Prevalence and Clinical Outcome of Inborn Neonates with Hypoglycaemia at the Point of Admission as seen in Rivers State University Teaching Hospital, Nigeria
Article Information
West BA*, Aitafo JE
Department of Paediatrics, Rivers State University Teaching Hospital, Nigeria
*Corresponding Author: West BA, Department of Paediatrics, Rivers State University Teaching Hospital, Nigeria
Received: 26 November 2020; Accepted: 14 December 2020; Published: 21 December 2020
Citation:
West BA, Aitafo JE. Prevalence and Clinical Outcome of Inborn Neonates with Hypoglycaemia at the Point of Admission as seen in Rivers State University Teaching Hospital, Nigeria. Journal of Pediatrics, Perinatology and Child Health 4 (2020): 137-148.
Share at FacebookAbstract
Background: Neonatal hypoglycaemia is one of the commonest abnormalities of the newborn which, if unrecognized may result in poor neurologic development, poor intellectual functions, seizures or even death. This study was therefore carried out to determine the prevalence of hypoglycaemia, its’ associated risk factors and clinical outcome among inborn neonates.
Methodology: This prospective study was conducted in the Neonatal Unit of the Rivers State University teaching Hospital from April 2019 to March 2020.
Results: Of the 468 neonates admitted, 71 (15.2%) had hypoglycaemia with M:F ratio of 1.6:1. Hypoglycaemia was more common with presentations on the first day of life, those who commenced breastfeeding from day 2 of admission and above and had hypothermia. The commonest clinical features in hypoglycaemic neonates were difficulty in breathing (45.1%), seizures (7.0%) and cyanosis (5.6%), although there was no statistical significance (P>0.05). Maternal risk factors significantly associated with neonatal hypoglycaemia were Gestational Diabetes (P<0.0001) and Prolonged rupture of membranes (P=0.003). More neonates with probable sepsis, neonatal jaundice, prematurity and Macrosomia were hypoglycaemic though not of statistical significance (P>0.05). Of the 71 neonates with hypoglycaemia, 3 (4.2%) died.
Conclusion: Neonatal hypoglycaemia is still a common problem among inborn neonates in Rivers State University Teaching Hospital as evidenced by a prevalence of 15.2%. The common clinical features were difficulty breathing, seizures and cyanosis. Associated maternal risk factors were Gestational Diabetes and Prolonged rupture of membranes. Routine blood glucose screening of all sick neonates at point of admission is therefore advocated for early dete
Keywords
Hypoglycaemia, Prevalence, Inborn neonates, Clinical outcome, Port Harcourt
Hypoglycaemia articles; Prevalence articles; Inborn neonates articles; Clinical outcome articles; Port Harcourt articles
Article Details
1. Introduction
Neonatal hypoglycaemia (NNH) is one of the commonest metabolic abnormalities seen in the newborn [1-3]. If unrecognized or poorly treated it may result in poor neurologic development, poor intellectual function, motor deficits, seizure disorders or even death [4, 5]. The presentation of NNH is often variable and thus a high index of suspicion is required for diagnosis [5]. Affected neonates may present with non-specific clinical features such as poor suck, jitteriness, abnormal cry, fast breathing, hypotonia, apnea, convulsions and coma [3, 6, 7, 8]. The prevalence of NNH has been reported in 5-15% of otherwise healthy neonates [3, 9, 10]. Prevalence rates as high as 11-32.7% have been reported, especially when the study population included high risk infants in resource poor countries [3- 5, 11]. Risk factors for NNH include maternal Diabetes Mellitus, hypertension in pregnancy, septicaemia and prolonged labour. Other factors include prematurity, birth asphyxia, macrosomia, neonatal sepsis, cold stress and respiratory distress [4, 8, 12]. The outcome of neonates with hypoglycaemia depends on several factors including rapidity of onset, associated co-morbidities and adequacy of treatment [4, 8]. Whereas several studies have been done on NNH in developing countries and in Nigeria, [2-6, 11, 12] no recent study has been done in this part of the country; in particular, none has been done in our centre; Rivers State University Teaching Hospital (a tertiary hospital serving all the local governments in Rivers State and its environs). The present study was therefore conducted to determine the prevalence, its’ associated risk factors and clinical outcome of inborn neonates with hypoglycaemia in the Rivers State University Teaching Hospital, Nigeria.
