Psychological Features in a Family affected by Hypermobile Ehlers- Danlos Syndrome (hEDS)
Article Information
Caroline de Percin1, Malika Foy1, Karelle Benistan1,2*
1AP-HP, Hôpital Raymond Poincaré, Centre de référence des Syndromes d’Ehlers-Danlos non-vasculaires, Garches, France
2INSERM U1179, Université Versailles Saint-Quentin-en-Yvelines, Montigny-le-Bretonneux, France
*Corresponding Author: Dr Karelle Benistan, Centre de référence des Syndromes d’Ehlers-Danlos non-vasculaires, Hôpital Raymond Poincaré, 92380 Garches, France
Received: 01 July 2021; Accepted: 19 July 2021; Published: 22 December 2021
Citation: Caroline de Percin, Malika Foy, Karelle Benistan. Psychological Features in a Family affected by Hypermobile Ehlers- Danlos Syndrome (hEDS). Journal of Psychiatry and Psychiatric Disorders 5 (2021): 196-202.
Share at FacebookAbstract
Hypermobile Ehlers-Danlos Syndrome (hEDS) is a genetic disease that is hard to diagnose. The diagnosis relies solely on clinical features due to the lack of a diagnostic test. It is characterized by a high level of pain and fatigue, as well as instability of the body, affecting the quality of life. The variability and the invisibility of the symptoms have an impact on the psychological well-being and behaviour of the patients, and make the situation difficult to understand by their relatives. We report here the case of several family members affected by hEDS, showing psychological symptoms often found in hEDS patients. Adopting a multidisciplinary approach, both physical and psychological, is decisive to more efficient medical and global care.
Keywords
Hypermobile Ehlers-Danlos Syndrome; Psychological features; Chronic pain; Chronic fatigue; Behaviour; Hereditary disease
Hypermobile Ehlers-Danlos Syndrome articles; Psychological features articles; Chronic pain articles; Chronic fatigue articles; Behaviour articles; Hereditary disease articles
Hypermobile Ehlers-Danlos Syndrome articles Hypermobile Ehlers-Danlos Syndrome Research articles Hypermobile Ehlers-Danlos Syndrome review articles Hypermobile Ehlers-Danlos Syndrome PubMed articles Hypermobile Ehlers-Danlos Syndrome PubMed Central articles Hypermobile Ehlers-Danlos Syndrome 2023 articles Hypermobile Ehlers-Danlos Syndrome 2024 articles Hypermobile Ehlers-Danlos Syndrome Scopus articles Hypermobile Ehlers-Danlos Syndrome impact factor journals Hypermobile Ehlers-Danlos Syndrome Scopus journals Hypermobile Ehlers-Danlos Syndrome PubMed journals Hypermobile Ehlers-Danlos Syndrome medical journals Hypermobile Ehlers-Danlos Syndrome free journals Hypermobile Ehlers-Danlos Syndrome best journals Hypermobile Ehlers-Danlos Syndrome top journals Hypermobile Ehlers-Danlos Syndrome free medical journals Hypermobile Ehlers-Danlos Syndrome famous journals Hypermobile Ehlers-Danlos Syndrome Google Scholar indexed journals Psychological features articles Psychological features Research articles Psychological features review articles Psychological features PubMed articles Psychological features PubMed Central articles Psychological features 2023 articles Psychological features 2024 articles Psychological features Scopus articles Psychological features impact factor journals Psychological features Scopus journals Psychological features PubMed journals Psychological features medical journals Psychological features free journals Psychological features best journals Psychological features top journals Psychological features free medical journals Psychological features famous journals Psychological features Google Scholar indexed journals Chronic pain articles Chronic pain Research articles Chronic pain review articles Chronic pain PubMed articles Chronic pain PubMed Central articles Chronic pain 2023 articles Chronic pain 2024 articles Chronic pain Scopus articles Chronic pain impact factor journals Chronic pain Scopus journals Chronic pain PubMed journals Chronic pain medical journals Chronic pain free journals Chronic pain best journals Chronic pain top journals Chronic pain free medical journals Chronic pain famous journals Chronic pain Google Scholar indexed journals Chronic fatigue articles Chronic fatigue Research articles Chronic fatigue review articles Chronic fatigue PubMed articles Chronic fatigue PubMed Central articles Chronic fatigue 2023 articles Chronic fatigue 2024 articles Chronic fatigue Scopus articles Chronic fatigue impact factor journals Chronic fatigue Scopus