"SHE" is at Risk: Analysis of Clinical Profiles, Interventions and Outcomes of Peripheral Arterial Disease in Women over a Period of 15 Years from India
Article Information
Rajendra Prasad Basavanthappa, Adharsh Kumar Maruthu Pandian*, Ashwini Naveen Gangadharan
Department of Vascular and Endovascular surgery, Ramaiah medical college and Hospital, Bengaluru, India
*Corresponding author: Dr. Adharsh Kumar Maruthu Pandian, Department of Vascular and Endovascular surgery, MS Ramaiah medical college, MS Ramaiah nagar, Mathikere, Bengaluru – 560094, Karnataka, India
Received: 25 December 2020; Accepted: 11 January 2021; Published: 20 January 2021
Supplementary File
Citation:
Rajendra Prasad Basavanthappa, Adharsh Kumar Maruthu Pandian, Ashwini Naveen Gangadharan. SHE" is at Risk: Analysis of Clinical Profiles, Interventions and Outcomes of Peripheral Arterial Disease in Women over a Period of 15 Years from India. Journal of Women’s Health and Development 4 (2021): 010-019.
Share at FacebookAbstract
Background: Peripheral arterial disease (PAD) is gaining equal status like Coronary artery disease (CAD) and Cerebrovascular accident (CVA) worldwide in terms of morbidity, economic issues and mortality. Females with PAD exhibit more of asymptomatic/ subclinical disease pattern. Any gender-based differences in terms of clinical profiles and treatment outcomes of PAD is crucial to be studied. Our study is a first of its kind in Indian subcontinent analysing only female PAD patients.
Objective: The purpose of this article is to assess the risk factor profiles, natural course of the disease, varied treatment options and their outcomes in different age groups of female PAD population coming to our centre.
Methods: This is a retrospective study and included all female patients who were diagnosed with PAD between the age group of 25 to 90 years and either underwent Vascular intervention or had conservative treatment for the same at Ramaiah medical college hospital, Bangalore, over a period of 15 years from 2004 to 2018.
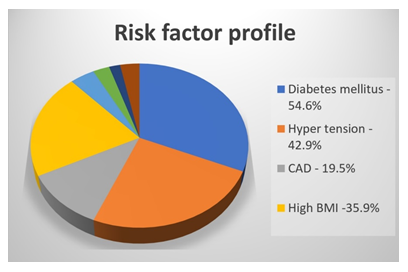
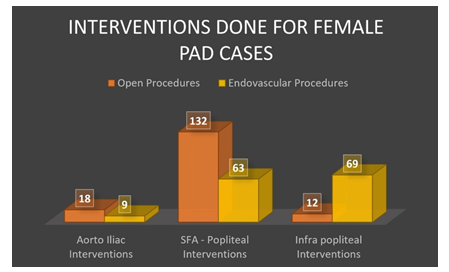
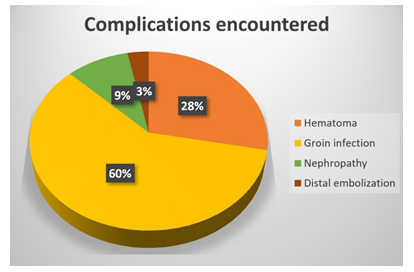
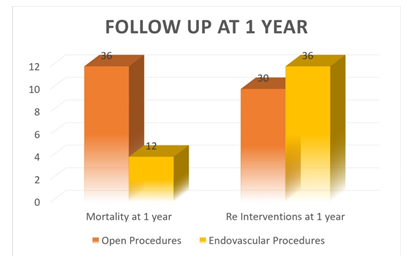
Results: The mean age of all cases was 59.41 years. Most common risk factors were “diabetes mellitus” (54.6%), “hypertension” (42.9%) and obesity (35.9%). Aorto Iliac segment interventions were done in 27 cases, SFA & popliteal in 195 cases and infra-popliteal in 81 cases. Technical success rate of open procedures was 96 % and for endovascular 90%. Major complications encountered were groin infection, hematoma, nephropathy and distal embolization. In a follow-up of 1 year, 48 patients succumbed to death due to coronary event and 66 of them required re-intervention due to either bypass graft thrombosis or new tissue loss.
