Recurrent Pyogenic Granuloma caused by Intraosseous Vessel: A Case Report
Article Information
Halenur Var, Efe Can Sivrikaya*
Department of Oral Maxillofacial Surgery, Faculty of Dentistry, Karadeniz Technical University, Trabzon, Turkey
*Corresponding Author: Efe Can Sivrikaya, Department of Oral Maxillofacial Surgery, Faculty of Dentistry, Karadeniz Technical University, Ktu loj 33/8 Ortahisar, Trabzon, Turkey
Received: 20 August 2020; Accepted: 29 August 2020; Published: 03 November 2020
Citation: Halenur Var, Efe Can Sivrikaya. Recurrent Pyogenic Granuloma caused by Intraosseous Vessel: A Case Report. Dental Research and Oral Health 3 (2020): 202-206.
Share at FacebookAbstract
Pyogenic granuloma is a benign localized lesion of the skin and mucosa closely related to trauma, chronic irritation and hormonal changes. The method of treatment is surgical excision. However relapses can occur. For this reason, treatment with alternative methods such as cryotherapy, electrocautery and laser has been investigated in recent years. In this case, the cause of PG was a feeder vessel. The lesion was excised before and recurred within two weeks. An intraosseous feeder vessel was identified by a magnetic resonance imaging. This vessel was exposed and cauterized with electrocautery.
Keywords
Electrocautery, Labial Pyogenic Granulo-ma, Vascular Malformation
Electrocautery article; Labial Pyogenic Granulo-ma article; Vascular Malformation article
Electrocautery articles Electrocautery Research articles Electrocautery review articles Electrocautery PubMed articles Electrocautery PubMed Central articles Electrocautery 2023 articles Electrocautery 2024 articles Electrocautery Scopus articles Electrocautery impact factor journals Electrocautery Scopus journals Electrocautery PubMed journals Electrocautery medical journals Electrocautery free journals Electrocautery best journals Electrocautery top journals Electrocautery free medical journals Electrocautery famous journals Electrocautery Google Scholar indexed journals Labial Pyogenic Granulo-ma articles Labial Pyogenic Granulo-ma Research articles Labial Pyogenic Granulo-ma review articles Labial Pyogenic Granulo-ma PubMed articles Labial Pyogenic Granulo-ma PubMed Central articles Labial Pyogenic Granulo-ma 2023 articles Labial Pyogenic Granulo-ma 2024 articles Labial Pyogenic Granulo-ma Scopus articles Labial Pyogenic Granulo-ma impact factor journals Labial Pyogenic Granulo-ma Scopus journals Labial Pyogenic Granulo-ma PubMed journals Labial Pyogenic Granulo-ma medical journals Labial Pyogenic Granulo-ma free journals Labial Pyogenic Granulo-ma best journals Labial Pyogenic Granulo-ma top journals Labial Pyogenic Granulo-ma free medical journals Labial Pyogenic Granulo-ma famous journals Labial Pyogenic Granulo-ma Google Scholar indexed journals Vascular Malformation articles Vascular Malformation Research articles Vascular Malformation review articles Vascular Malformation PubMed articles Vascular Malformation PubMed Central articles Vascular Malformation 2023 articles Vascular Malformation 2024 articles Vascular Malformation Scopus articles Vascular Malformation impact factor journals Vascular Malformation Scopus journals Vascular Malformation PubMed journals Vascular Malformation medical journals Vascular Malformation free journals Vascular Malformation best journals Vascular Malformation top journals Vascular Malformation free medical journals Vascular Malformation famous journals Vascular Malformation Google Scholar indexed journals angiogenesis articles angiogenesis Research articles angiogenesis review articles angiogenesis PubMed articles angiogenesis PubMed Central articles angiogenesis 2023 articles angiogenesis 2024 articles angiogenesis Scopus articles angiogenesis impact factor journals angiogenesis Scopus journals angiogenesis PubMed journals angiogenesis medical journals angiogenesis free journals angiogenesis best journals angiogenesis top journals angiogenesis free medical journals angiogenesis famous journals