journals Chronic fatigue PubMed journals Chronic fatigue medical journals Chronic fatigue free journals Chronic fatigue best journals Chronic fatigue top journals Chronic fatigue free medical journals Chronic fatigue famous journals Chronic fatigue Google Scholar indexed journals Behaviour articles Behaviour Research articles Behaviour review articles Behaviour PubMed articles Behaviour PubMed Central articles Behaviour 2023 articles Behaviour 2024 articles Behaviour Scopus articles Behaviour impact factor journals Behaviour Scopus journals Behaviour PubMed journals Behaviour medical journals Behaviour free journals Behaviour best journals Behaviour top journals Behaviour free medical journals Behaviour famous journals Behaviour Google Scholar indexed journals Hereditary disease articles Hereditary disease Research articles Hereditary disease review articles Hereditary disease PubMed articles Hereditary disease PubMed Central articles Hereditary disease 2023 articles Hereditary disease 2024 articles Hereditary disease Scopus articles Hereditary disease impact factor journals Hereditary disease Scopus journals Hereditary disease PubMed journals Hereditary disease medical journals Hereditary disease free journals Hereditary disease best journals Hereditary disease top journals Hereditary disease free medical journals Hereditary disease famous journals Hereditary disease Google Scholar indexed journals Ehlers-Danlos Syndromes articles Ehlers-Danlos Syndromes Research articles Ehlers-Danlos Syndromes review articles Ehlers-Danlos Syndromes PubMed articles Ehlers-Danlos Syndromes PubMed Central articles Ehlers-Danlos Syndromes 2023 articles Ehlers-Danlos Syndromes 2024 articles Ehlers-Danlos Syndromes Scopus articles Ehlers-Danlos Syndromes impact factor journals Ehlers-Danlos Syndromes Scopus journals Ehlers-Danlos Syndromes PubMed journals Ehlers-Danlos Syndromes medical journals Ehlers-Danlos Syndromes free journals Ehlers-Danlos Syndromes best journals Ehlers-Danlos Syndromes top journals Ehlers-Danlos Syndromes free medical journals Ehlers-Danlos Syndromes famous journals Ehlers-Danlos Syndromes Google Scholar indexed journals hyperalgesia articles hyperalgesia Research articles hyperalgesia review articles hyperalgesia PubMed articles hyperalgesia PubMed Central articles hyperalgesia 2023 articles hyperalgesia 2024 articles hyperalgesia Scopus articles hyperalgesia impact factor journals hyperalgesia Scopus journals hyperalgesia PubMed journals hyperalgesia medical journals hyperalgesia free journals hyperalgesia best journals hyperalgesia top journals hyperalgesia free medical journals hyperalgesia famous journals hyperalgesia Google Scholar indexed journals psychological articles psychological Research articles psychological review articles psychological PubMed articles psychological PubMed Central articles psychological 2023 articles psychological 2024 articles psychological Scopus articles psychological impact factor journals psychological Scopus journals psychological PubMed journals psychological medical journals psychological free journals psychological best journals psychological top journals psychological free medical journals psychological famous journals psychological Google Scholar indexed journals Ehlers-Danlos Syndromes articles Ehlers-Danlos Syndromes Research articles Ehlers-Danlos Syndromes review articles Ehlers-Danlos Syndromes PubMed articles Ehlers-Danlos Syndromes PubMed Central articles Ehlers-Danlos Syndromes 2023 articles Ehlers-Danlos Syndromes 2024 articles Ehlers-Danlos Syndromes Scopus articles Ehlers-Danlos Syndromes impact factor journals Ehlers-Danlos Syndromes Scopus journals Ehlers-Danlos Syndromes PubMed journals Ehlers-Danlos Syndromes medical journals Ehlers-Danlos Syndromes free journals Ehlers-Danlos Syndromes best journals Ehlers-Danlos Syndromes top journals Ehlers-Danlos Syndromes free medical journals Ehlers-Danlos Syndromes famous journals Ehlers-Danlos Syndromes Google Scholar indexed journals
Article Details
1. Introduction
Ehlers-Danlos Syndromes (EDS) are a heterogeneous group of hereditary connective tissue disorders characterized by joint hypermobility, skin laxity and tissue fragility. Their prevalence is estimated at 1/5000. The 2017 International Classification of the EDS defines 13 subtypes, due to gene mutations encoding connective tissue structural proteins or enzymes involved in their metabolism [1].
