Outcome of Closed Reamed Interlocking Nailing in Closed Diaphyseal Femoral Fracture in Adult
Article Information
Sharif Hossain1*, Mahbuba Sultana2, Molla Muhammad Abdullah Al Mamun3, Minhaz Uddin4, Khaled Mahmud5
1D-Ortho, MS-Ortho, Registrar (Orthopaedics), Shaheed Tajuddin Ahmad Medical College hospital, Gazipur, Bangladesh
2MBBS, M-phil, Assistant Professor (Microbiology), Shaheed Tajuddin Ahmad Medical College, Gazipur, Bangladesh
3Assistant Professor (Orthopaedics), Shaheed Tajuddin Ahmad Medical College Hospital, Gazipur, Bangladesh
4MS-Ortho, Assistant Registrar (Orthopaedics), Dhaka Medical College Hospital, Bangladesh
5FCPS (Ortho), Junior Consultant, UHC, Pakundia, Kishoregonj, Bangladesh
*Corresponding Author: Md. Sharif Hossain, D-Ortho, MS-Ortho, Registrar (Orthopaedics), Shaheed Tajuddin Ahmad Medical College hospital, Gazipur, Bangladesh.
Received: 08 September 2023; Accepted: 19 September 2023; Published: 29 September 2023
Citation:
Sharif Hossain, Mahbuba Sultana, Molla Muhammad Abdullah Al Mamun, Minhaz Uddin, Khaled Mahmud. Outcome of Closed Reamed Interlocking Nailing in Closed Diaphyseal Femoral Fracture in Adult. Journal of Orthopedics and Sports Medicine. 5 (2023): 381-387.
Share at FacebookAbstract
Background: Diaphyseal femur fracture most commonly occurs due to high-velocity trauma. There are various treatment modalities for diaphyseal femur fracture in adults: traction, brace, platting, intramedullary nail, external fixator, and intramedullary interlocking nail.
Aim: To evaluate the functional outcome of treatment of diaphyseal fracture of the femur by closed-reamed interlocking intramedullary nail.
Methods: This Quasi-experimental study was conducted in the Dhaka Medical College Hospital, Dhaka, to analyze the clinical and radiological outcome of Closed Interlocking Intramedullary Nailing in Diaphyseal Fractures of the Femur. For this purpose, among admitted patients, a total of 38 patients were selected who fulfilled the inclusion and exclusion criteria. All relevant data of the patient was recorded according to the questionnaire. The SPSS computer software program, version 22.0, analyzed data. The level of significance was set at 0.05 (P < 0.05).
Result: Among 38 patients, the mean age was 32.84 ± 13.94 years (age range 18-60 years); the majority of the patients, 10(26.3%), were in the second decade as well as 10(26.3%) in the third decade and 8(21.1%) in the fourth decade. Male: Female ratio 2.8:1. Road traffic accidents in 30(78.9%) patients were observed to be the main cause in this series, followed by fall from height in 6(15.8%) cases. In this study, transverse fractures were 24 (63.1%), spiral fractures were 8(21.1%), and oblique were 6(15.8%) cases. Majority patients 30(78.9%) had full range of knee flexion (>120 degree), 6(15.8%) patients had <90 degree and 2(5.3%) patients 110 degree of knee flexion. Only 2(5.3%) patients had a 1cm limb length discrepancy, and 4(10.5%) patients had 5 degrees of malalignment. The mean hospital stay was 11.7 ± 2.3 days (8-15 days). The union rate was found in 94.7% of cases. The mean union time was 14.3±4.1 weeks. The mean operative time was 101.6±23.6 minutes. Functional outcome was assessed based on the Friedman and Wyman scoring system. Good results were obtained in 32 cases (84.2%), fair results in 6 cases (15.8%), and no poor outcome was found.
Conclusion: Closed Intramedullary interlocking nailing is an effective treatment method for diaphyseal fractures of the femur because of stable fixation, higher rate of union, lower rate of complications like infection or non-union, and allows early weight-bearing return to activities.
