Possibilities of Resting State Functional Magnetic Resonance Imaging in the Assessment of the Functional State of the Brain in Patients with Opioid Addiction
Article Information
Tarumov D2, Trufanov A1,2*, Chakchir O1, Abdulaev SH2, Partsernyak A2, Efimtsev A3, Bystrova D1, Kurasov E2, Shamrey V2, Zhelezniak I2
1Saint Petersburg Academic University, Saint Petersburg, Russia
2Russian Military-medical academy, Saint Petersburg, Russia
3Almazov National Medical Research Centre, Saint Petersburg, Russia
*Corresponding Authors: Dr. Artem Trufanov, Saint Petersburg Academic University, Saint Petersburg, Russia
Received: 21 July 2019; Accepted: 05 August 2019; Published: 08 August 2019
Citation: Tarumov D, Trufanov A, Chakchir O, Abdulaev SH, Partsernyak A, Efimtsev A, Bystrova D, Kurasov E, Shamrey V, Zhelezniak I. Possibilities of Resting State Functional Magnetic Resonance Imaging in the Assessment of the Functional State of the Brain in Patients with Opioid Addiction. Journal of Psychiatry and Psychiatric Disorders 3 (2019): 168-178.
Share at FacebookAbstract
Background and Purpose: The opioid addiction is among the most often found types of addictive pathology conceding on prevalence only to an alcohol addiction. To estimate the functional state of the brain in patients with opioid dependence syndrome using fMRI.
Materials and Methods: 82 men were examined, 64 of them aged 30.9+2.6 years having opioid dependence syndrome (F11.2). The control group (CG) included 18 healthy. Functional MRI was performed on Siemens Espree 1.5T MRI system using the BOLD technique. Based on the MATLAB (Neural Network Toolbox) software, the CONN Functional Connectivity Toolbox 17 was started, which preprocessed the received data separately for each study. Next was the stage of noise reduction and two-level processing, a correlation was estimated based on the "interested" areas (ROI-to-ROI).
Results: In all patients suffering from opioid addiction, at resting-state fMRI, "oppression" of functional connections is noted in comparison with the normals. These changes are noted both in the default mode networks, and in the cortical and subcortical structures, which indicate: a violation of control functions, making the right decision, thinking, cognitive and emotional components in narcotic drug addicts.
Conclusions: The obtained data on functional changes in brain structures in patients suffering from opioid addiction will help to clarify the pathogenetic mechanisms of this pathology, with the possibility of subsequent development of basic objective diagnostic criteria of the opioid dependence syndrome, excluding the subjectivity of a narcologist at the stage of drawing up an expert opinion.
Keywords
Epigenetics; Attachment; Neuropsychiatric disorders; Cardiometabolic disorder
Epigenetics articles, Attachment articles, Neuropsychiatric disorders articles, Cardiometabolic disorder articles
Epigenetics articles Epigenetics Research articles Epigenetics review articles Epigenetics PubMed articles Epigenetics PubMed Central articles Epigenetics 2023 articles Epigenetics 2024 articles Epigenetics Scopus articles Epigenetics impact factor journals Epigenetics Scopus journals Epigenetics PubMed journals Epigenetics medical journals Epigenetics free journals Epigenetics best journals Epigenetics top journals Epigenetics free medical journals Epigenetics famous journals Epigenetics Google Scholar indexed journals Attachment articles Attachment Research articles Attachment review articles Attachment PubMed articles Attachment PubMed Central articles Attachment 2023 articles Attachment 2024 articles Attachment Scopus articles Attachment impact factor journals Attachment Scopus journals Attachment PubMed journals Attachment medical journals Attachment free journals Attachment best journals Attachment top journals Attachment free medical journals Attachment famous journals Attachment Google Scholar indexed journals Neuropsychiatric disorders articles Neuropsychiatric disorders Research articles Neuropsychiatric disorders review articles Neuropsychiatric disorders PubMed articles Neuropsychiatric disorders PubMed Central articles Neuropsychiatric disorders 2023 articles Neuropsychiatric disorders 2024 articles Neuropsychiatric disorders Scopus articles Neuropsychiatric disorders impact factor journals Neuropsychiatric disorders Scopus journals Neuropsychiatric disorders PubMed journals Neuropsychiatric