Psychosocial Impact of COVID-19 Lockdown on Mental Wellbeing among 11 States of India: A Markov Modeling Approach
Article Information
Vishwak Reddy V1, Satya Revanth Karri2, Tabitha Jezreel2, Shadaan Afeen2, Praveen Khairkar3,*
1Assistant Professor, Department of Psychiatry, Kamineni Institute of Medical Sciences, Narketpally, State of Telangana, India
2Postgraduate, Department of Psychiatry, Kamineni Institute of Medical Sciences, Narketpally, State of Telangana, India
3Professor, Department of Psychiatry, Kamineni Institute of Medical Sciences, Narketpally, State of Telangana, India
*Corresponding Author: Dr. Praveen Khairkar, MD. Professor and Head, Department of Psychiatry, KIMS, Narketpally, Telangana State, India
Received: 10 July 2020; Accepted: 16 July 2020; Published: 29 July 2020
Citation: Vishwak Reddy V, Satya Revanth Karri, Tabitha Jezreel, Shadaan Afeen, Praveen Khairkar. Psychosocial Impact of COVID-19 Lockdown on Mental Wellbeing among 11 States of India: A Markov Modeling Approach. Journal of Psychiatry and Psychiatric Disorders 4 (2020): 158-174.
Share at FacebookAbstract
Objectives: Amid unprecedented health and socioeconomic crisis emanating from COVID-19 pandemic lockdown in India with effect from 25th March 2020 extending into its fourth phase is a matter of great concern to mental health professionals. The present study aims to evaluate psychological impact during current pandemic in difficult to reach, autonomous process of community spread of COVID-19 in partially observable system using respondent driven system with hidden Markov modeling approach.
Methods: The participants were asked to complete a demographic and clinical profile data form, psychological and behavioral changes in past 14 days, their stress levels, depression and anxiety was screened using standardized and validated DASS-21 Scale. Chi-square test, Mann Whitney U test and Pearson’s Correlation Coefficient was performed.
Results: A total of 891 people responded from 11 different states across the country and majority (90%) of them were from five South Indian states. We observed the prevalence of 22% of depression, with 15% anxiety and 27.5% with either of them. Young age, widow/unmarried marital status, moderate level of education, students, non-working status during lockdown, past history of psychiatric illnesses, presence of physical symptoms related to COVID-19, hypochondriacal thoughts, fear of contamination, social contagion, were found to be significantly associated (p<0.05) with reference to presence and/or severity of depression and anxiety.
Conclusion: Markov Modeling using respondent driven sampling is a innovative way of sampling method which can be used in difficult to reach out population in changing dynamic system. Findings of high prevalence of psychopathologies warrants appropriate planning and timely designing an intervention in coordination with mental health professionals to flatten curve in due course of time.
Keywords
COVID-19; Pandemic; Mental health; Markov Modeling Approach
COVID-19 articles, Pandemic articles, Mental health articles, Markov Modeling Approach articles
COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Pandemic articles Pandemic Research articles Pandemic review articles Pandemic PubMed articles Pandemic PubMed Central articles Pandemic 2023 articles Pandemic 2024 articles Pandemic Scopus articles Pandemic impact factor journals Pandemic Scopus journals Pandemic PubMed journals Pandemic medical journals Pandemic free journals Pandemic best journals Pandemic top journals Pandemic free medical journals Pandemic famous journals Pandemic Google Scholar indexed journals Mental health articles Mental health Research articles Mental health review articles Mental health PubMed articles Mental health PubMed Central articles Mental health 2023 articles Mental health 2024 articles Mental health Scopus articles Mental health impact factor journals Mental health Scopus journals Mental health PubMed journals Mental health medical journals Mental health free journals Mental health best journals Mental health top journals Mental health free medical journals Mental health famous journals Mental health Google Scholar indexed journals Modeling Approach articles Modeling Approach Research articles Modeling Approach review articles Modeling Approach PubMed articles Modeling Approach PubMed Central articles Modeling Approach 2023 articles Modeling Approach 2024 articles Modeling Approach Scopus articles Modeling Approach impact factor journals Modeling Approach Scopus journals Modeling Approach PubMed journals Modeling Approach medical journals Modeling Approach free journals Modeling Approach best journals Modeling Approach top journals Modeling Approach free medical journals Modeling Approach famous journals Modeling Approach Google Scholar indexed journals Markov articles Markov Research articles Markov review articles Markov PubMed articles Markov PubMed Central articles Markov 2023 articles Markov 2024 articles Markov Scopus articles Markov impact factor journals Markov Scopus journals Markov PubMed journals Markov medical journals Markov free journals Markov best journals Markov top journals Markov free medical journals Markov famous journals Markov Google Scholar indexed journals Mental health articles Mental health Research articles Mental health review articles Mental health PubMed articles Mental health PubMed Central articles Mental health 2023 