Keywords
Closed reamed; Interlocking nailing; Closed diaphyseal; Femoral fracture
Orthopaedics articles Orthopaedics Research articles Orthopaedics review articles Orthopaedics PubMed articles Orthopaedics PubMed Central articles Orthopaedics 2023 articles Orthopaedics 2024 articles Orthopaedics Scopus articles Orthopaedics impact factor journals Orthopaedics Scopus journals Orthopaedics PubMed journals Orthopaedics medical journals Orthopaedics free journals Orthopaedics best journals Orthopaedics top journals Orthopaedics free medical journals Orthopaedics famous journals Orthopaedics Google Scholar indexed journals Fractures articles Fractures Research articles Fractures review articles Fractures PubMed articles Fractures PubMed Central articles Fractures 2023 articles Fractures 2024 articles Fractures Scopus articles Fractures impact factor journals Fractures Scopus journals Fractures PubMed journals Fractures medical journals Fractures free journals Fractures best journals Fractures top journals Fractures free medical journals Fractures famous journals Fractures Google Scholar indexed journals Femur articles Femur Research articles Femur review articles Femur PubMed articles Femur PubMed Central articles Femur 2023 articles Femur 2024 articles Femur Scopus articles Femur impact factor journals Femur Scopus journals Femur PubMed journals Femur medical journals Femur free journals Femur best journals Femur top journals Femur free medical journals Femur famous journals Femur Google Scholar indexed journals Extremity injuries articles Extremity injuries Research articles Extremity injuries review articles Extremity injuries PubMed articles Extremity injuries PubMed Central articles Extremity injuries 2023 articles Extremity injuries 2024 articles Extremity injuries Scopus articles Extremity injuries impact factor journals Extremity injuries Scopus journals Extremity injuries PubMed journals Extremity injuries medical journals Extremity injuries free journals Extremity injuries best journals Extremity injuries top journals Extremity injuries free medical journals Extremity injuries famous journals Extremity injuries Google Scholar indexed journals Femoral shaft fractures articles Femoral shaft fractures Research articles Femoral shaft fractures review articles Femoral shaft fractures PubMed articles Femoral shaft fractures PubMed Central articles Femoral shaft fractures 2023 articles Femoral shaft fractures 2024 articles Femoral shaft fractures Scopus articles Femoral shaft fractures impact factor journals Femoral shaft fractures Scopus journals Femoral shaft fractures PubMed journals Femoral shaft fractures medical journals Femoral shaft fractures free journals Femoral shaft fractures best journals Femoral shaft fractures top journals Femoral shaft fractures free medical journals Femoral shaft fractures famous journals Femoral shaft fractures Google Scholar indexed journals Gunshot injuries articles Gunshot injuries Research articles Gunshot injuries review articles Gunshot injuries PubMed articles Gunshot injuries PubMed Central articles Gunshot injuries 2023 articles Gunshot injuries 2024 articles Gunshot injuries Scopus articles Gunshot injuries impact factor journals Gunshot injuries Scopus journals Gunshot injuries PubMed journals Gunshot injuries medical journals Gunshot injuries free journals Gunshot injuries best journals Gunshot injuries top journals Gunshot injuries free medical journals Gunshot injuries famous journals Gunshot injuries Google Scholar indexed journals Adult Respiratory Distress Syndrome articles Adult Respiratory Distress Syndrome Research articles Adult Respiratory Distress Syndrome review articles Adult Respiratory Distress Syndrome PubMed articles Adult Respiratory Distress Syndrome PubMed Central articles Adult Respiratory Distress Syndrome 2023 articles Adult Respiratory Distress Syndrome 2024 articles Adult Respiratory Distress Syndrome Scopus articles Adult Respiratory Distress Syndrome impact factor journals Adult Respiratory Distress Syndrome Scopus journals Adult Respiratory Distress Syndrome PubMed journals Adult Respiratory Distress Syndrome medical journals Adult Respiratory Distress Syndrome free journals Adult Respiratory Distress Syndrome best journals Adult Respiratory Distress Syndrome top journals Adult Respiratory Distress Syndrome free medical journals Adult Respiratory Distress Syndrome famous journals Adult Respiratory Distress Syndrome Google Scholar indexed journals Fracture malalignment articles Fracture malalignment Research articles Fracture malalignment review articles Fracture malalignment PubMed articles Fracture malalignment PubMed Central articles Fracture malalignment 2023 articles Fracture malalignment 2024 articles Fracture malalignment Scopus articles Fracture malalignment impact factor journals Fracture malalignment Scopus journals Fracture malalignment PubMed journals Fracture malalignment medical journals Fracture malalignment free journals Fracture malalignment best journals Fracture malalignment top journals Fracture malalignment free medical journals Fracture malalignment famous journals Fracture malalignment Google Scholar indexed journals Post-traumatic arthritis articles Post-traumatic arthritis Research articles Post-traumatic arthritis review articles Post-traumatic arthritis PubMed articles Post-traumatic arthritis PubMed Central articles Post-traumatic arthritis 2023 articles Post-traumatic arthritis 2024 articles Post-traumatic arthritis Scopus articles Post-traumatic arthritis impact factor journals Post-traumatic arthritis Scopus journals Post-traumatic arthritis PubMed journals Post-traumatic arthritis medical journals Post-traumatic arthritis free journals Post-traumatic arthritis best journals Post-traumatic arthritis top journals Post-traumatic arthritis free medical journals Post-traumatic arthritis famous journals Post-traumatic arthritis Google Scholar indexed journals Cloverleaf nail articles Cloverleaf nail Research articles Cloverleaf nail review articles Cloverleaf nail PubMed articles Cloverleaf nail PubMed Central articles Cloverleaf nail 2023 articles Cloverleaf nail 2024 articles Cloverleaf nail Scopus articles Cloverleaf nail impact factor journals Cloverleaf nail Scopus journals Cloverleaf nail PubMed journals Cloverleaf nail medical journals Cloverleaf nail free journals Cloverleaf nail best journals Cloverleaf nail top journals Cloverleaf nail free medical journals Cloverleaf nail famous journals Cloverleaf nail Google Scholar indexed journals Metaphyseal fractures articles Metaphyseal fractures Research articles Metaphyseal fractures review articles Metaphyseal fractures PubMed articles Metaphyseal fractures PubMed Central articles Metaphyseal fractures 2023 articles Metaphyseal fractures 2024 articles Metaphyseal fractures Scopus articles Metaphyseal fractures impact factor journals Metaphyseal fractures Scopus journals Metaphyseal fractures PubMed journals Metaphyseal fractures medical journals Metaphyseal fractures