angiogenesis Google Scholar indexed journals vascular bleeding articles vascular bleeding Research articles vascular bleeding review articles vascular bleeding PubMed articles vascular bleeding PubMed Central articles vascular bleeding 2023 articles vascular bleeding 2024 articles vascular bleeding Scopus articles vascular bleeding impact factor journals vascular bleeding Scopus journals vascular bleeding PubMed journals vascular bleeding medical journals vascular bleeding free journals vascular bleeding best journals vascular bleeding top journals vascular bleeding free medical journals vascular bleeding famous journals vascular bleeding Google Scholar indexed journals
Article Details
1. Introduction
The pyogenic granuloma (PG) or pyogenic fibroma is a common vascular proliferation first described in 1844 by Hullihen [1-3]. It is described as active tumor that responds to various stimuli, such as local chronic low-grade local irritation [4], traumatic injury, hormonal factors [5] or certain kinds of drugs [6]. PG commonly occurs in gingiva [7]. It is rarely found in other locations such as the lips, tongue, buccal mucosa are the next most common sites [4, 8, 9]. PG can occurs in patients of all ages [10, 11] but predominant in the second decade of life in young adult females, possibly because of the vascular effects of female hormones [4, 8, 9]. PG can be classified in to two groups: capillary and non-capillary lobular hemangioma [12]. Clinically, PG is slow growing painless lesion [4, 9] but it may also grow rapidly [13]. Some factors such as inducible nitricoxide synthase [14], vascular endothelial growth factor [15], basic fibroblast growth factor [16] or connective tissue growth factor [17] are known to be involved in angiogenesis and rapid growth of PG. Treatment of PG is usually full surgical excision with sub-periosteal curettage. Lesions may recur up to16% after surgical excision [18]. To prevent recurrence potential irritant factors must be removed [18]. Excision with cryotherapy, laser or electrosurgery is performed to prevent vascular recurrence. This paper presents a case report of a recurrent PG caused by intraosseous vessel, which was treated with success after the identification of a feeder vessel by a magnetic resonance imaging, and its cauterization by electrocautery.
2. Case Report
A 25-year-old female patient was admitted to the Karadeniz Technical University Faculty of Dentistry Department of Oral and Maxillofacial Surgery with complaining about a volumetric increase in the papilla region between first and second molars of the upper left arch. The clinical appearance of the lesion was granulomatous, reddish, with a pedunculated base, measuring approximately 15x9x3 at buccal aspect (figure 1a). The patient stated that PG excision had been performed several times before but recurrence occurred within 2 weeks. Radiolucent area was determined between the right maxillary first and second molars on panormaic radiography in routine examination (figure 2). After, T2 TSE Magnetic resonance imaging was performed. In MR, the presence of three intraosseous vessels in the right maxillary posterior region was determined (figure 3).The patient was informed and consent. The lesion was removed by excisional biopsy (figure 1b). The fragments were individually sent for histopathological examination. The microscopic sections of the main lesion revealed capillary PG. The image revealed a large vessel in the interproximal bone between the upper right the first and second molar, associated with the lesion. This vessel may be feeder so a blood vessel was exposed and cauterized with electrocautery (figure 1c). After 4 months control follow up, no signs of recurrence were noted.
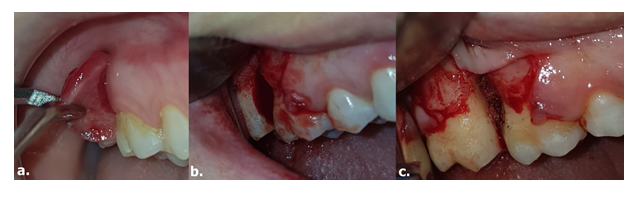
figure 1: a) The clinical appearance of lesion (15x9x3 mm); b) Hemorrhage after excision; c) The feeder vessel site after cauterization.

figure 2: Radiolucent area between the maxillary right first molar and the second molar in panoramic radiography.