Conclusion: PAD in females remains a major healthcare problem in our community, often due to delayed presentation and self-neglect, which leads to financial burden,
Keywords
Gender Differences, Peripheral Arterial Diseases, Prevalence, Risk Factors, Females, Vascular Interventions, Outcomes, Experience in Single Centre
Gender Differences articles; Peripheral Arterial Diseases articles; Prevalence articles; Risk Factors articles; Females articles; Vascular Interventions articles; Outcomes articles; Experience in Single Centre articles
Article Details
1. Introduction
Across the globe, Peripheral arterial diseases (PAD) in women have become a major concern to health in recent times. PAD is gaining equal status in comparison to Coronary artery disease (CAD) and Cerebrovascular accident (CVA) worldwide in terms of morbidity, economic issues and mortality. Pathology of PAD involves formation of intra-arterial atheroma with core of cholesterol and fibrous cover causing occlusion of medium and large sized arteries in extremities [1]. Progression of PAD is in multiple levels; hence the presentation varies from one person to another even between different genders, which is why it is essential to study in detail about this, implement all possible stra-tegies to treat and in first place to prevent this disease [1]. Women population with PAD exhibit more of asymptomatic/ atypical/subclinical disease pattern [2].
Hirsch et al., in a scientific statement from American heart association (AHA) in 2012, has stressed the importance of this and suggested the need to raise awareness, make individualized treatment plans and widen the research options in females with PAD [3]. Almost 20-30 % women older than 70 years suffer from PAD which is thought probably due to decrease in vascular protective effect of oestrogen which usually promotes vasodilatation and also has antioxidative effects [4]. In one study analysing gender difference in PAD, it was seen that females were more likely to be admitted as emergencies rather than elective for vascular interventions in comparison to males [5]. As women population continues to age, there will also be a continuous demand on health care system and any difference between gender in terms of natural course and treatment outcomes of PAD is crucial to be studied [6]. The purpose of this article is to assess the clinical profiles, various treatment options given and their outcomes in different age groups of female PAD population coming to our centre. This is the first of its kind study in Indian subcontinent analysing only female PAD patients.
2. Materials and Methods
This observational cross sectional, study included all female patients who were diagnosed with peripheral arterial disease (PAD) between the age group of 25 to 90 years, admitted and either underwent Vascular intervention or had conservative management for the same at Ramaiah medical college and teaching hospital, Bangalore, over a period of fifteen years from 2004 to 2018. This data was collected from our hospital medical registers and death registers. Though the term “PAD” refers to a variety of non-coronary syndromes, this article focusses on extremity vessels only – lower limb arteries below the level of renals and upper limb arteries after the subclavian origin. Patients with extremity ischaemia due to trauma, carotid interventions, interventions for aneurysmal disease were excluded from this study. Various details about patients like their demographics, comorbidities, medical management, indications of operative interventions, types of intervention performed and their outcomes including mortality data was collected.
Study included 384 patients in total with both upper limb and lower limb PAD. Important risk factors noted in study were diabetes mellitus, hypertension and hyperlipidaemia. If only medical management were done for these cases, their details were recorded. Apart from this, if intervened, indications for operative intervention either Critical limb threatening ischaemia (CLI) or Claudication; Number of various open interventions like endarterectomies, arterial bypasses and endovascular interventions (angioplasty) was also recorded. Technical success rate of these procedures, Complications, number of re-interventions and mortality at the end of 1 year in these cases were recorded. Data collection and procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional). No personal data that could be directly linked to a patient were used in this study and their confidentiality was strictly protected, all throughout the data collection and analysis.
3. Results
A total of 384 female patients were included in this retrospective review who fit into above mentioned criterions. Patients with Lower extremity PAD were 318 and those with upper extremity PAD were 66. Female PAD patients between age group of 25 to 90 were included in study with mean age of all cases being 59.41 years. 17 % belonged to age group of 25-40 years, 36% belonged to age group of 40-60 years and 47% belonged to age group of 60-90 years. The most common amongst risk factors encountered in patients with PAD was diabetes mellitus, found in 54.6% of cases; followed by hypertension (42.9%), obesity (35.9%) and coronary artery disease (19.5%) (Chart 1). A comparison of risk factor profiles noted in our study and that of various other studies with female PAD also shows a similar trend with HTN and DM patients forming the major group (Table 1). Most of the PAD cases were evaluated by CT/MRI (Computed tomography/ Magnetic resonance imaging) angiogram (318 cases) and doppler ultrasound was used to diagnose the remaining patients (66 cases). Out of the 384 cases, number of patients that required intervention was 303 and those managed conservatively was 81, of which 66 cases were having upper extremity ischemia.
