Relationship between Maternal Vitamin-D deficiency and serum Calcium level with Primary Caesarean Section and Postpartum Hemorrhage
Article Information
Dr. Mortuza Begum1*, Dr.Srabani Barua2, Dr. Anowara Begum3, Dr. Fahmida Islam Chowdhury4, Dr. Most. Zeenat Rehena5, Dr Rozina Ahmed6, Dr. Adnan Bacha7
1Consultant, Department of Obstetrics and Gynaecology, Chittagong Medical College Hospital, Chittagong, Bangladesh
2Junior Consultant, Department of Obstetrics and Gynaecology, Chittagong Medical College Hospital, Chittagong, Bangladesh
3Senior consultant, Department of Obstetrics and Gynaecology, Chittagong Medical College Hospital, Chittagong, Bangladesh
4Associate professor, Department of Obstetrics and Gynaecology, Chittagong Medical College Hospital, Chittagong, Bangladesh
5Assistant professor, Department of Obstetrics and Gynaecology, Chittagong Medical College Hospital, Chittagong, Bangladesh
6Assistant professor, Department of Obstetrics and Gynaecology, Chittagong Medical College Hospital, Chittagong, Bangladesh
7Assistant Professor, Department of Surgery, Southern Medical College Hospital, Chittagong, Bangladesh
*Corresponding Author: Dr. Mortuza Begum, Consultant, Department of Obstetrics and Gynaecology, Chittagong Medical College Hospital, Chittagong, Bangladesh.
Received: 02 March 2024; Accepted: 11 March 2024; Published: 14 March 2024
Citation: Dr. Mortuza Begum, Dr.Srabani Barua, Dr. Anowara Begum, Dr. Fahmida Islam Chowdhury, Dr. Most. Zeenat Rehena, Dr Rozina Ahmed, Dr. Adnan Bacha. Relationship between Maternal Vitamin-D deficiency and serum Calcium level with Primary Caesarean Section and Postpartum Hemorrhage. Obstetrics and Gynecology Research 7 (2024): 16-23.
Share at FacebookAbstract
Introduction:
Maternal nutrition, particularly Vitamin-D and calcium levels, plays a crucial role in pregnancy outcomes. This study aimed to investigate the relationship between maternal Vitamin-D deficiency and serum calcium levels with primary Cesarean section (C-section) and postpartum hemorrhage (PPH).
Methods:
In this cross-sectional observational study, 110 pregnant women from Chattogram Medical College Hospital and other private hospitals in Chattogram were assessed from January 2022 to December 2023. Data were collected on demographics, obstetric history, and maternal health, focusing on Vitamin-D and calcium supplementation, delivery methods, and neonatal outcomes.
Result:
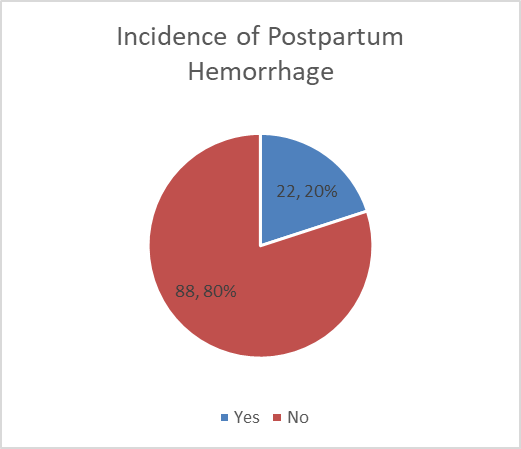
The participant group, predominantly aged 20-29 (61.82%) and housewives (57.27%), showed diverse educational backgrounds with 31.82% being illiterate. Nearly half were nulliparous (46.36%), with most pregnancies planned (69.09%). Overweight was prevalent (42.73%), and irregular calcium supplementation (74.55%) was common, while only 14.55% regularly took Vitamin D supplements. Vaginal deliveries were predominant (69.09%), with 20.00% experiencing PPH. Neonatal asphyxia was the most common complication (22.73%). A significant Vitamin D deficiency (65.45%) was observed, correlating positively with PPH (r = .322, p = 0.002) and negatively with neonatal complications (r = -.233, p = 0.026).
