Review of Nursing Interventions to Reduce the Sodium Intake for Patients with Chronic Heart Failure
Article Information
Qianyi Wang1, Shuhua Shang1, Jinyu Sun2, Guozhen Sun1, 3*, Zejuan Gu3*
1Nanjing Medical University School of Nursing, Nanjing, China
2The First Clinical Medical College of Nanjing Medical University, Nanjing, China
3Department of Cardiology, The First Affiliated Hospital, Nanjing Medical University, Nanjing, China
*Corresponding Author: Guozhen Sun, Nanjing Medical University School of Nursing, Nanjing, China
Received: 07 April 2019; Accepted: 13 April 2019; Published: 17 April 2019
Citation: Qianyi Wang, Shuhua Shang, Jinyu Sun, Guozhen Sun, Zejuan Gu. Review of Nursing Interventions to Reduce the Sodium Intake for Patients with Chronic Heart Failure. Cardiology and Cardiovascular Medicine 3 (2019): 059-075.
Share at FacebookAbstract
This study aimed to systematically evaluate the effect of nursing interventions on reducing dietary sodium intake in patients with chronic heart failure, further to provide insight on the most utilized nursing practices. Only randomized controlled trials on dietary sodium management of nursing interventions were collected from Pubmed, CINAHL, Web of Science, Embase and The Cochrane Library (CENTRAL). Among 515 available studies, a total of 8 ones met the inclusion criteria and were included. The meta-analysis result suggested that nursing interventions could reduce dietary sodium intake in patients with chronic heart failure within 6 months compared with conventional care [SMD (-0.305, 95%CI -0.561, -0.049)]. Considering the sodium levels estimated by the 3-day food record is much lower than those by the 24-hour urinary sodium, it is better to analyze separately to further clarify the effect of nursing interventions. Hence, further meta-analysis results showed that the sodium intake estimated by the 3-day diet record/diary in the experimental group was lower than that in the control group [SMD -0.523, 95%CI (-0.894 to -0.152), P=0.006]. Similarly, the sodium intake in the experimental group was lower than that in the control group by 24-hour urine specimen [WMD -364.318, 95% CI (-603.953 to -124.684), P=0.003]. We concluded that nursing interventions can reduce dietary sodium intake in patients with chronic heart failure in the short term. However, the long-term effects are uncertain, and long-term planned randomized controlled trials in heart failure patients are required to further verify the effect in the future.
Keywords
Heart failure; Nursing; Sodium dietary; Meta-analysis; Systematic review
Article Details
Abbreviations: HF-Heart failure; CHF-Chronic heart failure; HFSA-Heart Failure Society of America; ESC-European Society of Cardiology; RCT-Randomized controlled trial; WMD-Weighted mean difference; CAH-Critical care hospital; SRD-Sodium restricted diet; CMS-Centers for Medicare and Medicaid Services; TPB-Theory of planned behavior; LSD-Low sodium diet; PATCH-Patient activation intervention; UC-Control trial of usual care; PFE-Patient-family education; FPI-Family-partnership intervention
1. Introduction
Heart failure (HF) is an international public health problem, with an estimated 38 million cases worldwide, which is increasing with population aging [1]. Despite the rapid development of medical technology and reduction of the mortality in HF patients, the risk of rehospitalization still remains high in patients with chronic heart failure (CHF), with the readmission rate of 25% [2]. Nonadherence with medication and/or diet is the most common reason of these admissions to the hospital [3]. Especially, excessive sodium intake can lead to fluid overload, which in turn can lead to hospitalization and poor quality of life [4]. To manage HF, it requires not only pharmacological therapy, but also non-pharmacological treatment, which is targeted at increasing patients’ self-care [5]. HF self-care behaviors are recommended in the relevant guidelines published by the Heart Failure Society of America (HFSA) [6], the European Society of Cardiology (ESC) [7] and Heart Failure Group of Chinese Society of Cardiology [8], including the restriction of sodium, fluid and alcohol intake, recommendation of physical activity, monitoring signs and symptoms, smoking cessation and keeping follow-up with medical professionals and so forth. Therefore, a sodium-restricted diet has been recommended as one of the standard components of HF management [4, 6-8]. However, in clinical practice, current sodium consumption in HF patients probably exceeds far more than a guideline-recommended amount [9, 10]. As one of the most important part of the multi-disciplinary health care team, nurses take on multiple tasks [11], and play an indispensable role in the management of dietary sodium in HF patients. Several studies have demonstrated the effectiveness of nurse-led/participatory interventions in reducing dietary sodium intake in HF patients, but other studies [12, 13] found no significant effect. Basing on a systematic review of the current literature, we aimed to appraise the effectiveness of nursing interventions for decreasing sodium intake for CHF patients, summarize the current evidence, and provide references for future studies on dietary sodium management in HF patients.
