Percutaneous Endoscopic Lumbar Discectomy Vs Open Lumbar Microdiscectomy: A Comparison of Patient-Reported Outcomes in a Retrospective Cohort Follow-Up Design during the First Years of Implementation of Endoscopic Lumbar Discectomy
Article Information
Rune Mygind Mieritz1, 4*, Baskaran Ketharanathan1, Thomas von Bonsdorff3, Søren Wacher Qvistgaard3, Mogens Bach Pedersen2, Hanne Dinesen2, Mette K Schulz1,3, Frantz R Poulsen1, 3
1Department of Neurosurgery, Odense University Hospital, Odense, Denmark
2Molholm Privat Hospital, Vejle, Denmark
3Department of Clinical Research and BRIDGE (Brain Research – Inter-Disciplinary Guided Excellence), University of Southern Denmark, Odense, Denmark
4Department of Neurosurgery, Aarhus University Hospital, Aarhus, Denmark
*Corresponding Author: Rune Mygind Mieritz, Department of Neurosurgery, Odense University Hospital, Odense, Denmark
Received: 29 March 2022; Accepted: 05 April 2022; Published: 21 April 2022
Citation:
Rune Mygind Mieritz, Baskaran Ketharanathan, Thomas von Bonsdorff, Søren Wacher Qvistgaard, Mogens Bach Pedersen, Hanne Dinesen, Mette K Schulz, Frantz R Poulsen. Percutaneous Endoscopic Lumbar Discectomy Vs Open Lumbar Microdiscectomy: A Comparison of Patient-Reported Outcomes in a Retrospective Cohort Follow-Up Design during the First Years of Implementation of Endoscopic Lumbar Discectomy. Journal of Spine Research and Surgery 4 (2022): 063-071.
Share at FacebookAbstract
Background: The purpose of this study was to compare the patient-reported outcome of two different surgical techniques for lumbar disc herniation disease—percutaneous endoscopic lumbar transforaminal discectomy (PELD) versus open lumbar microdiscectomy (OLM)—in the first years of implementation of PELD in a clinical setting.
Methods: Fifty-one patients were included and stratified according to surgical treatment. Patient records were reviewed, and the patient-reported outcomes were assessed using the Oswestry Disability Index (ODI) and the EQ-5D-3L.
Results: OLM and PELD both significantly improved patient-reported outcomes for the patients. The OLM group had a significant larger improvement in ODI-score (p = 0.019) and EQ-5D-3L sum score, p = 0.009 compared to the PELD group. The OLM group was also the only group showing statistical significant improvement of EQ VAS-score (p < 0.001).
Conclusion: The results of the current study favors the OLM procedure over PELD in the first years of implementation of PELD in a clinical setting. Other studies list the advantages of PELD as minimal invasiveness, shorter time of operation and time of in hospital admission. The narrow population, study limitations and retrospective study design should be taken into consideration when interpreting these results, and hence randomized controlled trials are needed.
Keywords
Lumbar Disc Herniation, Microdis-cectomy, Endoscopic Lumbar Discectomy, Treatment Outcome, Surgery
Lumbar Disc Herniation articles; Microdis-cectomy articles; Endoscopic Lumbar Discectomy articles; Treatment Outcome articles; Surgery articles
Article Details
1. Introduction
Lumbar disc herniation (LDH) causing backpain with or without disabling radiculopathy is common. Although most patients can be treated conservatively, a growing proportion of patients undergo surgical treatment [1]. Open lumbar microdiscectomy (OLM) is the most common surgical discectomy technique and is considered by many to be the gold standard. A variety of minimally invasive discectomy techniques are emerging, including micro endoscopic discectomy, chemonucleolysis, laser discectomy, and percutaneous endoscopic lumbar discectomy (PELD) [2, 3]. A recent meta-analysis by Ruan et al. comparing PELD and OLM for lumbar disc herniation indicated similar effects of the two surgical approaches in terms of functional outcomes, complication rates, and reoper-ation rates. Some advantages of PELD over OLM have been suggested, i.e. less traumatic surgery with shorter operation time and hospital stay, lower infection rate, and less challenging surgery in obese patients [4]. One concern regarding PELD, however, is the initial learning curve and thus the challenges of imple-menting it in a clinical setting [5].
At Mølholm Hospital in Denmark, OLM has been used in the routine treatment of disc herniation for decades, and was introduced PELD in 2013. The current study was designed to investigate and compare the clinical outcome of 51 patients who underwent either PELD or OLM for a lumbar herniated disc during the first years of implementing PELD in a clinical setting. We used a retrospective, matched cohort follow-up design with pre- and postoperative data obtained through validated health status questionnaires completed by patients with lower back pain.