free journals Metaphyseal fractures best journals Metaphyseal fractures top journals Metaphyseal fractures free medical journals Metaphyseal fractures famous journals Metaphyseal fractures Google Scholar indexed journals Injured bone articles Injured bone Research articles Injured bone review articles Injured bone PubMed articles Injured bone PubMed Central articles Injured bone 2023 articles Injured bone 2024 articles Injured bone Scopus articles Injured bone impact factor journals Injured bone Scopus journals Injured bone PubMed journals Injured bone medical journals Injured bone free journals Injured bone best journals Injured bone top journals Injured bone free medical journals Injured bone famous journals Injured bone Google Scholar indexed journals Osteogenic articles Osteogenic Research articles Osteogenic review articles Osteogenic PubMed articles Osteogenic PubMed Central articles Osteogenic 2023 articles Osteogenic 2024 articles Osteogenic Scopus articles Osteogenic impact factor journals Osteogenic Scopus journals Osteogenic PubMed journals Osteogenic medical journals Osteogenic free journals Osteogenic best journals Osteogenic top journals Osteogenic free medical journals Osteogenic famous journals Osteogenic Google Scholar indexed journals Soft tissue articles Soft tissue Research articles Soft tissue review articles Soft tissue PubMed articles Soft tissue PubMed Central articles Soft tissue 2023 articles Soft tissue 2024 articles Soft tissue Scopus articles Soft tissue impact factor journals Soft tissue Scopus journals Soft tissue PubMed journals Soft tissue medical journals Soft tissue free journals Soft tissue best journals Soft tissue top journals Soft tissue free medical journals Soft tissue famous journals Soft tissue Google Scholar indexed journals Knee articles Knee Research articles Knee review articles Knee PubMed articles Knee PubMed Central articles Knee 2023 articles Knee 2024 articles Knee Scopus articles Knee impact factor journals Knee Scopus journals Knee PubMed journals Knee medical journals Knee free journals Knee best journals Knee top journals Knee free medical journals Knee famous journals Knee Google Scholar indexed journals
Article Details
1. Introduction
Fractures of the shaft of the femur are common. They are estimated to constitute 5-10% of all fractures. In most instances, they are produced by high-energy trauma and may be accompanied by multiple life-threatening injuries elsewhere in the body system [1]. Fractures of the femur shaft are a major cause of morbidity and mortality in patients with lower extremity injuries. Most fractures are sustained in young adults during high-velocity injuries [2,3]. Fractures due to severe trauma are preponderant in young patients and show a predilection for males [1]. As industrialization and urbanization are progressing year to year with rapid increase in traffic, the incidence of high-energy trauma is increasing at the same speed. Femoral shaft fractures result from high-energy trauma, commonly road traffic accidents, gunshot injuries, and falls from height [4]. Fractures of the femur shaft can be life-threatening due to an open wound, fat embolism, Adult Respiratory Distress Syndrome (ARDS), or resultant multiple organ failure [2]. Even with survival after initial trauma, disability usually results from femoral shortening, fracture malalignment, or prolonged extremity immobilization by traction or casting to maintain fracture length and alignment during the early phases of healing. Shortening and malalignment of the leg can lead to a limp and post-traumatic arthritis [2,3]. Fractures of the femoral shaft may be treated by traction alone, traction followed by a standard cast brace, external fixation, or open reduction and internal fixation. The options in internal fixation include intramedullary nailing and plate and screw fixation. The choice of treatment method in any particular case may be influenced by factors such as the type and location of the fracture, the degree of comminution, the age of the patient, and the patient's social and economic standing [1]. When Sir Gerhard Kuntscher described his cloverleaf nail, it revolutionized the treatment protocol [5]. He refurbished it by using locking screws to abut the nail, and then was born the concept of interlocking nailing [4]. Today, various types of interlocking nails are available in the market and are widely used in clinical practice for femoral diaphyseal fractures [6-8]. Over the years, intramedullary nailing has become the standard treatment of long-bone diaphyseal and selected metaphyseal fractures, providing sufficient stability with limited soft-tissue dissection. Furthermore, this technique preserves the muscle envelope around the fracture and, therefore, the extra-osseous blood supply to the bone. Consequently, revascularization of the injured bone is enhanced, and periosteal callus formation is promoted. Unlike screws and plates, intramedullary stabilization has the advantage of "load-sharing." It eliminates the need for additional support, i.e., casting. Early rehabilitation with muscle strengthening and joint range-of-motion exercises is possible, and if good bone contact is achieved, even early weight-bearing is allowed [9]. Several factors are responsible for the healing of fractures in static nailing. Due to close nailing, the undisturbed fracture hematoma helps form sufficient external callus. The muscle envelope of the thigh favors callus formation. The endosteal debris deposited at the fracture site due to reaming is internal bone grafts and increased osteogenic potentials. The proximal and distal interlocking bolts increase the rigidity of the nail bone construct [10]. The interlocking nail system combines the best of both, i.e., it offers axial and rotational stability in comminuted and unstable fractures and involves minimal interference with soft tissue around the bone, especially when introduced in a closed manner [11]. The effect on early outcomes of the various modalities of treatment can be measured concerning the functional status of the knee, total hospitalization time, bony union, and the presence or absence of complications [1]. Closed interlocked intramedullary (I.M.) nailing is the preferred treatment for most femoral shaft fractures in many centers. Locked nails provide rotational stability and maintain length in comminuted or segmental fractures. However, there are some drawbacks. Any malalignment present at the time of interlocking will persist. Misjudgment of length is common, and rotational malalignment may occur even in experienced hands [12]. Intramedullary interlocking nailing has now been regarded as the gold standard against which other methods are compared [4,5]. Here, we have attempted to evaluate the Outcome of Closed Interlocking Intramedullary Nailing in Diaphyseal Fractures of the Femur. The study aims to evaluate the functional outcome of treatment of diaphyseal fracture of femur by closed reamed interlocking intramedullary nail.