Conclusion:
The study underscores the significant role of maternal Vitamin-D levels in the incidence of PPH and highlights the need for focused nutritional counseling and supplementation in prenatal care to improve maternal and neonatal health outcomes.
Keywords
Maternal Nutrition; Vitamin-D Deficiency; Serum Calcium; Cesarean Section; Postpartum Hemorrhage
Maternal Nutrition articles; Vitamin-D Deficiency articles; Serum Calcium articles; Cesarean Section articles; Postpartum Hemorrhage articles
Article Details
Introduction
Maternal health during pregnancy is a critical determinant of both maternal and neonatal outcomes. The period of gestation is not only a phase of physical change but also a time when nutritional needs are heightened, directly impacting the health and well-being of the mother and the developing fetus [1]. Among the various nutrients essential during pregnancy, Vitamin-D and calcium stand out due to their significant roles in maternal and fetal health. The importance of maternal nutrition, particularly Vitamin-D and calcium, in the context of pregnancy outcomes, cannot be overstated. Vitamin-D plays a crucial role in the immune function and bone metabolism of both the mother and fetus, while calcium is vital for fetal skeletal development and maternal bone preservation [2]. The deficiency of these nutrients during pregnancy has been linked to various adverse outcomes, including preeclampsia, gestational diabetes, and fetal growth restriction [3]. Globally, the prevalence of Vitamin-D deficiency and hypocalcemia in pregnant women is alarmingly high. Studies have shown that Vitamin-D deficiency affects a significant portion of pregnant women worldwide, with varying prevalence rates depending on geographical location, lifestyle, and dietary habits [4]. This deficiency is not only a concern for maternal bone health but also has implications for fetal development. The physiological roles of Vitamin-D and calcium in pregnancy are multifaceted. Vitamin-D is essential for the regulation of calcium and phosphate metabolism, which is crucial for maintaining maternal and fetal bone health and cellular processes [5]. Calcium plays a pivotal role in muscular, nervous, and circulatory systems, and its deficiency can lead to serious health issues for both the mother and the fetus [6]. Deficiencies in Vitamin-D and calcium during pregnancy have been associated with several complications. Vitamin-D deficiency has been linked to an increased risk of Cesarean section due to dystocia and may affect the myometrium, potentially impacting labor and delivery outcomes [7]. Similarly, altered calcium levels can lead to various medical disorders in pregnancy and poor neonatal outcomes [8]. Primary Cesarean section and postpartum hemorrhage are significant complications in obstetrics, often leading to increased maternal morbidity and mortality. Recent research suggests a correlation between Vitamin-D deficiency, altered calcium levels, and increased risks of these complications [9]. For instance, a study found a significant association between low maternal vitamin D levels and increased rates of primary Cesarean section and uterine atony, leading to postpartum hemorrhage [10]. However, another study reported that vitamin D status at the time of delivery was not a predictor of postpartum hemorrhage overall or atonic postpartum hemorrhage, indicating variability in findings and the need for further research [11]. Despite the growing body of evidence, there are gaps in current research, particularly in studies directly correlating Vitamin-D and calcium levels with the specific outcomes of primary Cesarean section and postpartum hemorrhage. Most existing studies are observational and do not establish a clear causal relationship. This highlights the need for more comprehensive observational studies to better understand this relationship and its implications for clinical practice. The potential implications of understanding the relationship between maternal Vitamin-D and calcium levels and obstetric complications are vast. Improved knowledge in this area could lead to better prenatal care strategies, potentially reducing the incidence of primary Cesarean sections and postpartum hemorrhage. This, in turn, could contribute to improved maternal and fetal outcomes, highlighting the importance of nutritional assessment and intervention in prenatal care [12].