articles Mental health 2024 articles Mental health Scopus articles Mental health impact factor journals Mental health Scopus journals Mental health PubMed journals Mental health medical journals Mental health free journals Mental health best journals Mental health top journals Mental health free medical journals Mental health famous journals Mental health Google Scholar indexed journals respondent-driven sampling articles respondent-driven sampling Research articles respondent-driven sampling review articles respondent-driven sampling PubMed articles respondent-driven sampling PubMed Central articles respondent-driven sampling 2023 articles respondent-driven sampling 2024 articles respondent-driven sampling Scopus articles respondent-driven sampling impact factor journals respondent-driven sampling Scopus journals respondent-driven sampling PubMed journals respondent-driven sampling medical journals respondent-driven sampling free journals respondent-driven sampling best journals respondent-driven sampling top journals respondent-driven sampling free medical journals respondent-driven sampling famous journals respondent-driven sampling Google Scholar indexed journals psychiatric illness articles psychiatric illness Research articles psychiatric illness review articles psychiatric illness PubMed articles psychiatric illness PubMed Central articles psychiatric illness 2023 articles psychiatric illness 2024 articles psychiatric illness Scopus articles psychiatric illness impact factor journals psychiatric illness Scopus journals psychiatric illness PubMed journals psychiatric illness medical journals psychiatric illness free journals psychiatric illness best journals psychiatric illness top journals psychiatric illness free medical journals psychiatric illness famous journals psychiatric illness Google Scholar indexed journals mortality rate articles mortality rate Research articles mortality rate review articles mortality rate PubMed articles mortality rate PubMed Central articles mortality rate 2023 articles mortality rate 2024 articles mortality rate Scopus articles mortality rate impact factor journals mortality rate Scopus journals mortality rate PubMed journals mortality rate medical journals mortality rate free journals mortality rate best journals mortality rate top journals mortality rate free medical journals mortality rate famous journals mortality rate Google Scholar indexed journals non-probability sampling articles non-probability sampling Research articles non-probability sampling review articles non-probability sampling PubMed articles non-probability sampling PubMed Central articles non-probability sampling 2023 articles non-probability sampling 2024 articles non-probability sampling Scopus articles non-probability sampling impact factor journals non-probability sampling Scopus journals non-probability sampling PubMed journals non-probability sampling medical journals non-probability sampling free journals non-probability sampling best journals non-probability sampling top journals non-probability sampling free medical journals non-probability sampling famous journals non-probability sampling Google Scholar indexed journals
Article Details
1. Introduction
COVID-19 (Corona Virus Disease-2019) is a global public health emergency declared to be pandemic by World Health Organization (WHO) in March 2020 posing enormous health, economic and social challenges to the entire human population [1, 2]. Like many other countries, a complete lockdown is announced in India with effect from 25th March 2020 [3]. The total number of cases reported worldwide as of June 17th, 2020 is 8,264,468 whereas India’s total Covid-19 tally is at 354,161 with a death toll of 11,921 [4]. Due to the limited knowledge about its proper treatment and unavailability of vaccine so far the COVID-19 continues to haunt every individual’s life, thus having direct or indirect impact on everyone’s mental health. The updates about the new corona virus nevertheless, is increasing daily and more data on its route of transmission, reservoirs, incubation period, symptoms, and clinical outcomes, including survival rates, are getting surmounted around the world [5]. Despite the tremendous advancement of medical sciences, healthcare technology, almost all the nations are struggling to slow down the transmission of the disease and flatten its curve by testing and treating positive patients, quarantining suspected persons through contact tracing, restricting large gatherings, maintaining complete or partial lock down which definitely thwarts the psychological resilience of the public [6]. The on-going COVID-19 lockdown in India for more than 12 weeks now is inducing fear and constant worry compelling us to drastically make changes in our normative way of life resulting in catastrophic effects on self, family and health of the community. Such situation implicitly reflects the diathesis for proximate bio-psychosocial risk factors for depression and anxiety including relatively higher mortality rate [7]. Community is witnessing social insecurity as the community spread of roaming untested or untreated individuals are on high [8] and to add to scenario there are reports that even some families discriminate among their members if they are inflicted to infection and died due to COVID-19, these are apparent predisposing/precipitating adverse mental health in Indian community currently happening during these epidemics.
