Pyogenic Dorsal and Lumbar Spondylodiscitis treated with Minimally Invasive Endoscopic Procedure and Posterior Percutaneous Instrumentation
Article Information
Rita Macedo Sousa*, Carlos Branco, Diogo Sousa, João Reis, André Guimarães, Ricardo Geraldes, Pedro Teixeira Gomes
Department of Orthopaedics, Centro Hospitalar de Trás-os-Montes e Alto Douro, Portugal
*Corresponding Author: Rita Macedo Sousa, Department of Orthopaedics, Centro Hospitalar de Trás-os-Montes e Alto Douro, Portugal
Received: 14 January 2021; Accepted: 25 January 2021; Published: 29 January 2021
Citation:
Rita Macedo Sousa, Carlos Branco, Diogo Sousa, João Reis, André Guimarães, Ricardo Geraldes, Pedro Teixeira Gomes. Pyogenic Dorsal and Lumbar Spondylodiscitis treated with Minimally Invasive Endoscopic Procedure and Posterior Percutaneous Instrumentation. Journal of Spine Research and Surgery 3 (2021): 001-009.
Share at FacebookAbstract
Introduction: Spondylodiscitis is a rare infection of the intervertebral disc and nearby bone structures, which incidence has been increasing in the past decades. Conservative treatment is the gold standard, but sometimes surgery is needed to relief the symptoms and eradicate the infection, preserve the neurological function, and restore structural alignment and stability.
Case presentation: The authors present a clinical case of a 73-year-old-male with T11-12 and L4-L5 spondylodiscitis with an epidural collection at this last level, treated surgically with an interlaminar endoscopic debridement and posterior percutaneous instrumentation after failing of isolated medical treatment.
Discussion: The diagnosis of spondylodiscitis may sometimes be difficult due to its non-specific symptoms and sometimes inconclusive blood tests. Endoscopic surgery along with posterior percutaneous instrumentation provides a minimally invasive surgical option in multimorbid patients and/or in early stages of the disease, reducing the surgical trauma, complications and fastening the recovery.
Conclusion: Spondylodiscitis is a highly heterogeneous disease, remaining its diagnosis and treatment a complex challenge. With this case report the authors expect to raise awareness to the use of minimally invasive techniques in treating diseases of this type.
Keywords
Spondylodiscitis, Endoscopy, Endoscopic Spinal Surgery, Percutaneous Posterior Spinal Instrumentation, Minimally Invasive Surgery
Spondylodiscitis articles Spondylodiscitis Research articles Spondylodiscitis review articles Spondylodiscitis PubMed articles Spondylodiscitis PubMed Central articles Spondylodiscitis 2023 articles Spondylodiscitis 2024 articles Spondylodiscitis Scopus articles Spondylodiscitis impact factor journals Spondylodiscitis Scopus journals Spondylodiscitis PubMed journals Spondylodiscitis medical journals Spondylodiscitis free journals Spondylodiscitis best journals Spondylodiscitis top journals Spondylodiscitis free medical journals Spondylodiscitis famous journals Spondylodiscitis Google Scholar indexed journals Endoscopy articles Endoscopy Research articles Endoscopy review articles Endoscopy PubMed articles Endoscopy PubMed Central articles Endoscopy 2023 articles Endoscopy 2024 articles Endoscopy Scopus articles Endoscopy impact factor journals Endoscopy Scopus journals Endoscopy PubMed journals Endoscopy medical journals Endoscopy free journals Endoscopy best journals Endoscopy top journals Endoscopy free medical journals Endoscopy famous journals Endoscopy Google Scholar indexed journals Endoscopic Spinal Surgery articles Endoscopic Spinal Surgery Research articles Endoscopic Spinal Surgery review articles Endoscopic Spinal Surgery PubMed articles Endoscopic Spinal Surgery PubMed Central articles Endoscopic Spinal Surgery 2023 articles Endoscopic Spinal Surgery 2024 articles Endoscopic Spinal Surgery Scopus articles Endoscopic Spinal Surgery impact factor journals Endoscopic Spinal Surgery Scopus journals Endoscopic Spinal Surgery PubMed journals Endoscopic Spinal Surgery medical journals Endoscopic Spinal Surgery free journals Endoscopic Spinal Surgery best journals Endoscopic Spinal Surgery top journals Endoscopic Spinal Surgery free medical journals Endoscopic Spinal