Methods
This cross-sectional observational study was conducted at Chattogram Medical College Hospital and other private hospitals in Chattogram from January 2022 to December 2023. The study enrolled 110 currently pregnant women who provided informed consent. Inclusion criteria were limited to pregnant women between 32-40 gestational weeks, while exclusion criteria encompassed those with planned or ongoing abortions, pregnancy of <32 gestational weeks and mothers with chronic diseases that could influence study outcomes. Data were collected using a structured sheet, capturing demographic details, obstetric history, lifestyle factors, supplementation of calcium and Vitamin D, delivery details, and neonatal outcomes. Key clinical measurements included serum Vitamin-D and calcium levels. The primary focus was to examine the association between maternal Vitamin-D deficiency and serum calcium levels with the incidence of delivery method and postpartum hemorrhage (PPH). The study also focused on maternal and neonatal outcome and complications. Statistical analysis was planned to include descriptive and inferential statistics to assess the relationships between the variables. Ethical approval for the study was obtained from the institutional review boards of the involved hospitals.
Results
|
Variables |
Frequency |
Percentage |
|
Age |
||
|
<20 |
23 |
20.91% |
|
20-29 |
68 |
61.82% |
|
30-39 |
19 |
17.27% |
|
Occupation |
||
|
Housewife |
63 |
57.27% |
|
Service Worker |
33 |
30.00% |
|
Student |
15 |
13.64% |
|
Education Level |
||
|
Illiterate |
35 |
31.82% |
|
Primary |
27 |
24.55% |
|
SSC |
27 |
24.55% |
|
HSC |
13 |
11.82% |
|
Graduate |
8 |
7.27% |
|
Socioeconomic Status |
||
|
Lower class |
16 |
14.55% |
|
Lower Middle Class |
44 |
40.00% |
|
Upper Middle Class |
35 |
31.82% |
|
Upper Class |
16 |
14.55% |
|
Residence |
||
|
Rural |
65 |
59.09% |
|
Urban |
41 |
37.27% |
|
Semi-Urban |
4 |
3.64% |
Table 1: Distribution of baseline demographic and socioeconomic characteristics of the participants (N=110)
In the study involving 110 participants, the distribution of baseline demographic and socioeconomic characteristics revealed a diverse group. The majority of participants were in the age group of 20-29 years, accounting for 61.82%, followed by those under 20 years (20.91%), and 30-39 years (17.27%). Regarding occupation, over half of the participants were housewives (57.27%), with service workers comprising 30.00%, and students making up 13.64%. The educational levels varied: 31.82% were illiterate, 24.55% had primary education, another 24.55% completed secondary school (SSC), 11.82% had higher secondary education (HSC), and 7.27% were graduates. In terms of socioeconomic status, the largest group was the lower middle class (40.00%), followed closely by the upper middle class (31.82%). The lower and upper classes each represented 14.55% of the participants. The majority of participants resided in rural areas (59.09%), with urban residents making up 37.27%, and a small fraction from semi-urban areas (3.64%).
|
Variables |
Frequency |
Percentage |
|
Parity |
||
|
Nulliparity |
51 |
46.36% |
|
Primipara |
33 |
30.00% |
|
2-3 parity |
25 |
22.73% |
|
>3 parity |
5 |
4.55% |
|
Gravida |
||
|
Primi gravida |
45 |
40.91% |
|
2nd Gravida |
29 |
26.36% |
|
3rd Gravida |
25 |
22.73% |
|
4th Gravida |
10 |
9.09% |
|
5th Gravida |
1 |
0.91% |
|
Planning of Pregnancy |
||
|
Planned |
76 |
69.09% |
|
Unplanned |
34 |
30.91% |
|
Antenatal Checkup |
||
|
Regular |
63 |
57.27% |
|
Irregular |
46 |
41.82% |
|
No Antenatal Care |
1 |
0.91% |
|
Adverse Obstetric History |
||
|
Yes |
40 |
36.36% |
|
No |
70 |
63.64% |
Table 2: Distribution of participants by obstetric history and characteristics (N=110)
The obstetric history and characteristics of the 110 participants in the study showed a diverse range of experiences. In terms of parity, nearly half of the participants were nulliparous (46.36%), followed by primiparas (30.00%), those with 2-3 children (22.73%), and a smaller group with more than three children (4.55%). Regarding gravidity, primi gravidas constituted the largest group (40.91%), followed by those in their second pregnancy (26.36%), third pregnancy (22.73%), fourth pregnancy (9.09%), and a minimal percentage in their fifth pregnancy (0.91%). When it came to pregnancy planning, a majority of the pregnancies were planned (69.09%), while 30.91% were unplanned. Regular antenatal checkups were reported by 57.27% of the participants, 41.82% had irregular checkups, and a very small fraction (0.91%) did not receive any antenatal care. Additionally, 36.36% of the participants had an adverse obstetric history, whereas 63.64% did not report any such history.