2. Methods
2.1 Population
The study was approved by the Danish Health and Medicines Authority and the Danish Data Protection Agency. Inclusion criteria were patients undergoing surgery for lumbar disc herniation at Mølholm Private Hospital, Vejle, Danmark between May 2013 and October 2015 who:
- had low back pain (LBP) and persisting and dominating radiculopathy corresponding clinically with disc herniation at the level of the disc on MRI and considered accessible by both PELD and OLM by the surgeon.
- had not responded to conservative treatment (mainly systematic back exercises over a period of 2-3 months).
- underwent single-level OLD or PELD (L3/4, L4/5, or L5/S1).
- had completed health status questionnaires prior to the surgical procedure.
Patients were excluded if they had had prior lumbar surgery at the same spinal level or both PELD and OLM surgery at the same spinal level, or if they were aged <18 or >80 years. The same neurosurgeon, who had over 30 years of experience with OLM and less than 1 year with PELD, operated on all patients. From May 2013 to October 2015, 78 patients underwent PELD (ICD-10 code KABC07) and 196 patients underwent OLM (ICD-10 code KABC16) at Mølholm Private Hospital, Vejle, Denmark.
2.1.1 PELD patients: All included PELD patients had actively consented to have PELD surgery after a discussion with the surgeon about its advantages and disadvantages. Arguments for PELD were less muscular damage and faster return to normal daily activity and work. An argument against PELD was the higher frequency of recurrent disc herniation. The distribution of spinal levels within the PELD group was: 2 patients with L2/3, 12 patients with L3/4, 51 patients with L4/5, and 13 patients with L5/S1 (total n=78). Of these, 55 patients were excluded from analysis: 17 due to missing preoperative data, five because their procedure was performed by a different surgeon, two because they were operated at spinal level L2/L3, 10 due to double surgery and 21 due to missing postoperative data (despite a reminder letter being sent out). This resulted in a total number of 23 patients included in the PELD group.
2.1.2 OLM patients: To match the number of patients in the PELD group, patients meeting the inclusion criteria were categorized by operated spinal level and thereafter randomly selected from a list to match the PELD patients per spinal level. To reduce selection bias, the groups were initially not matched by any other parameter. Of the 196 patients in the OLM group, 45 were randomly selected from the list. Of these 19 patients met the inclusion criteria with complete pre- and post-operative data. Five were excluded due to secondary surgery/reoperation. Twenty-one had missing post- operative data, why questionnaires (see below) were mailed. Of these, nine completed questionnaires returned. A total number of 28 patients were included in OLM matching PELD in numbers and spinal levels.
2.1.3 Surgical procedures:
2.1.3.1 OLM: Under general anaesthesia, patients were placed in a prone position. Lateral x-ray was used to verify the affected spinal level. An approximately 4-5 cm midline incision was followed by standard partial hemilaminectomy, flavectomy, and removal of herniated disc material under microscope. No attempt was made to extensively empty the disc space.
2.1.3.2 PELD: Under general anaesthesia, patients were placed in a prone position. The skin entry point and puncture was approximately 10-15 cm from the midline. Biplanar x-ray was used to verify the affected spinal level and for guidance to the target. An endoscope was inserted using a transforaminal approach. The herniated disc was removed from the centre to the posterolateral area, including removal of sequestrated disc fragments.
2.2 Data collection
Pre- and postoperative clinical questionnaires were obtained from the National Back Surgery Database (DaneSpine). To obtain postoperative data from patients with incomplete data in the DaneSpine registry, a notifying letter and health status quest-ionnaires (identical to those that were completed preoperatively) were mailed to patients together with a prepaid return envelope. Patient reported outcomes were evaluated using the EQ-5D-3L that has two elements: i) a descriptive system of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) each with three levels: no problems, some problems or extreme problems, and ii) a 0-100 visual analogue scale (EQ VAS) for self-reported health status [6]. The Oswestry Disability Index (ODI), with a score range of 0-50, was used to assess disability with back pain in regards to the World Health Organization’s widely accepted definition of disability [7]. Post-op questionnaires was completed at home, approx. 1 year after surgery (Table 1).
Background information on age, gender, operated level, operative technique, and duration of surgery was obtained from medical journals. A trained nurse contacted patients within 1 week and again 6 weeks after their procedure for a standardized telephone interview on postoperative personal complaints. These subjective complaints were treated as a binary variable: complaint vs. no complaint (Table 1).