Surgery famous journals Endoscopic Spinal Surgery Google Scholar indexed journals Percutaneous Posterior Spinal Instrumentation articles Percutaneous Posterior Spinal Instrumentation Research articles Percutaneous Posterior Spinal Instrumentation review articles Percutaneous Posterior Spinal Instrumentation PubMed articles Percutaneous Posterior Spinal Instrumentation PubMed Central articles Percutaneous Posterior Spinal Instrumentation 2023 articles Percutaneous Posterior Spinal Instrumentation 2024 articles Percutaneous Posterior Spinal Instrumentation Scopus articles Percutaneous Posterior Spinal Instrumentation impact factor journals Percutaneous Posterior Spinal Instrumentation Scopus journals Percutaneous Posterior Spinal Instrumentation PubMed journals Percutaneous Posterior Spinal Instrumentation medical journals Percutaneous Posterior Spinal Instrumentation free journals Percutaneous Posterior Spinal Instrumentation best journals Percutaneous Posterior Spinal Instrumentation top journals Percutaneous Posterior Spinal Instrumentation free medical journals Percutaneous Posterior Spinal Instrumentation famous journals Percutaneous Posterior Spinal Instrumentation Google Scholar indexed journals Minimally Invasive Surgery articles Minimally Invasive Surgery Research articles Minimally Invasive Surgery review articles Minimally Invasive Surgery PubMed articles Minimally Invasive Surgery PubMed Central articles Minimally Invasive Surgery 2023 articles Minimally Invasive Surgery 2024 articles Minimally Invasive Surgery Scopus articles Minimally Invasive Surgery impact factor journals Minimally Invasive Surgery Scopus journals Minimally Invasive Surgery PubMed journals Minimally Invasive Surgery medical journals Minimally Invasive Surgery free journals Minimally Invasive Surgery best journals Minimally Invasive Surgery top journals Minimally Invasive Surgery free medical journals Minimally Invasive Surgery famous journals Minimally Invasive Surgery Google Scholar indexed journals Pyogenic Dorsal articles Pyogenic Dorsal Research articles Pyogenic Dorsal review articles Pyogenic Dorsal PubMed articles Pyogenic Dorsal PubMed Central articles Pyogenic Dorsal 2023 articles Pyogenic Dorsal 2024 articles Pyogenic Dorsal Scopus articles Pyogenic Dorsal impact factor journals Pyogenic Dorsal Scopus journals Pyogenic Dorsal PubMed journals Pyogenic Dorsal medical journals Pyogenic Dorsal free journals Pyogenic Dorsal best journals Pyogenic Dorsal top journals Pyogenic Dorsal free medical journals Pyogenic Dorsal famous journals Pyogenic Dorsal Google Scholar indexed journals Lumbar Spondylodiscitis articles Lumbar Spondylodiscitis Research articles Lumbar Spondylodiscitis review articles Lumbar Spondylodiscitis PubMed articles Lumbar Spondylodiscitis PubMed Central articles Lumbar Spondylodiscitis 2023 articles Lumbar Spondylodiscitis 2024 articles Lumbar Spondylodiscitis Scopus articles Lumbar Spondylodiscitis impact factor journals Lumbar Spondylodiscitis Scopus journals Lumbar Spondylodiscitis PubMed journals Lumbar Spondylodiscitis medical journals Lumbar Spondylodiscitis free journals Lumbar Spondylodiscitis best journals Lumbar Spondylodiscitis top journals Lumbar Spondylodiscitis free medical journals Lumbar Spondylodiscitis famous journals Lumbar Spondylodiscitis Google Scholar indexed journals intervertebral disc articles intervertebral disc Research articles intervertebral disc review articles intervertebral disc PubMed articles intervertebral disc PubMed Central articles intervertebral disc 2023 articles intervertebral disc 2024 articles intervertebral disc Scopus articles intervertebral disc impact factor journals intervertebral disc Scopus journals intervertebral disc PubMed journals intervertebral disc medical journals intervertebral disc free journals intervertebral disc best journals intervertebral disc top journals intervertebral disc free medical journals intervertebral disc famous journals intervertebral disc Google Scholar indexed journals neurological function articles neurological function Research articles neurological function review articles neurological function PubMed articles neurological function PubMed Central articles