|
Variables |
Frequency |
Percentage |
|
BMI |
||
|
Healthy Weight |
35 |
31.82% |
|
Overweight |
47 |
42.73% |
|
Obese |
27 |
24.55% |
|
Morbidly Obese |
1 |
0.91% |
|
Smoker |
||
|
Yes |
7 |
6.36% |
|
No |
103 |
93.64% |
|
Calcium Supplement During Antenatal Period |
||
|
Regular |
28 |
25.45% |
|
Irregular |
82 |
74.55% |
|
No |
0 |
0.00% |
|
Vitamin D Supplement During Antenatal Period |
||
|
Regular |
16 |
14.55% |
|
Irregular |
58 |
52.73% |
|
No |
36 |
32.73% |
Table 3: Distribution of participants by maternal health and lifestyle factor (N=110)
In the study comprising 110 participants, the distribution of maternal health and lifestyle factors presented a varied picture. Body Mass Index (BMI) categories showed that the largest group was overweight (42.73%), followed by those with a healthy weight (31.82%), obese (24.55%), and a very small percentage falling into the morbidly obese category (0.91%). Regarding smoking habits, only a minority of the participants were smokers (6.36%), while a significant majority (93.64%) did not smoke. When it came to calcium supplementation during the antenatal period, a quarter of the participants (25.45%) reported regular supplementation, but a notable majority (74.55%) had irregular supplementation habits, and none of the participants reported abstaining from calcium supplements entirely. Vitamin D supplementation showed that only 14.55% of the participants took it regularly during their antenatal period, more than half (52.73%) had irregular supplementation, and a substantial proportion (32.73%) did not take Vitamin D supplements at all.
|
Variables |
Frequency |
Percentage |
|
Time of Delivery |
||
|
At 37-38 weeks |
33 |
30.00% |
|
at 39-40 weeks |
51 |
46.36% |
|
40-42 weeks |
27 |
24.55% |
|
Mode of Delivery |
||
|
Vaginal |
76 |
69.09% |
|
Cesarean Section |
34 |
30.91% |
|
Delivery Complications |
||
|
No |
62 |
56.36% |
|
Prolonged Labor |
36 |
32.73% |
|
Obstructed labor |
10 |
9.09% |
|
Preterm Labor |
2 |
1.82% |
Table 4: Distribution of participants by delivery details and complications (N=110)
In the study of 110 participants, the distribution of delivery details and complications revealed diverse childbirth experiences. The timing of delivery varied, with 46.36% of participants delivering at 39-40 weeks, 30.00% at 37-38 weeks, and 24.55% delivering between 40-42 weeks. Regarding the mode of delivery, a majority of the participants (69.09%) had vaginal deliveries, while 30.91% underwent Cesarean sections. Delivery complications were reported in a significant portion of the cases. The majority of participants (56.36%) experienced no complications during delivery. However, 32.73% faced prolonged labor, 9.09% had obstructed labor, and a small percentage (1.82%) experienced preterm labor.
