Outcome of C-arm Guided Epidural Steroid Injections in Patients with Prolapsed Lumbar Intervertebral Disc with Radiculopathy
Article Information
Tamjid Ali MD1*, Moshiur Rahman Khasru2, Salek AKM3, Alauddin Sikdar4, Quazi Tamanna Haque5
1Consultant Physiatrist, Department of Physical Medicine and Rehabilitation, Rajshahi Medical College Hospital, Bangladesh
2Associate Professor, Department of Physical Medicine and Rehabilitation, BSMMU, Dhaka, Bangladesh
3Professor and Chairman, Department of Physical Medicine and Rehabilitation, Khulna Medical College Hospital, Bangladesh
4Consultant Physiatrist, Department of Microbiology, Rajshahi Medical College, Bangladesh
5Lecturer, Department of Microbiology, Rajshahi Medical College, Bangladesh
*Corresponding Author: Tamjid Ali, Department of Physical Medicine and Rehabilitation, Rajshahi Medical College Hospital. Bangladesh.
Received: 03 June 2023; Accepted: 09 June 2023; Published: 12 June 2023
Citation:
Tamjid Ali, Moshiur Rahman Khasru, Salek AKM, Alauddin Sikdar, Quazi Tamanna Haque. Outcome of C-arm guided Epidural Steroid Injections in Patients with Prolapsed Lumbar Intervertebral Disc with Radiculopathy. Journal of Orthopedics and Sports Medicine. 5 (2023): 286-292.
Share at FacebookAbstract
Background: Prolapsed Lumbar Intervertebral Disc (PLID) is one of the most common health problems worldwide, as well as in our country, and is one of the potential causes of temporary disability, morbidity, and reasoning of absence at workplaces.
Objective: To find out the outcome of C-arm guided transforaminal and caudal epidural steroid injection for low back pain with radiculopathy due to PLID.
Methodology: This was a randomized clinical trial conducted among purposively selected 54 patients with PLID with radiculopathy as per selection criteria, attending the Department of Physical Medicine & Rehabilitation in BSMMU, Dhaka, from March 2020 to February 2021. Patients (N=54) were randomly allocated into two groups; patients in group A (n=26) were treated with C-arm guided transforaminal and caudal epidural steroid injection with conservative treatment, and patients in group B (n=28) were treated with conservative treatment only. All patients were followed up in 1st week, 1st month, and 3rd month.
Results: The mean age of the participants in group A and group B were 40.88 (± 8.70) and 43.00 (± 11.54) years, respectively. In group A, 9 (34.6%) were housewives, 4 (15.4%) were manual workers, while in group B, 10 (35.7%) were housewives, and 8 (28.6%) were manual workers. In group A, 21 (80.8%) had three disc involvement, while in group B, 19 (67.9%) had three discs involvement, where L4-5-disc involvement was most common in both groups. There was no significant statistical difference between the groups regarding VAS scores at baseline (p=0.235), 1st week (p=0.164), and 1st month (p=0.125). The VAS score was significantly reduced in group A compared to group B at 3rd month (p=0.001). The ODI score was significantly reduced in group A compared to group B at 1st week (p=0.034), 1st month (p=0.016), and at 3rd month (p=0.001).
Conclusion: C-arm guided transforaminal and caudal Epidural Steroid Injection significantly improves pain and functional outcomes of patients with radiculopathy due to PLID. Long-term, large scale and multicenter research studies are required to establish the outcome and effectiveness of this procedure.