Previous research has revealed psychosocial impacts on people at the individual, and community levels during outbreaks of infection like SARS [9] but comparatively at a lower scale than ongoing COVID-19. So far about six published studies highlighting mental health during the COVID-19 pandemic showed variable sufferings ranging from as high as 45% anxiety [10], 37% depression [11], 32% with stress [12] and as low as 8% anxiety and 15% depression [13]. Only Indian study [14] was published about mental health issues in community but unfortunately study was conducted just before the massive lockdown hence not capturing the impact of psychosocial forfeiture. All the rest of six studies which have used electronic database for collecting the information and apart from an isolated Indian study [14] which used snowball sampling method for analysis, other studies did not mention their sampling techniques adequately. However, snowball sampling although useful in difficult to reach out groups, is a non-probability sampling analysis from which generalizability cannot be ascertained. The respondent-driven sampling (RDS) is a better evidence based design using Markov modeling [15] which can overcome the inherent measurement biases. Indeed in probability theory, 4 types of Markov models can be used to explain randomly changing systems as happening in COVID-19 pandemic. The construct of Markov model assumes that future states depend only on the current state, not on the events that occurred before and has been effectively used [16] for assessing the impact of health and economic domains of interventions in infectious diseases before. The present study aims to evaluate psychological impact during current pandemic in difficult to reach, autonomous process of community spread of COVID-19 in partially observable system from India using RDS with hidden Markov modeling approach.
2. Materials and Methods
2.1 Setting and participants
After having received ethical approval from our Institutional Ethical Committee, we adopted a cross-sectional, respondent-driven sampling (RDS) method using Markov modeling for recruiting the hard-to-reach populations living throughout almost all the states of India using an online, anonymous survey questionnaire, containing 67 questions. It was first disseminated to 19,660 hospital staff, medical students, central and state government employee(s), various institutional friends, groups of researchers and colleagues of all the religious groups across 25 possible states of the country with effect from 1st April to 12th May 2020 for almost 6 weeks through electronic platform. The hidden Markov modeling (Figure 3) is used like a variant of a link-tracing network sampling method to collect data from such hard-to-reach population scenario. Thus by tracing the links in the underlying social network, the process exploits the social structure to expand the sample and reduce its dependence on the initial convenience sample and treat the data as a probability sample vis-vis a against snowball type of non-probability sampling. All respondents were provided with informed consent. Minimum age required to participate in the study survey was 16 years. Meantime for the completion of the questionnaire was about 10 to 12 minutes. A single reminder was sent to all the recipient and an opt-out option was also incorporated. The confidentiality of the information was strictly maintained.
2.2 Survey development
Previous surveys on the psychological impacts of pandemics were reviewed and authors incorporated additional questions related to the COVID-19 outbreak in relation to the following domains: (1) socio-demographic data; (2) history of medical & psychiatric illnesses; (3) physical symptoms & behaviour changes in the past 14 days; (4) knowledge and source of information about COVID-19; (5) precautionary measures against COVID-19; (6) view on uncertainties; (7) mental health status.