2. Methodology
This was a prospective study conducted over one year (from April 2019 to March 2020) in the neonatal unit of the Rivers State University Teaching Hospital (RSUTH). The RSUTH the only state owned tertiary hospital is a 375 bedded hospital which serves as a referral for all the government owned primary health centres (PHC), general hospitals as well as private owned health facilities in the state and its environs. It consists of various departments such as Paediatrics, Obstetrics and gynaecology, surgery, internal medicine, pathology, radiology, physiotherapy, pharmacy and nursing. The department of Paediatrics consist of various specialties such as neonatology, nephrology, endocrinology, infectious and immunology, haem-oncology, pulmonology, cardiology, social, adolescent and community paediatrics. The neonatology unit which is run by 2 consultant paediatricians, resident doctors, house officers and nurse: patient ratio of 4:1 consist of 2 sections; the inborn and outborn sections. The inborn section which admits all neonates less than 28 days old whose mothers had antenatal care in RSUTH, PHC and government owned general hospitals and delivered in RSUTH, PHC and general hospitals consist of 23 cots, 7 incubators, 10 phototherapy machines, 2 resuscitaire as well as oxygen cylinders and oxygen concentrators. The outborn sections which admits all neonates less than 28 days old whose mothers did not receive ANC in RSUTH, PHC or any of the general hospital irrespective of their place of delivery consist of 7 cots, 3 incubators, 4 phototherapy machines, a resuscitaire and oxygen cylinders and oxygen concentrators.
Ethical clearance was obtained from the Rivers Sate Health Research Ethics Committee and informed consents were obtained from the parents/caregivers before commencement of the study. All inborn neonates whose parents/caregivers gave consent were consecutively recruited into the study. All outborn, inborn neonates whose parents did not give consent and those who had already received dextrose containing intravenous fluids were excluded from the study. A research proforma was administered to each recruited neonate. The information obtained included demographic characteristics of mothers and pregnancy history noting maternal risk factors for hypoglycaemia. The neonates age at admission, sex, birth order and gestational age obtained from the first day of the last menstrual cycle or from abdominal ultrasound scan done in the first trimester of pregnancy. Birth weight, temperature at presentation and clinical features were also recorded. Diagnosis was made based on the unit protocol either clinically with or without the use of laboratory investigations where necessary.
Random blood sugar level was performed at the point of admission using ACCU-CHEK Active glucometer device (Serial No. GB11802561). The glucometer strips were inserted into the glucometer and when the meter starts blinking, blood obtained from a heel prick of the patient (after cleaning with cotton and 70% alcohol) was applied to the test area of the strip. The blood sugar level was displayed in about 10 seconds and recorded. The blood sugar level of <2.6 mmol/l was considered hypoglycaemic [5-7]. All symptomatic hypoglycaemic babies were given a bolus of 4mls/kg of 10% Dextrose Water(DW) followed by continuous glucose infusion at the rate of 6-8 mg/kg/min until the patient recovered [8]. Those who were not symptomatic received an initial bolus of 2 mls/kg of 10% DW followed by continuous glucose infusion. Those who had no contraindications to oral feeding were fed and comorbidities treated according to the Unit’s protocol. Data was analysed using statistical package for the Social Sciences (SSPS) version 23. Data was presented as frequency and percentages for categorical variables and as mean and standard deviations for continuous variables. Statistical significance was placed at P value <0.05 at 95% confidence interval.