Keywords
Prolapsed lumbar intervertebral disc; C-arm guided transforaminal and caudal Epidural Steroid Injection; Visual analogue scale; Oswestry Disability Index
Physical medicine articles Physical medicine Research articles Physical medicine review articles Physical medicine PubMed articles Physical medicine PubMed Central articles Physical medicine 2023 articles Physical medicine 2024 articles Physical medicine Scopus articles Physical medicine impact factor journals Physical medicine Scopus journals Physical medicine PubMed journals Physical medicine medical journals Physical medicine free journals Physical medicine best journals Physical medicine top journals Physical medicine free medical journals Physical medicine famous journals Physical medicine Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Lumbar intervertebral discs articles Lumbar intervertebral discs Research articles Lumbar intervertebral discs review articles Lumbar intervertebral discs PubMed articles Lumbar intervertebral discs PubMed Central articles Lumbar intervertebral discs 2023 articles Lumbar intervertebral discs 2024 articles Lumbar intervertebral discs Scopus articles Lumbar intervertebral discs impact factor journals Lumbar intervertebral discs Scopus journals Lumbar intervertebral discs PubMed journals Lumbar intervertebral discs medical journals Lumbar intervertebral discs free journals Lumbar intervertebral discs best journals Lumbar intervertebral discs top journals Lumbar intervertebral discs free medical journals Lumbar intervertebral discs famous journals Lumbar intervertebral discs Google Scholar indexed journals Disc herniation articles Disc herniation Research articles Disc herniation review articles Disc herniation PubMed articles Disc herniation PubMed Central articles Disc herniation 2023 articles Disc herniation 2024 articles Disc herniation Scopus articles Disc herniation impact factor journals Disc herniation Scopus journals Disc herniation PubMed journals Disc herniation medical journals Disc herniation free journals Disc herniation best journals Disc herniation top journals Disc herniation free medical journals Disc herniation famous journals Disc herniation Google Scholar indexed journals Rheumatic diseases articles Rheumatic diseases Research articles Rheumatic diseases review articles Rheumatic diseases PubMed articles Rheumatic diseases PubMed Central articles Rheumatic diseases 2023 articles Rheumatic diseases 2024 articles Rheumatic diseases Scopus articles Rheumatic diseases impact factor journals Rheumatic diseases Scopus journals Rheumatic diseases PubMed journals Rheumatic diseases medical journals Rheumatic diseases free journals Rheumatic diseases best journals Rheumatic diseases top journals Rheumatic diseases free medical journals Rheumatic diseases famous journals Rheumatic diseases Google Scholar indexed journals Radiculopathy articles Radiculopathy Research articles Radiculopathy review articles Radiculopathy PubMed articles Radiculopathy PubMed Central articles Radiculopathy 2023 articles Radiculopathy 2024 articles Radiculopathy Scopus articles Radiculopathy impact factor journals Radiculopathy Scopus journals Radiculopathy PubMed journals Radiculopathy medical journals Radiculopathy free journals Radiculopathy best journals Radiculopathy top journals Radiculopathy free medical journals Radiculopathy famous journals Radiculopathy Google Scholar indexed journals Epidural steroid injection articles Epidural steroid injection Research articles Epidural steroid injection review articles Epidural steroid injection PubMed articles Epidural steroid injection PubMed Central articles Epidural steroid injection 2023 articles Epidural steroid injection 2024 articles Epidural steroid injection Scopus articles Epidural steroid injection impact factor journals Epidural steroid injection Scopus journals Epidural steroid injection PubMed journals Epidural steroid injection medical journals Epidural steroid injection free journals Epidural steroid injection best journals Epidural steroid injection top journals Epidural steroid injection free medical journals Epidural steroid injection famous journals Epidural steroid injection Google Scholar indexed journals Orthopaedic surgery articles Orthopaedic surgery Research articles Orthopaedic surgery review articles Orthopaedic surgery PubMed articles Orthopaedic surgery PubMed Central articles Orthopaedic surgery 2023 articles Orthopaedic surgery 2024 articles Orthopaedic surgery Scopus articles Orthopaedic surgery impact factor journals Orthopaedic surgery Scopus journals Orthopaedic surgery PubMed journals Orthopaedic surgery medical journals Orthopaedic surgery free journals Orthopaedic surgery best journals Orthopaedic surgery top journals Orthopaedic surgery free medical journals Orthopaedic surgery famous journals Orthopaedic surgery Google Scholar indexed journals Spondylolisthesis articles Spondylolisthesis Research articles Spondylolisthesis review articles Spondylolisthesis PubMed articles Spondylolisthesis PubMed Central articles Spondylolisthesis 2023 articles Spondylolisthesis 2024 articles Spondylolisthesis Scopus articles Spondylolisthesis impact factor journals Spondylolisthesis Scopus journals Spondylolisthesis PubMed journals Spondylolisthesis medical journals Spondylolisthesis free journals Spondylolisthesis best journals Spondylolisthesis top