neurological function 2023 articles neurological function 2024 articles neurological function Scopus articles neurological function impact factor journals neurological function Scopus journals neurological function PubMed journals neurological function medical journals neurological function free journals neurological function best journals neurological function top journals neurological function free medical journals neurological function famous journals neurological function Google Scholar indexed journals spinal canal articles spinal canal Research articles spinal canal review articles spinal canal PubMed articles spinal canal PubMed Central articles spinal canal 2023 articles spinal canal 2024 articles spinal canal Scopus articles spinal canal impact factor journals spinal canal Scopus journals spinal canal PubMed journals spinal canal medical journals spinal canal free journals spinal canal best journals spinal canal top journals spinal canal free medical journals spinal canal famous journals spinal canal Google Scholar indexed journals
Article Details
1. Introduction
The term spinal infection comprises a range of infectious diseases of the spine, with a classification based on the location and the affected tissue (vertebral body, intervertebral disc, spinal canal and paraspinal tissues) [1, 2], or on the etiology of the infection (pyogenic, granulomatous and parasitic) [1, 2]. Spondylodiscitis is, by definition, an infection of the intervertebral disc and nearby bone structures. This rare entity, represents 0.15-5% of all cases of osteomyelitis [2], with an estimated annual incidence in Europe of 0.4-2.8 new cases/100,000 habitants per year [3]. Despite this, the incidence has been increasing, due to the increase in life expectancy (especially in the immunocompromised population), infections associated to healthcare, and the expansion of spinal surgery [1-5]. Advances in diagnosis and treatment of this condition, whether conservative or surgical, have substantially decreased the morbidity and mortality rates in the past few decades [4], but it still remains between 2-20% [1, 6]. Among the risk factors are advanced age, male sex (1.5-2:1) immunocompromised status (such as HIV infection, intravenous drug abuse, immunosuppression), underlying co-morbidities (like diabetes, renal failure, rheumatological disease, hepatic cirrhosis), previous infections, previous spinal surgery, outpatient spinal procedures, and a low socioeconomic status [1, 2, 6].
There are three infection pathways described: endogenous, exogenous and extension from a contiguous infection site (per continuitatem) [6-8]. Hematogenous spread is the most common [2, 6], with a distant infected site identified in 50% of the patients [2]. The lumbar spine the most affected region (followed by the thoracic, cervical and sacral spine) [1, 2, 7]. Usually a mono-microbial infection, Staphylococcus aureus is the most frequent causative agent in developed countries [2, 3, 6, 7] (20-84% of all cases [2]), followed by Enterobacteriae spp. (7-33%; most commonly Escherichia coli) [2, 6]. Mycobacterium tuberculosis the most common cause worldwide [3, 6, 7]. In endemic zones, Brucella must be considered [2, 6, 7]. In 30 to 40% of the patients a pathogen is not identified [2, 5].
Clinically, the symptoms are non-specific, which can delay the prompt diagnosis [1, 2, 4, 5, 7]. The pain is the most common symptom (85%) [1, 7], and typically is worse at night [2]. Fever (50%), malaise, anorexia, weight loss, difficulty in walking, inability to bend over, neurological deficits (27% to 1/3 at presentation), and even abdominal pain in children, are other associated symptoms [2, 7]. Diagnosis relies upon the clinical history, physical examination (tenderness, paravertebral muscle spasm and restricted range of motion [2]), blood tests (usually inconclusive; elevated white blood cell count, erythrocyte sedimentation rate, C-reactive protein, serum levels of alkaline phosphatase, and anemia; blood cultures – positive 30-78%; urine cultures [2, 7]) and imaging (radiographs, CT scan, MRI – the imaging modality of choice -, and nuclear imaging [1, 2, 7]). It might be difficult in early stages [1].
