Prevalence of Vitamin D Deficiency in Pregnant Diabetic Patients in Western Libya
Article Information
Ghrew Murad1,3*, Ellafi Hanan2, Msalati Abdulghani2, Bashein Abdulla2, Sultan Mohammed4, Sedaa Khaled2
1Faculty of Biology, Medicine and Health, University of Manchester, UK
2Department of Biochemistry and Molecular Biology, Faculty of Medicine, University of Tripoli, Libya
3Department of Medicine, Faculty of Medicine, University of Tripoli, Libya
4Department of Obstetrics and Gynaecology, Faculty of Medicine, University of Tripoli, Libya
Corresponding author: Murad Ghrew, Department of Medicine, Faculty of Medicine, University of Tripoli, Libya
Received: 24 June 2019; Accepted: 18 July 2019; Published: 22 July 2019
Citation:
Ghrew Murad, Ellafi Hanan, Msalati Abdulghani, Bashein Abdulla, Sultan Mohammed, Sedaa Khaled. Prevalence of Vitamin D Deficiency in Pregnant Diabetic Patients in Western Libya. Archives of Internal Medicine Research 2 (2019): 004-013.
Share at FacebookAbstract
Despite the relative abundance of sunny weather, surprisingly, there is increasing evidence that vitamin D deficiency is extremely prevalent in females of reproductive age in Middle East countries. There is also increasing interest in the non-classical roles of vitamin in health and disease including its relation to incidence of gestational diabetes, its impact on glycaemic control in diabetes mellitus, and its association with some complications of pregnancy like preeclampsia. The objective of this study was to estimate the prevalence of Vitamin D deficiency in pregnant diabetic patients in west Libya and analyse potential links to socioeconomic and cultural factors. This is a cross sectional observational study. Random plasma was collected form expected mothers attending the Antenatal Diabetes Clinic at Tripoli’s Main Maternity Hospital. Demographics and socioeconomic and cultural factors were recorded at the same time. Samples were analysed for vitamin D level and biochemical screening panel. Vitamin D level was obtained from 160 patients (mean age 35 years). Over all 95 % of the study population had vitamin D levels below normal (defined as vitamin D level of < 20 ng/mL). Results were subcategorised into severe deficiency (<10 ng/ml, 51.9%-83 patients), deficiency (< 20 ng/mL, 43.1%, 69 patients), insufficiency (20 - 30 ng/ml, 3.8%, 6 patients) and sufficient (> 30 ng/ml, only 1.3%, 2 patients). All patients were taking daily vitamin D Supplements at a dose of 400 IU as per hospital policy. Vitamin D deficiency is extremely prevalent in pregnant diabetic patients in Libya. There is no clear association with socioeconomic risk factors like employment, type of accommodation or geographic distribution. However, most of the study population had life style characterized by minimal exposure to direct sun light. Routine supplementation of Vitamin D
Keywords
Vitamin D; Libya; Pre-eclampsia; Pregnancy; Diabetes mellitus
Vitamin D articles Vitamin D Research articles Vitamin D review articles Vitamin D PubMed articles Vitamin D PubMed Central articles Vitamin D 2023 articles Vitamin D 2024 articles Vitamin D Scopus articles Vitamin D impact factor journals Vitamin D Scopus journals Vitamin D PubMed journals Vitamin D medical journals Vitamin D free journals Vitamin D best journals Vitamin D top journals Vitamin D free medical journals Vitamin D famous journals Vitamin D Google Scholar indexed journals Pre-eclampsia articles Pre-eclampsia Research articles Pre-eclampsia review articles Pre-eclampsia PubMed articles Pre-eclampsia PubMed Central articles Pre-eclampsia 2023 articles Pre-eclampsia 2024 articles Pre-eclampsia Scopus articles Pre-eclampsia impact factor journals Pre-eclampsia Scopus journals Pre-eclampsia PubMed journals Pre-eclampsia medical journals Pre-eclampsia free journals Pre-eclampsia best journals Pre-eclampsia top journals Pre-eclampsia free medical journals Pre-eclampsia famous journals Pre-eclampsia Google Scholar indexed journals Pregnancy articles Pregnancy Research articles Pregnancy review articles Pregnancy PubMed articles Pregnancy PubMed Central articles Pregnancy 2023 articles Pregnancy 2024 articles Pregnancy Scopus articles Pregnancy impact factor journals Pregnancy Scopus journals Pregnancy PubMed journals Pregnancy medical journals Pregnancy free journals Pregnancy best journals Pregnancy top journals Pregnancy free medical journals Pregnancy famous journals Pregnancy Google Scholar indexed journals Diabetes mellitus articles Diabetes mellitus Research articles