disorders medical journals Neuropsychiatric disorders free journals Neuropsychiatric disorders best journals Neuropsychiatric disorders top journals Neuropsychiatric disorders free medical journals Neuropsychiatric disorders famous journals Neuropsychiatric disorders Google Scholar indexed journals Cardiometabolic disorder articles Cardiometabolic disorder Research articles Cardiometabolic disorder review articles Cardiometabolic disorder PubMed articles Cardiometabolic disorder PubMed Central articles Cardiometabolic disorder 2023 articles Cardiometabolic disorder 2024 articles Cardiometabolic disorder Scopus articles Cardiometabolic disorder impact factor journals Cardiometabolic disorder Scopus journals Cardiometabolic disorder PubMed journals Cardiometabolic disorder medical journals Cardiometabolic disorder free journals Cardiometabolic disorder best journals Cardiometabolic disorder top journals Cardiometabolic disorder free medical journals Cardiometabolic disorder famous journals Cardiometabolic disorder Google Scholar indexed journals pathogenetic mechanisms articles pathogenetic mechanisms Research articles pathogenetic mechanisms review articles pathogenetic mechanisms PubMed articles pathogenetic mechanisms PubMed Central articles pathogenetic mechanisms 2023 articles pathogenetic mechanisms 2024 articles pathogenetic mechanisms Scopus articles pathogenetic mechanisms impact factor journals pathogenetic mechanisms Scopus journals pathogenetic mechanisms PubMed journals pathogenetic mechanisms medical journals pathogenetic mechanisms free journals pathogenetic mechanisms best journals pathogenetic mechanisms top journals pathogenetic mechanisms free medical journals pathogenetic mechanisms famous journals pathogenetic mechanisms Google Scholar indexed journals pathology articles pathology Research articles pathology review articles pathology PubMed articles pathology PubMed Central articles pathology 2023 articles pathology 2024 articles pathology Scopus articles pathology impact factor journals pathology Scopus journals pathology PubMed journals pathology medical journals pathology free journals pathology best journals pathology top journals pathology free medical journals pathology famous journals pathology Google Scholar indexed journals magnetic resonance imaging articles magnetic resonance imaging Research articles magnetic resonance imaging review articles magnetic resonance imaging PubMed articles magnetic resonance imaging PubMed Central articles magnetic resonance imaging 2023 articles magnetic resonance imaging 2024 articles magnetic resonance imaging Scopus articles magnetic resonance imaging impact factor journals magnetic resonance imaging Scopus journals magnetic resonance imaging PubMed journals magnetic resonance imaging medical journals magnetic resonance imaging free journals magnetic resonance imaging best journals magnetic resonance imaging top journals magnetic resonance imaging free medical journals magnetic resonance imaging famous journals magnetic resonance imaging Google Scholar indexed journals resting state functional magnetic resonance imaging articles resting state functional magnetic resonance imaging Research articles resting state functional magnetic resonance imaging review articles resting state functional magnetic resonance imaging PubMed articles resting state functional magnetic resonance imaging PubMed Central articles resting state functional magnetic resonance imaging 2023 articles resting state functional magnetic resonance imaging 2024 articles resting state functional magnetic resonance imaging Scopus articles resting state functional magnetic resonance imaging impact factor journals resting state functional magnetic resonance imaging Scopus journals resting state functional magnetic resonance imaging PubMed journals resting state functional magnetic resonance imaging medical journals resting state functional magnetic resonance imaging free journals resting state functional magnetic resonance imaging best journals resting state functional magnetic resonance imaging top journals resting state functional magnetic resonance imaging free medical journals resting state functional magnetic resonance imaging famous journals resting state functional magnetic resonance imaging Google Scholar indexed journals default mode network articles default mode network Research articles default mode network