3. Results
3.1 Prevalence of hypoglycaemia at the point of admission among inborn neonates
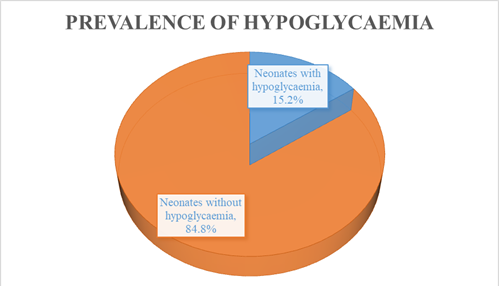
Of 468 neonates admitted during the period of study, 71 (15.2%) had hypoglycaemia while 397 (84.8%) did not have hypoglycaemia, Figure 1.
3.2 Socio-demographic characteristics of neonates with hypoglycaemia
Of 71 neonates with hypoglycaemia, males predominated 44 (62.0%) with Male: Female ratio of 1.6:1. Majority presented within 24 hours of life, 70 (98.6%) and were of 1st birth order, 28 (39.4%). The mean age at presentation was 3.07 ± 8.53 hours and mean birth order of 1.99 ± 1.05. Hypoglycaemia was mostly seen in neonates with gestational age 37-42 weeks, 38 (53.6%), birth weights <2.5 kg and 2.5-3.99 kg, 29 (40.8% each) and those fed from day 2 of admission and above, 44 (62.0%). The mean gestational age was 36.62 ± 2.49 weeks. Neonates with temperature at presentation <36°C were mostly hypoglycaemic, 40 (56.3%) with mean temperature at presentation being 35.79 ± 0.61°C, Table 1.
3.3 Association of neonatal hypoglycaemia with maternal risk factors
Hypoglycaemia was observed mostly in neonates of mothers with prolonged rupture of membranes 20 (28.2%), gestational diabetes 20 (28.2%) and hypertension 18 (25.5%). Neonatal hypoglycaemia was significantly associated with infants of mothers with gestational diabetes (P value <0.0001) and prolonged rupture of membranes (P value = 0.003), Table 2.
3.4 Comparison of Clinical features in neonates with and without hypoglycaemia
The commonest clinical features seen in neonates with hypoglycaemia at the point of admission were difficulty in breathing 32 (45.1%), seizures 5 (7.0%) and cyanosis 4 (5.6%) while the least was altered consciousness 1 (1.4%). There was no statistical difference in the clinical features among neonates with and without these clinical features, Table 3.
3.5 Comparison of Neonatal risk factors in neonates with or without hypoglycaemia
Neonatal hypoglycaemia was significantly associated with infants of diabetic mothers, P value <0.0001. More neonates with probable sepsis, neonatal jaundice, macrosomia, birth trauma and meningitis had hypoglycaemia although there was no statistical significance, P value >0.05 (Table 4).
3.6 Outcome of neonates with hypoglycaemia
Of 71 inborn neonates with hypoglycaemia, 67 (94.4%) were discharged home, 1 (1.4%) was discharged against medical advice while 3 (4.2%) died, Table 5.
|
Variables |
Frequency, n=71 (%) |
|
Sex |
|
|
Male |
44 (62.0) |
|
Female |
27 (38.0) |
|
Age at presentation (hours) |
|
|
< 24 |
70 (98.6) |
|
≥ 24 |
1 (1.4) |
|
Birth order |
|
|
1st |
28 (39.4) |
|
2nd |
27 (38.1) |
|
3rd and above |
16 (22.5) |
|
Gestational age (weeks) |
|
|
< 37 |
31 (43.6) |
|
37-42 |
38 (53.6) |
|
> 42 |
2 (2.8) |
|
Birth weight (kg) |
|
|
< 2.5 |
29 (40.8) |
|
2.5-3.99 |
29 (40.8) |
|
≥ 4 |
13 (18.4) |
|
Commencement of breastfeeding |
|
|
Day 1 |
27 (38.0) |
|
Day 2 and above |
44 (62.0) |
|
Temperature at presentation (°C) |
|
|
< 36 |
40 (56.3) |
|
36-37.4 |
30 (42.3) |
|
≥ 37.5 |
1 (1.4) |
Table 1: Socio-demographic characteristics of neonates with hypoglycaemia.