Treatment has several essential goals: relief of pain, eradication of the infection, preservation of the neurological function, restoration of the spinal stability, decompression of the spinal canal, and promotion of bone fusion [2, 7, 8]. Conservative treatment, with antibiotics in combination with other non-pharmacological treatments, remains the gold standard [2, 3, 7]. Surgical treatment is indicated in cases of failure of medical treatment, sepsis, spinal cord compression with progressive neurological deficits, spinal instability, significant deformity or paravertebral/epidural abscess [1-3, 5-7, 9]. Despite the fact that open surgery remains the standard of care, less invasive endoscopic techniques have been described [2, 10]. Posterior percutaneous instrumentation is safe and effective in relieving pain and preventing deformity and neurological compromise in non-complicated cases involving the lower thoracic or lumbar spine [2], reducing the need for braces after (versus non instrumented procedures). In combination with minimally invasive techniques (like endoscopy) diminished the surgical trauma, and so lead to less intraoperative blood loss, few postoperative compli-cations, shorter hospital stay and a faster recovery time [1, 11] in selected patients. Additional antibiotic treatment should be administrated in all cases [1].
Even though the prognosis is good if treatment is initiated promptly [6], the delay in diagnosis can explain why the mortality ranges between 2 and 20% [1, 6].
2. Case Report
A 73-year-old male, partially dependent in daily activities, with an history of hypertension, dyslipidemia, type 2 diabetes, ischemic cardiomyopathy with preserved ejection fraction (with previous CABG), peripheral arterial disease, obstructive sleep apnea (in treatment with a nocturnal CPAP) and an ex-smoker, was admitted to our emergency department with complains of low back pain and fever (39ºC). The pain began gradually and progressed in over a month, after a urinary tract infection treated with levofloxacin. Blood work at admission revealed an anemia (Hb 8.12 g/dl), an elevated white blood cell count (13500 with 88% neutrophils), and a CRP of 25,30 mg/dl (normal <0.5). Lumbar x-ray revealed no signs of acute traumatic osteo-articular lesions (Figure 1). Blood and urine cultures were obtained at admission, the patient started empirically ceftriaxone and azithromycin and was admitted to the medical ward for study and treatment. Four days after admission in the medical ward the patient remained febrile despite antipyretics, and with high levels of CRP. Blood cultures came back positive for Escherichia coli, and antibiotic treatment was adjusted to piperacillin/tazobactam. The thoraco-abdominal-pelvic CT scan at day 5 revealed discreet erosion of the end plates of T11-12 (Figure 2), an MRI was then ordered, and confirmed spondylodiscitis of T11-12 and L4-5, with an epidural collection at this level (Figure 3 a, b, c and d).
Once there was no clinical improvement after two weeks of treatment, CRP levels were constantly high, and being a multimorbid patient, a minimally invasive endoscopic procedure along with a posterior percutaneous fixation was proposed. For the surgery, the patient was positioned in prone, under general anesthesia. A percutaneous biopsy at T11 and T12 was performed. Then an interlaminar endoscopic approach for L4-L5 was performed, aided by a C-arm view. Irrigation with a normal saline was maintained and debridement and discectomy performed (Figure 4), followed by a posterior percutaneous instrumentation of T10-L1 and L4-S1 (Figure 5 a and b). The incisions were closed in layers and the biopsy material and the debris were sent to microbiology analysis, which came back negative.
Surgery and postoperative period were uneventful. The patient symptoms and blood work improved after surgery (he never had fever again), and he began rehabilitation. He completed a cycle of 4 days of ceftriaxone and azithromycin, followed by 21 days of piperacillin/tazobactam (after isolation of E. Coli in blood cultures) and 19 days of ceftriaxone. At discharge time he had a complete resolution of the symptoms and WBC, CRP and ESR were normal. At 12 months follow up the patient remained well, walking without wearing any aiding device, with return to his previous functional status. The CT scan (Figure 6) revealed partial fusion of T11-12 and no signs of recurrence.

Figure 1: Lumbar x-ray at admission (lateral view).
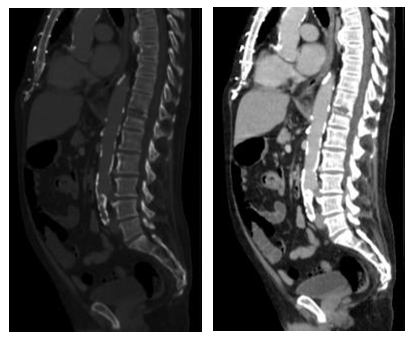
Figure 2: Thoraco-abdominal-pelvic CT scan.