review articles default mode network PubMed articles default mode network PubMed Central articles default mode network 2023 articles default mode network 2024 articles default mode network Scopus articles default mode network impact factor journals default mode network Scopus journals default mode network PubMed journals default mode network medical journals default mode network free journals default mode network best journals default mode network top journals default mode network free medical journals default mode network famous journals default mode network Google Scholar indexed journals medial prefrontal cortex articles medial prefrontal cortex Research articles medial prefrontal cortex review articles medial prefrontal cortex PubMed articles medial prefrontal cortex PubMed Central articles medial prefrontal cortex 2023 articles medial prefrontal cortex 2024 articles medial prefrontal cortex Scopus articles medial prefrontal cortex impact factor journals medial prefrontal cortex Scopus journals medial prefrontal cortex PubMed journals medial prefrontal cortex medical journals medial prefrontal cortex free journals medial prefrontal cortex best journals medial prefrontal cortex top journals medial prefrontal cortex free medical journals medial prefrontal cortex famous journals medial prefrontal cortex Google Scholar indexed journals
Article Details
Abbreviations:
MRI – magnetic resonance imaging; RS-fMRI – resting state functional magnetic resonance imaging; DMN – default mode network; MPFC – medial prefrontal cortex; PCC – posterior cingulate cortex; LP – inferior parietal and temporal lobes1. Introduction
The opioid addiction is among the most often found types of addictive pathology conceding on prevalence only to an alcohol addiction [1, 2]. Separately taken ways and methods of early identification of the persons using opioid narcotic drugs are less informative and don't answer current trends in the growth of addictive pathology, which demands revision of this concept in general from the point of view of complex diagnostics of these conditions. It causes expediency of search for additional (to existing clinical-psychopathological and laboratory) complex diagnostic methods of addictive disorders (primarily opioid and alcohol addiction) including psychological, laboratory and objectifying instrumental methods, including functional and structural neuroimaging. At the same time, views on the etiology and pathogenesis of the opioid dependence syndrome often don't coincide. Introduction in clinical practice of functional radiological methods of neuroimaging can help in studying the pathophysiological mechanisms of the formation of addictions and in the assessment the effectiveness of its treatment [1, 2].
In recent years a new type of functional magnetic resonance imaging (fMRI), a resting state functional MRI, has become more and more applicable in studying of emotional, sensory and cognitive processes in cases of the central nervous system pathology and in normal conditions. RS-fMRI allows evaluating the functional connectivity, which characterizes the functional connectivity of remote brain regions, which in turn helps to understand the functional organization of the brain. Low-frequency fluctuations of temporary sequences are at the heart of signal acquisition, when conducting the resting-state fMRI.
Unlike methods of a research dependent on performance of a cognitive load, the use of resting-state fMRI is especially favorable as it doesn't require active participation of a patient which allows to exclude subjectivity and to investigate local neuronic reactions and interregional communications for all areas of a brain within the same research protocol [3]. Resting-state functional MRI helps to look more broadly at the functional connections between different parts of the central nervous system both in norm and in pathology of various genesis. In the coming years, functional connectivity can become the basis for the development of biomarkers of mental disorders and neurodegenerative diseases, as well as for evaluating the effectiveness of the therapy [4, 5]. The default mode network (DMN) is associated with the processes of control and thinking, including emotional and its cognitive components, and consists of the medial prefrontal cortex (MPFC), posterior regions of a cingulate gyrus, precuneus (PCC), inferior parietal and temporal lobes (LP) [4].