|
Maternal risk factors |
Total |
Neonates with Hypoglycaemia n=71 (%) |
Neonates without hypoglycaemia n=397 (%) |
P value |
|
Hypertension |
95 |
18 (25.4) |
77 (19.4) |
0.250 |
|
PROM |
76 |
20 (28.2) |
56 (14.1) |
0.003* |
|
Gestational diabetes |
57 |
20 (28.2) |
37 (9.3) |
<0.0001* |
|
Chorioamnionitis |
26 |
3 (4.2) |
23 (5.8) |
0.782 |
|
Antepartum haemorrhage |
18 |
1 (1.4) |
17 (4.3) |
0.333 |
|
Peripartum pyrexia |
16 |
1 (1.4) |
15 (3.8) |
0.486 |
|
Oligohydramnios |
9 |
2 (2.8) |
7 (1.8) |
0.632 |
|
HIV |
5 |
2 (2.8) |
3 (0.8) |
0.167 |
|
Hepatitis B infection |
4 |
1 (1.4) |
3 (0.8) |
0.483 |
HIV=Human immunodeficiency virus
Table 2: Association of neonatal hypoglycaemia with maternal risk factors.
|
Clinical features |
Total |
Neonates with Hypoglycaemia n= 71 (%) |
Neonates without hypoglycaemia n=397 (%) |
P value |
|
Difficulty in breathing |
208 |
32 (45.1) |
176 (44.4%) |
0.922 |
|
Seizures |
25 |
5 (7.0) |
20 (5.0) |
0.563 |
|
Cyanosis |
13 |
4 (5.6) |
9 (2.3) |
0.119 |
|
Vomiting |
17 |
2 (2.8) |
15 (3.8) |
1.000 |
|
Lethargy |
12 |
2 (2.8) |
10 (2.5) |
0.701 |
|
Jitteriness |
11 |
2 (2.8) |
9 (2.3) |
0.677 |
|
Apneoa |
9 |
1 (1.4) |
8 (2.0) |
1.000 |
|
Poor suck |
8 |
1 (1.4) |
7 (1.8) |
1.000 |
|
Altered consciousness |
4 |
1 (1.4) |
3 (0.8) |
0.483 |
Table 3: Comparison of Clinical features in neonates with and without hypoglycaemia.
|
Neonatal risk factors |
Total |
Neonates with hypoglycaemia |
Neonates without hypoglycaemia |
P value |
|
Probable sepsis |
265 |
42 (59.2) |
223 (56.2) |
0.640 |
|
Neonatal jaundice |
229 |
41 (57.7) |
188 (47.4) |
0.107 |
|
Prematurity |
215 |
31 (43.7) |
184 (46.3) |
0.700 |
|
Macrosomia |
72 |
13 (18.3) |
59 (14.9) |
0.458 |
|
Birth asphyxia |
54 |
6 (8.5) |
48 (12.1) |
0.377 |
|
Congenital malaria |
42 |
4 (4.2) |
39 (9.8) |
0.175 |
|
IDM |
42 |
17 (23.9) |
25 (6.3) |
<0.0001* |
|
Severe anaemia |
39 |
3 (4.2) |
36 (9.1) |
0.243 |
|
TTN |
18 |
1 (1.4) |
17 (4.3) |
0.333 |
|
Congenital abnormality |
15 |
1 (1.4) |
14 (3.5) |
0.711 |
|
Birth trauma |
10 |
2 (2.8) |
8 (2.0) |
0.653 |
|
Meningitis |
7 |
3 (4.2) |
4 (1.0) |
0.074 |
IDM=Infants of diabetic mother; TTN= Transient tachypnea of the newborn
Table 4: Comparison of Neonatal risk factors in neonates with or without hypoglycaemia.
|
Outcome (%) |
Frequency, n=71 |
|
Discharged |
67 (94.4%) |
|
DAMA |
1 (1.4) |
|
Died |
3 (4.2) |
DAMA=Discharged against medical advice
Table 5: Outcome of neonates with hypoglycaemia.