2. Methodology and Materials
This is a retrospective experimental study; 38 patients were enrolled and analyzed in this study. The study was conducted at the Department of Orthopedics and Traumatology, Dhaka Medical College Hospital, Dhaka, Bangladesh. The study duration was two years, from July 2017 to June 2019. The ethical approval was taken from the ethics committee of the Dhaka Medical College. All adult patients with clinical and radiological evidence of a closed femur shaft fracture were admitted to the hospital for operation and fulfilled the inclusion and exclusion criteria. Purposive sampling is according to the availability of the patients and strictly considers the inclusion and exclusion criteria. Data was collected with a pre-tested semi-structured questionnaire containing history, clinical examination, laboratory Investigations, pre-operative, post-operative follow up findings, and complications.
Inclusion criteria:
- Patient age was 18 to 65 years.
- Admitted in hospital within 24 hours of injury.
- Closed simple fracture (AO type 32A1, 32A2, 32A3).
Exclusion criteria:
- Open fracture
- Patient with associated fracture neck of femur.
- Female with pregnancy
- Patients age less than 18 years and more than 65 years
- Pathological Fracture
- Comminuted fracture
- Segmental fracture
- Patients who can’t communicate with the interviewer
- Patients who were not interested to participate
2.1 Operational definition
That portion of the bone lies between 5cm distal to the lesser trochanter and a point 8cm proximal to the adductor tubercle [1]. Reduction is achieved by indirect technique in fracture table and fracture fixed through locked intramedullary nail. The femoral Interlocking nail is an intramedullary load-sharing fixation device. C-Arm is a mobile medical imaging intensifier device based on X-ray technology and can be used flexibly in various operating rooms within a hospital. A c C-shaped arm connects the X-ray source and X-ray detector on either end.
Fracture union: Clinically- Painless full weight bearing without external support. Radiologically bridging the fracture site at three cortices in two views [13].
Delayed Union: Delayed union was considered when the radiographs failed to demonstrate progressive consolidation between 16-24 weeks after nailing [13].
Fracture nonunion: Defined as fragments that are still not united within 9 months or failed to show healing progression by consecutive 3 months after operation [14].
Consolidation: Clinically- The fracture site is not tender, no movement can be obtained, and attempted angulation is painless. Radiologically- The fracture line is obliterated, crossed by bone trabeculae with well-defined callus around it [15].
All patient was followed up at the end of a) the 2nd week, b) the 6th week, c) the 12th week, d) the 16th week, and e) the 24th week. Active flexion and extension of the knee and hip were encouraged as early as possible. The total active range of movement of the knee and hip was determined. Any complication was noted during follow-up, and appropriate measures were taken to control it. A radiograph was taken at each visit to follow up on the fracture healing, and fracture alignment was assessed during each visit and counseled the patient about the further job, the role of physiotherapy, psychological support, and rehabilitation. After selection and proper counseling, the study's objectives and procedure were explained in detail to the patients. They were encouraged to participate voluntarily and allowed to withdraw from the study even after participating whenever they felt. Their written consent was taken in a prescribed form. The researcher prepared a pre-tested semi-structured questionnaire containing history, clinical findings, and previous treatment patterns, and the guide verified it. The researcher himself collected data-history, clinical, and radiological examination diagnosed femoral shaft fracture. Treatment was given by CRIF by closed-reamed interlocking intramedullary nail under C-arm guidance. All data were recorded systematically in a preformed data collection form (questionnaire). Quantitative data were expressed as mean, standard deviation and qualitative data as frequency distribution and percentage. The analysis of different variables was done according to standard statistical analysis by using SPSS version 22.0. The significance level was set at 0.05 for all analyses, and p- value <0.05 was considered significant.