Heroin dependence is a severe recurrent disorder associated with impaired cognitive control over a dose and frequency of use of this psychoactive substance and formed abstinence syndrome [6]. In case of chronic narcotic or alcohol intoxication, the anterior areas of the brain are in a single complex closed state of excitation with the participation of systems of "reward", "motivation to action", "emotional memory," and "cognitive control." The "reward" system is located in the additional core and the pale globe; the system of "motivation to action" is in the orbitofrontal and subcallosal cortex; the system of "emotional memory" is in the amygdala and hippocampus; the system of "cognitive control" is in the prefrontal and orbitofrontal cortex and the anterior cingulate cortex. It is supposed that depression of sensitivity of the “rewards” system to natural incentives, disturbance the activity and weakening the system of "cognitive control," or, on the contrary, increasing the activity of "emotional memory" and "motivation to action" systems lead to "closure of the addictive circle" and the development of dependence. Decision-making function is carried out in several areas of a brain [7, 8] and may require the exchange of information through the motor, emotional and cognitive cortical areas [9, 10]. Two separate, but interconnected functional ways make their contribution and promote making a "healthy" decision for the drug-addict. The first one is the way "from top to down" proceeding from a frontal cortex which exercises executive control over compulsive impulses of subcortical structures (for example, from a corpus striatum) [11, 12]. The second is the "bottom-up" way coming from subcortical structures which try to overcome inhibition of a cortex [13, 14]. Thus, the functional integrity of cortical and subcortical patterns is a key component in the ability to choose the right actions appropriate to a specific situation, in particular, related to abstinence from taking narcotic drugs.
2. Research Objective
To estimate the functional state of the brain in patients with opioid dependence syndrome using fMRI.
3. Materials and Methods
For the purpose of the study, 82 males were selected, 64 of them aged 30.9 ± 2.6 years having opioid dependence syndrome (F11.2). For 9.1 ± 3.4 years they were receiving treatment at the psychiatry clinic and at toxicology department of the interdistrict Narcological Dispensary No. 2 and Psychiatry Department of S. M. Kirov Military Medical Academy. All patients were examined by an addiction psychiatrist who confirmed the availability of criteria for inclusion in the experiment. The MRI study was performed at the Department of Rentgenology and Radiology of S. M. Kirov Military Medical Academy.
The control group (CG) included 18 healthy subjects at the age of 27.7 ± 1.3 years. For the purpose of the subsequent optimal processing of the neurofunctional data, all patients suffering from the opioid addiction syndrome were divided into two subgroups according to the prescription of narcotic drug discontinuation: 1st subgroup - 16 patients in the state of heroin intoxication, 2nd subgroup - 15 patients with remission of up to 1 month.
All subjects were informed of the ongoing research and signed informed voluntary consent. The criterion for exclusion from the experiment was the presence of coarse morphological changes in the brain, confirmed by MRI, and the refusal to conduct the study. Four patients from the second subgroup received supportive therapy with antidepressants from the group of selective serotonin reuptake inhibitors. Therefore, 5 days before the planned study, they voluntarily stopped taking medications, and after the MRI, they immediately resumed the treatment. Patients from the first subgroup (the state of intoxication) received opioids (Tramadol at a dose of up to 250 mg/day) as part of short-term replacement therapy to reduce the severity of withdrawal symptoms. The study also included patients diagnosed with acute parenteral opioid poisoning delivered by ambulance to the toxicology department of the clinic of military therapy.
The study was conducted in two stages. At the first stage the selection of patients with a diagnosis of opioid dependence syndrome, studying their medical records, collecting anamnesis, determining the actual condition of the patient, and the length of use of narcotic drugs were carried out for the fMRI procedure. Patients under the age of 18 and older than 40 years who abused other non-opioid psychoactive substances were not included in the second stage of the study. During the second stage, resting state fMRI was performed using the BOLD technique. Traditional MRI sequences were used for the morphological evaluation of the brain and the sequence of ISOTROPIC-FE 3D was used to map activation patterns to the brain structures. When the MRI was performed, the patient was lying on the back in the MRI machine; the scanning area was the head, the head coil was used. When scanning, the patient was instructed not to think about anything and not to move. When the resting state fMRI was performed, the patient was in a state of complete rest for 6 minutes without any stimuli.