Hypermobile EDS, the most frequent type (more than 80% of patients with EDS), is defined by diagnostic criteria [1]. Genetic transmission most often has an autosomal dominant pattern. The diagnosis relies solely on clinical features due to the lack of a diagnostic test. The patients show repeated sprains and dislocations which cause functional consequences leading to disabilities. They also suffer from chronic pain and fatigue, affecting their quality of life [2, 3]. Other clinical features are often found in hEDS patients such as pulmonary, abdominal, neuropsychological, cardiac, gynecological or bladder and sphincter-related symptoms [4, 5].
Hypermobile EDS is poorly understood by health professionals, which frequently leads to medical wandering, and alternative diagnosis are frequently initially wrongly made. These situations are especially hard to cope with by the patients because of the misunderstanding they are facing and the impossibility to move forward. The medical wandering, chronic pain and fatigue are known to have psychological consequences [6, 4, 7]. We report here the case of several members of a large family affected by hEDS and showing psychological features arising from the diagnosis’ annoucement, lack of recognition and chronic pain.
2. Patients and Methods
This study related the experience of a doctor and a psychologist’s experience in a non vascular EDS National Reference Center. The doctor and the psychologist see patients with hypermobile EDS every day. The psychologist attended the doctor’s consultation in order to have a precise understanding of the patients’ symptoms and saw the patients afterwards for a diagnostic and therapeutic psychological approach.
3. Results
We received a 44-year-old female (patient II1) in the Non Vascular Ehlers-Danlos Reference Center for a suspicion of hypermobile EDS (hEDS). Her clinical history and her medical examination led to a hEDS diagnosis according to the 2017 International Classification of the Ehlers-Danlos Syndromes [1]. She reported that her siblings, her children and several of her nephews and nieces also displayed symptoms. Consequently, we decided to meet the family members who had suggestive symptoms (Figure 1).
The diagnosis of hEDS was confirmed for three of this patient’s nieces : III5, III7 and III9. However patients III2 and III8 did not meet enough criteria to reach a hEDS diagnosis. Moreover hEDS diagnosis was excluded for patients II3, II5, III1, III3, III6, III10. Patients IV1 and IV2, aged 3 and 6, displayed joint hypermobility and will have to be reevaluated later. Patients I1, I2, II7, III4, and III11 were not examined.
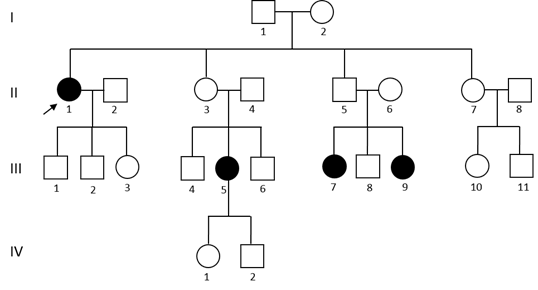
Figure 1: Family pedigree. Circles indicate females, squares indicate males. Symbols in black indicate individuals affected with hEDS. Arrow indicates the proposita. Patients III2 and III8 did not meet enough criteria to reach a hEDS diagnosis. hEDS diagnosis was excluded for patients II3, II5, III1, III3, III6, III10. Patients IV1 and IV2, aged 3 and 6, displayed joint hypermobility. Patients I1, I2, II7, III4, and III11 were not examined.
3.1 The diagnosis’s announcement
Some family members have met the psychologist after their medical consultation. For patients II1, III5, III7 and III9, the diagnosis, with the recognition of their symptoms and a feeling of being understood, came as a relief [8]. The diagnosis allowed them to recognize and deal with their limits. Patient III7 accepted her weaknesses and difficulties to manage her daily life. Interestingly patient II2, who was seen independently of his wife, (patient II1), had a less positive reaction because he suddenly had to give up any hope that the symptoms might lighten or disappear. He also mentioned a fear of the future. Patient II3 had also suffered from chronic pain for a long time. Her hope of getting a hEDS diagnosis was deceived and she tended to show depression symptoms. The impossibility to make a hEDS diagnosis would extend the period of medical wandering, which idea was difficult to bear for her.