Diabetes mellitus review articles Diabetes mellitus PubMed articles Diabetes mellitus PubMed Central articles Diabetes mellitus 2023 articles Diabetes mellitus 2024 articles Diabetes mellitus Scopus articles Diabetes mellitus impact factor journals Diabetes mellitus Scopus journals Diabetes mellitus PubMed journals Diabetes mellitus medical journals Diabetes mellitus free journals Diabetes mellitus best journals Diabetes mellitus top journals Diabetes mellitus free medical journals Diabetes mellitus famous journals Diabetes mellitus Google Scholar indexed journals Libya articles Libya Research articles Libya review articles Libya PubMed articles Libya PubMed Central articles Libya 2023 articles Libya 2024 articles Libya Scopus articles Libya impact factor journals Libya Scopus journals Libya PubMed journals Libya medical journals Libya free journals Libya best journals Libya top journals Libya free medical journals Libya famous journals Libya Google Scholar indexed journals child bearing age articles child bearing age Research articles child bearing age review articles child bearing age PubMed articles child bearing age PubMed Central articles child bearing age 2023 articles child bearing age 2024 articles child bearing age Scopus articles child bearing age impact factor journals child bearing age Scopus journals child bearing age PubMed journals child bearing age medical journals child bearing age free journals child bearing age best journals child bearing age top journals child bearing age free medical journals child bearing age famous journals child bearing age Google Scholar indexed journals osteoblasts articles osteoblasts Research articles osteoblasts review articles osteoblasts PubMed articles osteoblasts PubMed Central articles osteoblasts 2023 articles osteoblasts 2024 articles osteoblasts Scopus articles osteoblasts impact factor journals osteoblasts Scopus journals osteoblasts PubMed journals osteoblasts medical journals osteoblasts free journals osteoblasts best journals osteoblasts top journals osteoblasts free medical journals osteoblasts famous journals osteoblasts Google Scholar indexed journals cardiovascular disease articles cardiovascular disease Research articles cardiovascular disease review articles cardiovascular disease PubMed articles cardiovascular disease PubMed Central articles cardiovascular disease 2023 articles cardiovascular disease 2024 articles cardiovascular disease Scopus articles cardiovascular disease impact factor journals cardiovascular disease Scopus journals cardiovascular disease PubMed journals cardiovascular disease medical journals cardiovascular disease free journals cardiovascular disease best journals cardiovascular disease top journals cardiovascular disease free medical journals cardiovascular disease famous journals cardiovascular disease Google Scholar indexed journals bowel disease articles bowel disease Research articles bowel disease review articles bowel disease PubMed articles bowel disease PubMed Central articles bowel disease 2023 articles bowel disease 2024 articles bowel disease Scopus articles bowel disease impact factor journals bowel disease Scopus journals bowel disease PubMed journals bowel disease medical journals bowel disease free journals bowel disease best journals bowel disease top journals bowel disease free medical journals bowel disease famous journals bowel disease Google Scholar indexed journals sclerosis articles sclerosis Research articles sclerosis review articles sclerosis PubMed articles sclerosis PubMed Central articles sclerosis 2023 articles sclerosis 2024 articles sclerosis Scopus articles sclerosis impact factor journals sclerosis Scopus journals sclerosis PubMed journals sclerosis medical journals sclerosis free journals sclerosis best journals sclerosis top journals sclerosis free medical journals sclerosis famous journals sclerosis Google Scholar indexed journals
Article Details
1. Introduction
The Middle East weather is known for its moderate temperature and long periods of sunshine which gives abundant opportunities for outdoor activities and sunlight exposure, the main source of vitamin D. However, there is growing evidence that vitamin D deficiency is very prevalent, especially in females of child bearing age [1, 2]. The aetiology of this is likely to be multifactorial and could be related in part to life style choices like active sunlight avoidance to maintain pale skin colour, religious dress codes (Hijab, scarfs) and limited opportunities for outdoor activities [3].