4. Discussion
The prevalence of hypoglycaemia among inborn neonates at the point of admission in the neonatal unit of the Rivers State University Teaching Hospital of 15.2% was considered high. This therefore supports the fact that hypoglycaemia is a common metabolic complication in the neonatal period. This prevalence is comparable to the 11% reported by Ochoga et al. [3] in Benue State, North western Nigeria but much lower than the 27.3%, 28.3%, 30.5%, 32.7%, 32.6%, 33.3% and 41% documented by Ogunlesi [13], Frank-Briggs et al. [11], Efe et al. [5], Dedeke et al. [4], De et al. [14], Thinesh et al. [15] and Pal et al. [16] in Ogun state, in a previous study carried out in Port Harcourt, Lafia (Nasarawa State), Ile-Ife in Nigeria, India and Nepal respectively. These varying prevalence rates could be attributable to the varying geographic locations, varying risk factors as well as difference in the inclusion criteria, screening methods and the cut-off values of random blood sugar used. The low prevalence reported by Ochoga et al. [3] could be because of the lower cut-off value of random blood sugar of < 2.2 mmol/L used unlike the present study, which used < 2.6 mmol/L and as such more babies were diagnosed hypoglycaemic. The higher prevalence of hypoglycaemia in the previous study in Port Harcourt done more than a decade ago could be attributed to the fact that cord blood estimation of random blood sugar was done for all babies at birth irrespective of their clinical status whereas in the present study capillary blood was used for the estimation of blood glucose in only sick babies admitted into the neonatal unit. The study by De et al. [14] and Thinesh et al. [15] in India involved the assessment of several samples for glucose estimation within the first 48hrs of life which could have accounted for the much higher prevalence of hypoglycaemia in their study unlike the present study where glucose estimation was done at the point of admission only. In addition, the present study assessed only inborn babies while most other studies assessed both inborn and outborn neonates accounting for the much higher prevalence as observed in the study by Dedeke et al. [4] and Ochoga et al. [3] which documented significantly higher proportion of referred neonates with hypoglycaemia than the inborn neonates. The prevalence obtained in the present study was however much higher than the 2.2% and 0.4% documented by Mukunya et al. [17] and Najate and Saboktakin [18] in Uganda and Iran respectively. The low prevalence in Uganda could be attributed to the fact that it was a community study of healthy newborns and as such the possibility of early commencement of breastfeeding as compared to the present study of sick neonates who may not have commenced feeds. The very low prevalence in the Iranian study could be because of their very large sample size of over 14,000 babies as compared to the much smaller sample size used in the present study.
More males had hypoglycaemia in the present study with a M:F ratio of 1.6:1. This trend was also reported in other studies in Nigeria [3, 4], India [14, 19] and Iran [18]. Contrary to the present study, a descriptive cross-sectional study in Nasarawa state [5], Nigeria documented an equal sex ratio. The reason for this difference could not be ascertained.
About half of term neonates (gestational age = 37-42 weeks) had hypoglycaemia followed by the late preterm babies which constituted more than a third of cases. Hypoglycaemia was also reported as being commoner in term neonates by Thinesh et al. [15] in India. This is contrary to most other studies [4, 14, 18] which documented a predominance of hypoglycaemia in the preterms. The reason for the predominance of hypoglycaemia in the term babies as compared to the preterms could not however be ascertained. A third of late preterm neonates had hypoglycaemia in the present study. This is because preterms have limited glycogen and fat stores with higher metabolic demands because of their relatively large brain size and their inability to mount a counter regulatory response to hypoglycaemia [20]. These babies also have immature glycogenolytic and gluconeogenesis enzymes coupled with delayed onset of feeding as a result of prematurity.