2. Materials and Methods
The PRISMA statement [14] and the guidance in the Cochrane Handbook [15] for systematic reviews and meta-analyses were followed.
2.1 Retrieval strategies
Two reviewers (WY and SH) systematically searched across several databases, including PubMed, CINAHL, Web of Science, Embase and the Cochrane Central Register of Controlled Trials for relevant articles from their inception up to December, 2018. Search terms for sodium intake were combined with search terms for heart failure. Search strategies were adapted for each database as necessary. Taking the retrieval of the PubMed database as an example, the complete search strategy is shown in Table 1.
|
S.no. |
Search |
|
#1: |
(((((((((((((Heart Failure[MeSH Terms]) OR Heart Failure, Diastolic[MeSH Terms]) OR Heart Failure, Systolic[MeSH Terms]) OR Cardiac Failure[Title/Abstract]) OR Myocardial Failure[Title/Abstract]) OR Congestive Heart Failure[Title/Abstract]) OR cardiac dysfunction[Title/Abstract]) OR cardiac insufficiency[Title/Abstract]) OR heart failure[Title/Abstract]) OR CHF[Title/Abstract]) OR HF[Title/Abstract])) |
|
#2: |
((((((((((((Sodium, Dietary[MeSH Terms]) OR Sodium Chloride, Dietary[MeSH Terms]) OR Sodium Chloride[MeSH Terms]) OR Diet,Sodium-Restricted[MeSH Terms]) OR Sodium, Dietary[Title/Abstract]) OR salt[Title/Abstract]) OR salt intake[Title/Abstract]) OR sodium intake[Title/Abstract]) OR Sodium-Restricted Diet*[Title/Abstract]) OR Low-Sodium Diet*[Title/Abstract]) OR Low-Salt Diet*[Title/Abstract]) OR Salt-Free Diet[Title/Abstract])) |
|
#3: |
(((((((randomized controlled trial[Publication Type]) OR controlled clinical trial[Publication Type]) OR randomized[Title/Abstract]) OR palcebo[Title/Abstract]) OR clinical trails as topic[MeSH Terms: noexp]) OR clinical trails as topic[Title/Abstract]) OR trial[Title]). |
|
#4: |
#1 AND #2 AND #3 |
Table 1: Search strategy (take the retrieval of the PubMed database as an example).
2.2 Study selection criteria and types of outcome measures
The literature selection in this present study was based on the following inclusion and exclusion criteria:
Publications had to (1) describe randomized controlled trial (RCT), (2) target adults (aged ≥ 18 years) with chronic stable heart failure, (3) integrate nurse-led or nurse-involved interventions, (4) evaluate sodium intake as outcome measures, which could be estimated by means of 24-hour urine secretions or dietary anamnesis. To avoid discrepancy, we further defined that control group using usual care, referred to receiving usual treatment with medical and nursing staff and the general health education nursing services. On the basis of the standard care, the experimental interventions could be conducted with in-depth counseling, interviews, reminders, structural health education or other individualized, comprehensive managements designed to reduce dietary sodium intake in patients with chronic heart failure. In this process, nurses may act as leaders, managers or resource coordinators of intervention projects. Publications had to be available in (5) full-text, (6) English and there were no limits on year published. Studies involving patients with other complication such as end-stage hepatic failure, renal failure, active malignancy and so forth were precluded.