3.2 Pain, fatigue and management strategies
Diagnosed patients suffered from chronic pain and fatigue which could vary in intensity depending on multiples factors. They also suffered from a lack of credibility due to the invisibility and variability of the symptoms. They developped very different strategies to deal with their symptoms. Patient III7 showed hyperalgesia (increased sensitivity to pain) and a predisposition toward somatosensory amplification (a tendency to perceive normal somatic and visceral sensations as being relatively intense, disturbing and noxious). Thus, she would have needed to adapt her school hours to her physical condition, which was not accepted by the university staff. This led to the interruption of her studies. Patient III5 had high scores of kinesophobia (apprehension of movement), this factor hindering rehabilitation and actually prolonging disability and pain.
On the other hand, patient III9 spontaneously developped fatigue management strategies, according to its intensity, for example by resting in anticipation of a trip or a planned outing. She noticed that even if she felt fine, she should not exceed a given threshold regarding the intensity of physical activities.
All four diagnosed patients admitted that chronic joint instability and proprioceptive disorders induced a feeling of not being in control of their body and gave them a strong feeling of insecurity and fear. Patient III7 was ashamed of it, which lead to social exclusion. Patients II1 and III7 consequently developed feelings of anger, which did not seem to affect their relatives.
3.3 Relatives’s behavior towards illness
Illness seemed to have a big place in this family, where they all tended to compare their symptoms and diagnosis to each other’s. Family dynamics played an important role on each patient’s disease management. The relatives’ behavior also impacted the way the patients dealt with their illness. For example, patient II1 mentioned that her daughter acknowledged her sufferings only when the disability became visible, which lead to complicated mother-daughter relationships. She then needed a lot of care and attention from her husband, who was her caregiver and very present at home. He tried to not become overprotective, especially since his wife came to be quite demanding and difficult to handle. He admitted it was not always easy and was aware of how important it was that he took time for himself.
Although genetic diseases usually expose relatives to specific feelings of guilt due to the hereditary characteristic of the illness, in this family, patient II5, (father of patients III7 and III9), did not feel guilty for transmitting the disease to his daughters. His daughters were not resentful towards him for transmitting it. His wife (II6) generally tended to prioritize her two sick daughters and to ignore her own needs and limits. She confessed that it could eventually lead to resentment or anger. Patient III9 stressed that her parents’ attention was focused on her sister who was more affected than her and that she felt neglected. She experienced the typical difficulties of having a sick sibling, even though she had been diagnosed with hEDS too. She expressed that her brother developed the same feeling of lack of parental attention.
4. Discussion
Chronic pain and fatigue are the most challenging features of hEDS. The invisibility and variability of the symptoms exacerbates others’ misunderstanding of the disease and contributes to a lack of social support [9]. In the school and work environments, the understanding of the principals and employers can vary highly, as sadly experienced by patient III7. Any deschooling should alert doctors, especially as it is often detrimental to health and wellbeing [10]. In case of abnormal fatigue, health professionals should look for an associated pathology, such as dysautonomia. Therapeutic education is essential to help the patient develop strategies for managing fatigue. When they manage to do so, they substantially improve their management of pain and fatigue in the long term, a situation stressed by patient III9.
Many studies report a high level of anxiety and depression among patients with EDS, independently of age, tiredness and back pain [6]. Current literature mentions a significant association between hEDS and anxiety disorders, and this relationship has been studied for over 30 years; the relationship between hEDS and depression is also increasingly recognized [4].
However among the patients visiting the non-vascular EDS National Reference Center, and in particular in this family, patients such as II3, whose hEDS diagnosis has not been confirmed, tend to show more depression symptoms than patients diagnosed with hEDS. The impossibility of making an hEDS diagnosis for her extended the period of medical wandering. Studies show that anxiety and depression are linked to chronic pain and decreased functionality, independently of the EDS diagnosis [4, 7].
Indeed our experience shows that patients’ psychological difficulties are more related to fatigue and the genetic transmission of the disease than to the diagnosis itself. When the hEDS diagnosis can be confirmed, the patients seem to be less anxious or depressed.
The diagnosis puts the family into a long-term perspective [11]. Most relatives worry about the future of the child or of the sick parent. The illness of their relative confronts some of them to their helplessness which results in specific defense mechanisms. Patients could interpret it as aggress-iveness or indifference. Other relatives become overprotective contrary to the patient’s wish, since the child or relative with hEDS often appreciate it when they are given a chance to be independent.