3. Result
A total of 38 patients were enrolled and analyzed in this study. Among the study population, the mean age was 32.84 ± 13.94 years, with maximum patients (52.6%) below 30 years followed by a 21.1% age range of 31-40 years. Minimum age of 18 and maximum 60 years (Table 1 and 2). Most of the patients were male (73.68%), and the rest 1026.32%) patients were female (Figure 1). Male: Female ratio 2.8:1. Table 3 shows the occupational distribution of the study population where the majority of the patients, 14 (36.84%) were business people, 10(26.32%) patients were day laborers, 8(21.05%) patients were homemaker and 6(15.79%) patients were service holder. According to Table 2, road traffic accident in 30(78.9%) patients was observed to be the main cause of fracture in our series, followed by fall from height 6(15.8%) cases. Most patients (63.2%) had right-sided injury and 36.8% had left-sided injury. In our study transverse fractures were 24(63.1%), spiral fractures were 8(21.1%) and oblique were 6(15.8%) cases. Most of the 22(57.9%) patients were operated on more than 7 days after admission, and 16(42.1%) patients were operated on 5-7 days of trauma (Table 3). Based on Table 4, most of the 30(78.9%) patients had full knee flexion (>120 degrees), 6 (15.8%) patients had < 90 degrees, and 2(5.3%) patients had 110 degrees of knee flexion. Only 2(5.3%) patients had a 1cm limb length discrepancy. The complication rate was only 10.6% of the total population, where only 2(10.6%) patients had 5° malalignment (Table 5 and 6). Out of 38 patients, none suffered from any superficial or deep infection within the study period. Several 24(63.2%) patients had a total hospital stay of more than 10 days, followed by 14(36.8%) patients had up to 10 days. Minimum hospital stays are 8 days, and the maximum is 15 days. The union rate was found in predominant cases, 94.7%. The mean union time was 14.3 ± 4.1 weeks. The mean operative time was 101.6 ± 23.6 minutes (Table 7). Functional outcome was assessed based on the Friedman and Wyman scoring system. Good results were obtained in 32 cases (84.2%), fair results in 6 cases (15.8%), and no poor outcome was found. According to the Friedman and Wyman [25] scoring system, good and fair results were considered satisfactory (Figure 2 and 3). The poor results were considered unsatisfactory. In our study, none of them had unsatisfactory results.
|
Age (in years) |
Frequency (n) |
Percentage (%) |
|
≤ 20 |
10 |
26.3 |
|
21-30 |
10 |
26.3 |
|
31-40 |
8 |
21.1 |
|
41-50 |
4 |
10.5 |
|
≥ 51 |
6 |
15.8 |
|
Total |
38 |
100 |
|
Mean ± SD |
32.84 ± 13.94 |
|
|
Range |
(18-60) years |
|
Table 1: Age distribution of the study population (N=38).
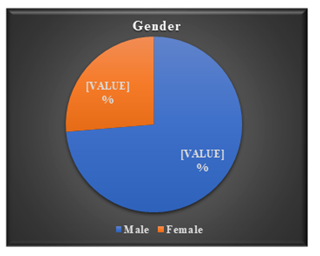
Figure 1: Gender distribution of the study population.
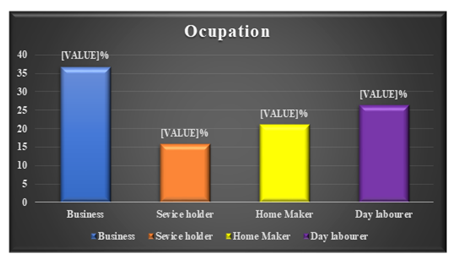
Figure 2: Occupation distribution of the study population (N=38).
|
Variables |
Frequency (n) |
Percentage (%) |
|
Mode of injury |
||
|
Road traffic accident (RTA) |
30 |
78.9 |
|
Fall from height |
6 |
15.8 |
|
Fall of heavy object |
2 |
5.3 |
|
Side |
||
|
Right |
24 |
63.2 |
|
Left |
14 |
36.8 |
|
Pattern of fracture |
||
|
Transverse |
24 |
63.1 |
|
Spiral |
8 |
21.1 |
|
Oblique |
6 |
15.8 |
Table 2: Feature of the injury of the study population (N=38).
|
Days |
Frequency (n) |
Percentage (%) |
|
1-7 |
16 |
42.1 |
|
>7 |
22 |
57.9 |
|
Total |
38 |
100 |
|
Mean ± SD |
8.1 ± 2.32 days |
|
Table 3: Distribution of the study patients by interval between admission and surgery (N=38).
|
Variables |
Frequency (n) |
Percentage (%) |
|
Knee flexion (Degree) |
||
|
0-110 |
2 |
5.3 |
|
0-130 |
10 |
26.3 |
|
0-135 |
12 |
31.5 |
|
0-140 |
8 |
21.1 |
|
0-80 |
2 |
5.3 |
|
0-90 |
4 |
10.5 |
|
Limb length discrepancy |
||
|
1 cm |
2 |
5.3 |
|
No discrepancy |
36 |
94.7 |
Table 4: Distribution of the study patients by knee flexion and limb length discrepancy (N=38).