journals Spondylolisthesis free medical journals Spondylolisthesis famous journals Spondylolisthesis Google Scholar indexed journals Body Mass Index articles Body Mass Index Research articles Body Mass Index review articles Body Mass Index PubMed articles Body Mass Index PubMed Central articles Body Mass Index 2023 articles Body Mass Index 2024 articles Body Mass Index Scopus articles Body Mass Index impact factor journals Body Mass Index Scopus journals Body Mass Index PubMed journals Body Mass Index medical journals Body Mass Index free journals Body Mass Index best journals Body Mass Index top journals Body Mass Index free medical journals Body Mass Index famous journals Body Mass Index Google Scholar indexed journals Visual Analog Scale articles Visual Analog Scale Research articles Visual Analog Scale review articles Visual Analog Scale PubMed articles Visual Analog Scale PubMed Central articles Visual Analog Scale 2023 articles Visual Analog Scale 2024 articles Visual Analog Scale Scopus articles Visual Analog Scale impact factor journals Visual Analog Scale Scopus journals Visual Analog Scale PubMed journals Visual Analog Scale medical journals Visual Analog Scale free journals Visual Analog Scale best journals Visual Analog Scale top journals Visual Analog Scale free medical journals Visual Analog Scale famous journals Visual Analog Scale Google Scholar indexed journals Sensory involvement articles Sensory involvement Research articles Sensory involvement review articles Sensory involvement PubMed articles Sensory involvement PubMed Central articles Sensory involvement 2023 articles Sensory involvement 2024 articles Sensory involvement Scopus articles Sensory involvement impact factor journals Sensory involvement Scopus journals Sensory involvement PubMed journals Sensory involvement medical journals Sensory involvement free journals Sensory involvement best journals Sensory involvement top journals Sensory involvement free medical journals Sensory involvement famous journals Sensory involvement Google Scholar indexed journals Sequestrated disc articles Sequestrated disc Research articles Sequestrated disc review articles Sequestrated disc PubMed articles Sequestrated disc PubMed Central articles Sequestrated disc 2023 articles Sequestrated disc 2024 articles Sequestrated disc Scopus articles Sequestrated disc impact factor journals Sequestrated disc Scopus journals Sequestrated disc PubMed journals Sequestrated disc medical journals Sequestrated disc free journals Sequestrated disc best journals Sequestrated disc top journals Sequestrated disc free medical journals Sequestrated disc famous journals Sequestrated disc Google Scholar indexed journals Overweight articles Overweight Research articles Overweight review articles Overweight PubMed articles Overweight PubMed Central articles Overweight 2023 articles Overweight 2024 articles Overweight Scopus articles Overweight impact factor journals Overweight Scopus journals Overweight PubMed journals Overweight medical journals Overweight free journals Overweight best journals Overweight top journals Overweight free medical journals Overweight famous journals Overweight Google Scholar indexed journals Physical therapy articles Physical therapy Research articles Physical therapy review articles Physical therapy PubMed articles Physical therapy PubMed Central articles Physical therapy 2023 articles Physical therapy 2024 articles Physical therapy Scopus articles Physical therapy impact factor journals Physical therapy Scopus journals Physical therapy PubMed journals Physical therapy medical journals Physical therapy free journals Physical therapy best journals Physical therapy top journals Physical therapy free medical journals Physical therapy famous journals Physical therapy Google Scholar indexed journals
Article Details
1. Introduction
Lumbar intervertebral discs are complex structures that undergo significant axial loading, flexion/extension, lateral bending, and rotational forces. Because of the biomechanical demands placed upon these structures and their inability to remodel due to their avascular nature, lumbar disc prolapse is common [1]. The prolapsed lumbar intervertebral disc (PLID) can lead to substantial radicular symptoms, which, if persistent, may require surgical intervention [2]. More than 95% of lumbar disc herniation occurs at the L4-L5 and L5-S1 levels; the next most common is L3-L4, followed by L2-L3. Consequently, the most common lumbosacral radiculopathies are L5 and S1 [3]. The mean age of patients with a herniated disc was 41 years, with a male preponderance [4].
Al-Hasan et al. [5] reported in the Community Oriented Program for Control of Rheumatic Diseases (COPCORD) study that 174 per thousand Bangladeshi population with non-inflammatory back pain had PLID. Alike Cummins and Coworkers, male predominance (63.3%) was observed among respondents with PLID in Bangladesh [5]. There are some risk factors for PLID development, such as (i) obesity, (ii) individual involved in a physically demanding occupation, and (iii) positive family history for PLID [1].
Lumbar radiculopathy secondary to disc herniation resolved spontaneously in 23 to 48 % of cases. However, about 30 to 70 % of cases had pronounced symptoms after one year, with 5% to 15% of patients undergoing surgery resulting in high economic impact and strain on health services [6].