Then postprocessing and statistical analysis followed. Initially, the image files in the DICOM format were obtained. Using the “MRIConvert” program, the file format was changed from DICOM to NIFTI. Based on the MATLAB 2016a software, the CONN Functional Connectivity Toolbox 17 was installed and started, which preprocessed the received data separately for each study. The preprocessing stage included motion correction (realignment), spatial normalization and image smoothing according to the requirements of the software (Figure 1).
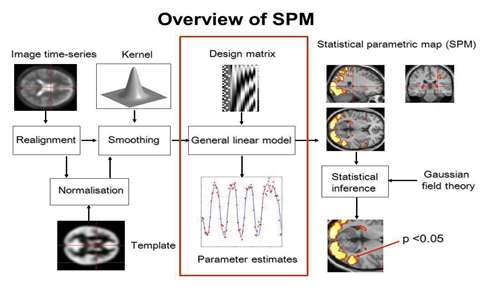
Figure 1: Processing of functional data by means of statistical parametric mapping.
During the preprocessing stage the images of each examinee were transformed to the standardized anatomical space. Spatial normalization of the images was carried out by creating a standard template using affine hard and nonlinear transformations (deformation or curvature of images for 3D processing). The affine transformation was carried out by 12 parameters (3 image displacements, 3 movements in space, 3 rotations along the x, y, z axes and 3 changes of the image size). The initial size of the voxel was 2 × 2 × 2 mm. After the stage of spatial normalization, a Gaussian smoothing with a half-width of 8 mm along the X, Y, and Z axes was performed. The changes in each voxel were estimated in accordance with the general linear model. Following the stage of noise reduction and two-level processing, a correlation was estimated based on the "interested" areas (ROI-to-ROI). As a result, 2 statistical t-cards were constructed from the reconstructed, normalized and smoothed images, characterizing the activation and functional inhibition of the brain structures, respectively, in response to the presentation of the stimulus material described above. The next stage was group analysis, during which a single-sample t-test was used to identify typical changes in the B.O.L.D.-signal for each group, obtaining parametric maps for each of them. The level of statistical significance did not exceed the threshold of p=0.05 for p-FDR (the false detection limit is the probability of false-positive connectivity between voxels, False Discovery Rate). For each patient, the number and location of activation areas in the projection of the brain substance was determined. The results were presented in a graphic form with the presence of illustrations of the activation areas in the projection of the brain in three planes, combining with anatomical structures, indicating the structures, as well as projecting to a three-dimensional reconstruction of the surface of the brain. Based on the obtained data, a graphical representation of the functional connections between the brain structures in the form of a connectome and in a 3D format was modeled, indicating the dominant structures and the intensity of the connectivity between themselves.
All the listed stages of processing of the neurofunctional data presented high requirements to the hardware component. The analysis was carried out using iMac Pro with an Intel Xeon (8-core/32-thread) processor and a 32 GB of RAM, based on the MacOS Sierra operating system.
4. Results and Discussion
It was established that all patients with opioid addiction syndrome in comparison with the control group showed weakening of functional communications of all DMN structures (pFDR <0.05). At the same time, changes in DMN in MPFC and PCC were more expressed in the patients of the first subgroup, and changes in DMN in LP were mostly expressed in the patients of the second subgroup. Normally, the medial prefrontal cortex participates in the processes of decision making and regulation of emotions. In the control group, it had functional connections with the medial frontal cortex, the left and right frontal pole, the left and right orbitofrontal cortex, the left nucleus accumbens, the right and left paracingulate gyrus. In this case, in patients who were in intoxication, functional connections in DMN (MPFC) became statistically weakened. It was revealed that the functional connection of the medial prefrontal cortex with the precuneus was increased in patients with early remission (Table 1). In the group of patients with the remission of up to 1 month, the depletion of functional connections in DMN (MPFC) in the studied groups is clearly visualized on Figure 2.