Mental health status was analyzed using the standardized Depression, Anxiety and Stress Scale (DASS-21). It is 21-item questionnaire developed by Lovibond and his colleagues [17]. Questions 3, 5, 10, 13, 16, 17 and 21 formed the depression subscale, while questions 2, 4, 7, 9, 15, 19, and 20 formed the anxiety subscale and questions 1, 6, 8, 11, 12, 14, and 18 formed the stress subscale. The DASS has been demonstrated to be a reliable (Cronbach’s Coefficient: 0.761 to 0.906) [18] and valid measure in assessing mental health in the many previously conducted studies [12, 19]
2.3 Statistical analysis
All the data was computed using SPSS Statistic 26.0 (IBM SPSS Statistics, New York, United States). Quantitative samples are standardized using one-sample Kolmogorov-Smirnov test (figure 2). Kolmogorov-Smirnov normality test compares the observed versus expected cumulative frequencies as we received the responses in 3 different waves. Since the hidden Markov Modeling for partially unobservable autonomous process/system was done, we maintained the matrix of observed values and further used appropriate parametric and nonparametric tests like Chi-square test, Mann-Whitney U-test for quantitative nominal and ordinal group data comparisons respectively. Pearson product-moment correlation coefficient was used to analyze the strength of associations between different clinical and psychosocial variables. A p value less than 0.05 were considered to be significant for all the tests.
3. Results
3.1 Development of COVID-19 in India and survey respondents
Although we contacted about 20,000 individuals from our side, only 891 had responded in 3 waves for complete and voluntarily response. There were following number of responses mainly from states of Telangana (572), Andhra Pradesh (136), Karnataka (55), Kerala (12), Tamil Nadu (21), Maharashtra (34), Gujarat (07), West Bengal (14), Uttar Pradesh (12), Delhi (17) and Punjab (11).
(Figure 1) shows the phase-wise development trend of the COVID-19 in India during initial period of lockdown, whereas 1st case in India being reported on 30th January 2020 but complete lockdown was announced from 25th March 2020 [3]. This survey was conducted from 1st April to 12th May 2020 during which period COVID-19 cases in India increased from 2059 to 72719 (about 36 times ). Number of death due to COVID-19 was only 58 till 1st April, but by 12th May it increased to 2369 (40 times) [4].
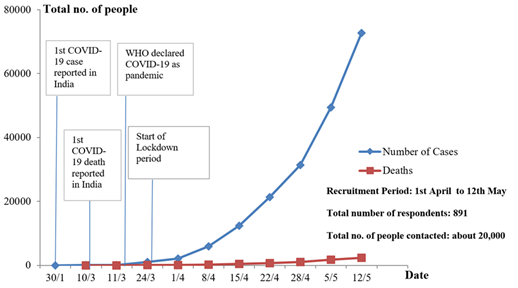
Figure 1: Chronological developmental phases of COVID-19 lockdown in India during our recruitment stage.
3.2 Socio-demographic profile
As seen from (Table 1), out of 891 respondents, most of them were in the age group of 21-40 years (589, 66%), males (477, 53%), Hindu by religion (811, 91%), married and/or living with spouse (432, 49%) and hailing from city (530, 59%). Overall, 200 (22%) of them were screened to be having depression, 138 (15%) had anxiety and 93 (10%) had significant stress based on DASS-21 scores. Age group of 16-20 years was significantly associated with depression (χ2=14.139, p=0.003) and stress (χ2=16.788, p=0.001) compared to other age groups. Unmarried and widow/divorcee marital status had more significant depression (χ2=18.922, p=0.000), anxiety (χ2=6.771, p=0.034) and stress (χ2 =14.694, p=0.001) compared to married group. Degree study group had significant high depression (χ2=7.359, p=0.025) and stress (χ2=6.771, p=0.034) compared to other study groups. Students had significant high depression (χ2=13.043, p=0.005) compared to the people with different occupations. Individuals who were not working during lockdown had significant high stress (χ2=8.429, p=0.015) compared to people who were working. Other socio-demographic variables like gender, religion, place of residence and socio-economic status, were not significantly associated with depression, anxiety, or stress on DASS-21 scores (p value >0.05). As seen in (Figure 2) using Kolmogirov-Smirnov test, a mean of 4.8 out of 1 to 10 likert scale was reported impact affected during this pandemic lockdown.