1.1 General objective
- To find out the outcome of C-arm guided transforaminal and caudal epidural steroid injection for low back pain with radiculopathy due to PLID
1.2 Specific objective
- To find out the effect on the severity and intensity of pain after C-arm guided transforaminal and caudal epidural steroid injection in patients with PLID with radiculopathy
- To determine the functional outcome of patients with PLID with radiculopathy after C-arm guided Transforaminal Epidural Steroid Injection (TFESI) and Caudal Epidural Steroid Injection (CESI)
- To compare the pain and functional outcome of radiculopathy due to PLID between the patients treated with C-arm guided Transforaminal Epidural Steroid Injection (TFESI) and Caudal Epidural Steroid Injection (CESI) along with standard conservative treatment and the patients who received only standard conservative treatment
2. Materials and Methods
This Randomized clinical trial study was conducted in the Department of Physical Medicine and Rehabilitation, BSMMU, in collaboration with the Department of Orthopaedic Surgery, BSMMU, and Dr. Sirajul Islam Medical College Hospital, Dhaka. from March 2020 to February 2021.
2.1 Inclusion criteria
- Patients with clinically diagnosed and MRI confirmed PLID with radiculopathy refractory to adequate standard conservative treatment
- Patients willing to participate and give informed written consent
2.2 Exclusion criteria
- Herniated disc with motor involvement
- Sensory involvement (Saddle anesthesia)
- Autonomic involvement (Incontinence of bowel and bladder)
- Sequestrated disc
- Patients with inflammatory back pain
- Spondylolisthesis
- Uncontrolled diabetes mellitus and hypertension
- History of receiving C-arm guided TFESI and CESI within the last six months
2.3 Data collection method
Data was collected through face-to-face interviews and a semi-structured questionnaire using assessment scales. All efforts were made to collect data accurately. For open questions, the respondents were asked in such a manner so that they could speak freely and explain their opinion in a normal and neutral way. No leading questions were asked.
2.4 Ethical consideration
From the ethical point of view, keeping compliance with Helsinki Declaration for Medical Research Involving Human Subjects 1964, a written consent was taken from all patients for inclusion in the study. The process of the treatment was simplified and explained to the patients. Voluntary participations were encouraged. When the researcher was assured that the patient completely understood the study protocol and became aware of his/her rights during the study, the written consent form was signed or fingerprinted by the patient. Before starting this study ethical clearance was taken from Institutional Review Board (IRB) of BSMMU. Permission was also taken from department of Orthopedic Surgery and Dr. Sirajul Islam Medical College and Hospital. The process of treatment had no harm for their health, and they had authority to stop the process of treatment. They were assured of protection of patients’ autonomy, privacy, confidentiality. Data taken from the participants were regarded as confidential and kept locked under investigator for purposeful use only.
3. Results
A total 65 respondents were enrolled in the study. In group A, 26 participants completed 3 months follow-ups, whereas in group B 28 participants completed follow up (Figure 1-7). However, 11 (17%) participants (Group-A=6 and Group-B=5) were dropped out and could not complete pre-scheduled follow-up due to the COVID-19 pandemic situation and its consequences, such as a lockdown. Therefore, 54 samples were considered in the final statistical analysis.
Table 1 shows that in group A, 23 (88.5%) were from the <50 years' age group, while in group B, 20 (71.4%) were from the <50 years' age group. No significant statistical difference was found between the groups regarding age as p=0.179 (obtained by Chi-square test). The mean age of the participants in group A and group B were 40.88 (± 8.70) and 43.00 (± 11.54) years, respectively.
|
Age group (in years) |
Group A (n =26) |
Group B (n=28) |
p value |
|
<50 |
23 (88.5%) |
20 (71.4%) |
0.179 |
|
51-60 |
3 (11.5%) |
8 (28.6%) |
|
|
Total |
26 (100.0%) |
28 (100.0%) |
|
|
Mean ± SD |
40.88 ± 8.70 |
43.00 ± 11.54 |
|
|
N=Total study participants, n=Participants in group |
|||
Table 1: Distribution of age of the study participants (N=54).
|
Gender |
Group A (n =26) |
Group B (n=28) |
p value |
|
Male |
14 (57.7%) |
12 (42.9%) |
0.586 |
|
Female |
12 (46.2%) |
16 (57.1%) |
|
|
Total |
26 (100.0%) |
28 (100.0%) |
|
|
N=Total study participants, n=Participants in group |
|||
Table 2: Distribution of gender of the study participants (N=54).
Table 2 shows that in group A, 14 (57.7%) were male, while 12 (42.9%) were male in group B. No significant statistical difference was found between the groups regarding gender as p=0.586 (obtained by Chi-square test).