Cases were intervened both for critical limb threatening ischemia (Rutherford class C5 C6 - 252 cases) and for severe claudication/rest pain (Rutherford class C3 C4 -51 cases). Aorto Iliac segment interventions were performed in 27 cases, SFA and popliteal segment interventions were performed in 195 cases and infra-popliteal segment interventions were performed in 81 cases (Chart 2). Immediate technical success rate of the open procedures was 96 % and for endovascular procedures it was 90%. The major complications encountered in these patients (both open/ endovascular) were groin infection, hematoma, nephropathy and distal embolization (Chart 3). In a follow-up of 1 year of these female patients it was seen that 48 of them succumbed to death due to a coronary event and 66 of them required re-interventions mainly due to lifestyle limiting claudication as a result of bypass graft thrombosis or new tissue loss in the intervened extremity (Chart 4). Total number of patients that finally ended up for an amputation after a vascular intervention was 72 cases, of which 33% had below knee amputation, 21% had trans-metatarsal amputation and 46% underwent above knee amputation.
|
Study |
Hypertension (%) |
Diabetes Mellitus (%) |
Coronary Artery Disease (CAD) (%) |
Obesity Dysli-pidaemia (%) |
Cerebrovascular Accident (CVA) (%) |
|
Vouyouka et al., (5) |
61.73 |
41.47 |
32.93 |
11.86 |
6.85 |
|
Gallagher et al., (6) |
87.3 |
54.1 |
44.5 |
49.8 |
- |
|
Choi et al., (23) |
78.5 |
64.2 |
11.3 |
41.3 |
14.7 |
|
Ferranti et al., (30) |
86.3 |
57.1 |
27.7 |
33.7 |
- |
|
Our Study |
42.9 |
54.6 |
19.5 |
35.9 |
7.8 |
Table 1: Comparison of risk factor profile of Female PAD cases in various studies.
4. Discussion
In this study, female patients with PAD admitted at a tertiary care centre in bangalore during the period from 2004 - 2018 were studied to explore the prevalence of risk factors and to determine the correlation between these factors and the disease. In one review by Higgins et al., prevalence of PAD in women between age group of 45 to 90 years was reported to range from 3% to 30% over a span of 5 decades [7]. Using US census data from 2010, the burden of PAD was calculated and it showed that there were increased number of women than men with PAD among US adults, who were more than 40 years of age [3]. In various clinical research trials women population with PAD were always under – represented, probable reason being selection bias wherein elderly women were less likely to attend clinical examinations, possibly refuse ankle blood pressure measurements and thereby delay diagnosis [8]. In our study of 384 female PAD cases it was seen that most of study population belonged to 60 – 90 years of
age group.
People with PAD have greater functional impairment like limitations in the ability of an individual to participate in social and occupational aspects of life with greater mobility loss than those without PAD [9]. Especially, female population with PAD has even more functional impairment and poor quality of life due to this, than those without peripheral arterial disease [10]. In our study female population with both upper (66 cases) and lower extremity (318 cases) ischaemia over a period of 15 years were included. Studies has suggested that there are basic gender differences in peripheral arterial disease cases, some of which are attributable to the variable levels of oestrogen and progesterone hormones in women [11]. Oestrogen is proven to improve the degradation of LDL cholesterol, to reduce the proliferation of the tunica media of the blood vessel wall, and to inhibit production of extracellular matrix [12]. Progesterone also plays an important anti-atherosclerotic role,acting both directly on the blood vessel wall and indirectly via potentiating the antioxidant action of oestrogen [12]. However, the effects of these two hormones usually abate after menopause, and it is unlikely that these will play a significant role in improving the outcomes after 60 years of age [13], as seen in our study population. Apart from this there are also certain other factors which delays the prompt medical treatment of vascular diseases in aged women. Elderly women are more likely than men to live alone, to be isolated, to live in extended care facilities and may also have to care for an even more disabled older spouse and, therefore, often neglect their own symptoms [14]. Current evidence suggests that lower socioeconomic status, in turn leading to lower education levels results in higher rates of smoking, obesity, physical inactivity, and increased risk of diabetes mellitus [15], however in our study the socio-economic status of the population was not taken into consideration, which may be one of the limitations of this study.