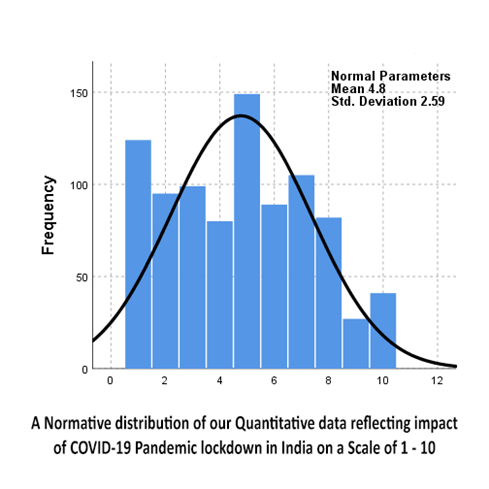
Figure 2: One-sample Kolmogorov-Smirnov normal test.
Table 1: Socio-demographic profile.
3.3 Health status and physical symptoms in past 14 days
Among 891 respondents, 404 (45%) members reports the presence of either children or elderly with medical ailments in the family, 88 (10%) of them had one or other chronic medical illnesses and 25 (3%) of them were pregnant or breast feeding female, but none of the above have shown any significant association with depression, anxiety, or stress (p value > 0.05). Individuals 106 (12%) with past history of psychiatric illness showed significantly higher depression (χ2=42, 244, p=0.000), anxiety (χ2=28.248, p=0.000) and stress (χ2=36.849, p=0.000) compared to those without psychiatric illness. 61(7%) individuals had presence of symptoms related to COVID-19 and they showed significantly higher depression (χ2=10.741,p=0.001), anxiety (χ2=28.471, p=0.000) and stress (χ2=14.030, p=0.000) (Table 2).
Table 2: Health status and physical symptoms in past 14 days.
3.4 Behavioral changes in past 14 days and preventive practices
Number and percentage of individuals with behavioral changes in past 14 days, like hypochondriacal thoughts of COVID-19 symptoms, excessive fear of contamination & contracting COVID-19, social contagion, restrict watching COVID-19 updates & information, psychological distress due to unavailability of alcohol are tabulated . Among all the five domains, hypochondriacal thoughts showed highest significance with depression (Z=-4.528, p=0.000) and stress (Z=-6.606, p=0.000) compared to other domains. Excessive fear of contamination & contracting COVID-19 showed highest significance with anxiety (Z=-6.481, p=0.000) (Table 3).
Table 3: Behavioral changes in past 14 days.
As far as preventive practices were concerns, 648 (72%) were completely satisfied with preventive/safety practices while only 61 (7%) showed irritation with supervising public authorities; 410 (46%) of them were very frequently worried of their future career or job related uncertainties 516 (58%) and almost similar figure of 399 (45%) were worried of their financial security. These later two groups showed significant association with psychological sufferings as depicted in (Table 4). However, 516 (58%) of our sample though spent complete day at home during lockdown did not show any significance with depression, anxiety and stress reflecting the fabric of family comfort.
Table 4: Preventive practices and concerns on uncertainties.
Table 5: Correlation analysis between different variables with presence and severity of depression, anxiety and stress on DASS-21 scale scores.
3.5 Correlation analysis
Pearson’s product-moment correlation(r) of sample was used to measure the strength of association as shown in (Table 5). We observed that age had significant negative correlation (r= -0.120**, p=0.000 for depression, r= -0.076**, p=0.023 for anxiety and r= -0.129, p=0.000 for stress) while hypochondriacal thoughts of COVID-19 symptoms and social contagion had significant (r=0.201**, p=0.000) positive correlation with presence and severity of depression, anxiety & stress. Among these, past history of psychiatric illnesses had highest positive correlation with presence (r=0.218**, p=0.000) and severity (r=0.279**, p=0.000) of depression as well as with presence and severity (r=0.251**, p=0.000) of anxiety.
