articles dementia PubMed articles dementia PubMed Central articles dementia 2023 articles dementia 2024 articles dementia Scopus articles dementia impact factor journals dementia Scopus journals dementia PubMed journals dementia medical journals dementia free journals dementia best journals dementia top journals dementia free medical journals dementia famous journals dementia Google Scholar indexed journals vaginal ultrasound articles vaginal ultrasound Research articles vaginal ultrasound review articles vaginal ultrasound PubMed articles vaginal ultrasound PubMed Central articles vaginal ultrasound 2023 articles vaginal ultrasound 2024 articles vaginal ultrasound Scopus articles vaginal ultrasound impact factor journals vaginal ultrasound Scopus journals vaginal ultrasound PubMed journals vaginal ultrasound medical journals vaginal ultrasound free journals vaginal ultrasound best journals vaginal ultrasound top journals vaginal ultrasound free medical journals vaginal ultrasound famous journals vaginal ultrasound Google Scholar indexed journals urinary bladder articles urinary bladder Research articles urinary bladder review articles urinary bladder PubMed articles urinary bladder PubMed Central articles urinary bladder 2023 articles urinary bladder 2024 articles urinary bladder Scopus articles urinary bladder impact factor journals urinary bladder Scopus journals urinary bladder PubMed journals urinary bladder medical journals urinary bladder free journals urinary bladder best journals urinary bladder top journals urinary bladder free medical journals urinary bladder famous journals urinary bladder Google Scholar indexed journals
Article Details
1. Introduction
Pessary use in women with pelvic organ prolapse or SUI is a conservative alternative treatment for managing pelvic organ prolapse in patients who are not interested in, or are poor candidates, for surgical intervention. Given the growing aging population, having reliable non-surgical options are essential in the management of these patients. While pessary use is often considered relatively benign, some studies show that at long term follow up, up to 50% have some complications [1]. One large disadvantage of pessary use is the risk of pessary retention in patients who are lost to follow up. While self-management of vaginal pessary may increase patient autonomy, improve compliance and length of use, and improve quality of life [2], concern exists that self-manage-ment may lead to increased pessary retention and, possibly, complications. Case reports and systematic reviews [3] exist in the literature demonstrating potential risks of pessary use. Gorden et al details two cases of patients presenting with rectovaginal fistulas from Gellhorn pessary use, one of who had dementia and was lost to follow up with retained pessary [4]. Riberio and colleagues present a case of a neglected vaginal pessary presenting with pseudo-hematuria, and on CT scan was found to have retro-vesically retained vaginal pessary that was removed [1]. Case reports of vesicovaginal fistulas due to pessary exist for not only forgotten pessaries, but also in well maintained pessaries [5, 6]. We present a case of a vesicovaginal fistula with a migrated intra-vesical pessary.
2. Case Presentation
We present an 89 years woman with a significant past medical history of dementia, pelvic organ prolapse managed by pessary, and urinary tract infection. She originally had her pessary placed in the 1980s and self-managed it with changes at home. In 2012, she presented to our institution’s urology group with inability to remove her pessary over the two years prior; she had been twisting it intermittently to prevent the pessary from becoming embedded. At that time, the urologist was unable to remove the pessary in office due to tissue encapsulation. On exam there was no erythema or undue tenderness, however a small amount of malodorous discharge was appreciated. The urologist recommended she follow up with her gynecologist who routinely works with pessaries, and the urologist emphasized that she not delay this appointment, as the patient had already procrastinated addressing this retained pessary. The patient was agreeable. Patient was lost to follow up so it is unclear in our records whether this was addressed at that time. The patient’s son was under the impression that this pessary had been replaced in 2015. Over the next 6 years, the patient developed dementia and was cared for at an assisted living facility. In March 2020, her primary care doctor noted vaginal bleeding. The patient at this time was not interested in further workup, so the PCP agreed to refer to gynecology for pelvic exam and vaginal ultrasound if the bleeding increased. The patient continued with low volume intermittent vaginal bleeding for which she declined additional workup for. Additionally, in August 2020, the patient began having recurrent UTIs. Over the next year, she would present with 6 total culture proven urinary tract infections that was associated with worsened urinary incontinence. She was not on any prophylaxis for these recurrent infections.
In August 2021, the patient was admitted for presumed urosepsis with 5 days of ampicillin and ceftriaxone, though her final cultures had normal flora on growth. 5 days after discharge, the patient presented to urgent care with continued urgency, frequency, and dysuria. Here, she was given a one time dose of cefepime and discharged with a 7 day course of Bactrim. The next day, she presented to our institution’s emergency department with altered mental status and septic shock with systolic pressures in the 70s. CT was obtained and was read as concern for pessary erosion into the uterine cavity with uterine wall inflammatory changes. Urogynecology team was consulted and their exam was consistent with a migrated gelhorn pessary that had mucosa overlaying the distal most aspect. In consultation with urogynecology and the reconstructive urology team a CT cystogram was ordered. The CT cysto-gram demonstrated the entire pessary within the urinary bladder lumen, with its distal tip protruding into the vagina with evidence of a vesicovaginal fistula (Figure 1). The patient was taken to the OR for a cystotomy, pessary extraction (Figure 2), and bladder repair. A foley catheter was placed with plans to manage the vesicovaginal fistula on an elective basis. The patient recovered from her surgery well.