Hypertension and diabetes mellitus were found in almost one-third of our study population. Hypertension promotes fatty streak deposition on the endothelial lining of blood vessels leading to atherosclerotic plaque formation and progression, and endothelial dysfunction. Additionally, hypertensive shearing forces lead to plaque rupture [16]. Similarly, diabetes mellitus-associated hyperglycaemia results in impairment of vascular repair mechanisms, alteration of the ROS (reactive oxygen species) generation, and changes in platelet reactivity and coagulation pathway [17]. Consequently, diabetes mellitus also increases an individual’s risk for PAD by two- to fourfold [18]. In our study hypertension and diabetes mellitus was seen in 42.9% and 54.6% of cases respectively. Apart from these various other factors like coronary artery disease, obesity and prior cerebrovascular accident were all found in lesser frequencies in our study. This is probably attributed to the common underlying pathophysiological mechanisms that result in progressive atherosclerosis of medium- and large-sized blood vessels [18]. However, one important limitation seen in our sample was selection bias; in which data on certain other clinical profiles like lipid status, renal function status and smoking or tobacco usage (as most of working women of low socio-economic status chew tobacco and affluent young females have the habit of smoking in our locality) of these patients was not available to be assessed.
It was seen that after clinical evaluation, these patients were subjected to either duplex or angiographic evaluation for confirmation of diagnosis and plan for intervention. Duplex enables radiation-free non-invasive detection and localization of stenoses in the peripheral arteries. Apart from it, duplex is also useful for follow-up after angioplasty or monitoring of bypass grafts post-surgery [19]. However, differences in diagnostic sensitivity or accuracy pose a challenge for its generalized application, especially in women [20]. In highly calcified arteries as seen with diabetics, obesity, insonation in the area of open ulcers or excessive scarring and especially for females in aorto iliac segments, duplex poses a particular sex-related challenge [20]. Angiographic evaluation on other hand, provides information regarding extent of the disease and help to determine whether the patient is a candidate for revascularization or not [19]. In our study angiographic evaluation was performed for all lower limb ischaemia cases and upper limb ischemia’s were evaluated with a duplex scan. Although women’s native arterial diameters are smaller than that of men in the same age, there are no documented sex differences in the diagnostic sensitivity or accuracy of these advanced imaging techniques [21].
In our study, all cases of upper limb ischaemia were managed conservatively with either anticoagulation/ thrombolysis according to our centre’s protocol of treatment of upper limb ischaemia. Hultgren et al., have reported a higher proportion of supra-inguinal procedures among women undergoing revascularization for PAD (44% versus 19%) [22], whereas in our study population it was the opposite with infra inguinal procedures constituting almost 2/3rds of the intervened cases. Higher rates of emergent hospital admission and nursing home discharges in women with PAD have also been observed which reflects the disparities in family or social support available to women who are considering elective revascularization [22]. In our study too, out of the 303 interventions performed, 96 has been done as emergency for acute limb ischaemia cases. Among the lower limb ischaemia’s, conservative management was done in 15 cases who had delayed presentation using prostaglandin infusion/anticoagulation. Choi et al., has found that after interventions, women were associated with higher adverse events in those who presented with claudication compared with men, but there was no significant difference of outcomes between the two groups in patients who presented with CLI [23]. In our study most of female PAD cases had operative indication as critical limb threatening ischaemia (Rutherford c5, c6 – 252 cases) and it was less for claudication (Rutherford c3, c4 – 51 cases). Belkin et al., established that females frequently have more severe infra-inguinal disease at first presentation itself and present for limb salvages [24]. Our study data also reflects this trend, as more females underwent intervention for critical limb threatening ischaemia as compared to claudication as operative indication.
Various studies have observed inferior patency rates following surgical revascularization in females [25]. Grenn et al., observed that 5-year cumulative patency rates in female population following surgical revascularisation was about 45% compared to the male counterparts [25]. In our study, a total of 162 open and 141 endovascular interventions were performed and technical success rate for open surgery was 96% whereas for endovascular interventions it was 90%. Of these cases almost 66 cases required re-intervention (either for thrombosed bypass graft or new tissue loss in previously operated extremity) within a follow-up period of 1 year and 72 cases ultimately ended up in amputation, 33 of which were done for acute limb ischaemia. The average rate of lower limb amputation complicating PAD in female population, reported in the literature was 5% [26]. The slightly higher percentage of women who underwent amputation in our study group (11.5%) is supported by several studies reporting poor limb salvage rates in women [26]. Inferior rates of limb salvage in women has been suggested to be related to delayed diagnosis in women, anatomic differences in females or a poor diagnostic awareness among clinicia-ns [26].