4. Discussion
World has experienced many pandemics previously, but current global impact of COVID-19 has been clearly profound, and the public health threat due to this is the most serious seen since the 1918 H1N1 influenza pandemic [20]. Except one study [14], there is limited information available in the literature pertaining to the psychological impacts of such pandemics especially in a country like India. The present study rapidly assessed mental health status of representatives from 11 states of India using Markov Modeling when reaching the population during COVID-19 has been difficult. The present study successfully used hidden Markov modeling of the peer recruitment process when system is only partially observable and our study has showed that in contrary to the conventional wisdom, bias from the usual convenience sample of initial subjects could be progressively attenuated [21] as the sample expanded wave by wave over a period of 6 weeks of analysis. This model employed data from peer recruitments to estimate the probability of recruitment across groups. These probabilities were organized into a recruitment matrix, specifying the probability of members of each group (e.g., Hindu contacted mostly by investigator VR, PK and RK, Muslim contacted by SA, Christens by TZ, and Buddhist by PK), and therefore we assume that these probabilities could be served as the “transition probabilities” of the hidden Markov model (Figure 3) making it possible to be more representative of the Indian population.
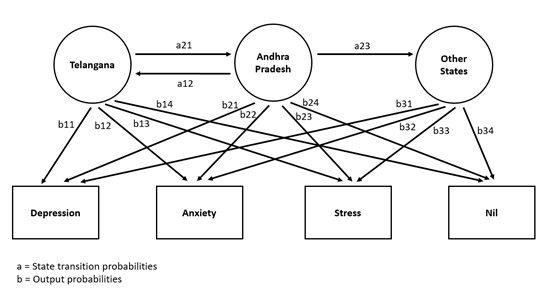
Figure 3: Probabilistic parameters of hidden Markov Modeling in our Response Driven Sampling from 11 States of India.
Indeed, this model also enables us to partially overcome bias related to sample size if the initial sample is nonrandom, and if the number of waves which we assume reaches a threshold value large enough to eliminate bias from the initial selection making the results generalizable for the representative population.
In our present study among 891 responses, depression was found in 22%, anxiety in 15% and stress in 10% individuals and 27.5% with either of them. Studies done in China, Italy and Turkey during COVID-19 reported higher rates compared to India except one from China [13]. Among socio-demographic predictors, our study found that young age group (16-20 years) had higher rates of depression, anxiety & stress compared to other age groups. Similar findings were reported by other studies [11, 13]. Although fatality rate is high in older people, young people are at more risk of psychological maladjustment. Lack of experience in handling crisis situations, excessive usage of social media as well as inherent restlessness induced by being housebound, can possibly contribute to the significant high rates in this age group. Most of the young age group were represented by students and they are certainly more vulnerable as there could be more worries regarding uncertainties of opening of colleges, scheduling and rescheduling of competitive exams, marked on-going delay in academic progress, adjustment issues with online module of teaching, restlessness created by being housebound, and lastly helplessly being away from peer groups and/or gatherings for such a prolonged period of time. We did not find any significant association in other socio-demographic parameters (Table 1), interestingly most of the studies [10, 12, 13, 19] reported significant higher rates in female gender, however uniquely to their contrary, we could not find any significant differences (Table 1). In our study, Widow/Divorcee and/or unmarried marital status had significantly more depression, anxiety & stress compared to married ones and our findings are in conformation with those again by [13]. Further, we observed that graduate educated have had significantly more depression and stress compared to higher or lower educational group, which is unique finding of this study, whereas studies by Wang C and Mazza C [12, 19] reported uneducated had comparatively more depression. The acquisition of knowledge on many things (information & uncertainties of COVID-19) but not as comprehensively as highly educated people might provoke more depression and build up stress rather than not being totally aware as observed in people with low education.