3.1 Distribution of occupational status of study participants (N=54)

Figure 1: Shows that in group A, 9 (34.6%) were housewives, 4 (15.4%) were manual workers, while in group B, 10 (35.7%) were housewives and 8 (28.6%) were manual workers. No significant statistical difference was found between the groups regarding occupational status as p=0.685 (obtained by Fisher's Exact test).
Table 3 shows that in group A, 7 (26.9%) were from the lower class and 16 (61.5%) were from the lower middle class; while in group B, 13 (46.4%) were from the lower class and 14 (50.0%) were from the lower middle class. No significant statistical difference was found between the groups regarding socio-economic status as p=0.407 (obtained by Fisher's Exact test).
|
Socio-economic status |
Group A (n =26) |
Group B (n=28) |
p value |
|
Lower class |
7 (26.9%) |
13 (46.4%) |
0.407 |
|
Lower middle class |
16 (61.5%) |
14 (50.0%) |
|
|
Upper middle class |
2 (7.7%) |
1 (3.6%) |
|
|
Higher class |
1 (3.8%) |
0 (0.0%) |
|
|
Total |
26 (100.0%) |
28 (100.0%) |
|
|
N=Total study participants, n=Participants in group |
|||
Table 3: Distribution of socio-economic status of study participants (N=54).
Table 4 shows that in group A, 17 (65.4%) had normal weight while 19 (67.9%) had normal weight in group B. No significant statistical difference was found between the groups regarding BMI as p=1.000 (obtained by Chi-square test). The mean BMI of the participants in group A and group B was 23.98 (± 2.87) and 24.11 (± 2.52) kg/m2, respectively.
|
Body Mass Index (BMI) |
Group A (n =26) |
Group B (n=28) |
p value |
|
Normal weight |
17 (65.4%) |
19 (67.9%) |
1 |
|
Over weight |
9 (34.6%) |
9 (32.1%) |
|
|
Total |
26 (100.0%) |
28 (100.0%) |
|
|
N=Total study participants, n=Participants in group |
|||
Table 4: Distribution of Body Mass Index (BMI) of study participants (N= 54).
3.2 Distribution of study participants by comorbidity (N=54)
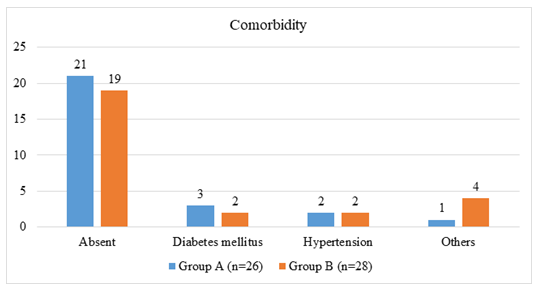
Figure 2: shows that in group A, 21 (80.8%) had no comorbidity and 3 (11.5%) had diabetes mellitus while in group B, 19 (67.9%) had no comorbidity and 2 (7.1%) had diabetes mellitus.
Table 5 shows that in group A, 23 (88.5%) had a duration of a symptom of>90 days, while in group B, 24 (85.7%) had a duration of a symptom of>90 days. No significant statistical difference was found between the groups regarding the duration of symptoms as p=0.945 (obtained by Chi-square test).
|
Duration (in days) |
Group A (n =26) |
Group B (n=28) |
P value |
|
42-90 |
3 (11.5%) |
4 (14.3%) |
1 |
|
>90 |
23 (88.5%) |
24 (85.7%) |
|
|
Total |
26 (100.0%) |
28 (100.0%) |
|
|
N=Total study participants, n=Participants in group |
|||
Table 5: Distribution of duration of symptom of study participants (N=54).
3.3 Distribution of disc involvement among groups (N=54)
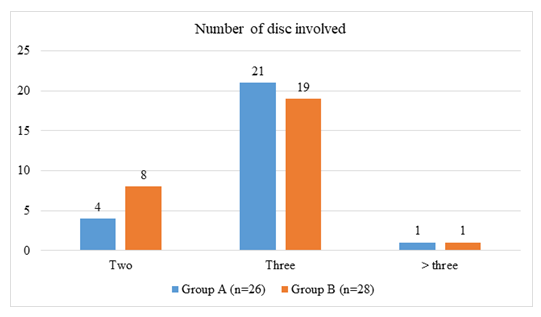
Figure 3: shows that in group A, 21 (80.8%) had three discs' involvement, while in group B, 19 (67.9%) had three discs' involvement. No significant statistical difference was found between the groups regarding disc involvement as p=0.659 (obtained by Fisher's Exact test).