2.3 Trial selection and data extraction
The search strategy was performed in the 5 English databases to screen and select the relevant references and remove the duplicate studies. Two authors (WY and SH) independently extracted data and rated the quality of the studies according to a bias rating tool [15], resolving differences by discussions with the third author (SZ). The following items were extracted, including: author, year, country, number and mean age of the subjects, characteristics of the intervention and control, duration, and evaluation method and outcome measures. We planned to perform a meta-analysis if sufficient reliable data were available.
2.4 Data analysis
We used mean difference and standardized mean difference to assess the continuous outcomes and the meta-analysis was displayed graphically as forest plot and calculated using STATA 12.0 software. P<0.05 was considered significant. If the standard deviation is not reported in the original text, the confidence interval and t values provided in the literature will be converted to the standard deviation according to the method in the system evaluation manual [15]. The I2 statistic was used to assess the presence of clinical and methodological heterogeneity. If I2 values are less than 50%, it can be generally considered that multiple similar studies are homogeneous, and fixed effect model can be selected for meta-analysis. On the contrary, if I2 values is greater than 50%, it can imply substantial heterogeneity, even with considerable heterogeneity, a random effect model would be used. At the same time, subgroup and sensitivity analyses can be considered to explore possible reasons for heterogeneity. If the source of heterogeneity cannot be determined, descriptive analysis will be adopted instead of meta-analysis. The weighted mean difference (WMD) method will be applied when the measurement tool is consistent for the continuous variable. Conversely, if different measurement tools are used for the same variables, the standardized mean difference (SMD) will be used for analysis. 95% confidence intervals (95% CI) was calculated for all analyses. Publication bias will be assessed by visual analysis of funnel plots, if at least 10 studies were included in a meta-analysis.
3. Results
3.1 Search results
The literature search retrieves a total of 515 records, including 226 in PubMed, 60 in Embase, 16 in CINAHL, 19 in Web of Science and 194 in Cochrane. After removing 144 duplicates, 371 references were remained and 62 publications were selected based on the title and abstract for full-text review. After independent assessment by two authors, another 54 publications were excluded. In the end, 8 articles satisfied the predefined inclusion criteria for analysis. A flow chart of the search and selection process is presented in Figure 1.
3.2 Study characteristics
These articles were originated from the United States (n=2), Canada (n=2), Sweden (n=1), Mexico (n=1), Brazil (n=1) and Iran (n=1), with a total of 530 samples. All the studies were RCTs of patients with confirmed diagnosis of HF, who had received or were still receiving optimal medical treatments according to guidelines (without change in diuretic dose recently). The study interventions were performed in different study Settings. Among them, 3 were conducted in the specialty HF clinics or ambulatory clinics, 3 in university-affiliated hospitals, 1 at a rural critical care hospital (CAH). And only one study was recruited from a cardiology clinic, community hospital and a university hospital simultaneously. The mean age of patients across the 8 studies was 63.6 years old, and the total sample of the studies providing data was nearly equally divided by gender (52.8% male). Only three studies mentioned ethnicity and were primarily Caucasian (90%). The majority of the patients were married, retired, or living at home with their spouses and children. In addition, the duration of the studies and interventional time points were varied. In most cases, intervention was initiated once patients were enrolled and assessed, and they were followed up for at least 3 months. The majority of studies [12, 13, 16, 17] were followed up for 6 months, and a few studies [18, 19] had a longer follow-up period from 12 months to 24 months. In this review, the measured values within 6 months were used for analysis. The details of the included 8 articles are summarized in Table 2.