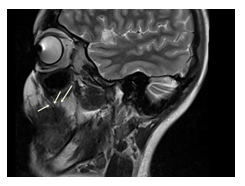
figure 3: It is observed by MR that the three intraosseous vessels are located in the right maxillary posterior region.
3. Discussion
Pyogenic granuloma is often seen vascular proliferation that generally presents as a solitary, sessile, or pedunculated lesion with a fragile surface prone to bleeding, ulceration, and crusting [19]. Treatment of PG is usually full surgical excision with sub-periosteal curettage. However, lesions may recur up to 16% after surgical excision [18, 20] and the relapse rates (3–8.2%) [21-23]. Recently, some other treatment protocols have been stated [18]. These are laser theraphy, cryotherapy and electrocautery treatment option which may need to be tried in cases with recurrence to prevent bleeding of the vascular structure [18]. To prevent recurrence of PG, vascular bleeding must be controlled. Hemostasis can be achieved using different methods such as mechanical, thermal/energy-based, chemical (pharmacological-based) methods. Conventional methods for control of bleeding include suturing, manual compression, or ligatures [24]. Both of electrosurgery and laser cauterization (LC) are thermal methods. ES has been defined as the intentional passage of high-frequency wave forms, or currents, through the tissues of the body to achieve a controllable surgical effect [25]. In addition ES and LC can create areas of char and necrosis of tissue, increasing the possibilities of infection, and damaging wound edge which can be lead to impaired healing [18, 26]. ND:YAG and Co2 lasers are often used because of their superior coagulation properties [18]. Tay et al [27] conducted flash lamp pumped pulsed dye laser and reported that as the number of sessions increased, relapse decreased. Other surgical treatment options of PG to prevent recurrence include cryosurgery in form of either liquid nitrogen spray or a cryoprobe [28, 29]. Ishida and Ramos-Silva [28] stated that cryosurgery would also prevent relapse of granulomas.
However, Ghodsi [29] described that one session of cryosurgery may not be enough. In present study, since cautery was used, one session was sufficient. In the present case, there is radiolucency between the first and second molars in the panoramic film and MRI. Abe et al [30] described that MRI to visualize pyogenic granuloma is successful method. Kusakere et al [31]. described that angiography was used because of the superior detection of feeder vessels. The patient refused to angiography imaging. After that, electrosurgical treatment was performed and only one session was sufficient. In the literature, electrosurgical use is few for pyogenic granulomas with high recurrence. As a result, one-session electrosurgery prevented recurrence in this case. In cases with frequent recurrence of pyogenic granuloma, firstly pathology and then ES can be recommended.
References
- Hullihen S. Case of Aneurism by Anastomosis of the Superior Maxillare. The American journal of dental science 4 (1844): 160.
- Plachouri KM, Georgiou S. Therapeutic approaches to pyogenic granuloma: an updated review. International journal of dermatology 58 (2019): 642-648.
- Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: Various concepts of etiopathogenesis. Journal of oral and maxillofacial pathology: JOMFP 16 (2012): 79.
- Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology: clinical pathologic considerations 4th ed (2003): 115-116.
- Mussalli N, Hopps RM, Johnson N. Oral pyogenic granuloma as a complication of pregnancy and the use of hormonal contraceptives. International Journal of Gynecology & Obstetrics 14 (1976): 187-191.
- Miller R, Ross J, Martin J. Multiple granulation tissue lesions occurring in isotretinoin treatment of acne vulgaris-successful response to topical corticosteroid therapy. Journal of the American Academy of Dermatology 12 (1985): 888-889.
- Sternberg SS, Antonioli DA, Carter D, et al. Diagnostic surgical pathology. Diagnostic surgical pathology 3 ed (1999): 69-174.
- Eversole LR. Clinical outline of oral pathology: diagnosis and treatment. 3rd ed (2002): 113-114.
- Neville BW, Damm DD, Allen CM, et al. Oral & maxillofacial pathology 2 ed (2002): 437-495.