3.4 Distribution of disc involvement (N=54)
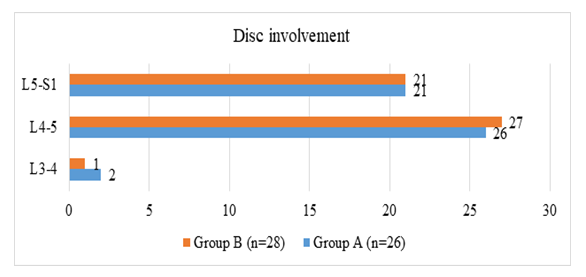
Figure 4: shows that in group A, 21 (80.8%) had L5-S1 disc involvement and 27 (87.1%) had L4-5 disc involvement. In group B, 21 (75.0%) had L5-S1 disc involvement, and 26 (92.8%) had L4-5 disc involvement.
3.5 Distribution by root involvement (N=54)
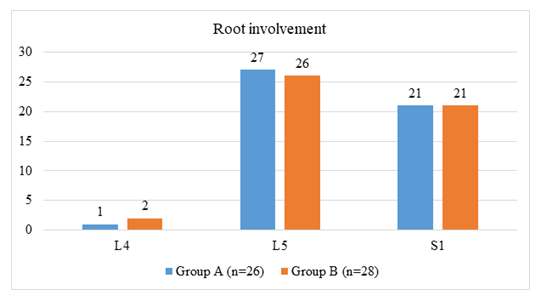
Figure 5: shows that in group A, 27 (87.1%) had L5 root involvement, and 21 (80.8%) had S1 root involvement. In group B, 26 (92.8%) had L5 root involvement, and 21 (75.0%) had S1 root involvement.
3.6 Distribution of study participants by VAS score (N=54)
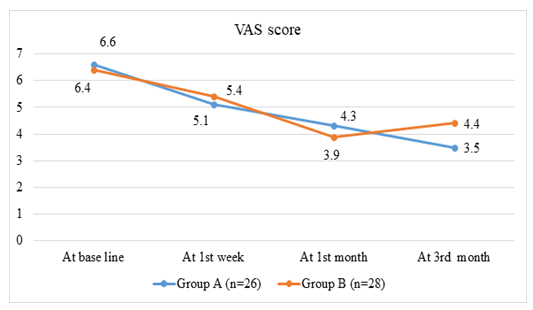
Figure 6: Shows that in group A, at the beginning of treatment, the mean VAS score of the respondents was 6.6. The VAS score gradually decreased in 1st week, 1st month, and in 3rd month, it was 3.5. In group B, at the beginning of treatment, the mean VAS score of the respondents was 6.4. The VAS score decreased in 1st week to 5.4 and in 1st month to 3.9; in 3rd month, it increased to 4.4.
Table 6 shows that there was no significant statistical difference between the groups regarding VAS scores at baseline, 1st week, and 1st month as p>0.05. Significant statistical difference was found between the groups regarding VAS scores in the 3rd month (p=0.001) (obtained by Independent sample t-test).
|
VAS |
Group A (Mean ± SD) |
Group B (Mean ± SD) |
p value |
|
At base line |
6.6 ± 0.5 (n=32) |
6.4 ± 0.8 (n=33) |
0.235 |
|
At 1st week |
5.1 ± 0.6 (n=32) |
5.4 ± 0.6 (n=33) |
0.164 |
|
At 1st month |
4.3 ± 0.9 (n=30) |
3.9 ± 0.9 (n=30) |
0.125 |
|
At 3rd month |
3.5 ± 0.9 (n=26) |
4.4 ± 0.9 (n=28) |
0.001 |
|
N=Total study participants, n=Participants in group |
|||
Table 6: Comparison of study participants by Visual Analog Scale (VAS) score (N=54).
3.7 Distribution of study participants by ODI score (N=54)

Figure 7: Shows that in group A, at the beginning of treatment, the mean ODI score of the respondents was 56.5. The ODI score gradually decreased in 1st week, 1st month, and in 3rd month, 25.7. In group B, at the beginning of treatment, the mean ODI score of the respondents was 57.3. The ODI score decreased in the 1st week to 46.8 and the 1st month to 29.6; in the 3rd month, it increased to 34.4.