Vitamin D plays key “classical” role in maintaining calcium and phosphate homeostasis and in promotion of proliferation and differentiation of bone forming osteoblasts. Consequently, severe vitamin D deficiency leads to the well described skeletal conditions; rickets in children and osteomalacia in adults [4].
The last decade was marked by increasing interest in studying the “non-classical” roles of vitamin D. A growing body of evidence suggests that vitamin D may have important role in; immunity and inflammatory response to infections especially granulomatous diseases like tuberculosis [5], reduction of incidence of cancer [6], glucose homeostasis in type II diabetes mellitus [7], and cardiovascular disease [8]. Vitamin D deficiency has also been implicated as a potential etiological factor in inflammatory bowel disease, multiple sclerosis [9], and accelerated decline in cognitive functions [10].
In diabetes Mellitus, Vitamin D role is complex. Studies suggested that vitamin D can reduce pancreatic islet cell destruction through suppression of pro-inflammatory cytokines such as tumour necrosis factor (TNF)-α and therefore reduce the incidence and type I diabetes mellitus [11]. Some studies suggest that Vitamin D replacement in vitamin D deficient subjects may to improve glycaemic control in type II Diabetes mellitus although evidence has not been substantiated in systematic review of interventional studies [12, 13]. Maternal vitamin D deficiency is associated with increasing risk of pre-eclampsia, preterm birth, low birthweight, impaired postnatal growth and increased risk of gestational diabetes [14, 15].
Cochrane systematic review published in 2016 indicated that vitamin D supplementation could reduce the risk of pre-eclampsia and increase length and head circumference at birth [16]. Similar conclusions were drawn on other systematic reviews [17]. In many antenatal clinics, including the Antenatal Diabetes Clinic at Aljala Hospital, it has been routine practice to advice pregnant mothers to take 400 IU vitamin D as daily supplement. While this dose may be sufficient as supplement to ensure adequate levels in mothers with no pre-existing deficiency, this dose is not adequate for replacement in patients with overt vitamin D deficiency [18].
Vitamin D epidemiological data is very limited in Libya. We conducted this study to try to quantify the problem in one of the most vulnerable groups, pregnant diabetics given that 3 risk factors are linked to this group namely, known high prevalence of deficiency in females of child bearing age, increased risk of gestational diabetes and poor glycaemic control and increased incidence of pregnancy complications in vitamin D deficiency state. We have also attempted to try to understand socioeconomic factors and life style choices and their influence on vitamin D level and lastly we examined the effect of vitamin D routine supplement on vitamin D levels.
Methods
1.1 Ethical Statement
The study was conducted in accordance with the international guidelines laid down in the Declaration of Helsinki [19]. All subjects gave their informed consent for their participation in this study. The clinical team was blinded to the result and all patients received the standard care as per clinic policies and protocols.
1.2 Study Population and data collection
The target study population of this study was the attendees of the Antenatal Diabetes clinic at the main maternity hospital in Tripoli (Aljala Hospital) which has a catchment area that covers most of West Libya including the capital Tripoli. Patients were recruited at random in any trimester of pregnancy. Patients with pre-existing diagnosis of vitamin D deficiency were excluded. We also excluded patients with known malabsorption, stage 4&5 Chronic Kidney Disease and patients on therapeutic doses of Vitamin D. 160 patients aged between 18- 46 participated in the study.
Information about demographic characteristics, life style choices, socioeconomic status were collected by one member of the research team through interview and completion of predesigned questionnaire.
1.3 Laboratory analysis
After detailed consenting process, venous blood was collected into 10ml serum separator tube (BD Vacutainer-Becton Dickenson) with clot activator. All samples were centrifuged at room temperature at 3000 rpm for 10 minutes, immediately after that all samples were divided into 3 Eppendorf tubes. 25 (OH) vitamin D concentrations were measured on ARCHITECTi1000sr immunoassay (Abbott Diagnostics, USA) 20. The device was regularly calibrated as per the manufacturer standards. Data were managed and analysed by SPSS version 22. Descriptive study and inferential statistics are used. A p value < 0.05 was considered as significant.