2.3 Statistical analysis
Data were analyzed using STATA/IC v.14.1 software. Two-sample T-tests, Mann-Whitney/Wilcoxon sum rank tests were used for analysis of differences in continuous variables and Pearson’s chi2 tests were used to compare categorical variables (Tables 1 and 2). P-values lower than 0.05 were considered statistically significant.
3. Results
3.1 Population
A total of 51 patients (23 PELD and 28 OLM) were included in the study. The cohort included 17 women and 34 men with a mean age of 52 years (range 31 to 70 years) and a mean follow-up of 13 months (Table 1). Group matching was assessed regarding gender and age and was found comparable between the PELD and OLM groups (Table 1). Multivariate analysis showed no statistical significant difference between the PELD and OLM groups regarding gender ratio (male : female, 15 : 8 in PELD and 19 : 9 in OLM, p = 0.84), mean age at the time of operation (52.34 ± 1.7 years in PELD and 52.71 ± 1.33 years in OLM, p = 0.98), mean follow-up (11.78 ± 1.22 months in PELD and 15.11 ± 1.03 months in OLM, p = 0.086), and mean operating time (39.69 ± 2.24 minutes in PELD and 46.25 ± 3.43 minutes in OLM, p = 0.067).
3.2 Patient reported outcomes
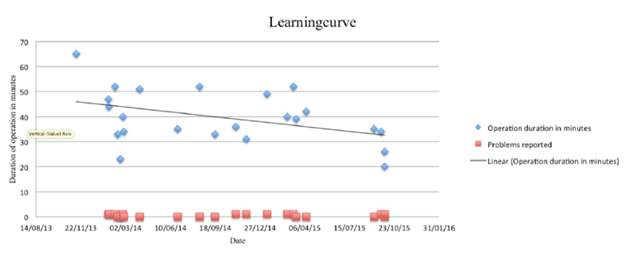
PELD had a mean ODI-score before operation of 20.17 ± 2.15 which improved to 10.48 ± 1.4 after operation (p < 0.001). PELD improved in EQ-VAS 6.5 ± 5.8 in absolute values. There was no significant change in EQ VAS scores when comparing pre- to postoperative (p = 0.15). The EQ-5D-3L sum score improved overall from 8.91 ± 0.36 to 7.7 ± 0.34 (p = 0.059) (Table 2). OLM had a mean ODI-score before operation of 24.79 ± 1.72 and 8.36 ± 1.63 after operation (p < 0.001). The mean EQ-VAS score improved from pre- to postoperative (53.32 ± 4.95 to 74.71 ± 4.59, p < 0.001). The EQ-5D-3L sum score improved overall from 9.21 ± 0.26 to 6.68 ± 0.32 (p < 0.001). The mean change difference in ODI-score pre- to postoperative was −9.7 ± 2.41 in PELD, −16.43 ± 2.09 in OLM and EQ-VAS 6.48 ± 5.76 in PELD, 21.39 ± 5.72 in OLM. When comparing the mean change difference in PELD and OLM, OLM had a significantly greater decrease, and thereby improvement, in ODI-score (p = 0.0195) and EQ-VAS (P = 0.037). Comparing EQ-5D-3L in PELD and OLM change differences, OLM had a statistically significant larger improvement in EQ-5D-3L sum score (p = 0.009). Stratification of EQ-5D-3L in each of its five dimensions, showed statistical significant intergroup difference for one dimension only: self-care (p = 0.007). There was no significant difference in the proportion of subjective postoperative complaints (some degree of persisting back and/or leg pain/altered sensibility) between PELD (48 %) and OLM (57 %; p = 0.507, Table 1). The reoperation rate for PELD patients was 12.8%, and all reoperations were performed by OLM surgery. The reoperation rate in OLM group was 7.1%. No serious complications such as nerve root injury or infection were observed in either PELD or OLM patients. Despite the small PELD cohort, a reduction in duration of mean surgical procedure was observed over time (Figure 1) from year 1 to year 2 (p = 0.309). Furthermore, the accumulation of patient complaints, year 1 vs. year 2, showed no significant change over time (p = 0.146).