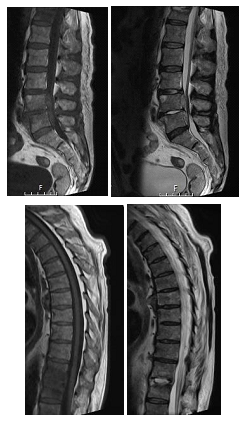
Figure 3: T1-weighted (a) and T2-weighted (b) sagittal lumbar MRI; T1-weighted (c) and T2-weighted (d) sagittal dorsal MRI.
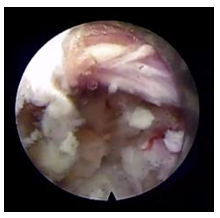
Figure 4: Endoscopic debridement at L4-L5 space.

Figure 5: Post-op x-ray – a) lumbar x-ray ; b) dorsal x-ray.
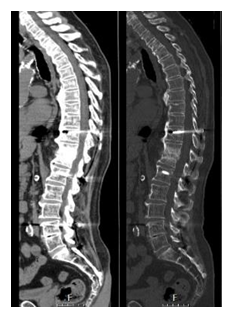
Figure 6: Post-op CT scan (at 12 months).
3. Discussion
Spondylodiscitis is an infection of the disc and the adjacent vertebrae [1], that although rare is increasing in prevalence [1-5]. In most cases, in developed countries, is caused by Staphylococcus aureus [2, 3, 6, 7], being Mycobacterium tuberculosis the most common cause worldwide [3, 6, 7]. The elevated mortality rate associated (2-20%) can be explain by the delay in diagnosis [1, 6], since the symptoms are non-specific [1, 2, 4, 5, 7] and the blood tests usually inconclusive. Blood cultures are positive in 30-78% of the cases [2] and should be performed, if possible, before the antibiotic treatment begins. A biopsy should be performed when the suspicion is high and the cultures negative [2, 7]. CT scan guided biopsy is the gold standard [2]. Open biopsy should be reserved for cases of negative CT-guided biopsy cultures [2, 7].
The first line of treatment is conservative [1-3, 7] and is a combination of an antimicrobial regimen (if possible after cultures are taken), pain killers and non-pharmacological measures [2, 7]. Immobilization with bed rest is recommended for no longer than two weeks (except in cases of major defects), and the patient should wear a protective brace after this [1, 2]. Braces will redistribute the load, and thereby decreasing pain and additional deformity by reducing the pressure and stress over the affected segments, and should be worn for six to ten weeks or until complete healing [7]. The length of the antimicrobial therapy is controversial ranging from six weeks to three months in pyogenic spondylodiscitis, three to six months in Brucella infections, nine to 24 months in tuberculosis [1, 2, 7]. The treatment must be monitored and discontinued when there is a resolution of the symptoms and a normalization of the acute phase reactants [1, 2]. Predictors of treatment failure (after four weeks) are lack of clinical improvement, persistent symptoms, and a persistently high C-reactive protein [2]. Prolonged unsuccessful conservative treatment compromise the remaining bone stock, leading to a much bigger and difficult surgery [2]. Residual back pain is more common in cases treated conservatively [1, 7] (16-50% [2]), as well as pseudarthrosis and instability, and the consequential kyphotic deformity [1, 2, 7].