In the study involving 110 participants, the incidence of Postpartum Hemorrhage (PPH) was a significant aspect of the findings. The data revealed that 20.00% of the participants experienced PPH, while a substantial majority, 80.00%, did not encounter this complication.
|
Variables |
Frequency |
Percentage |
|
Complications |
||
|
No Complications |
70 |
63.64% |
|
Neonatal Asphyxia |
25 |
22.73% |
|
Congenital anomaly |
2 |
1.82% |
|
Very low birth weight |
7 |
6.36% |
|
Stillbirth |
4 |
3.64% |
|
Neonatal jaundice |
1 |
0.91% |
|
Fetal Weight |
||
|
< 2.5kg |
27 |
24.55% |
|
≥ 2.5-3.5kg |
75 |
68.18% |
|
> 3.5kg |
8 |
7.27% |
Table 5: Distribution of participants by neonatal outcome (N=110)
In the study with 110 participants, the distribution of neonatal outcomes highlighted various aspects of newborn health. The majority of the newborns (63.64%) did not experience any complications. However, neonatal asphyxia was observed in 22.73% of the cases, making it the most common complication among the participants' newborns. Other complications included very low birth weight (6.36%), stillbirth (3.64%), congenital anomalies (1.82%), and neonatal jaundice (0.91%). Regarding fetal weight, a significant majority of the newborns (68.18%) had a birth weight in the range of ≥ 2.5-3.5kg. Those with a birth weight of less than 2.5kg accounted for 24.55% of the cases, and 7.27% of the newborns had a birth weight greater than 3.5kg.
|
Variables |
Frequency |
Percentage |
|
Serum Vitamin D |
||
|
Deficient |
72 |
65.45% |
|
Normal |
38 |
34.55% |
|
Serum Calcium |
||
|
Below Normal |
13 |
11.82% |
|
Normal |
97 |
88.18% |
Table 6: Distribution of participants by serum vitamin D and Calcium levels (N=110)
In the study of 110 participants, the distribution of serum Vitamin D and Calcium levels revealed notable findings. A significant proportion of the participants, 65.45%, were found to have deficient levels of serum Vitamin D, while 34.55% had normal levels. This indicates a high prevalence of Vitamin D deficiency among the study population. In contrast, the serum Calcium levels presented a different picture. The majority of participants, 88.18%, had normal serum Calcium levels, while only a smaller group, 11.82%, exhibited below-normal levels.
Table 7: Bivariate Correlation
In the study involving 110 participants, the bivariate correlation analysis revealed several significant relationships. Serum Vitamin D levels were positively correlated with serum Calcium levels (r = .335, p = 0.001) and the incidence of postpartum hemorrhage (r = .322, p = 0.002), but negatively correlated with neonatal complications (r = -.233, p = 0.026). Serum Calcium levels showed a positive correlation with the need for NICU (r = .234, p = 0.026) and a negative correlation with neonatal complications (r = -.334, p = 0.001). Postpartum hemorrhage was negatively correlated with the mode of delivery (r = -.326, p = 0.002) and delivery complications (r = -.361, p < 0.001). The need for NICU was negatively correlated with delivery complications (r = -.235, p = 0.025) and neonatal complications (r = -.386, p < 0.001). Fetal weight showed a significant negative correlation with neonatal complications (r = -.284, p = 0.006). Additionally, the mode of delivery was positively correlated with delivery complications (r = .416, p < 0.001).