|
Complication |
Frequency (n) |
Percentage (%) |
|
Malalignment |
||
|
5o recurvatum |
2 |
5.3 |
|
5o Varus |
2 |
5.3 |
|
Internal/external rotation |
0 |
0 |
|
No malalignment |
34 |
89.4 |
|
Infection (Type) |
||
|
Superficial infection |
0 |
0 |
|
Deep infection |
0 |
0 |
|
No infection |
38 |
100 |
Table 5: Complications of the study.
|
Length of hospital stay (days) |
Frequency (n) |
Percentage (%) |
|
Up to 10 days |
14 |
36.8 |
|
> 10 days |
24 |
63.2 |
|
Total |
38 |
100 |
|
Mean ± SD |
11.7 ± 2.3 |
|
|
Range |
(8-15) days |
|
Table 6: Distribution of the study patients by length of hospital stay (N=38).
|
Characteristics |
Frequency (n) |
Percentage (%) |
|
Union |
36 |
94.7 |
|
Delayed Union |
2 |
5.3 |
|
Total |
38 |
100 |
|
Union time (weeks) |
||
|
Mean ± SD |
14.3 ± 4.1 |
|
|
Range |
(10-24) weeks |
|
|
Operative time (minutes) |
||
|
Mean ± SD |
101.6 ± 23.6 |
|
|
Range |
(80-170) minutes |
|
Table 7: Distribution of the study participants according to union characteristics (N=38).
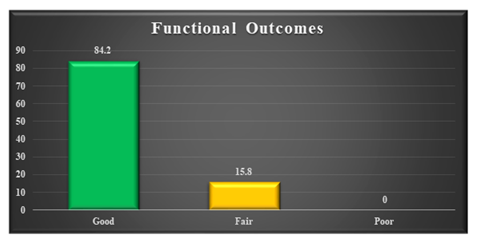
Figure 3: Function outcomes of the study population (N=38).
4. Discussion
This Quasi-experimental study was conducted in the Department of Orthopedics, Dhaka Medical College Hospital, Dhaka, from July 2017 to June 2019, including 38 patients with clinical and radiological evidence of closed fracture of the shaft of femur admitted to hospitals for operation. The study aimed to evaluate the functional outcome of treating a diaphyseal fracture of the femur by closed-reamed interlocking intramedullary nails. The treatment of shaft femur fractures has been revolutionized by the advent of Kuntscher’s nail in 1940 [16]. The scope of femoral shaft nailing has been broadened with reaming and interlocking of intramedullary nails. Since then, the unacceptable rates of malunion and non-union shown by various conservative treatment methods have fallen dramatically. In the present study, the majority of the patients, 10(26.3%), were in the second decade of life, as well as 10(26.3%) in the third decade and 8(21.1%) in the fourth decade. The mean age of the patients was 32.84 ± 13.94 years. Tiwari et al. [17] reported that a maximum of the patients (53.5%) were in the second decade of life, followed by 17.1% in the third decade and 14.7% in the fourth decade, and the mean age of the patients was 29.7 ± 11.21 years [17]. Another study by Winquist et al. [18] reported the 3rd, fourth, and fifth decades as a common age group, i.e., 70% middle age group population, with a mean age of 29 years age group population [18]. In present study among 38 patients 28(73.66%) were male and 10(26.32%) were female. Male: Female ratio 2.8:1. In agreement with this study, Tiwari et al. [17] reported in their study that male preponderance (85.3%) in the study while female patients constituted 14.7% of the study group [17]. Deepak et al. [19] reported 75% male predominance in 120 patients [19]. A male predominance has been reported in different previous studies. In their study, Bhandari et al. [20] reported a gender ratio of 6.69:1. In different Indian studies, too, a male predominance has been reported. However, Arun et al. [4] reported this ratio as 2.33:1, and CV and Shivanna [21] reported this ratio as 1.72:1, which is less than that in the present study. Thus, irrespective of the environment, all the studies show a skewed gender ratio, with more affected males than females. The reason for the predominance of males compared to females could be that these fractures are often afflicted by high-impact injuries, which is congruent to the traditional gender-related differences in activity profile. There were 38 cases in this study, most young males between 18-40 years of age making 63.2% of the total. Most young people lead an active life, are affected by road traffic accidents (78.9%), and are victims of falls from height (15.8%). As mentioned earlier, road traffic accident (RTA) was responsible for most femoral shaft fractures, followed by fall from height. Most victims of falls from height were either laborers working in the under-construction building or working on their farms and from trees. Mohammad et al. [7] presented with a history of falls of 66 (57.89%) and RTA 48 (42.11%) out of 114 patients. Tiwari et al. [17] reported that road traffic accident was the main cause of fracture (51.3%), whereas 46.3% and 2.4% of fractures were due to fall and assault, respectively. Metsemakers et al. [22] reported that road traffic accidents were the most common cause of injuries involving 172 patients (74.8%). This observation by various authors implies that fracture shaft femur is usually a result of high-energy trauma, so it is commonly associated with other injuries. In the present study, among the 38 patients, a maximum (36.84%) were business people, 26.32% of patients were laborers, 21.05% were homemakers, and 15.79% were service holders. The results of our study are comparable to another study. The study shows right-sided predominance compared to the left side (63.2% vs. 36.8%). Tiwari et al. [17] reported 61.1% with right-sided femoral shaft fractures and 38.9% patients with left [17]. Another study done by Deepak et al. [19] noted unilateral cases of closed fracture type with slightly higher involvement of the right (55%) as compared to the left side. The injury