HF-heart failure; CHF-chronic heart failure; EF-ejection fraction; LVEF-left ventricular ejection fraction; mo-month; NYHA-New York Heart Association; wk-week; TPB-theory of planned behavior; RSD-restriction of sodium diet; SM-self-management; RD-registered dietician; RN-registered nurse; IG-intervention group; CG-control group
3.3 Contents of nursing intervention
Diet-related nursing intervention in patients with HF includes providing menu or informing patients of sodium intake goal. In these eight randomized studies, nurse-led and/or nurse assisting a dietitian to provide nutrition education and consultation. A total of 5 studies [12, 13, 17, 20, 21] focused on the standardization of education intervention, in order to improve the HF patients’ nutrition knowledge and sodium restricted diet (SRD) adherence. 7 studies [12, 13, 16-20] helped patients in the intervention group to set a daily dietary sodium intake goal, which ranges from 1500 to 3000 mg/d. Most control groups [16, 18-21] accepted general dietary advice or received the standardized discharge diet instructions as recommended by Centers for Medicare and Medicaid Services (CMS) and the Joint Commission [13]. At the same time, there are 2 studies’ control groups [12, 17] receiving no dietary guidance. The intervention content is the focus of this review, and the general strategies of these included RCTs are shown in Table 3.
All studies developed and provided specific written educational materials, educational tools for the target population, which included a self-management (SM) workbooks [13], a SRD handout [17, 20], instructions from the dietitian [16] and a low-sodium shopper’s guide that reviewed content in commonly purchased foods [20]. In the educational courses, researchers usually used visual aids (e.g. plastic models of food portions [17], web links [13], etc.) along with verbal explanations, a step-on weight scale with large and bright readings [13], a specifically created calendar [12] and a diet manual [21] consisting of information about the amount of sodium in different foods and cooking methods to deepen patients’ understanding of knowledge related to heart failure and improving their compliance with dietary sodium management behaviors. Meanwhile, researchers usually conducted educational sessions, face-to-face interviews, review of dietary of the intervention group patients, and/or telephone follow-up to enhance the intervention effect. The duration of each educational activity (courses/sessions/lectures presented to small groups, etc.) ranged from 45 minutes to 1 hour. Personalized consulting was about 15 to 30 minutes, and follow-up call was limited to 10 to 15 minutes. Almost all studies selected a variety of strategies to meet individual patient learning needs. Welsh et al. [17] recommended that a research intervention nurse should provide education through two home visits and two follow-up telephone calls, in conjunction with visual aids suitable for content introduction, including diagrams of the heart, drawings of salt shakers, swollen extremities, which could help patients understand the connections among excessive dietary sodium intake, symptoms and hospitalization etc. In addition to multiple forms of intervention (verbal, written, and visual), the study by Young et al. provided an educational toolkit that contained a digital scale and an electronic pillbox. Colin-Ramirez et al. [18] prepared a list of recommended and discouraged foods based on their sodium content per serving and provided a set of 6 daily sample menus to patients, which was consistent with their energy requirements and sodium restriction. Furthermore, researchers told the intervention subjects to avoid sodium-rich foods and condiments, and use low-sodium or sodium-free cereals. Also, cooking with lemon juice, vinegar, vanilla, garlic, onion or flavoring was encouraged.
3.4 Theoretical framework of included studies
In the 8 studies included, only 3 studies used theory to guide the intervention. Welsh et al. [17] and Akhondzadeh et al. [21] cited the theory of planned behavior (TPB) as the theoretical framework and developed structured teaching strategies. These strategies could help medical personals address different problems including patients’ attitudes, subjective norms, and other problems in the learning process to promote HF patients’ adherence to a low sodium diet (LSD). Young L, et al. [13] proposed the patient activation intervention (PATCH) for study based on components of Lorig’s chronic disease self-management model, Hibbard’s patient activation theory, Bandura’s conceptualization of self-efficacy and Long and Weinert’s rural nursing theory. Hence, the intervention was triggered by the patients’ hospitalization and initiated during the stay in hospital when they felt most vulnerable and were most likely to accept the idea of making behavioral changes to avoid readmission. Furthermore, PATCH presented the tailored intervention sessions based on activation level, and set goals in advance to enhance the intervention effect.