One of the fascinating contradictory findings in our study was that presence of chronic medical ailments did not show any significant correlation with neither of depression, anxiety or stress uniquely compared to other previous studies [10. 12. 19] from other countries which clearly showed significant positive association of medical co-morbidity with depression, anxiety as well as stress. China and Italy being initially affected countries and reported high fatality rates (Fatality rates: Italy 14.4%, China 5.5%) compared to fatality rate in India (Fatality rate 2.8%) [22] could be one reason of less perception of danger in Indian population. Moreover, health is usually given less priority in Indian context compared to other factors, so usually most of the people with medical ailments feel no difference with other individuals. To our surprise 106 (12%) reported to be having history of psychiatric illnesses. Generally people are sceptical about revealing psychiatric problems here in India with lack of openness in general population mainly due to social stigma prevailing over mental illness, but may be this time due to panic created by COVID-19 might have broken the walls of stigma related to social psychiatry. Individuals with history of psychiatric illnesses were found to be having significantly high depression, anxiety & stress compared to other individuals as expected. It has been reported in many studies that symptomology could aggravate in individuals with mental illnesses in situations like disasters, pandemics with lot of uncertainties [23, 24, 25] and secondly, unavailability of most of the psychiatric services during lockdown might contribute for more reported rates. Only one study [10] evaluated from the perspective of presence of psychiatric illness in relation with COVID-19 and reported similar finding of the present study. Presence of one or more symptoms related COVID-19 in the past 14 days had significantly high depression, anxiety & stress (Table 2), like the findings of Wang et al., 2020 [12]. It is obvious that with the fear of presence of COVID-19 symptoms, individual may have lot of concerns, especially regarding testing process, embarrassing isolation and treatment outcome uncertainties, possible spread to family members, could compound in increased scores for depression and anxiety. Indian authorities too are installing a great number of helplines and encouraging more discussion on media by medical experts regarding clarification of symptoms, proper guidance in overcoming distress regarding symptoms of COVID-19.
In our present study, 72% of patients were completely satisfied initially with lockdown compared to free normal days and awareness of one’s own precautionary measures and only 7% were irritable or angry on the stringency of measures on so called responsive behaviour by public during lockdown reflecting community cooperation for harmonious acceptance of national lockdown decision. It is self-evident that hypochondriacal thoughts, excessive fear of contamination about contracting COVID-19, related social contagion, restricting oneself for prolonged watching COVID-19 updates, psychological distress due to unavailability of alcohol due to lockdown, response on personal & public preventive practices, worries of future career, occupational uncertainties and financial insecurity during lockdown are inherent processes which predicts and perhaps reflects the presence of underlying innate response to stress, as well as on-going anxiety and depression processes. Surprisingly in the present study almost all the above hypothesized predictors had shown significant correlation with higher rates of depression, anxiety, and stress (Tables 3 and 4).
On Pearson’s correlational coefficient a significant negative correlation with age but not with gender as contrary with the study by Ozdin et al., 2020 and Wang et al., 2020 [10, 12] is noteworthy finding. Similarly, the conventional understanding of vulnerable predisposed groups like those suffering with chronic medical illnesses have not necessarily shown to be more vulnerable for anxiety, depression, and stress (Table 5). This is in stark contradiction and unexpected, as biological inflammation has proven to be associated with higher fatality rate in COVID-19 outcome; not reporting underlying anxiety or depression is either a reflection of psychological denial or poor anticipation of untoward consequences. However, many individuals of our study are performing daily meditation and relaxation practices which helped them to live in present rather than imagining the negative outcome and therefore could be a positive predictor for comparative lesser mortality in India. So, in general population, the above predictors can act as warning signs of hidden negative and positive mental health issues. Since COVID-19 crisis is still on continuum, there is urgent need to address and highlight these predictor(s) via media, health care workers and plan appropriate direct or indirect online intervention(s) from health care system in coordination with mental health professionals, to accept the reality, help and reassure each other, improve our savings and work collectively to overcome this COVID-19 crisis hopefully.
5. Limitations
This study used respondent driven sampling (RDS) using hidden Markov modeling which has inherent problem of assumption based on probability of wave through which it achieves adequate sample size. However, over 6 weeks, we could only receive 891 responses from people living in almost 11 states spread across India which truly cannot reflect the mental health status of entire country. Further, the study sample included only the people who could use smart phone and are educated, and therefore could not represent more of rural and/or most of less educated people which constitute 65% of India. Another limitation is long, online self-reported levels of depression, anxiety or stress may not always completely be aligned with assessment by mental health professionals.