Various studies have reported increased rates of perioperative wound complications in women [27]. Belkin et al., observed a greater frequency of wound complications (infections, hematomas, and seromas) in women undergoing in situ lower extremity arterial bypass [24]. Nguyen et al., also identified female gender as an independent predictor of wound complications after lower extremity bypass and observed associations with major wound complications, increased length of hospital stays, and lower quality of life [27]. Factors like smaller diameter of blood vessels and increased incidence of multilevel disease at presentation may contribute to the higher incidence of procedural complications in female population [23]. In our study various complications like hematoma, groin infection, nephropathy and distal embolization was seen following both open and endovascular interventions, out of which groin hematoma and infections occurred in a higher frequency. Particularly with hematoma and bleeding complications, a possible explanation can be difference in the pharmacokinetics of heparin in females [28]. Females tend to metabolize heparin slower, even after correcting for age and weight differences. One of the studies showed that despite strict weight-based dosages given, women were at a higher risk of aPTT (activated partial thromboplastin time) overshoot [28]. Increased rate of periprocedural infections was also seen in our study group after open reconstructions and major amputations. Although the increased infection risk in these studies may be attributable to a higher prevalence of diabetes mellitus, certain other studies have identified female gender itself as an independent predictor of occurrence of wound complications [29]. The basis biologically for such differences in the infection rates of females has not been completely described but may include differences in metabolism, fat content and distribution, mainly in the upper thighs and abdomen of women [29].
Magnant et al., reported similar perioperative mortality rates among men and women undergoing infra-inguinal bypass for lower extremity ischemia but decreased long-term survival in women and also established a gender-dependent effect of diabetes mellitus on outcomes, with increased mortality in diabetic women [30]. Egorova et al., noted an increased hospital mortality rate in women with PAD after interventions and observed the highest mortality risk in women undergoing surgical revascularization and amputations [30]. Choi et al., has reported that compared with the male group, females showed a significantly higher rates of all-cause death, MI, or major amputation following vascular intervention [23]. In our study 48 cases in age group of 60-90 years succumbed to death (13%) over follow-up period of 1-year time due to a coronary event, however no procedure related deaths were reported in our study population. Apart from selection bias due to its retrospective nature, other limitations that we noticed in our study was residual or unmeasured confounding factors that could have influenced the results.
5. Conclusion
PAD in females remains a major healthcare problem in our community, often due to delayed presentation and self-neglect, which adds on to the financial burden at first consultation to a hospital. Challenges in treatment of these patients are, higher prevalence of asymptomatic disease and late presentation, that leads to increased risk of coronary or limb related adverse events and mortality, despite intervention. Sincere research efforts in form of large prospective observational study should be carried out in future, to further determine the effects of female sex on different aspects of PAD including risk factors, clinical burden, treatment options and their outcomes.
Financial Support and Sponsorship
Nil.
Disclosure Statement
There are no conflicts of interest.
References
- Mufti Alsadiqi AI, Subki AH, Abushanab RH, et al. Peripheral artery disease risk factors in Jeddah, Saudi Arabia: a retrospective study. Int J Gen Med 12 (2019): 49-54.
- Jelani Q, Petrov M, Martinez SC, et al. Peripheral Arterial Disease in Women: an Overview of Risk Factor Profile, Clinical Features, and Outcomes. Curr Atheroscler Rep 40 (2018).
- Alan T Hirsch, Matthew A Allison. A Call to Action: Women and Peripheral Artery Disease A Scientific Statement From the American Heart Association - Endorsed by the Vascular Disease Foundation and its Peripheral Artery Disease Coalition. AHA Journal ,Circulation 125 (2012): 1449-1472.
- Qurat-ul-ain Jelani, Sara C Martinez, et al. Peripheral Arterial Disease in Women: an Overview of Risk Factor Profile, Clinical Features, and Outcomes. Current Atherosclerosis Reports 20 (2018): 40.
- Vouyouka A G, Egorova NN, Salloum A, et al. Lessons learned from the analysis of gender effect on risk factors and procedural outcomes of lower extremity arterial disease. Journal of Vascular Surgery 52 (2010): 1196-1202.
- Gallagher Katherine A, Andrew J Meltzer, Reid A Ravin, et al. Gender Differences in Outcomes of Endovascular Treatment of Infrainguinal Peripheral Artery Disease. Vascular and Endovascular Surgery 8 (2011): 703-711.