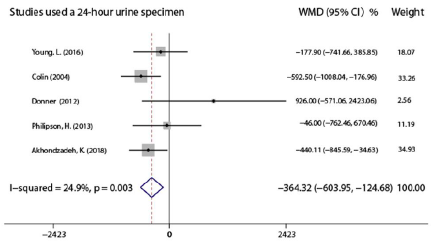
3.5 Change in sodium intake
Meta-analysis results showed that there was a significant decrease in sodium intake of the experimental group compared to the control arm in a short term after the end of the nursing intervention program [SMD -0.305, 95% CI (-0.561 to -0.0.049), P=0.02, Figure 2], and the pooled studies were homogeneous (I2=47.2%). At present, 24-hour urine sodium has been considered as the gold standard to measure sodium consumption [22, 23], and 5 studies [12,13,16,19,21] instructed patients to collect a 24-hour urine specimen to measure sodium intake. However, the other 3 studies [17,18,20] used a 3-day food record/diary, which was also used to assess sodium and total dietary intake in patients with HF. Dunbar et al. [24] pointed out that the sodium levels for the 3-day food record were much lower than those from the 24-hour urinary sodium. Also the nutrition software calculated without considering the sodium added in the diet, indicative of common underreporting and under-estimating sodium consumed through dietary assessments. Therefore, it is better to distinguish in the integrated analysis in order to further clarify the effect of nursing intervention. Further meta-analysis results showed that the sodium intake estimated by the 3-day diet record/diary in the experimental group was lower than that in the control group after the end of the nursing intervention [SMD -0.523, 95%CI (-0.894 to -0.152), P=0.006, Figure 3]. The 3 studies [17, 18, 20] were homogeneous (I2=8.3%). Similarly, the sodium intake in the experimental group was lower than that in the control group by 24-hour urine specimen [WMD-364.318, 95%CI (-603.953 to -124.684), P=0.003, Figure 4]. The 5 studies [12, 13, 16, 19, 21] were homogeneous as well (I2=24.9%).
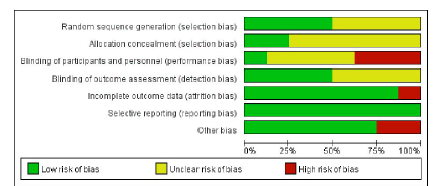
3.6 Risk of bias across studies
The risks of bias in the eight included studies were different. Four studies [12, 13, 18, 21] were conducted with specific randomization, among which two [13, 21] reported the methods of allocation concealment. Since it is difficult for nurses to perform a double blind (participant and provider) intervention in hospital, the main observation was result evaluator blinding. Details of the assessment risk of bias of the included studies using the Cochrane Handbook for Systematic Reviews of Interventions-version 5.1.0 are provided in Table 4 and all the results are summarized in Figure 5. Finally, Egger’s test did not exhibit a significant published bias regarding the sodium intake outcome (P=0.471).
|
Bias |
Author |
Arcand, et al. [20] |
Welsh], D, et al. [17] |
Colin-Ramirez, et al. [18] |
Young L, et al. [13] |
Colín Ramírez, et al. [16] |
Donner, et al. [12] |
Philipson H, et al. [19] |
Akhondzadeh K, et al. [21] |
|
Year |
2005 |
2013 |
2014 |
2016 |
2004 |
2012 |
2013 |
2018 |
|
|
Selection bias: random sequence generation |
U |
U |
L |
L |
U |
L |
U |
L |
|
|
Selection bias: allocation concealment |
U |
U |
U |
L |
U |
U |
U |
L |
|
|
Performance bias: adequate participant and provider blinding |
U |
U |
H |
H |
U |
U |
H |
L |
|
|
Detection bias: adequate result evaluator blinding |
U |
U |
L |
L |
U |
U |
L |
L |
|
|
Attrition bias: integrity of outcome indicator data |
H |
L |
L |
L |
L |
L |
L |
L |
|
|
Reporting bias: selective outcome reporting |
L |
L |
L |
L |
L |
L |
L |
L |
|
|
Other bias |
L |
H |
L |
H |
H |
L |
L |
L |
|
|
Literature quality grade |
B |
B |
B |
B |
B |
B |
B |
A |
|
H-the risk of bias is high; L-the risk of bias is low; U-unclear
Table 4: Assess risk of bias of the included studies using the Cochrane Handbook for Systematic Reviews of Interventions-version 5.1.0.
