Reconstruction of the Lower Lip with A Buccal Fat Pad Free Graft– Report of A Case
Article Information
Fares Kablan1*, Daniel Oren1, Asaf Zigron1, Khaldoon Abu Saleh1, Idan Redenski1 and Samer Srouji1,2
1Department of Oral and Maxillofacial Surgery, Galilee College of Dental Sciences, Galilee Medical Center, Nahariya, Israel
2The Azrieli Faculty of Medicine, Bar-Ilan University, Safed, Israel
*Corresponding Author: Fares Kablan, Department of Oral and Maxillofacial Surgery, Galilee College of Dental Sciences, Galilee Medical Center, Nahariya, Israel
Received: 24 August 2023; Accepted: 13 September 2023; Published: 30 September 2023
Citation: Fares Kablan, Daniel Oren, Asaf Zigron, Khaldoon Abu Saleh, Idan Redenski and Samer Srouji. Reconstruction of the Lower Lip with A Buccal Fat Pad Free Graft– Report of A Case. Archives of Clinical and Medical Case Reports. 7 (2023): 366-369
Share at FacebookAbstract
The lips are a critical component that contributes both to esthetics and function. Partial or total resection of the lower lip following diagnosis of squamous cell carcinoma is frequently required. Reconstruction of lip tissues depends on the size and area of the defect. Multiple methods have been introduced for such cases, all with their challenges and downsides in restoring acceptable aesthetics and function. While defects covering roughly one-third of the lip surface can be treated by primary closure, more significant defects may require more complex methods. Recently the free buccal fat pad graft has been described as a volumizer graft, able to reconstruct different defects in the oral cavity. This report aims to describe a case diagnosed with SCC in which a wedge resection of about 50% of the lower lip was reconstructed with a free buccal fat pad graft. Lip tissue underwent primary closure and compensation of the lost lip volume was obtained. Thus, the buccal fat pad graft was shown to be an adequate tool for cases of lip tissue reconstruction.
Keywords
Free Buccal fat pad; Lip reconstruction
Article Details
Abbreviations:
BFP: Buccal Fat Pad; FFG: Free Fat Graft; PBFPF: Pedicle Buccal Fat Pad Flap; BFFG: Buccal Free Fat Graft
1. Introduction
The lips are crucial in phonetics, facial esthetics, and facial expression. Squamous cell carcinoma (SCC) is the most common malignancy affecting the lower lip. 90% of all lip SCCs involve the lower lip, which has been shown to be exposed to higher doses of UV radiation from sunlight than the upper lip [1]. However, labial defects resulting from tumor resection can severely impair patients’ quality of life [2]. Several reconstruction techniques have been reported in the literature with extensive lip defects necessitating complex methods to restore lip anatomy and volume [3-5].
The buccal fat pad (BFP), first described by Bichat, is considered a multipurpose graft for intraoral soft tissue defects. Reports emerged on using the BFP as a pedicled and free graft [6,7]. However, the Pedicle fat pad graft (PBFPF) use for lip reconstruction has yet to be documented. Herein, we report a case in which an SCC-affected lip was reconstructed using a free buccal fat pad graft(BFFG).
2. Case Report
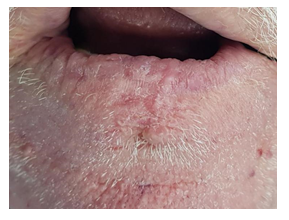
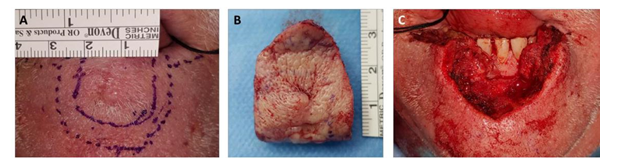
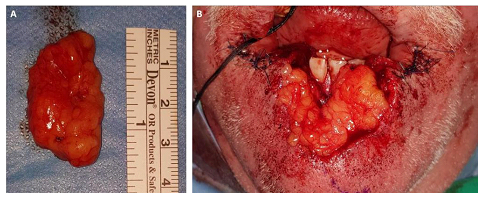
A 64 old male was admitted to the oral and maxillofacial surgery department. His medical history included diabetes mellitus and hypertension, with a history of heavy smoking. The patient admitted to our department with a painful indurated exophytic lesion over the dry vermilion, with skin involvement and leukoplakia (Figure 1). The patient underwent an incisional biopsy with no post-operative complications (Figure 2), and a moderate to poorly differentiated squamous cell carcinoma with invasion of skin tissue was diagnosed. Subsequent imaging ruled out lymph node involvement. The patient was informed of the diagnosis, the proposed surgical procedure, including harvesting of the BFFG and subsequent lip reconstruction, and possible complications associated with the process. Under general anesthesia with nasal intubation, after marking the tumor borders, a vermilionectomy and a wide V-shaped resection of the tumor with 1.0 cm margins were performed (Figure 3). Pathological examination (frozen sections) performed during the surgery verified that the surgical margins were tumor-free. Once the lesions was removed, the reconstruction included a mucosal advancement flap and undermining of the adjacent skin and mucosal edges, with bilateral dissection of the Orbicularis Oris muscle to allow re-approximation during wound closure. (Figure 3). A BFFG was harvested from the maxillary vestibule using blunt dissection and transferred as a free graft to add volume after the resection (Figure 4). The advancement flap was released and sutured to adjacent skin using resorbable sutures (Ethicon, NJ, USA) (Figure 4). The BFFG was adapted to the surgical bed, followed by re-approximation of residual lip margins (Figure 5).