|
2nd Subgroup |
Control Group |
||
|
structures of the brain |
T value |
structures of the brain |
T value |
|
Medial frontal cortex |
9.19 |
Medial frontal cortex |
10.12 |
|
Precuneus |
8.48* |
Precuneus |
3.81 |
|
Left frontal pole |
7.52 |
Left frontal pole |
7.24 |
|
– |
– |
Right frontal pole |
8.55 |
|
– |
– |
Left nucleus accumbens |
3.45 |
|
– |
– |
Right orbitofrontal cortex |
3.81 |
|
– |
– |
Left orbitofrontal cortex |
4.06 |
|
– |
– |
Left paracingulate gyrus |
8.37 |
|
– |
– |
Right paracingulate gyrus |
8.09 |
Note: T value – communication intensity level; * – p<0,05
Table 1: Functional connections of the medial prefrontal cortex with other structures of the brain.
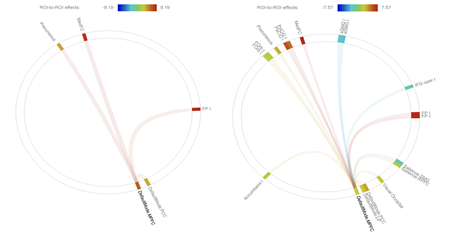
Figure 2: A connectome representing functional connections in the DMN (MPFC). Left - remission of up to 1 month; Right - control group.
This fact should be correlated with the possible restoration of a normal functional connection with longer periods of remission in narcotic drug addicts. Figure 3 shows the spatial mapping of the functional DMN (MPFC) connectome in 3D format in patients in the state of early remission (a) and in normal state (b).
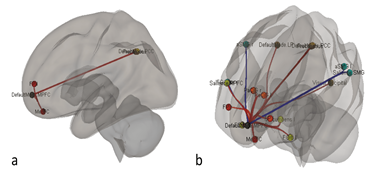
Figure 3: 3D visualisation of functional connections of DMN (MPFC) in patients in the state of early remission (a) and in normal state (b).
For clarity, Figures 4a and 4b shows a general view of the network of DMN (MPFC, LP, PCC) of the brain of patients in a state of intoxication and in normal condition.
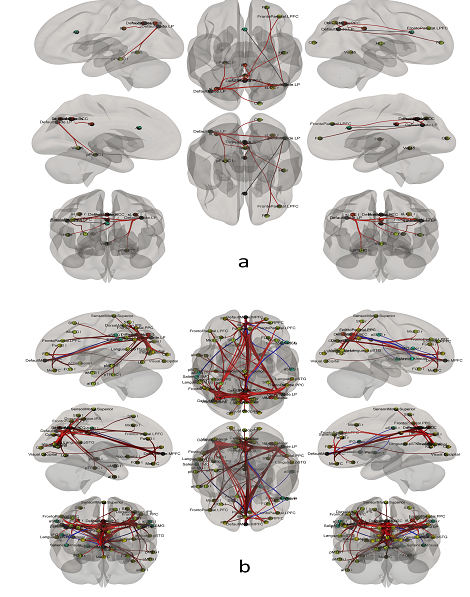
Figure 4: 3D visualisation of functional connections of DMN in patients who are in a condition of intoxication (a) and in normal state (b).