to surgery interval for 16(42.1%) patients was less than 7 days and more than 7 days for 22(57.9%) patients before getting operated. The average injury surgery interval was 8.1 days. Tiwari et al. [17] demonstrated that the injury to surgery interval for 7 (17.1%) patients was less than 24 hours, 1-3 days for 16 (39.1%) patients, 4-6 days for 16 (39.1%) patients and 2 (4.9%) patients had to wait for more than 6 days before operation. The average injury-surgery interval was 3.7 days. In current series transverse fractures were 24(63.1%), spiral fractures were 8(21.1%) and oblique were 6(15.8%) cases. Tiwari et al. [17] reported that the majority of the fractures (51.2%) were transverse fractures, followed by spiral and comminuted fractures (17.1%) and oblique (14.6%). Deepak et al. [19] reported that the most common pattern of fracture was comminuted and transverse fractures. In the present study, maximum patients 30(78.9%) had full range of knee flexion (>120 degree), 6(15.8%) patients had < 90 degree and 2(5.3%) patient 110 degree of knee flexion. Tiwari et al. [17] reported that 8(19.5%) and 2 (4.8%) patients had knee flexion <120º and <90º respectively. Wiss et al. [23] reported an average knee flexion of 125 degrees, with only 3 patients having less than 90-degree flexion. Mohammad et al. [7] represented a full range of movements (from 0-1300) in 102 patients (89.47%). Seven patients (6.14%) had a range of movements from 0 to 90. Five patients (4.38 %) had a knee range of movements 0-600, consistent with the present study. In the present study, only 2(5.3%) patients had 1cm limb length shortening, and 4(10.5%) patients had 5-degree malalignment. Tiwari et al. [17] noted in their study that 2(4.8%) and 1 (2.4%) patient had limb length shortening by 2 cm and 1 cm respectively. Deepak et al. [19] reported that the shortening of the limb was seen in four cases (13.33%), of which two had 2 cm shortening, and the other two cases had 1 to 1.5 cm shortening. In the present study, the mean duration of operation was 101.6 ± 23.6 minutes (range 80 to 170 minutes), which is quite satisfactory regarding the outcome and safety of patients and surgeons as C-Arm is used throughout the procedure. A similar study done by Umar et al. [24] showed the mean duration of surgery was 180 minutes (range 120 to 540 minutes) ±SD (76 minutes). So, it is quite impressive in our study. In the present study, 36(94.7%) patients achieved union. The average time for healing of the fracture was 14.3 ± 4.1 weeks. Two patients developed delayed union and needed dynamization. CV and Shivanna [21] showed in their study that the average union time was 16.84 weeks. Qureshi et al. [10] reported a mean union time of 14.3 ± 1.3 weeks, similar to our study. In the present study, a maximum of patients, 24(63.2%) had a total hospital stay of more than 10 days, followed by 14(36.8%) patients who had up to 10 days. Minimum hospital stays are 8 days and maximum 15 days. The average hospital stay was 11.7 days. In agreement with the present study, Tiwari et al. [17] reported that the hospital stay of all patients ranged between 8 to 24 days. 19 (46.3%) patients were admitted to the hospital for 7-14 days, while 51.3% and 2.4% were admitted for 15-21 and 21-28 days respectively. The mean hospital stay was 15.4 ± 3.71 days. Metsemakers et al. [25] found that the mean duration for the hospitalization period was 15 days. The current study assessed functional outcomes based on Friedman and Wyman criteria [25]. Good results were obtained in 32 cases (84.2%), fair results in 6 cases (15.8%), and no poor outcome was found. In our study, none of them had unsatisfactory results. Our results are comparable to other standard studies [9,25]. Another recent study by CV and Shivanna [21] noted 83.34% good, 6.67% fair, and 10% poor results by closed reduction and internal fixation using intramedullary interlocking nailing for the fractured shaft of the femur.
4. Limitations of the Study
Every hospital-based study has limitations, and the present study is no exception. The limitations of the present study are mentioned. Therefore, the present study's results may differ from the whole of the country or the world at large. The study was done in a limited period; cases were collected from only one center and may only represent part of the country's population. The sample size was small. Follow-up was short. C-Arm was out of order from February 2019 to July 2019. Patients are very reluctant to follow up.
6. Conclusion and Recommendations
In light of the findings of the study, it can be concluded that closed Intramedullary interlocking nailing is an effective, successful, and time-tested method of treatment for diaphyseal fractures of the femoral shaft because of stable fixation, lower rate of complications like infection or non-union and allows early weight bearing & return to routine activities. Interlocking nailing gives rotational and axial stability and should be given a choice for diaphyseal femur fracture treatment whenever possible. Further multi-centered cohort studies with large sample sizes should be recommended. Further prospective study with a larger sample and longer follow-up period is recommended. Adequate instruments, especially C-Arm, should be made available round the clock at the emergency operation theatre.