4. Discussion
4.1 Summary of evidence
The purpose of this systematic review is to evaluate the effect of nursing intervention on reducing dietary sodium intake in CHF patients. General strategies for nursing intervention are quite abundant. In addition to specific written educational materials and tools, the researchers also conducted face-to-face education and counseling for the experimental groups, or provided personalized courses to review the diet with the intervention subjects or enhanced the intervention effect through telephone follow-up. Changes in dietary behavior are associated with multiple factors such as age, comorbidity, economic status, education background, social support, and personal cognition. Therefore, it is not likely that any one nursing intervention will work for all patients. In that case, instruction is required to be flexible enough to meet individual patient/family needs and be adjusted to address factors that could prohibit patients’ RSD adherence [25]. At the same time, lots of current nursing intervention research to promote RSD compliance in patients with CHF is still limited by lack of a theoretical framework, due to unclear mechanisms of the intervention [13]. In addition, the influence of family and social support on individual behavior change had not received enough attention. Among the available literatures, only 3 studies [13, 17, 21] demonstrated that families should be involved in the education program based on the dietary compliance occurred in the context of the family. Dunbar et al. [24] defined HF patients and one family member as ‘dyads’, and all subjects were divided into three groups, including control trial of usual care (UC), patient-family education (PFE), and family-partnership intervention (FPI). Dyads in FPI received additional sessions that focused on teaching them how to give support, communication, empathy, and autonomy support for one another’s role in order to decrease family members’ complaints or criticism of HF patients and promote the solution of problems within the family. The results indicated that the FPI demonstrated a greater maintenance effect of reducing sodium intake for those with poor family function than the PFE group, which provided information alone. It was an important finding suggesting that we should pay more attention to the interaction between HF patients and family caregivers in the future intervention studies.
The results of six original studies [16-21] showed that the nursing intervention had a positive impact on the adherence intention to the RSD and could reduce sodium intake in patients with HF. Two studies [12, 13] which did not result in significant changes on sodium intake suggested that it might be related to a lack of individualized education plans within the intervention strategies, as well as some interactive education programs. Besides, partially collecting urine specimens, heavy perspiration, chronic diarrhea and drug usage may interfere with the consistency of 24-hour urine excretion and dietary intake [23].
5. Limitations and Potential Biases in the Review Process
First, only English literatures were included in this review, and it might lead to incomplete inclusion. Second, the overall qualities of the eight articles were mostly medium, and the RCTs were different in designs, which could lead to some bias in the final results. Third, nursing intervention strategies were not entirely the same, and sample size of some studies is small, which might give rise to clinical heterogeneity. Finally, the studies included in this review were from multiple countries, and the different racial and physical quality of the subjects in each study was also the possible cause of the clinical heterogeneity.
6. Conclusions
Nurse-led and/or nurse-engaged interventions can improve the short-term (≤6 mo) effect of dietary sodium intake management in patients with CHF, but the long-term effect is uncertain. It is recommended to optimize strategies for nurses to educate CHF patients on the modification of the life style, such as restrictive behaviors, and extend the follow-up time in future studies in order to provide more valuable evidence.
Compliance with Ethical Standards: Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Braunwald E. The war against heart failure: the Lancet lecture. Lancet 385 (2015): 812-824.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62 (2013): 147-239.
- Kuehneman T, Gregory M, de Waal D, et al. Handu D Academy of Nutrition and Dietetics Evidence-Based Practice Guideline for the Management of Heart Failure in Adults. Journal of the Academy of Nutrition and Dietetics 118 (2018): 2331-2345.