Surgical treatment is indicated in cases of failure of medical treatment, sepsis, spinal cord compression with progressive neurological deficits, spinal instability, significant deformity or paravertebral/epidural abscess [1-3,5-7, 9]. Surgery should provide along with a eradication of the infection and pain relief, a decompression of the spinal canal, a restoration of spinal stability and correction of deformities and promote bone fusion [2, 7, 8]. Tissue sample harvesting should also be performed [2]. Open surgery remains the gold standard, but there are no specific guidelines for the perfect technique [1, 2]. There are multiple techniques described – anterior versus posterior versus combined approach, one stage versus two stages surgery, instrumentation or not [1, 2]. Open surgery with extensive debridement and fusion caries high risks of morbidity, especially in older patients [12]. Less invasive endoscopic techniques have been described [2, 10] and permit, like the open ones, direct observation and collection of samples for the diagnosis (with a higher diagnostic efficacy [11]), debridement of infected material in the epidural space, as well as in the intersomatic space [13]. Endoscopic debridement along with a posterior percutaneous instrumentation decrease the surgical trauma, and lead to less intraoperative blood loss, few postoperative complications, shorter hospital stay and a faster recovery time [1, 11] in multimorbid patients and/or in early stages of the disease [11], and decrease the need for braces after surgery. This approach is contraindicated in patients with advanced stage of infection, motor deficits or extensive bone destruction [14]. Additional antibiotic treatment should be administrated in all cases [1]. During follow-up, if there is no response to therapy, it is advisable to repeat attempts to isolate the causative agent [7]. In cases of infected spinal instrumentation or abscesses, without conditions for surgical debridement and drainage, prolonged suppressive cycles of antibiotic treatment may be necessary [2]. Follow-up MRI is not recommended because abnormal findings may persist even after complete recovery [2, 7].
4. Conclusion
Spondylodiscitis is a highly heterogeneous disease, remaining its diagnosis and treatment a complex challenge. Conservative treatment is the treatment of choice in patients without neurological deficit, spinal instability, deformity, and sepsis or with high surgical risk. In patients in which surgical procedures are necessary, endoscopic techniques associated with a percutaneous posterior instrumentation can be an alternative to a traditional open surgery in multimorbid patients and/or in early stages of the disease. By reporting this case, we aim to demonstrate that these minimally invasive procedures can provide good clinical outcomes while avoiding extensive open surgery and its associated risks.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Lener S, Hartmann S, Barbagallo GMV, et al. Management of spinal infection: a review of the literature. Acta Neurochir (Wien) 160 (2018): 487-496.
- Mavrogenis AF, Megaloikonomos PD, Igoumenou VG, et al. Spondylodiscitis revisited. EFORT Open Rev 2 (2017): 447-461.
- Soares Do Brito J, Tirado A, Fernandes P. Perfil epidemiológico da espondilodiscite tratada cirurgicamente. Acta Med Port 29 (2016): 319-325
- Tsai TT, Yang SC, Niu CC, et al. Early surgery with antibiotics treatment had better clinical outcomes than antibiotics treatment alone in patients with pyogenic spondylodiscitis: a retrospective cohort study. BMC Musculoskelet Disord 18 (2017): 1-7.
- Graells XSI, Kulcheski AL, Bondan ET, et al. Thoracolumbar Spondylodiscitis and the Surgical Approach: a Retrospective Analysis. Coluna/Columna 18 (2019): 154-157.
- Herren C, Jung N, Pishnamaz M, et al. Spondylodiscitis: Diagnosis and treatment options - A systematic review. Dtsch Arztebl Int 114 (2017): 875-882.
- Gregori Fabrizio, Grasso Giovanni, Iaiani Giancarlo, et al. Treatment algorithm for spontaneous spinal infections: A review of the literature. J Craniovertebral Junction Spine 10 (2019): 3-9.
- Duarte RM, Vaccaro AR. Spinal infection: State of the art and management algorithm. Eur Spine J 22 (2013): 2787-2799.
- Zarghooni K, Röllinghoff M, Sobottke R, et al. Treatment of spondylodiscitis. Int Orthop 36 (2012): 405-411.
- Kang T, Park SY, Lee SH, et al. Spinal epidural abscess successfully treated with biportal endoscopic spinal surgery. Med (United States) 98 (2019).
- Turel M, Kerolus M, Deutsch H. The role of minimally invasive spine surgery in the management of pyogenic spinal discitis. J Craniovertebr Junction Spine 8 (2017): 39-43.
- Choi, Seung-Jin, Ji, et al. Pyogenic Lumbar Spondilodiscitis Treated by Percutaneous Transforaminal Endoscopic Procedure: A Case Report. Kor J Spine 1 (2004): 277-281.
- Mao YM, Li Y, Cui X. Percutaneous endoscopic debridement and drainage for spinal infection: Systemic review and meta-analysis. Pain Physician 22 (2019): 323-330.
- Lin CY, Chang CC, Chen YJ, et al. New strategy for minimally invasive endoscopic surgery to treat infectious spondylodiscitis in the thoracolumbar spine. Pain Physician 22 (2019): 281-293.