Results
In a total of 160 Libyan pregnant diabetic women participated in this study, the prevalence of vitamin D deficiency defined as vitamin D level < 20 ng/ml was 95%. Only 2 (1.3%) participants had vitamin D level considered sufficient/normal (> 30 ng/ml). Six participants had level measured 20 - 30 ng/ml classified as insufficient level. The mean age of participants was 34.95 ± 5.5, (range 25 years, 21 - 46).
On subgroup analysis based on cultural habits and risk factors, there were no significant differences in the incidence of vitamin D deficiency in subgroups based on age, gestational age, gravity, parity, type of diabetes, effectiveness of diabetic control, presence of chronic medical conditions other than diabetes, skin colour, dressing style, use of sun screen, life style and exercise.
Table1: Maternal characteristics and vitamin D status of 160 Libyan Diabetic pregnant women.
Thus, 51.9% of participants were housewives, 45.6% were employed and 2.5% were students. 56.9% of them lived in Tripoli and its suburbs while 43.1% lived outside Tripoli in west Libya.
In figure 1, 85 women had diabetes mellitus type II (53.1%), 48 (30%) had gestational diabetes and 27 (16.9%) had diabetes type I. Only 61.7% of participants had HbA1c level of < 7 which is considered as evidence of good diabetic control. There was higher incidence of severe vitamin D deficiency in patients with Gestational Diabetes in comparison with Type I and Type II diabetes but this also did not reach statistical significance (66.7 %, 48.1%, and 44.7%. P 0.19).
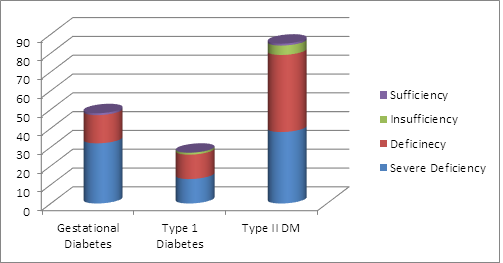
Figure 1: Vitamin deficiency pattern according to type of Diabetes mellitus
Diabetic control did not seem to be associated with any level of vitamin status in this group, P 0.89. Only two participants had Chronic Kidney Disease (CKD1-2) While 22.5% had thyroid dysfunction which was not associated with increased risk of vitamin deficiency.
Non-of the participants was known with existing gestational problem. In multigravidas, 66.9% of them had history of complication in previous pregnancy and 58.8% had history of previous neonatal complication. 45% of the participants were in their third Trimester, 38.8% in the second trimester and 16.3% in the first trimester. 89.4% were multigravida and 10.6% were primigravida. There was tendency for higher incidence of severe deficiency in the 3rd trimester in comparison with 1st and 2nd however this difference did not reach statistical significance in this study population (Figure 2).
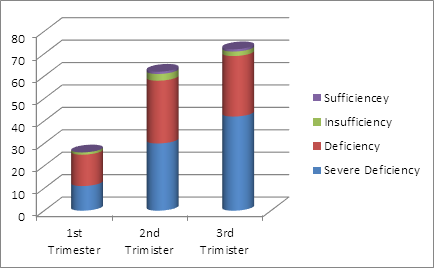
Figure 2: Vitamin D status in pregnant diabetics grouped according to gestational age.
Likewise, multigravida participants had higher incidence of severe vitamin D deficiency in comparison with primigravida (53.8% vs 35.3%) but this did not reach statistical significance, P 0.11. 81.9% of women reported regular intake of milk and dairy product while 3.1% did not eat dairy products at all. Only 37.5% of participants reported regular inclusion of fish and/or fish oil in their diet while 86.3 % consumed meat and liver on regular basis. 146 of participants were of white skin colour while 14 were black. 91.6% of white women had severe vitamin D deficiency. The description of white skin colour included all the categories of skin tone in Fitzpatrick scale except dark brown (grade VI) which was considered black. There was no statistical difference in the incidence of severe vitamin D deficiency between the 2 groups.
Only minority of participants (4/160) reported that they spend most of the day time outdoors (e.g. working in farm or sports teacher), none of them had severe deficiency but all had deficiency (vitamin D 10-20 ng/ml). There was no statistical difference between the 3 groups (mostly indoors, part outdoors, mostly outdoors. P 0.15). 64.4% of participants reported they were not engaged in any regular exercise. Only 19.4 % of women reported regular use of sunscreen. 90% wore scarf and 10% wore full body cover including vail. This is for cultural and religious reasons therefore skin is insulated from exposure to sunlight most of the time in all participants.