- Lawoyin JO, Arotiba JT, Dosumu OO. Oral pyogenic granuloma: a review of 38 cases from Ibadan, Nigeria. The British journal of oral & maxillofacial surgery 35 (1997): 185-189.
- Al-Khateeb T, Ababneh K. Oral pyogenic granuloma in Jordanians: a retrospective analysis of 108 cases. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons 61 (2003): 1285-1288.
- Amirchaghmaghi M, Falaki F, Mohtasham N, et al. Extragingival pyogenic granuloma: a case report. Cases journal 1 (2008): 371.
- Parisi E, Glick PH, Glick M. Recurrent intraoral pyogenic granuloma with satellitosis treated with corticosteroids. Oral diseases 12 (2006): 70-72.
- Shimizu K, Naito S, Urata Y, et al. Inducible nitric oxide synthase is expressed in granuloma pyogenicum. The British journal of dermatology 138 (1998): 769-773.
- Bragado R, Bello E, Requena L, et al. Increased expression of vascular endothelial growth factor in pyogenic granulomas. Acta dermato-venereologica 79 (1999).
- Hagiwara K, Khaskhely NM, Uezato H, et al. Mast cell “densities” in vascular proliferations: a preliminary study of pyogenic granuloma, portwine stain, cavernous hemangioma, cherry angioma, Kaposi's sarcoma, and malignant hemangioendothelioma. The Journal of dermatology 26 (1999): 577-586.
- Igarashi A, Hayashi N, Nashiro K, et al. Differential expression of connective tissue growth factor gene in cutaneous fibrohistiocytic and vascular tumors. Journal of cutaneous pathology 25 (1998): 143-148.
- Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. Journal of oral science 48 (2006): 167-175.
- Warner J, Jones EW. Pyogenic granuloma recurring with multiple satellites. A report of 11 cases. Br J Dermatol 80 (1968): 218-227.
- Nthumba PM. Giant pyogenic granuloma of the thigh: a case report. Journal of medical case reports 2 (2008): 95.
- Gordon-Nunez MA, de Vasconcelos Carvalho M, Benevenuto TG, et al. Oral pyogenic granuloma: a retrospective analysis of 293 cases in a Brazilian population. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons 68 (2010): 2185-2188.
- Sachdeva SK. Extragingival Pyogenic Granuloma: an Unusual Clinical Presentation. Journal of dentistry 16 (2015): 282-285.
- Saravana GH. Oral pyogenic granuloma: a review of 137 cases. The British journal of oral & maxillofacial surgery 47 (2009): 318-319.
- Echave M, Oyaguez I, Casado MA. Use of Floseal(R), a human gelatine-thrombin matrix sealant, in surgery: a systematic review. BMC surgery 14 (2014): 111.
- Osman FS. Dental electrosurgery: general precautions. Journal 48 (1982): 641.
- Tan SR, Tope WD. Effectiveness of microporous polysaccharide hemospheres for achieving hemostasis in mohs micrographic surgery. Dermatologic surgery: official publication for American Society for Dermatologic Surgery [et al] 30 (2004): 908-914.
- Tay YK, Weston WL, Morelli JG. Treatment of pyogenic granuloma in children with the flashlamp-pumped pulsed dye laser. Pediatrics 99 (1997): 368-370.
- Ishida CE, Ramos-e-Silva M. Cryosurgery in oral lesions. International journal of dermatology 37 (1998): 283-285.
- Ghodsi SZ, Raziei M, Taheri A, et al. Comparison of cryotherapy and curettage for the treatment of pyogenic granuloma: a randomized trial. Br J Dermatol 154 (2006): 671-675.
- Abe M, Hoshi K, Shojima M, et al. A large pyogenic granuloma with extensive maxillary bone resorption penetrating the maxillary sinus: A rare case report. J Oral Max Surg Med 29 (2017): 254-257.
- Kusakabe A, Kato H, Hayashi K, et al. Pyogenic granuloma of the stomach successfully treated by endoscopic resection after transarterial embolization of the feeding artery. Journal of gastroenterology 40 (2005): 530-535.