|
Group |
PELD |
OLM |
p-value |
|
Males |
15 |
19 |
|
|
Females |
8 |
9 |
0.842 |
|
Age |
52.34 ± 1.70 |
52.71±1.33 |
0.977 |
|
Time to follow-up, months |
11.78 ± 1.21 |
15.11±1.03 |
0.086 |
|
Operation duration, minutes |
39.69 ± 2.24 |
||
|
Spine level |
|||
|
L3/L4 |
3 |
6 |
|
|
L4/L5 |
18 |
18 |
0.552 |
|
L5/S1 |
2 |
4 |
|
|
Previous operation |
3 |
15 |
0.003* |
|
Personal complaints |
11 |
16 |
0.507 |
PELD: Percutaneous Endoscopic Lumbar Transforminal Discectomy; OLM: Open Lumbar Microdiscectomy; Mean±Standard Error of Mean. *p-value<0,05 is considered significant
Table 1: Demography of patient population.
|
PELD |
OLM |
PELD vs OLM |
|||||
|
Group |
pre |
post |
change |
pre |
post |
change |
p-value |
|
ODI |
20.2 |
10.5 |
-9.7 ± 2.41* |
24.8 |
8.4 |
-16.43 ± 2.09* |
0.019* |
|
EQ-5D-3L |
|||||||
|
EQ -Mobility |
1.8 |
1.5 |
-0.3 ± 0.16 |
1.9 |
1.3 |
-0.57 ± 0.12 |
0.201 |
|
EQ - Self-care |
1.2 |
1.3 |
0.13 ± 0.13 |
1.4 |
1.1 |
-0.36 ± 0.09 |
0.007* |
|
EQ - Usual activities |
2.3 |
1.8 |
-0.82 ± 0.15 |
2.3 |
1.5 |
-0.52 ± 0.17 |
0.305 |
|
EQ - Pain/discomfort |
2.4 |
1.9 |
-0.48 ± 0.17 |
2.5 |
1.8 |
-0.71 ± 0.12 |
0.33 |
|
EQ - Anxiety/depression |
1.3 |
1.2 |
-0.09 ± 0.11 |
1.1 |
1.1 |
-0.36 ± 0.08 |
0.757 |
|
EQ-5D-3L sum score |
8.9 |
7.7 |
-1.26 ± 0,47 |
9.2 |
6.7 |
-2.5 ± 0.31* |
0.009 |
|
EQ-VAS |
62.6 |
69 |
6.48 ± 5.76 |
53.3 |
74.4 |
21.39 ± 5.72* |
0.037* |
PELD, Percutaneous Endoscopic Lumbar Transforaminal Discectomy; OLM, Open Lumbar Microdiscectomy; EQ-5D-3L: EuroQol 5 Dimenssion 3 level questionnaire, EQ VAS; EuroQol visual analog scale, ODI: Oswestry disability index. Mean±Standard Error of Mean. *p-value<0,05.
Table 2: Patient reported outcomes.
4. Discussion
In the present study, both PELD and OLM resulted in significantly improved scores of patient reported outcomes, although the overall greatest improvement in ranking scores of patient reported outcomes was found in the OLM group during the first years of imple-mentation of PELD. The literature on patient reported or clinical outcome after PELD is limited. Some studies suggest advantages of PELD over OLM with regards to parameters such as duration of operation, time of admission, and its minimal invasiveness [3, 8-10]. In the present study, the mean surgical time was shorter in the PELD group although not significantly (Table 1). Some studies describe significantly better outcome for PELD patients of ODI or VAS compared to OLM [8, 9] while others do not [5]. A resent meta-analysis indicates similar results [4]. None of the included PELD patients underwent re-operation with PELD surgery. However, evaluating the excluded patients from the PELD group, ten patients underwent initial PELD surgery and secondary surgery with OLM technique (dual surgery). The reoperation rate in the OLM group was 7.1%,which was consistent with the clinic’s general OLM reoperation rate. When assessing the journals from these patients, we found the reason for repeated surgery was unacceptable clinical outcome.
Reoperation rates reported in the literature vary. The meta-analysis from Ruan et al reported 7.92% after PELD and 5.94% after OLM4. These authors suggested that PELD surgery may be preferred for reoperation as it avoids cutting through scar tissue and further damage to the paraspinal muscles. In this study, OLM re-operation technique was chosen partly due to the location of the herniated disc (ie. Herniated disc not at the level of the disc or anatomical compromised at L5/S1 level due to iliac crest) and because of the surgeons’ extensive experience with OLM surgery. Since PELD is a fairly new technique, it is also possible that PELD patients experiencing pain recurrence and an unsatisfactory result after the first surgery were re-operated with a lower threshold than was the case for OLM patients. This possible lower threshold could have contributed to a skewed rate of incidence regarding re-operation, and hence be a potential confounder. Wang et al. found a significant difference favoring outcomes by an experienced PELD surgeon in VAS, duration of operation and admission, by comparing with a less experienced one. Furthermore, a reduction in the incidence of patient complaints was seen from the first 40 patients to the next 40 patients [11]. In the present study, a learning curve was also demonstrated, i.e. reduction in PELD surgical procedure time (Figure 1). This, however, was not reflected in patient outcome.