3. Discussion
There has been a growing interest over the last decade in the role of vitamin D in health especially its non-classical role. In the context of pregnancy, vitamin D deficiency has been implicated as contributing factor to multiple complications. Good vitamin D levels are also important in maintaining good diabetic control.
For cultural and religious reasons, women of child bearing age in the Middle East tend to be minimally exposed to sun light. This is because of the religious code of full body cover sometimes including the face. Even ladies who do not cover the face as part of the religious dress code, they tend to avoid sun exposure as pale skin tone is more desirable as opposed to tanned skin in western society [21, 22]. For this reason diabetic pregnant women are one of the most vulnerable groups for vitamin D Deficiency in the Middle East. In this cross sectional observational study we examined the level of vitamin D in 160 randomly selected sample of pregnant diabetic patients attending the antenatal diabetes clinic at AlJala Obstetrics and Gynaecology Hospital in Tripoli.
Although the generally accepted measure of vitamin D status is circulating 25(OH)D concentration, there is little consensus on which assay method should be used and what are the cut points for normal and abnormal ranges [23]. In this study, we used ARCHITECTi1000sr immunoassay (Abbott Diagnostics, USA). We also defined deficiency as vitamin D level of < 20 ng/ml and severe deficiency as level of < 10 ng/ml. A level of 20 – 30 ng/ml was considered insufficiency while a level of > 30 ng/ml is considered sufficient level. These cut points are widely used in the American literature although some authorities consider normal is a level above 40 or 50 ng/ml [24].
Using these definitions and this assay technology our study shows that vitamin D deficiency is highly prevalent among pregnant diabetic ladies. 95% of study population had a level of < 20 ng/ml, deficiency. 51.9% have severe deficiency defined as vitamin D level of < 10 ng/ml. Patients with severe deficiency are not only at risk of “non-classical” problems but also at risk of classical manifestations of vitamin D deficiency like bone demineralization and hypocalcaemia.
In this study we could not find any significant associations in subgroup analysis based on age, parity, and gestational age, and gravity, type of diabetes, diabetic control, skin colour, dress code and life style. We think this was related partly to the sample size as the study was not designed to detect difference in these groups but merely to estimate the total prevalence and describe demographic and risk factors characteristics. The other reason for lack of differences in these subgroups is the extremely high incidence of deficiency in all categories. We have not analysed skin colour into detailed subgroups but we suspect that most of the Libyan population are of brown tone within the range of Fitzpatrick scale of II-V therefore are at higher risk of vitamin D deficiency. All participants were not exposed to sun light in any significant time due to dress code, life style and cultural choices of protecting skin to maintain paler tone. Although this was not evident in this study but we think these factors are playing a major role in this widely prevalent deficiency status [25].
Although this group of patients were all taking vitamin D supplement of 400IU as per national recommendations, this level of supplementation did not appear to ameliorate their deficiency status.
Conclusion
Vitamin D deficiency is very prevalent in diabetic pregnant patients in west Libya. It appears that daily supplements of 400 IU are not sufficient to maintain adequate vitamin D level. This leaves this vulnerable group at risk of both classical and non-classical complications of vitamin D deficiency and therefore routine screening for vitamin D deficiency should be considered. Patients with Vitamin D deficiency need therapeutic doses to restore normal level.
References
- Halicioglu O, Aksit S, Koc F, Akman SA, Albudak E, et al. Vitamin D deficiency in pregnant women and their neonates in spring time in western Turkey. Paediatr Perinat Epidemiol26 (2012): 53-60.
- Narchi H, Kochiyil J, Zayed R, Abdulrazzak W, Agarwal M. Maternal vitamin D status throughout and after pregnancy. J Obstet Gynaecol30 (2010): 137.
- Holick MF. Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr 61 (1995): 638-645.
- Simon HS Pearce, Tim D Cheetham. Diagnosis and management of vitamin D deficiency. BMJ 340 (2010): 5664.
- Coussens AK, Wilkinson RJ, Hanifa Y, Nikolayevskyy V, Elkington PT, et al. Vitamin D accelerates resolution of inflammatory responses during tuberculosis treatment. Proc Natl Acad Sci USA109 (2012): 15449-15454.