Discussion
The demographic and socioeconomic characteristics of our study population, predominantly comprising women in the age group of 20-29 years (61.82%) and primarily housewives (57.27%), reflect a diverse group. This diversity is crucial as it mirrors the general population, providing a comprehensive perspective on maternal health. The high percentage of illiteracy (31.82%) among participants is noteworthy and aligns with findings from other regions, indicating a potential link between educational status and maternal health outcomes [13,14]. Our study revealed that nearly half of the participants were nulliparous (46.36%), with a majority of the pregnancies being planned (69.09%). Regular antenatal checkups, reported by 57.27% of our participants, are essential for monitoring pregnancy progress and identifying potential complications [15]. The fact that a large group of participants was overweight (42.73%) is concerning, as maternal obesity is known to be associated with adverse pregnancy outcomes [16]. The irregular calcium supplementation habits (74.55%) and low regular intake of Vitamin D supplements (14.55%) observed in our study are alarming, considering the crucial role of these nutrients in pregnancy [17,18]. In terms of delivery details, our finding that 46.36% of participants delivered at 39-40 weeks, with a majority having vaginal deliveries (69.09%), is in line with standard obstetric practice. However, the high incidence of delivery complications (43.64%), particularly prolonged labor (32.73%), and the observed incidence of PPH (20.00%), are significant. These findings are higher than some reported rates and suggest the need for enhanced monitoring and intervention strategies during labor [19]. Neonatal outcomes in our study were generally positive, with 63.64% of newborns not experiencing any complications. However, the occurrence of neonatal asphyxia in 22.73% of cases is a critical concern, as it is a leading cause of neonatal morbidity and mortality globally [20,21]. The majority of the newborns having a birth weight within the normal range (≥ 2.5-3.5kg) is reassuring and indicative of adequate maternal and fetal health during pregnancy. In our study, the correlation analysis revealed significant insights into maternal and neonatal health. Serum Vitamin D levels showed a positive correlation with both serum Calcium levels (r = .335, p = 0.001) and the incidence of postpartum hemorrhage (PPH) (r = .322, p = 0.002), suggesting a crucial role of Vitamin D in pregnancy outcomes. Interestingly, these levels were negatively correlated with neonatal complications (r = -.233, p = 0.026), indicating a complex interplay between maternal Vitamin D status and neonatal health. Similarly, serum Calcium levels were positively correlated with the need for NICU (r = .234, p = 0.026), highlighting the importance of calcium in neonatal well-being. However, a negative correlation with neonatal complications (r = -.334, p = 0.001) was observed, aligning with findings from other studies that emphasize the protective role of adequate calcium levels [22,23]. The mode of delivery was intricately linked with both PPH and delivery complications, as indicated by the negative correlations (r = -.326, p = 0.002 and r = -.361, p < 0.001, respectively). This aligns with research suggesting that certain delivery methods may influence the risk of complications [24,25]. Furthermore, the need for NICU care showed a negative correlation with delivery complications (r = -.235, p = 0.025), reinforcing the notion that more complex deliveries might lead to increased neonatal care requirements.
Limitations of the Study
The study was conducted in one of the public medical college and a few private hospitals of Chittagong, encompassing a small sample size. So, the results may not represent the whole community.
Conclusion
In conclusion, our study provides valuable insights into the complex interplay between maternal health, particularly Vitamin D and Calcium levels, and their impact on pregnancy and neonatal outcomes. The demographic and socioeconomic characteristics of our participants, predominantly young women and housewives with varied educational backgrounds, reflect the diverse nature of the population studied. The high prevalence of Vitamin D deficiency among these women and its significant correlation with the incidence of postpartum hemorrhage highlight the critical role of adequate Vitamin D levels in maternal health. Additionally, the positive correlation of serum Calcium levels with neonatal health underscores the importance of this nutrient in the early stages of life. Our findings also draw attention to the high rates of delivery complications and the notable incidence of neonatal asphyxia, emphasizing the need for enhanced prenatal care and nutritional management. The correlations observed between maternal nutrient levels, delivery methods, and neonatal outcomes suggest that comprehensive and targeted interventions are essential to improve maternal and neonatal health outcomes.
Funding:
No funding sources
Conflict of interest:
None declared
Ethical approval:
The study was approved by the Institutional Ethics Committee
References
- Vestergaard AL, Christensen M, Andreasen MF, et al. Vitamin D in pregnancy (GRAVITD) – a randomised controlled trial identifying associations and mechanisms linking maternal Vitamin D deficiency to placental dysfunction and adverse pregnancy outcomes – study protocol. BMC Pregnancy Childbirth 15 (2023): 177.
- Boychuk AV, Budnik TO. Vitamin D status in pregnant women and its effect on pregnancy and maternal outcomes. INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine) 18 (2022): 324-330.
- van der Pligt PF, Ellery SJ, de Guingand DL, et al. Maternal plasma vitamin D levels across pregnancy are not associated with neonatal birthweight: findings from an Australian cohort study of low-risk pregnant women. BMC Pregnancy Childbirth 23 (2023): 67.