Post-operatively, the patient was maintained on a soft diet. The patient had no complications during follow-ups at one, four, eight, and 24-weeks post-operatively. Both functional and aesthetic outcomes were satisfactory, with normal lip function and sensation, mouth opening of 45 mm, good color and texture, and excellent volume at the grafted site (Figure 6). The patient did not report any discomfort, and no subsequent surgeries were required 12 months after the initial surgery.
Figure 3: Resection of the tumor. According to histopathological diagnosis of SCC, a resection of the tumor was performed with 1.0 cm margins (A, B). Following the resection, undermining of the adjacent skin and mucosal edges was performed together with dissection of the orbicularis oris muscle (C).
3. Discussion
Reconstruction of lip defects resulting from tumor ablative surgery is challenging, especially when the defect is larger than one-third of the lip size [8]. Achievement of complete and adequate lip defects closure necessitates using tension-free margins and grafts with sufficient volume and thickness. Several surgical techniques employing local and regional grafts and flaps have been proposed for lower lip reconstruction [1,2,5,9], such as the rotational fan flap [10], pedicled flaps utilizing the facial [5,11] or labial [12] vasculature. However, these flaps may result in perioral scars and microstomia [8,13-15], and donor site morbidity [16].
The free BFFG has been described as a graft able to support the reconstruction of soft tissue defects in the oral cavity [6]. These include intraoral defects in the hard palate, oral mucosa, and the alveolar ridges [7,17,18] as well as the reconstruction of major oral defects [19-22]. The ease of harvest, handling, and minimal donor-site morbidity of the BFFG enhances defect healing and rapid epithelialization [23,24]. The use of adipose grafts has been recently shown to possess major biological advantages, such as promoting soft tissue repair through neovascularization or migration of support cells from the graft into the engraftment site [25,26]. Moreover, the therapeutic potential of stem cells residing in adipose tissue has also been shown in previous reports, supporting the use of adipose tissue as a biological initiator of tissue remodeling and repair, both in pre-clinical and clinical studies [27-30].
Kim and Sasidaran reported on the free BFFG for soft tissue augmentation in the facial region with excellent outcomes. They stated that this graft is an effective option as a volumizer for filling defects in the head and neck area [31]. Recently, the BFFG has been utilized for aesthetic filling in complex maxillofacial cases following facial deformity-related reconstruction, post-traumatic surgical correction, and facial augmentation after tumor ablation [32,33].
Herein, we report for the first time a successful lower lip reconstruction utilizing the BFFG in a patient with lower lip deficiency secondary to resection of a malignant tumor. The fat graft compensated the resected volume and enhanced the closure of the surgical site. Adequate mouth closure and opening without microstomia and a natural contour of the reconstructed lower lip were obtained, providing acceptable aesthetic and functional results without extensive harvest of autologous tissue. The intra-oral donor site of the BFPG underwent complete healing, with no post-operative complications or visible scars.
4. Summary
The technique described in the current case may provide a simple and reliable tool for lower lip reconstruction, achieving aesthetic lower lip rehabilitation in a single stage with minimal scarring and morbidity.
Author contributions
Conceptualization, Surgeries and follow-up: F.K; writing, F.K et al; Review&editing: F.K ,I.R, S.S
References
- McCarn KE, Park SS. Lip Reconstruction. Otolaryngol Clin North Am 40 (2007): 361-380.
- Lubek JE, Ord RA. Lip Reconstruction. Oral Maxillofac Surg Clin North Am 25 (2013): 203-214.
- Matin MB, Dillon J. Lip Reconstruction. Oral Maxillofac Surg Clin North Am 26 (2014): 335-357.
- Neligan PC. Strategies in Lip Reconstruction. Clin Plast Surg 36 (2009): 477-485
- Karapandzic M. Reconstruction of lip defects by local arterial flaps. Br J Plast Surg27 (1974): 93-97.
- Egyedi P. Utilization of the buccal fat pad for closure of oro-antral and/or oro-nasal communications. J Maxillofac Surg 5 (1977): 241-244.
- Kablan F, Laster Z. The Use of Free Fat Tissue Transfer from the Buccal Fat Pad to Obtain and Maintain Primary Closure and to Improve Soft Tissue Thickness at Bone-Augmented Sites: Technique Presentation and Report of Case Series. Int J Oral Maxillofac Implants 29 (2014): e220-e231.
- Ogino A, Onishi K, Okada E, et al. Unit advancement flap for lower lip reconstruction. J Craniofac Surg 29 (2018): 668-670.