Genetic transmission of hEDS most often has an autosomal dominant pattern with a theoretical risk of transmission of 50% to each child [1]. Unlike patient II5, most of the parents feel guilty of transmitting the disease to their children, even though they do not feel responsible for it. However, they are never resentful toward their own parents for transmitting it to them. Unlike their own parents, the future parents now know that they have hEDS and that their illness is genetically transmitted. This knowledge accentuates their guilt in having potentially ill children and raises a lot of questions.
The doctor answers their questions and guaranties the child will receive well- adjusted medical care if needed. We notice that sometimes the sick child can feel a special “link” with the sick parent, creating mutual understanding from which the healthy child can feel excluded. This adds to the typical difficulties of having a sick brother and sister, experienced by patients III9 and III8. Their symptoms force patients to modify or restrict their behaviors and activities [9], as for patient III7. The first step for her was to accept what she couldn’t do anymore while being aware of everything she could still do. These remaining abilities were valued and built upon. Once she accepted her limits and capabilities, she was able to accept being helped. Hypermobile EDS is a disease that can lead to disabilities.
Patient II1 had worries regarding the future and particularly the evolution of her physical abilities, especially since she occasionally used a wheelchair. She was aware that consulting a psychologist could help her manage her fears. When the patient apprehend the future more positively, the evolution of the symptoms is in favor of an improvement of his global well-being; he surrounds himself with helpful relatives, feels less excluded, has a better acceptance of his body and of the way others look at him, is more proactive in finding helpful solutions and taking better care of himself.
In conclusion, this family is highly reprensentative of the psychological difficulties hEDS patients, and their families, meet. Hypermobile EDS is a rare genetic disease leading patients through a long period of medical wandering. Patients suffer from chronic pain and fatigue.
The variability of the symptoms makes the situation difficult to understand for relatives, who can have a hard time adopting the right attitude. Taking a multidisciplinary approach, both physical and psychological, is decisive to the long-term efficiency of the care.
Fundings
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declared no conflicts of interest with respect to the authorship or the publication of this article.
References
- Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers– Danlos syndromes. In American Journal of Medical Genetics, Part C: Seminars in Medical Genetics 175 (2017): 8-26.
- Bénistan K, Gillas F. Pain in Ehlers-Danlos syndromes. Joint Bone Spine (2019): 10-12.
- Bénistan K, Martinez V. Pain in hypermobile Ehlers-Danlos syndrome: New insights using new criteria. American Journal of Medical Genetics, Part A 179 (2019): 1226-1234.
- Bulbena A, Baeza-Velasco C, Bulbena-Cabré A, et al. Psychiatric and psychological aspects in the Ehlers–Danlos syndromes. In American Journal of Medical Genetics, Part C: Seminars in Medical Genetics 175 (2017): 237-245.
- Tinkle B, Castori M, Berglund B, et al. Hypermobile Ehlers–Danlos syndrome (a.k.a. Ehlers–Danlos syndrome Type III and Ehlers–Danlos syndrome hypermobility type): Clinical description and natural history. American Journal of Medical Genetics, Part C: Seminars in Medical Genetics 175 (2017): 48-69.
- Berglund B, Pettersson C, Pigg M, et al. Self-reported quality of life, anxiety and depression in individuals with Ehlers-Danlos syndrome (EDS): A questionnaire study. BMC Musculoskeletal Disorders 16 (2015).
- Hershenfeld SA, Wasim S, McNiven V, et al. Psychiatric disorders in Ehlers–Danlos syndrome are frequent, diverse and strongly associated with pain. Rheumatology International 36 (2016): 341-348.
- De Baets S, Vanhalst M, Coussens M, et al. The influence of Ehlers-Danlos syndrome – hypermobility type, on motherhood: A phenomenological, hermeneutical study. Research in Developmental Disabilities 60 (2017): 135-144.
- Terry RH, Palmer ST, Rimes KA, et al. Living with joint hypermobility syndrome: patient experiences of diagnosis, referral and self-care. Family Practice 32 (2015): 354-358.
- Hakim A, De Wandele I, O’Callaghan C, et al. Chronic fatigue in Ehlers–Danlos syndrome—Hypermobile type. American Journal of Medical Genetics, Part C: Seminars in Medical Genetics 175 (2017): 175-180.
- Chaumet H. Penser la maladie génétique, Enjeux psychologiques et perspectives (Paris: L’Harmattan. (ed.)) (2013).