- Aggarwal N, Singla R, Dutta U, et al. Prevalence of Vitamin D deficiency among pregnant women and effect of Vitamin D supplementation on maternal and fetal outcomes: A double-blind randomized placebo controlled trial. Asian Journal of Medical Sciences 13 (2022): 95-101.
- Fiscaletti M, Stewart P, Munns C. The importance of vitamin D in maternal and child health: a global perspective. Public Health Reviews 38 (2017): 19.
- Dipti Anand MM Dipti Anandand Gurjit Kaur, Gurjit Kaurand Alka Sehgal, Alka Sehgaland Shikha Rani, et al. Role of vitamin D and calcium supplementation in pregnancy alone or in combination. 4 (2015): 1341-1343.
- Aspray TJ. Vitamin D in Musculoskeletal Health and Beyond. Calcif Tissue Int 106 (2020): 1-2.
- Caballero B. Encyclopedia of human nutrition. Elsevier (2005).
- Sörsjö Stevenazzi A, Pihl S, Blomberg M, et al. The association between maternal vitamin D deficiency and postpartum hemorrhage and uterine atony. Acta Obstet Gynecol Scand 103 (2023): 286-293.
- Hubeish M, Husari HA, Itani SE, et al. Maternal Vitamin D Level and Rate of Primary Cesarean Section. Journal of Clinical Gynecology and Obstetrics 7 (2018): 43-51.
- Ullah MI, Uwaifo GI, Koch CA. Primary Hyperparathyroidism and Hypercalcemia During Pregnancy. Horm Metab Res 49 (2017): 638-641.
- Mahmood S, Pervin HH, Yousuf S. Association of serum vitamin D levels with gestational diabetes mellitus. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 10 (2021): 2198-2203.
- Gazmararian JA, Adams MM, Pamuk ER. Associations Between Measures of Socioeconomic Status and Maternal Health Behavior. American Journal of Preventive Medicine 12 (1996): 108-115.
- Mensch BS, Chuang EK, Melnikas AJ, et al. Evidence for causal links between education and maternal and child health: systematic review. Trop Med Int Health 24 (2019): 504-522.
- ANTENATAL CARE. In: Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice 3rd edition [Internet]. World Health Organization; 2015 [cited 2024 Feb 18].
- Leddy MA, Power ML, Schulkin J. The Impact of Maternal Obesity on Maternal and Fetal Health. Rev Obstet Gynecol 1 (2008): 170-178.
- Thomas M, Weisman SM. Calcium supplementation during pregnancy and lactation: Effects on the mother and the fetus. American Journal of Obstetrics and Gynecology 194 (2006): 937-945.
- Curtis EM, Moon RJ, Harvey NC, et al. Maternal vitamin D supplementation during pregnancy. British Medical Bulletin 126 (2018): 57-77.
- Thompson JMD, Irgens LM, Rasmussen S, et al. Secular trends in socio-economic status and the implications for preterm birth. Paediatric and Perinatal Epidemiology 20 (2006): 182-187.
- Lee AC, Mullany LC, Tielsch JM, et al. Risk Factors for Neonatal Mortality due to Birth Asphyxia in Southern Nepal. Pediatrics 121 (2008): e1381–1390.
- Kawakami MD, Sanudo A, Teixeira MLP, et al. Neonatal mortality associated with perinatal asphyxia: a population-based study in a middle-income country. BMC Pregnancy and Childbirth 21 (2021): 169.
- Vuralli D. Clinical Approach to Hypocalcemia in Newborn Period and Infancy: Who Should Be Treated? Int J Pediatr 19 (2019): 4318075.
- Imdad A, Jabeen A, Bhutta ZA. Role of calcium supplementation during pregnancy in reducing risk of developing gestational hypertensive disorders: a meta-analysis of studies from developing countries. BMC Public Health 11 (2011): S18.
- Chawanpaiboon S, Titapant V, Pooliam J. Maternal complications and risk factors associated with assisted vaginal delivery. BMC Pregnancy and Childbirth 23 (2023): 756.
- Gregory KD, Jackson S, Korst L, et al. Cesarean versus Vaginal Delivery: Whose Risks? Whose Benefits? Am J Perinatol 29 (2012): 7-18.