Table 7 shows that the VAS scores significantly reduced after treatment from 6.3 (± 0.6) to 3.5 (± 0.9) in group A (p<0.001). The VAS scores significantly reduced after treatment from 6.5 (± 0.7) to 4.4 (± 0.9) in group B (p<0.001) (obtained by paired t-test).
|
Group |
Pre-treatment score (Mean ± SD) |
Post-treatment score (Mean ± SD) |
p value |
|
Group A (n=26) |
6.3 ± 0.6 |
3.5 ± 0.9 |
<0.001 |
|
Group B (n=28) |
6.5 ± 0.7 |
4.4 ± 0.9 |
<0.001 |
|
N=Total study participants, n=Participants in group |
|||
Table 7: Comparison of pre-treatment and post-treatment VAS scores between two groups (N=54).
Table 8 shows that there was no significant statistical difference between the groups regarding ODI scores at baseline as p=0.957. At 1st week, 1st month, and 3rd month there was a significant statistical difference between the groups regarding ODI scores as p<0.05 (obtained by independent sample t-test).
|
ODI |
Group A (Mean ± SD) |
Group B (Mean ± SD) |
p-value |
|
At base line |
56.5 ± 7.1 (n=32) |
57.3 ± 6.9 (n=33) |
0.957 |
|
At 1st week |
43.5 ± 4.8 (n=32) |
46.8 ± 6.4 (n=33) |
0.034 |
|
At 1st month |
34.8 ± 8.3 (n=30) |
29.6 ± 7.2 (n=30) |
0.016 |
|
At 3rd month |
25.7 ± 9.4 (n=26) |
34.4 ± 8.9 (n=28) |
0.001 |
|
N=Total study participants, n=Participants in group |
|||
Table 8: Comparison of study participants by Oswestry Disability Index (ODI) score (N=54).
Table 9 shows that the ODI scores significantly reduced after treatment from 57.4 (± 7.3) to 25.7 (± 9.4) in group A where (p<0.001). The ODI scores significantly reduced after treatment from 57.9 (± 7.1) to 34.4 (± 8.9) in group B where (p<0.001) (obtained by paired t-test).
|
Group |
Pre-treatment score (Mean ± SD) |
Post-treatment score (Mean ± SD) |
p-value |
|
Group A (n=26) |
57.4 ± 7.3 |
25.7 ± 9.4 |
<0.001 |
|
Group B (n=28) |
57.9 ± 7.1 |
34.4 ± 8.9 |
<0.001 |
|
N=Total study participants, n=Participants in group |
|||
Table 9: Comparison of pre-treatment and post-treatment ODI scores between two groups (N=54).
4. Discussion
The study purposively included 54 patients with clinically diagnosed and MRI-confirmed PLID refractory to adequate standard conservative treatment. Patients were randomly allocated into group A (C-arm guided transforaminal and caudal epidural steroid injection with conservative treatment) and group B (conservative treatment only). Patients with a herniated disc with motor involvement, sensory involvement (saddle anesthesia), autonomic involvement (incontinence of bladder and bowel), sequestrated disc, spondylolisthesis, uncontrolled diabetes mellitus, hypertension and history of receiving C-arm guided TFESI and CESI within last 6 months were excluded from the study.
PLID occurs most commonly in the fourth to fifth decades of life [7]. The mean ages of the study participants were 40.88 and 43.00 years in group A and group B, respectively. These results were consistent with other studies which dealt with epidural steroid injections for PLID [8]. Among the 54 patients in the present study, 51.8% patients were female. PLID is more common in men than women. Examined the rheumatic disease profile of Bangladeshi patients and found that most PLID patients were male (63.3%). Other studies also reported male predominance [9]. The dissimilarity of the result might be due to the small size of the present study. Risk factors for PLID are heavy lifting, especially with torsional stress, strenuous physical activity, and occupational driving. One-fifth of the study participants were manual workers. As most of the study participants of the present study were female, the proportion of housewives was comparatively more compared to other professions. They had to work in the kitchen room with repeated squatting and a history of using a low commode, which might be the risk factor for PLID.
Participants of the present study were mainly from lower and lower-middle classes. Few were from the upper-middle class. No significant statistical difference was found between the groups regarding socio-economic status. One-third of the study population had overweight. The largest population-based study reported that being overweight and obese significantly increased the likelihood of having lumbar disc herniation [10].