The incidence of hypoglycaemia was same in the low birth weight and normal weight babies. This was contrary to other studies [4, 14, 18] where hypoglycaemia predominated in the low birth weight group.
It is not surprising that neonates who commenced feeding by the 2nd day of admission and above had hypoglycaemia much more than neonates who commenced feeds on the 1st day. Similar observation was made in Nasarawa state [5] in Nigeria, where neonates with feeding intolerance were more hypoglycaemic than neonates who were tolerating feeds. This was also the case with Ochoga et al. [3], Dedeke et al. [4], De et al. [14], Pal et al. [16] and Bhand et al. [19]. This is because there is usually a rapid depletion of glucose reserves in the face of feeding challenges as neonates have a limited capacity to store glucose [10]. This thus emphasizes the importance of commencing breastfeeding within 1 hour of delivery as recommended by the World Health Organization [21, 22]. This practice reduces neonatal morbidity and mortality as well as prevents the adverse neurological sequelae secondary to hypoglycaemia [21, 22]. It is worthy of note that breastfeeding has been shown to be an initial means of correction of neonatal hypoglycaemia [23].
Neonates with hypothermia with temperature <36°C had more hypoglycaemia in the present study as also observed by Ochoga et al. [3], Dedeke et al. [4] and Bhand et al. [19]. This is because cold neonates use up more glycogen thereby leading to hypoglycaemia. It is pertinent to note that Ochoga et al. [3] reported hypothermia as a significant risk factor for hypoglycaemia.
Hypoglycaemia was observed more in the present study in neonates whose mothers had hypertension in pregnancy, prolonged rupture of membranes, gestational diabetes, oligohydramnios, HIV infection and hepatitis B infection in descending order. Ochoga et al. [3], Thinesh et al. [15] and Bhand et al. [19] also observed eclampsia and maternal diabetes mellitus as the commonest maternal risk factors followed by intrapartum administration of glucose and maternal drug uses whereas Frank-Briggs et al. [11] reported pre-eclampsia and prolonged obstructed labour as the commonest maternal risk factors. The varying maternal risk factors could be because of varying geographic locations and their level of obstetric care. There was no significant association of neonatal hypoglycaemia with the maternal risk factors in the study by Ochoga et al. [3]. This was, however contrary to the present study which showed significant association of hypoglycaemia with neonates whose mothers had gestational diabetes and prolonged rupture of membranes thus a high index of suspicion is needed for neonates whose mother had these risk factors.
The commonest clinical features of neonates with hypoglycaemia was difficulty in breathing followed by seizures and cyanosis while the least was altered consciousness. A previous study carried out more than a decade ago in Port Harcourt by Frank-Briggs et al. [11] also documented respiratory distress and cyanosis as the commonest clinical features observed in neonates with hypoglycaemia. Ochoga et al. [13], however documented a significant association between hypoglycaemia with tachypnea and seizures. The present study however did not find any statistical association between hypoglycaemia with any of the clinical features. This might not be surprising as the clinical features of hypoglycaemia are non-specific and thus common to other morbidities. It is also interesting to note that Ochoga et al. [3] observed that all the clinical features observed in neonates with hypoglycaemia were also seen in the neonates without hypoglycaemia as also observed in the present study. Contrary to the present study, however, floppiness, poor suck and respiratory distress were the commonest clinical features observed by Dedeke et al. [4]. In this study, hypoglycaemia was significantly associated with poor suck, cyanosis, convulsions and pallor. In addition, Bhand et al. [19] documented jitteriness as the commonest clinical feature observed in hypoglycaemic neonates followed by lethargy, temperature instability and cyanosis.