Interesting are the results of the evaluation of the interrelationship between the structures of the cerebral cortex responsible for the system of "control of behavior" and decision-making (orbitofrontal cortex, prefrontal cortex) with subcortical structures responsible for emotions in the limbic system. It is shown that in patients with early remission weakened functional connections between cortical structures and the left contiguous nucleus, almond-shaped body from both sides were registered. In patients in a state of intoxication, functional connections between the orbitofrontal cortex and other subcortical structures were not reliably detected. In patients who are in a state of remission compared to the control group, the "left orbitofrontal cortex - left putamen" connection increased significantly (p <0.05) (Table 2).
|
2nd Subgroup |
Control Group |
||
|
Structures of the brain |
T value |
Structures of the brain |
T value |
|
Left orbitofrontal cortex – left putamen |
6.68* |
Left orbitofrontal cortex – left putamen |
2.65 |
|
– |
– |
Left orbitofrontal cortex – left amygdala |
5.82 |
|
– |
– |
Left orbitofrontal cortex – right amygdala |
6.37 |
|
– |
– |
Right orbitofrontal cortex – left amygdala |
5.16 |
|
– |
– |
Right orbitofrontal cortex – right amygdala |
4.83 |
Note: * – p<0,05
Table 2: Functional connections of orbitofrontal cortex with subcortical structures.
The data obtained can be interpreted from the position that the putamen is responsible for motor behavior, reinforcement of emotional memory, and plays a role in the perception of contempt and disgust, which is especially important in personal attitudes when abandoning narcotic drugs in the early stages. This fact should be correlated with activation of the putamen according to the fMRI data with the exercise of the stress test. It has been established that the functional connectivity of the subcortical structures in patients who are in intoxication and in a state of remission has been found to differ from the cortex by changing functional connections in individual subcortical structures (Table 3). Data are given for each group compared with the norm (p <0.05). It was revealed, that with increasing intensity of functional connections between individual structures of the brain, the neural network does not increase the amount of connections (Figure 5).
|
1st Subgroup |
2nd Subgroup |
||
|
Structures of the brain |
T value |
Structures of the brain |
T value |
|
left putamen – right putamen |
26.79↑ |
left putamen – right putamen |
8.20↓ |
|
left putamen – left thalamus |
8.20 |
left putamen – left orbitofrontal cortex |
6.68↑ |
|
left putamen – left globus pallidus |
7.67↓ |
left putamen – occipitalis pole |
6.59↑ |
|
left thalamus – right thalamus |
14.72↓ |
right putamen – left thalamus |
7.87↑ |
|
Left amygdala – right amygdala |
9.49↑ |
right thalamus – left thalamus |
15.88↓ |
|
right amygdala – right hippocampus |
10.69↑ |
- |
- |
Note: ↑ - an increase in the intensity of communication in comparison with the norm; ↓ – decrease in the intensity of communication in comparison with the norm, (p<0,05).
Table 3: Functional connections of subcortical structures.
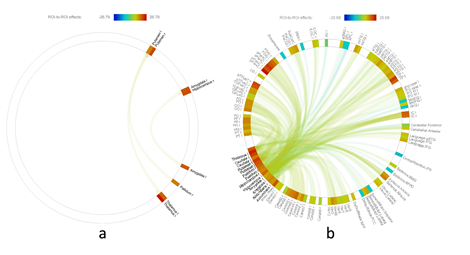
Figure 5: Functional connectomes of patients who are in a condition of intoxication (a) and in normal state (b).
The fact that the anterior cingulate cortex is involved in the performance of cognitive functions, such as reward expectancy, decision making, impulsiveness and emotions control, is confirmed, and the function of the posterior cingulate cortex is in the control of emotional memory. Table 4 presents data on the evaluation of functional connectivity of the anterior and posterior cingulate cortex with other surrounding structures.
|
1st Subgroup |
2nd Subgroup |
||
|
Structures of the brain |
T value |
Structures of the brain |
T value |
|
Left paracingulate gyrus |
21.97↑ |
Left paracingulate gyrus |
9.35↓ |
|
Right paracingulate gyrus |
8.49↓ |
- |
- |
|
Precuneus |
8.65↑ |
- |
- |
|
Left frontal pole |
6.47↑ |
- |
- |
Note: ↑ - an increase in the intensity of communication in comparison with the norm, (p<0,05); ↓ – decrease in the intensity of communication in comparison with the norm, (p<0,05).