- Arcand J, Ivanov J, Sasson A, et al. A high-sodium diet is associated with acute decompensated heart failure in ambulatory heart failure patients: a prospective follow-up study. The American journal of clinical nutrition 93 (2011): 332-337.
- Oosterom-Calo R, van Ballegooijen AJ, Terwee CB, et al. Determinants of heart failure self-care: a systematic literature review. Heart failure reviews 17 (2012): 367-385.
- Lindenfeld J, Albert NM, Boehmer JP, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. Journal of cardiac failure 16 (2010): 1-194.
- Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). European journal of heart failure 10 (2008): 933-989.
- Heart Failure Group of Chinese Society of Cardiology of Chinese Medical A, Chinese Heart Failure Association of Chinese Medical Doctor A, Editorial Board of Chinese Journal of C. Chinese guidelines for the diagnosis and treatment of heart failure 2018. Zhonghua Xin Xue Guan Bing Za Zhi 46 (2018): 760-789.
- Lemon SC, Olendzki B, Magner R, et al. The dietary quality of persons with heart failure in NHANES 1999-2006. Journal of general internal medicine 25 (2010): 135-140.
- Basuray A, Dolansky M, Josephson R, et al. Dietary sodium adherence is poor in chronic heart failure patients. Journal of cardiac failure 21 (2015): 323-329.
- Fu L, Li H, Hu Y. Effectiveness of nurse-led interventions on improving medication adherence in people living with HIV/AIDS: a systematic review. Chinese Journal of Nursing 49 (2014): 1413-1419.
- Donner Alves F, Correa Souza G, Brunetto S, et al. Nutritional orientation, knowledge and quality of diet in heart failure: randomized clinical trial. Nutricion hospitalaria 27 (2012): 441?448.
- Young L, Hertzog M, Barnason S. Effects of a home-based activation intervention on self-management adherence and readmission in rural heart failure patients: the PATCH randomized controlled trial. BMC cardiovascular disorders 16 (2016): 176.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed) 339 (2009): 2535.
- Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 343 (2011): 5928.
- Colin Ramirez E, Castillo Martinez L, Orea Tejeda A, et al. Effects of a nutritional intervention on body composition, clinical status, and quality of life in patients with heart failure. Nutrition (Burbank, Los Angeles County, Calif) 20 (2014): 890-895
- Welsh D, Lennie TA, Marcinek R, et al. Low-sodium diet self-management intervention in heart failure: pilot study results. European journal of cardiovascular nursing 12 (2013): 87?95.
- Colin-Ramirez E, McAlister F, Zheng Y, et al. The SODIUM-HF (Study of Dietary Intervention Under 100 MMOL in Heart Failure) pilot results. European heart journal 35 (2014): 721?722.
- Philipson H, Ekman I, Forslund HB, et al. Salt and fluid restriction is effective in patients with chronic heart failure. European journal of heart failure 15 (2013): 1304?1310.
- Arcand JA, Brazel S, Joliffe C, et al. Education by a dietitian in patients with heart failure results in improved adherence with a sodium-restricted diet: a randomized trial. American heart journal 150 (2005): 716.
- Akhondzadeh K, Ghezeljeh TN, Haghani H. The Effect of the Education Program on the Adherence Intention to the Dietary Sodium Restriction and the Amount of Sodium Intake in Patients With Chronic Heart Failure. Iranian Red Crescent Medical Journal 2018.
- Abshire M, Xu J, Baptiste D, et al. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. Journal of cardiac failure 21 (2015): 989-999.
- Bentley B. A review of methods to measure dietary sodium intake. The Journal of cardiovascular nursing 21 (2006): 63-67
- Dunbar SB, Clark PC, Stamp KD, et al. Family partnership and education interventions to reduce dietary sodium by patients with heart failure differ by family functioning. Heart and lung: the journal of critical care 45 (2016): 311-318.
- Welsh D, Marcinek R, Abshire D, et al. Theory-based low-sodium diet education for heart failure patients. Home healthcare nurse 28 (2010): 432.