6. Conclusions
Our study successfully used Hidden Markov modeling in respondent driven sampling as a novel way of approach in partially observable system/process in huge population like India which are difficult to reach like in the on-going COVID-19 pandemic. This pandemic is becoming a part of our life as its past and future are forming uninterrupted continuum in system dynamics. It is indeed a time of rapid learning and likely to create permanent long-term change for our mental health care processes for both sufferers like young age students and emergency health care providers. Appropriate planning and timely designing an intervention on multi-layer services as and when needed for improving life(s) and providing hopes by working in coordination with central and state authorities, media and all voluntary mental health professionals, to invest in our people, reunite and fight this devastating COVID-19 pandemic while waiting for the curve to be flatten in due course of time.
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
Acknowledgment
We are thankful to all the respondents from the country for graciously taking their valuable time out as well as all those who supported for their cordial cooperation to conduct the survey.
References
- Palacios Cruz M, Santos E, Velázquez Cervantes M, et al. COVID-19, a worldwide public health emergency. Revista Clínica Española (English Edition) (2020): 1-7.
- Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ 368 (2020): m408.
- Gettleman J, Schultz K. Modi Orders 3-Week Total Lockdown for 1.3 Billion Indians. The New York Times. (24 March 2020) ISSN 0362-4331.
- WHO Coronavirus Disease (COVID-19) Dashboard. Covid19.who.int. (2020). https://covid19.who.int/.
- Corman V, Landt O, Kaiser, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 25 (2020): 1-8.
- Chakraborty I, Maity P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Science of The Total Environment 728 (2020): 1-7.
- Xiang Y, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry 7 (2020): 228-229.
- Brooks S, Webster R, Smith L, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet 395 (2020): 912-920.
- Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). Journal of Traumatic Stress 18 (2005): 39-42.
- Özdin S, Bayrak Özdin ?. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry (2020): 1-8.
- Ahmed M, Ahmed O, Aibao Z, et al. Epidemic of COVID-19 in China and associated Psychological Problems. Asian Journal of Psychiatry 51 (2020): 1-7.
- Wang C, Pan R, Wan X, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. International Journal Of Environmental Research And Public Health17 (2020): 1-25.
- Lei L, Huang X, Zhang S, et al. Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by versus People Unaffected by Quarantine During the COVID-19 Epidemic in Southwestern China. Medical Science Monitor 26 (2020): 1-12.
- Roy D, Tripathy S, Kar S, et al. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry 51 (2020): 1-8.
- Volz E, Heckathorn Douglas D. Probability-Based Estimation Theory for Respondent Driven Sampling. Journal of Official Statistics 24 (2008): 79-97.
- Haeussler K, Hout AVD, Baio A Dynamic Bayesian Markov Model for Health Economic Evaluations of Interventions in Infectious Disease. BMC Med Res Methodol 18 (2018): 82.
- Lovibond LF, Lovibond The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy 33 (1995): 335-343.
- Le M, Tran T, Holton S, et al. Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PLOS ONE 12 (2017): 1-14.
- Mazza C, Ricci E, Biondi S, et al. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. International Journal of Environmental Research and Public Health17 (2020): 1-14.
- Kar SK, Yasir Arafat SM, Kabir R, et al. Coping with Mental Health Challenges During COVID-19. Coronavirus Disease 2019 (COVID-19): Epidemiology, Pathogenesis, Diagnosis, and Therapeutics (2020): 199-213.
- Heckathorn, D. Snowball versus Respondent driven Sampling. Sociol Methodol 41 (2011): 355-366.
- European Centre for Disease Prevention and Control (ECDC). GitHub (2020).
- Chatterjee S, Barikar CM, Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian Journal Of Psychiatry 51 (2020): 1-2.
- Goldmann E, Galea S. Mental Health Consequences of Disasters. Annual Review of Public Health35 (2014): 169-183.
- Hao F, Tan W, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain, Behavior, and Immunity 87 (2020): 100-106.