Table 4: Functional connections of the anterior and posterior cingulate cortex.
5. Conclusion
In all patients suffering from opioid addiction, "oppression" of functional connections is noted in comparison with the normals. These changes are noted both in the default mode network, and in the cortical and subcortical structures, what indicates a violation of control functions, making the right decision, thinking, cognitive and emotional components in narcotic drug addicts. Functional MRI results/data allow revealing a direct relationship between the terms of remission and clusters of activations, the functional connectivity of neural networks, which indicates functional restoration of the brain structures after the cessation of narcotic drugs consumption. Functional connectivity, in the coming years, can become an important biomarker for the diagnosis of addictive pathology and other psychiatric disorders.
Today there are no objective neuroimaging criteria for addictive disorders. The use of fMRI makes it possible to identify brain structures that are directly involved in opioid addiction, to determine connections between them and to create a map of neural networks of the "dependent" brain. The use of fMRI is of great importance in studying the mechanisms of pathogenesis, qualitative and effective diagnosis, and in the choice of tactics for the treatment of addictive disorders.
The obtained data on functional changes in brain structures in patients suffering from opioid addiction will help to clarify the pathogenetic mechanisms of this pathology, with the possibility of subsequent development of basic objective diagnostic criteria of the opioid dependence syndrome, excluding the subjectivity of a narcologist at the stage of drawing up an expert opinion.
Acknowledgment
Trufanov A, Chakchir O, Partsernyak A, Bystrova D. thanks for financial support the Skolkovo Foundation (grant agreement for Russian educational and scientific organisation no.7 dd. 19.12.2017) and Skolkovo Institute of Science and Technology (General agreement no. 3663-MRA dd. 25.12.2017).
Funding
This research was supported by the Skolkovo Foundation (grant agreement for Russian educational and scientific organisation no.7 dd. 19.12.2017) and Skolkovo Institute of Science and Technology (General agreement no. 3663-MRA dd. 25.12.2017).
Interest Statement
The authors declared that the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
References
- Walter H. Functional visualization in psychiatry and psychotherapy. H. Walter – ?.: Astrel, Poligraphizdat, (2010): 432.
- Purves D. Principles of Cognitive Neuroscience. Sunderland: Sinauer Associates 601(2013): 38-39.
- Zhang Y. Distinct resting-state brain activities in heroin-dependent individuals. Brain Res 1402 (2011): 46-53.
- Seliverstova ?. Reorganization of the default mode network in patients with Parkinson's disease: an analysis of individual components according to RS-fmri. Analysis of neurology 9 (2015): 4-9.
- Seliverstov YU. Resting state of functional magnetic resonance imaging: possibilities and future of the method. Analysis of neurology (2013): 15-19.
- Denier N. Abnormal functional integration of thalamic low frequency oscillation in the BOLD signal after acute heroin treatment. Hum Brain Mapp 36 (2015): 5287-5300.
- Brown L. Sensory and cognitive functions of the basal Ganglia. Curr Opinion Neurobiol 7 (1997): 157-163.
- Tekin S. Frontal-subcortical neuronal circuits and clinical neuropsychiatry 53 (2002): 647-654.
- Groenewegen HJ, Trimble M. The ventral striatum as an interface between the limbic and motor systems. CNS Spectr 12 (2007): 887-892.
- Groenewegen H. The basal ganglia and motor control. Neural Plast 10 (2003): 107-120.
- Elliott R. Executive functions their disorders. Br. Med. Bull 65 (2003): 49-59.
- McNab F. Prefrontal cortex and basal ganglia control access to working Memory. Nat. Neurosci 11 (2008): 103-107.
- Haber S. The cortico – basal ganglia integrative network. The role of the Thalamus / S. Haber, R. Calzavara. Brain Res. Bull 78 (2009): 69-74.
- Sadikot A. The primate centromedian–parafascicular complex anatomical organization with a note on neuromodulation. Brain Res. Bull 78 (2009): 122-130.