Declarations:
Funding:
No funding sources
Conflict of interest:
None declared
Ethical approval:
The study was approved by the Institutional Ethics Committee.
References
- Dim EM, Ugbeye ME, Ugwoegbulem OA. Adult traumatic femoral shaft fractures: A review of the literature. Ibom Medical Journal 5 (2012): 26-38.
- Shafi MK, Ahmed N, Khan AH, et al. Results of fracture union in closed reamed interlocking nail in fractures of femur. Pak J Med Sci 24 (2008): 698-701.
- Qureshi ZZ, Shah SW, Kumar J, et al. Management of diaphyseal femur fractures in adults with intramedullary interlocking nail. Biomedica 28 (2012): 117-120.
- Kumar A, Krishnaiah G, Biju R, et al. Study of outcome of closed interlocking intramedullary nailing of fracture shaft of femur in adults. IOSR J Dent Med Sci 14 (2015): 48-52.
- Ajit S, Amit S. Interlocking nailing of femoral diaphyseal fractures: Review of 47 cases. International Journal of Pharmaceutical Science Invention (IJPSI) 2 (2013): 20-23.
- Maruthi CV. Closed intramedullary interlocking nailing for fracture shaft of femur: Prospective study. International Journal of Orthopaedics 3 (2017): 602-604.
- Mohammad T, Sawati A, Ahmed A, et al. Outcomes in closed reamed interlocking nail in fractures of shaft of femur. Journal of Ayub Medical College Abbottabad 27 (2015): 811-816.
- Christie J, Kinninmonth AW, Howie CR. Intramedullary locking nails in the management of femoral shaft fractures. The Journal of Bone and Joint Surgery British 70 (1988): 206-210.
- Vécsei V, Hajdu S, Negrin LL. Intramedullary nailing in fracture treatment: history, science and Küntscher's revolutionary influence in Vienna, Austria. Injury 42 (2011): S1-S5.
- Quasem MF, Faruquee SR, Kamruzzama M, et al. Femoral Shaft fractures treated with Interlocking Intramedullary Nailing: A report of 127 cases. Journal of Bangladesh Orthopaedic Society 24 (2009): 79-84.
- Anastopoulos G, Asimakopoulos A, Exarchou E, et al. Closed interlocked nailing in comminuted and segmental femoral shaft fractures. Journal of Trauma and Acute Care Surgery 35 (1993): 772-775.
- Deshmukh RG, Lou KK, Neo CB, et al. A technique to obtain correct rotational alignment during closed locked intramedullary nailing of the femur. Injury 29 (1998): 207-210.
- Gupta C, Singh D, Kumar D, et al. Comprehensive study regarding intramedullary nailing in fractures of the femoral shaft. Int J Curr Res Med Sci 3 (2017): 25-33.
- Babb JR, Ahn JI, Azar FM, et al. Transphyseal anterior cruciate ligament reconstruction using mesenchymal stem cells. The American Journal of Sports Medicine 36 (2008): 1164-1170.
- Husni ME, Losina E, Fossel AH, et al. Decreasing medical complications for total knee arthroplasty: effect of critical pathways on outcomes. BMC Musculoskeletal Disorders 11 (2010): 1-7.
- Mostofi SB. Gerhard Küntscher 1900–1972. Who’s Who in Orthopedics (2005): 179-181.
- Tiwari A, Kohli SS, Kokne M. Study of management of diaphyseal fracture shaft femur by intramedullary interlocking nail. International Journal of Research in Orthopaedics 5 (2019): 1.
- Winquist RA, Hansen Jr ST, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. JBJS 66 (1984): 529-539.
- Deepak CD, Chethan BA. A study of functional outcome of femoral diaphyseal fractures by closed reduction and internal fixation using intramedullary interlocking nail in adults. International Journal of Orthopaedics Sciences 1 (2019): 132-138.
- Bhandari M, Guyatt GH, Tong D, et al. Reamed versus nonreamed intramedullary nailing of lower extremity long bone fractures: a systematic overview and meta-analysis. Journal of orthopaedic trauma. 14 (2000): 2-9.
- Maruthi CV. Closed intramedullary interlocking nailing for fracture shaft of femur: Prospective study. International Journal of Orthopaedics 3 (2017): 602-604.
- Metsemakers WJ, Roels N, Belmans A, et al. Risk factors for nonunion after intramedullary nailing of femoral shaft fractures: remaining controversies. Injury 46 (2015): 1601-1607.
- Wiss DA, Fleming CH, Matta JM, et al. Comminuted and rotationally unstable fractures of the femur treated with an interlocking nail. Clinical Orthopaedics and Related Research (1976-2007) 212 (1986): 35-47.
- Asif S, Umer M, Beg R, et al. Operative treatment of bilateral hip dislocation in children with arthrogryposis multiplex congenita. Journal of Orthopaedic Surgery 12 (2004): 4-9.
- Friedman RJ, Wyman JR ET. Ipsilateral hip and femoral shaft fractures. Clinical Orthopaedics and Related Research 208 (1986): 188-194.