Hypoglycaemia was observed mostly in neonates with probable sepsis followed by neonatal jaundice, prematurity, macrosomia, infants of diabetic mothers, birth trauma and meningitis. There was however statistical significance only in neonates with hypoglycaemia secondary to infants of diabetic mothers. Efe et al. [5] also observed that neonatal sepsis, birth asphyxia and neonatal jaundice had no statistical association with hypoglycaemia. The commonest diagnosis at admission in hypoglycaemic and non-hypoglycaemic neonates observed by Dedeke et al. [4] were preterm delivery, birth asphyxia and septicaemia. Hypoglycaemia in their study [4] was significantly more frequent among preterm babies. Ochoga et al. [3] documented hypoglycaemia in neonates with prematurity, jaundice, birth asphyxia, respiratory distress and congenital heart disease. In this study, hypoglycaemia was significantly more frequent among neonates with prematurity and respiratory distress. Najate and Saboktakin [18] documented prematurity as the commonest cause of hypoglycaemia followed by infants of diabetic mothers, sepsis, asphyxia and neonatal hyperinsulinism. These differences in the disease pattern in neonates with hypoglycaemia could be due to differences in the geographic locations, diagnostic criteria, study designs and varying risk factors.
Hypoglycaemia is a significant cause of neonatal mortality if not treated promptly as observed in the present study, which revealed a rate of 4.2%. This rate is much lower than the 23.3% and 53.8% reported by Dedeke et al. [4] and Najate and Saboktakin [18]. The high mortality rates reported in the latter studies could be because of the difference in the inclusion criteria as the latter studies included both inborn and outborn babies contrary to the present study where only inborn babies were recruited. This low mortality in the present study could be because of the high index of suspicion in the neonatal unit of the Rivers State University Teaching Hospital as glucose estimation is routinely done for all neonates at the point of admission and such babies treated promptly. This protocol is strictly followed in our unit because of the consequences of hypoglycaemia, as delay in diagnosis and treatment could lead to long term neurological sequelae such as seizure disorders, cerebral palsy, learning disabilities, developmental problems and even death [24-26].
5. Conclusion
Neonatal hypoglycaemia is still a common metabolic problem evidenced by the high prevalence observed among inborn neonates at the point of admission in the Rivers State University Teaching Hospital of 15.2%. The clinical features of neonates with hypoglycaemia are non-specific with the commonest being difficulty in breathing, seizures and cyanosis. Gestational diabetes and prolonged rupture of membranes are maternal risk factors associated with neonatal hypoglycaemia. The mortality of inborn neonates with hypoglycaemia was low being 4.2%. Routine blood glucose screening of sick neonates at the point of admission into neonatal units is therefore advocated for early detection and prompt treatment of hypoglycaemia.
References
- Adamkin DH. Postnatal glucose homeostasis in late preterm and term infants. A clinical report from the American Academy of Paediatrics, committee on foetus and newborn paediatrics. Paediatrics 127 (2011): 575-579.
- Kerstjens JM, Bocca-Tjeertes IF, de Winter AF, et al. Neonatal Morbidities and Developmental delay in moderately Pre-term born children. Paediatrics 130 (2012): 265-272.
- Ochoga MO, Aondoaseer M, Abah RO, et al. Prevalence of Hypoglycaemia in Newborn at Benue State University Teaching Hospital, Makurdi, Benue State, Nigeria. Open J Paediatr 8 (2018): 189-198.
- Dedeke IOF, Okeniyi JAO, Owa JA, et al. Point-of-admission neonatal hypoglycaemia in a Nigerian tertiary hospital: incidence, risk factors and outcome. Nig J Paediatr 38 (2011): 90-94.
- Efe A, Sunday O, Surajudeen B, et al. Neonatal hypoglycaemia: prevalence and clinical outcome in a tertiary health facility in North-central Nigeria. Int J Health Sci Res 9 (2019): 246-251.
- Abdelwaheb M, Veronique GD, Anne MN, et al. Hypoglycaemia in term newborns with a birthweight below the 10th percentile. Paediatr Child Health 15 (2010): 271-275.