A recent study by Son et al. assessing the learning curve for PELD surgery concluded that incomplete decompression and exiting nerve root complications were higher in the novice stage [5], and may be an explanation for the clinical results in the current study. The results of the present study might reflect the experience level of the surgeon more that the techniques itself i.e the patient reported outcomes may change to be in favor for PELD as the experience level increases.
4.1 Limitations
One limitation of the study is the retrospective study design and small cohort population. Furthermore all included PELD patients had actively consented to have PELD surgery after a discussion with the surgeon. This inclusion method leaves a skewed cohort population comparing groups, since OLM would otherwise be the standard procedure. The selection of candidates could be biased by patients who have declined PELD surgery. Few studies have investigated which patients are best suited for PELD surgery. A cut-off age of 57 years or younger [12] has been suggested, whereas others have suggested that PELD surgery is most suitable for adolescents [13]. The patients in this article had a mean age of 52.3 years (PELD) and 52.7 years (OLM) (Table 1).
5. Conclusion
PELD and OLM both improved patient reported outcomes, although OLM showed greater improvement in the first years of implementation PELD in a clinical setting. A limitation of the study retrospective study design and small cohort population. Both should be taken into consideration when interpreting the results, and in order to better investigate surgical benefits and outcomes of the two techniques, randomized controlled trials are needed.
Acknowledgement
Editing of a previous version of the manuscript by Claire Gudex from the University of Southern Denmark is greatly appreciated.
References
- Grotle M, Solberg T, Storheim K, et al. Public and private health service in Norway: a comparison of patient characteristics and surgery criteria for patients with nerve root affections due to discus herniation. Eur Spine J 23 (2014): 1984-1991.
- Gibson JNA, Waddell G. Surgical inter-ventions for lumbar disc prolapse. Cochrane Database Syst Rev (2007): CD001350.
- Rasouli MR, Rahimi-Movaghar V, Shok-raneh F, et al. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochra-ne Database Syst Rev (2014): CD010328.
- Ruan W, Feng F, Liu Z, et al. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: A meta-analysis. Int J Surg 31 (2016): 86-92.
- Son S, Ahn Y, Lee SG, et al. Learning curve of percutaneous endoscopic transforaminal lumbar discectomy by a single surgeon. Medicine (Baltimore) 100 (2021): e24346.
- Soer R, Reneman MF, Speijer BLGN, et al. Clinimetric properties of the EuroQol-5D in patients with chronic low back pain. Spine J 12 (2012): 1035-1039.
- Lauridsen HH, Hartvigsen J, Manniche C, et al. Danish version of the Oswestry Disability Index for patients with low back pain. Part 1: Cross-cultural adaptation, reliability and validity in two different populations. Eur Spine J 15 (2006): 1705-1716.
- Lee DY, Shim CS, Ahn Y, et al. Comparison of Percutaneous Endoscopic Lumbar Discec-tomy and Open Lumbar Microdiscectomy for Recurrent Disc Herniation. J Korean Neurosurg Soc 46 (2009): 515-521.
- Jang J-S, An S-H, Lee S-H. Transforaminal percutaneous endoscopic discectomy in the treatment of foraminal and extraforaminal lumbar disc herniations. J Spinal Disord Tech19 (2006): 338-343.
- Lee S-H, Chung S-E, Ahn Y, et al. Comparative radiologic evaluation of percu-taneous endoscopic lumbar discectomy and open microdiscectomy: a matched cohort analysis. Mt Sinai J Med 73 (2006): 795-801.
- Wang H, Huang B, Li C, et al. Learning curve for percutaneous endoscopic lumbar discec-tomy depending on the surgeon’s training level of minimally invasive spine surgery. Clin Neurol Neurosurg 115 (2013): 1987-1991.
- Kim CH, Chung CK, Choi Y, et al. The Selection of Open or Percutaneous Endo-scopic Lumbar Discectomy According to an Age Cut-off Point: Nationwide Cohort Study. Spine (Phila Pa 1976) 40 (2015): E1063-E1070.
- Lee DY, Ahn Y, Lee S-H. Percutaneous endoscopic lumbar discectomy for adolescent lumbar disc herniation: surgical outcomes in 46 consecutive patients. Mt Sinai J Med 73 (2006): 864-870.