- Calhoun KH. Reconstruction of small- and medium-sized defects of the lower lip. Am J Otolaryngol Neck Med Surg 13 (1992): 16-22.
- Gillies H. Plastic Surgery of the Face 1920. (2022).
- McHugh M. Reconstruction of the lower lip using a neurovascular island flap. Br J Plast Surg 30 (1977): 316-318.
- McGregor IA. Reconstruction of the lower lip. Br J Plast Surg 36 (1983): 40-47.
- Orsi VV, Pinto Oliveira AC. Lower Lip Reconstruction: Rudkin Technique And Bernard-Webster Technique. Plast Reconstr Surg 113 (2004): 1296.
- Yotsuyanàgi T, Nihei Y, Yokoi K, et al. Functional reconstruction using a depressor anguli oris musculocutaneous flap for large lower lip defects, especially for elderly patients. Plast Reconstr Surg 103 (1999): 850-856.
- Özkan Ö, Özkan Ö, Çinpolat A, et al. Functional lower lip reconstruction with the partial latissimus dorsi muscle free flap without nerve coaptation. Microsurgery 39 (2019): 131-137.
- Cakmak MA, Cinal H, Barin EZ, Sakat MS, Karaduman H, Tan O. Total lower lip reconstruction with functional gracilis free muscle flap. J Craniofac Surg 29 (2018): 735-737.
- Amin MA, Bailey BMW, Swinson B, Witherow H. Use of the buccal fat pad in the reconstruction and prosthetic rehabilitation of oncological maxillary defects. Br J Oral Maxillofac Surg 43 (2005): 148-154.
- Kablan F. The use of Buccal fat pad free graft in regenerative treatment of peri-implantitis: A new and predictable technique. Ann Maxillofac Surg 5 (2015): 179.
- Rapidis AD, Alexandridis CA, Eleftheriadis E, Angelopoulos AP. The use of the buccal fat pad for reconstruction of oral defects: Review of the literature and report of 15 cases. J Oral Maxillofac Surg 58 (2000): 158-163.
- Hao SP. Reconstruction of oral defects with the pedicled buccal fat pad flap. Otolaryngol - Head Neck Surg 122 (2000): 863-867.
- Dean A, Alamillos F, García-López A, Sánchez J, Peñalba M. The buccal fat pad flap in oral reconstruction. Head Neck 23 (2001): 383-388.
- Adeyemo WL, Ibikunle AA, James O, Taiwo OA. Buccal Fat Pad: A Useful Adjunct Flap in Cleft Palate Repair. J Maxillofac Oral Surg 18 (2019): 40-45.
- Kablan F. The use of buccal fat pad free graft in closure of soft-tissue defects and dehiscence in the hard palate. Ann Maxillofac Surg 6 (2016): 241.
- Staj?i? Z. The buccal fat pad in the closure of oro-antral communications: a study of 56 cases. J Cranio-Maxillofacial Surg 20 (1992): 193-197.
- Bellei B, Migliano E, Tedesco M, et al. Adipose tissue-derived extracellular fraction characterization: Biological and clinical considerations in regenerative medicine. Stem Cell Res Ther 9 (2018): 207.
- Zhang P, Feng J, Liao Y, et al. Ischemic flap survival improvement by composition-selective fat grafting with novel adipose tissue derived product - stromal vascular fraction gel. Biochem Biophys Res Commun 495 (2018): 2249-2256.
- Ebrahimian TG, Pouzoulet F, Squiban C, et al. Cell therapy based on adipose tissue-derived stromal cells promotes physiological and pathological wound healing. Arterioscler Thromb Vasc Biol 29 (2009): 503-510.
- Franck CL, Senegaglia AC, Leite LMB, et al. Influence of Adipose Tissue-Derived Stem Cells on the Burn Wound Healing Process. Stem Cells Int (2019).
- Shukla L, Luwor R, Ritchie ME, et al. Therapeutic Reversal of Radiotherapy Injury to Pro-fibrotic Dysfunctional Fibroblasts in Vitro Using Adipose-derived Stem Cells. Plast Reconstr Surg - Glob Open 8 (2020): e2706.
- Bashir MM, Sohail M, Bashir A, et al. Outcome of Conventional Adipose Tissue Grafting for Contour Deformities of Face and Role of Ex Vivo Expanded Adipose Tissue-Derived Stem Cells in Treatment of Such Deformities. J Craniofac Surg 29 (2018): 1143-1147.
- Kim JT, Sasidaran R. Buccal Fat Pad: An Effective Option for Facial Reconstruction and Aesthetic Augmentation. Aesthetic Plast Surg 41 (2017): 1362-1374.
- Jeong TK, Chung CH, Min KH. Multi-modal treatment strategy for achieving an aesthetic lower face. Arch Plast Surg 47 (2020): 256-262.
- Rahpeyma A, khajehahmadi S. Buccal Fat Pad Graft in Maxillofacial Surgery. Indian J Surg Oncol 12 (2021): 802-807.