- Dou R, Ng K, Giovannucci E, Manson J, Qian Z, et al. Vitamin D and colorectal cancer: Molecular, epidemiological and clinical evidence. British Journal of Nutrition 115 (2016): 1643-1660.
- Grammatiki M, Rapti E, Karras S, et al. Vitamin D and diabetes mellitus: Causal or casual association? Rev Endocr Metab Disord 18 (2017): 227.
- Stefan Pilz, Nicolas Verheyen, Martin Grubler, et al. Vitamin D and cardiovascular disease prevention. Nature Reviews Cardiology 13 (2016): 404-417.
- Brooke Rhead, Maria Baarnhielm, Milena Gianfrancesco, et al. Mendelian randomization shows a causal effect of low vitamin D on multiple sclerosis risk. Neurol Genet 2 (2016): 97.
- Miller JW, Harvey DJ, Beckett LA, et al. Vitamin D Status and Rates of Cognitive Decline in a Multiethnic Cohort of Older Adults. JAMA Neurol 72 (2015): 1295-1303.
- Wang Y, He D, Ni C, Zhou H, Wu S, et al. Vitamin D induces autophagy of pancreatic β-cells and enhances insulin secretion. Molecular Medicine Reports 14 (2016): 2644-2650.
- Anyanwu AC, Fasanmade OA, Odeniyi IA, Iwuala S, Coker HB, et al. Effect of Vitamin D supplementation on glycemic control in Type 2 diabetes subjects in Lagos, Nigeria. Indian journal of endocrinology and metabolis 20 (2016): 189-194.
- Nigil Haroon, Ammepa Anton, et al. Effect of vitamin D supplementation on glycemic control in patients with type 2 diabetes: a systematic review of interventional studies. Journal of Diabetes and Metabolic Disorders 14 (2015): 3.
- Mairead E Kiely, Joy Y Zhang, Michael Kinsella, Ali S Khashan, Louise C Kenny. Vitamin D status is associated with uteroplacental dysfunction indicated by pre-eclampsia and small-for-gestational-age birth in a large prospective pregnancy cohort in Ireland with low vitamin D status, The American Journal of Clinical Nutrition 104 (2016): 354-361.
- Lu-Lu Qin, Fang-Guo Lu, Sheng-Hui Yang, et al. Does Maternal Vitamin D Deficiency Increase the Risk of Preterm Birth: A Meta-Analysis of Observational Studies. Nutrients 8 (2016): 301
- De?Regil LM, Palacios C, Lombardo LK, Pena?Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database of Systematic Reviews (2016).
- Faustino R.Pérez-López, VinayPasupuleti, EdwardMezones-Holguin, et al. Effect of vitamin D supplementation during pregnancy on maternal and neonatal outcomes: a systematic review and meta-analysis of randomized controlled trials. Fertility and Sterility 103 (2015): 1278-1288.
- Leventis P, Kiely PDW. The tolerability and biochemical effects of high?dose bolus vitamin D2 and D3 supplementation in patients with vitamin D insufficiency. Scandinavian Journal of Rheumatology 38 (2009): 149-153.
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ 79 (2001): 373-374.
- Hutchinson K, Healy M, Crowley V, Louw M, Rochev Y. Verification of Abbott 25-OH-vitamin D assay on the architect system. Practical laboratory medicine 7 (2017): 27-35.
- Karras S, Paschou SA, Kandaraki E, Anagnostis P, et al. Hypovitaminosis D in pregnancy in the Mediterranean region: a systematic review. European Journal of Clinical Nutrition 70 (2016): 979-986.
- Marlene Chakhtoura, Maya Rahme, Nariman Chamoun, et al. Vitamin D in the Middle East and North Africa. Bone Reports 9 (2018): 120-121.
- Lai JK, Lucas RM, Clements MS, Harrison SL and Banks E. Assessing vitamin D status: Pitfalls for the unwary. Mol Nutr Food Res 54 (2010): 1062-1071.
- Ginde AA, Liu MC, Camargo CA. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Archives of internal medicine 169 (2009): 626-632.
- Mariam Omar, Faiza Nouh, Manal Younis, et al. Culture, Sun Exposure and Vitamin D Deficiency in Benghazi Libya. Journal of Advances in Medicine and Medical Research 25 (2018): 1-13.