- Higgins JP, Higgins JA. Epidemiology of peripheral arterial disease in women. J Epidemiol 13 (2003): 1-14.
- Mosenifar Z. Population issues in clinical trials. Proc Am Thorac Soc 4 (2007): 185-187.
- McDermott MM, Guralnik JM, Tian L, et al. Baseline functional performance predicts the rate of mobility loss in persons with peripheral arterial disease. J Am Coll Cardiol 50 (2007): 974-982.
- Collins TC, Suarez-Almazor M, Bush RL, et al. Gender and peripheral arterial disease. J Am Board Fam Med 19 (2006): 132-140.
- Barrett-Connor E, Bush TL. Estrogen and coronary heart disease in women. JAMA 265 (1991): 1861-1867.
- Price J, Leng GC. Steroid sex hormones for lower limb atherosclerosis. Cochrane Database Syst Rev 10 (2012): CD000188.
- MaysBW, Towne JB, FitzpatrickCM, et al. Women have increased risk of perioperative myocardial infarction and higher long-term mortality rates after lower extremity arterial bypass grafting. JVasc Surg 29 (1999): 807-812.
- Vouyouka AG, Kent KC. Arterial vascular disease in women. J Vasc Surg 46 (2007): 1295-1302.
- Nguyen LL, Henry AJ. Disparities in vascular surgery: is it biology or environment?. J Vasc Surg 51 (2010): S36-S41.
- Zaheer M, Chrysostomou P, Papademetriou V. Hypertension and atherosclerosis: patho-physiology, mechanisms and benefits of BP control. In: Andreadis EA, editor. Hypertension and Cardiovascular Disease (2016): 201-216.
- Paneni F, Beckman JA, Creager MA, et al. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J 34 (2013): 2436-2443.
- Kalbaugh CA, Kucharska-Newton A, Wruck L, et al. Peripheral artery disease prevalence and incidence estimated from both outpatient and inpatient settings among medicare fee-for-service beneficiaries in the Atherosclerosis Risk in Communities (ARIC) study. J Am Heart Assoc 6 (2017): e003796.
- Tendera M, Aboyans V, Bartelink M-L, et al. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatm. European heart journal 32 (2011): 2851-2906.
- Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gender medicine 6 (2009): 60-75.
- AhChong AK, Chiu KM, Wong M, et al. The influence of gender difference on the outcomes of infrainguinal bypass for critical limb ischaemia in Chinese patients. European journal of vascular and endovascular surgery: the official journal of the European Society for Vascular Surgery 23 (2002): 134-139.
- Hultgren R, Olofsson P, Wahlberg E. Sex-related differences in outcome after vascular interventions for lower limb ischemia. J Vasc Surg 35 (2002): 510-516.
- Choi KH, Park TK, Kim J, et al. Sex Differences in Outcomes Following Endovascular Treatment for Symptomatic Peripheral Artery Disease: An Analysis From the K- VIS ELLA Registry. J Am Heart Assoc 8 (2019): e010849.
- Belkin M, ConteMS, DonaldsonMC, et al. The impact of gender on the results of arterial bypass with in situ greater saphenous vein. Am JSurg 170 (1995): 97-102.
- Green RM, Abbott WM, Matsumoto T, et al. Prosthetic above-knee femoropopliteal bypass grafting: five-year results of a randomized trial. J Vasc Surg 31 (2000): 417-425.
- Swaminathan A, Vemulapalli S, Patel MR, et al. Lower extremity amputation in peripheral artery disease: improving patient outcomes. Vasc Health Risk Manag 10 (2014): 417-424.
- Nguyen LL, Brahmanandam S, Bandyk DF, et al. Female gender and oral anticoagulants are associated with wound complications in lower extremity vein bypass: an analysis of 1404 operations for critical limb ischemia. J Vasc Surg 46 (2007): 1191-1197.
- Cheng S, Morrow DA, Sloan S, et al. Predictors ofinitial nontherapeutic anticoagulation with unfractionated heparin in ST-segment elevation myocardial infarction. Circulation 119 (2009): 1195-1202.
- Ferranti KM, Osler TM, Duffy RP, et al. Vascular Study Group of New England. Association between gender and outcomes of lower extremity peripheral vascular interventions. J Vasc Surg 62 (2015): 990-997.
- Egorova N, Vouyouka AG, Quin J, et al. Analysis of gender-related differences in lower extremity peripheral arterial disease. J Vasc Surg 51 (2010): 372.e1-378.e1.