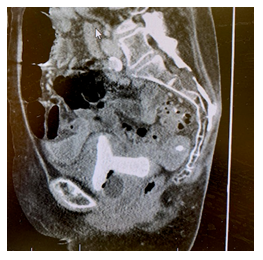
Figure 1: CT cystogram.

Figure 2: Pessary removal.
3. Discussion
This case demonstrates the frequent mismanagement of recurrent urinary tract infections in the elderly. AUA guidelines state that one of the first steps to management of recurrent urinary tract infections in women includes a pelvic exam to uncover any anatomic abnormalities leading to infection [7]. Vaginal estrogen should be offered for prophylaxis in peri/post-menopausal women and can be used in conjunction with low dose continuous antibiotics, as it prevents recurrent UTIs in post menopausal women [8]. After six symptomatic culture proven urinary tract infections over one year, our patient was not further evaluated with upper tract imaging and cystoscopy. Given the higher morbidity of urinary tract infections in the elderly, including estrogen in the prophylaxis regimen should be implemented in similar patient populations.
This case further highlights the importance of pessary follow up and demonstrates the need for a reliable tracking method of pessary patients. Physicians agree that a relative contraindication for pessary use is when follow up cannot be assured [2]. While a patient may be able to demonstrate autonomy with pessary changes when first placed, follow up is essential in the aging patient as their ability to self-manage may change as they age. The American College of Gynecology state that self care is not appropriate for pessary use for patients with dementia [9], though there is no specific recommendations for patients using pessaries prior to dementia onset. A pessary database may prevent episodes of the “forgotten pessary.” In their report, Riberio and colleagues suggest the use of electronic department registries to ensure these patients are not lost to follow up [1]. Similar quality initiatives are used for ureteral stents in many institutions, including ours. These systems provide notifications using automatic recall applications by querying the registry to alert providers of a possibly retained stent [10]. Other authors further suggest the use of a med-alert bracelet for cognitively impaired women as a reminder to care providers that a pessary is in place [11]. Given the morbidity and high healthcare cost associated with retained pessaries, we suggest that these pessary registries be implemented in healthcare institutions.
4. Conclusion
Our patient’s presentation highlights the simple yet important fundamentals of managing elderly women with recurrent urinary tract infections, including pel-vic exam and vaginal estrogen prophylaxis. Further, while pessaries are a reliable conservative method for managing pelvic organ prolapse in some elderly women, a tracking method is needed to prevent pessary retention. Given its success with ureteral stent tracking, we support the use of electronic department registries for ensuring pessary follow up.
Conflict of Interest
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Ribeiro J, Leite C. A curious cause of pseudo-haematuria: a neglected vaginal pessary. BMJ Case Rep (2017).
- Atnip SD. Pessary use and management for pelvic organ prolapse. Obstetrics & Gynecology Clinics of North America 36 (2009): 541-563.
- Abdulaziz M, Stothers L, Lazare D, et al. An integrative review and severity classification of complications related to pessary use in the treatment of female pelvic organ prolapse. Canadian Journal of Urology 9 (2015): E400-E406.
- Gordon G, Dolnicekb T, Malviyac V. A Problematic Peril of Pessaries: The Rare Case of Rectovaginal Fistulas Resulting From Pessary Use. J Clin Gynecol Obstet 4 (2015): 193-196.
- Arias BE, Ridgeway B, Barber MD. Complications of neglected vaginal pessaries: Case presentation and literature review. International Urogynecology Journal 19 (2008): 1173- 1178.
- Kaaki B, Mahajan ST. Vesico - vaginal fistula resulting from a wellcared-for pessary. International Uro - gynecology Journal 18 (2007): 971-973.
- Anger J Lee U, Ackerman L, Chou R, et al. Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. Journal of Urology 202 (2019): 282-289.
- Ferrante KL, Wasenda EJ, Jung CE, et al. Vaginal Estrogen for the Prevention of Recurrent Urinary Tract Infection in Postmenopausal Women: A Randomized Clinical Trial. Female Pelvic Med Reconstr Surg 27 (2021): 112-117.
- ACOG Practice Bulletin: clinical management guidelines for obstetrician-gynecologists, Number 85. Obstetricians and Gynecologists 110 (2007): 717-729.
- Lynch MF, Ghani KR, Frost I, et al. Preventing the forgotten ureteral stent: implementation of a web-based stent registry with automatic recall application. Urology 70 (2007): 423-426.
- O’Dell K, Atnip S. Pessary care: Follow up and management of complications. Urologic Nursing 32 (2012): 126-137.
- Bugge C, Dembinksy M, Kearney R, et al. Does self-management of vaginal pessaries improve care for women with pelvic organ prolapse?. BMJ 372 (2021).
- Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: Discontinuation rates and adverse events. British Journal of Obstetrics and Gynecology 116 (2009): 1715-1721.