- World Health Organization. Division of child health and development and maternal and newborn health/safe motherhood. Hypoglycaemia of the newborn: review of literature. Geneva: World Health Organization (1997).
- Sperling MA. Hypoglycaemia. In Eds.: Kleigman RM, Stanton BF, Geme JW, et al. Nelson textbook of Paediatrics. 20th Philadelphia: Elsevier Saunder (2011): 773-788.
- Cornblath M, Hawdon JM, Williams AF, et al. Controversies regarding Definition of Neonatal Hypoglycaemia: Suggested Operational thresholds. Paediatrics 105 (2000): 1141-1145.
- Hay WW, Raju T, Higgins R, et al. Knowledge Gaps and Research Needs for Understanding and Treating Neonatal Hypoglycaemia. J Paediatrics 155 (2009): 612-617.
- Frank-Briggs AI, Ojule AC and Nkanginieme KE. Neonatal hypoglycaemia: Prevalence and clinical Manifestations in Port Harcourt, Nigeria. Port Harcourt Med J 2 (2008): 166-170.
- Williams AF. Hypoglycaemia in the newborn: a review. Bull World Health Org 75 (1997): 261-290.
- Ogunlesi T. Mortality within the first 24 hours of admission among neonates aged less than 24 hours in a special care baby unit (SCBU) in Nigeria: The role of significant hypothermia and hypoglycaemia. Iran J Neonatol 6 (2015): 1-8.
- De KA, Biswas R, Samanta M, et al. Study of blood glucose levels in normal low birth weight newborns and impact of early breastfeeding in a tertiary care centre. Ann Nig Med 5 (2011): 53-58.
- Thinesh KJ, Valdeesuwaran M, Arasar ST. Incidence of hypoglycaemia in newborns with risk factors. Inter J Contemp Pediatr 5 (2018): 1952-1955.
- Pal DK, Manandhar DS, Rajbhandaris S, et al. Neonatal hypoglycaemia in Nepal: Prevalence and risk factors. Arch Dis Child Fetal Neonatal Ed 82 (2000): 46-51.
- Mukunya D, Odongkara B, Piloya Y, et al. Prevalence and factors associated with neonatal hypoglycaemia in northern Uganda: A cross-sectional study. Trop Med Health 89 (2020):
- Najati N, Saboktakin L. Prevalence and underlying aetiologies of neonatal hypoglycaemia. Pakistan J Biol Sci 13 (2010): 753-756.
- Bhand SA, Sheikh F, Siyal AR, et al. Neonatal hypoglycaemia; Presenting pattern and risk factors of neonatal hypoglycaemia. Professional Med J 21 (2014): 745-749.
- Sharmer A, Davis A, Shekhawdt PS. Hypoglycaemia in the preterm neonate: Aetiopathogenesis, diagnosis, management and long-term outcomes. Transl Pediatr 6 (2017): 335-348.
- Neovita study group. Timing of invitation, patterns of breastfeeding and infant survival: Prospective analysis of pooled data from three randomised trials. Lancet. Glob Health 4 (2016): e266-275.
- World Health Organization, Nutrition: Ten steps to successful breastfeeding (revised 2018). Geneva: World Health Organization (2019).
- Jain A, Aggarwal R, Jeevasanker M, et al. Hypoglycaemia in the newborn. Indian J Pediatr 75 (2008): 63-67.
- Haworth JC, McRae KN. The neurological and developmental effects of neonatal hypoglycaemia: a follow up of 22 cases. Can Med Ass J 92 (1965): 861-865.
- Cryper PE. Glucose homeostasis and hypoglycaemia. In Eds.: Wilson JD, Foster DW. Williams Textbook of Endocrinology, 8th Philadelphia: WB Saunders (1992): 1223-12253.
- Lucas A, Morley R, Cole TJ. Adverse neurodevelopment outcome of moderate neonatal hypoglycaemia. BMJ 297 (1988): 1304-1308.