Medical comorbidities such as diabetes, hyperlipidemia, and smoking have also been reported as possible risk factors for lumbar disc herniations [11]. The majority of the study participants had no comorbidity, while 5 patients had diabetes mellitus and 4 patients had hypertension. The majority of the study participants had three discs involvement; the most affected disc was L4-L5, followed by L5-S1, which matched other studies. PLID occurs most commonly occurs at L4/5 and L5/S1 disc levels [7]. In 1st month, the reduction of VAS score was more in group B compared to group A. This might be due to the lower adherence of patients of group A to conservative treatment. Patients of group A might believe that they were treated with ESI, which might provide a better outcome than conservative treatment. So, they did not strictly follow physical therapy, exercise programs, lifestyle modifications, and behavioral therapy. On the other hand, patients in group B strictly adhered to the conservative treatment, which provided them with a better outcome in 1st month. In 3rd month, a significant reduction in VAS score was found in group A compared to group B. Inflammatory agents released by the herniation are a significant contributor to the pain and nerve root irritation. Corticosteroids have been shown to reduce inflammation by inhibiting either the synthesis or release of a number of pro-inflammatory mediators and by causing a reversible local anesthetic effect [12]. prospectively compared the effect of transforaminal ESI injection and conservative treatment among patients with PLID with radiculopathy and observed treatment improvement in both transforaminal ESI injection and conservative treatment group. But the improvement was significantly more in the TFESI group. Another Bangladeshi study compared the effects of epidural steroid injections with conservative management in patients with lumbar radiculopathy. They also found that pain reduction was significantly more in the epidural steroid injection group.
The comprehensive review of [13] reported that in a substantial proportion of patients with lumbar radicular pain caused by contained disc herniations, lumbar transforaminal injection of corticosteroids is effective in reducing pain, restoring function, reducing the need for other health care, and avoiding surgery, stated that caudal epidural injections of local anesthetic with or without steroids might be an effective therapy for patients with disc herniation or radiculitis. The systematic review demonstrated that trained physicians' epidural injections performed under fluoroscopy improve pain and function in well-selected patients with lumbar disc herniation. Determined the difference in short- and long-term pain improvement between lumbar Epidural Steroid Injections (ESIs) and conservative management in patients with lumbar radiculopathy and observed that ESI is considered to be a better option compared to conservative treatment.
Though there was no significant difference between the groups regarding ODI scores at baseline, significant improvement was observed in the ESI group compared to the conservative group from 1st week. This difference persisted throughout the follow-up period. The result was inconsistent with the study conducted among the Bangladeshi population. They also found that the functional improvement, assessed in ODI, was more compared to conservative treatment, which observed clinically meaningful and significant improvement in all parameters after caudal epidural injections in patients with disc herniation or radiculitis [14]. compared the effectiveness of caudal epidural injection versus non-steroidal anti-inflammatory drugs (NSAIDs) in the treatment of low back pain accompanied by radicular pain and reported that the caudal epidural injection group's improvement was better and faster than the NSAID groups, and the differences between assessment scores of the groups were statistically significant, except the 3rd month Oswestry scores.
However, the study found no significant difference in functional improvement between ESI and placebo groups. This might be the absence of fluoroscopic guided ESI administration in the patients in the study by Arden et al. [8]. The use of fluoroscopy offers several advantages, including verification of the correct level and side; confirmation, with use of contrast medium, that the injection is accurately placed in the epidural space; and avoidance of intravascular injection [15]. True complications following fluoroscopically guided ESI appear to be rare. In fact, a large cohort of over 1,500 consecutive injections revealed no major complications. No patient in the present study had post injection complications except headache, which subsided by oral paracetamol and adequate hydration.
5. Conclusion
C-arm guided transforaminal, and caudal Epidural Steroid Injection is effective in pain and functional outcome of patients with radiculopathy due to Prolapsed Lumbar Intervertebral Disc.
6. Recommendations
- C-arm guided transforaminal and caudal Epidural Steroid Injections would be an effective treatment for patients with radiculopathy due to PLID
- Long-term, large scale and multicenter research studies are needed to establish the outcome and effectiveness of this procedure
7. Limitations of the Study
Some limitations were perceived while planning and conducting the study. The following were the limitation of the study:
- Due to the COVID-19 pandemic, only 65 patients were included in the study, and 54 of them could complete the follow-up schedule, which might not represent the population
- Long-term follow-up could not be done
- The study place and population were selected purposively, which might result in selection bias
- The study was conducted in only one institution (BSMMU), so the results might not represent the entire population
Conflict of Interest:
None.
Acknowledgement:
We are grateful to the Department of Physical Medicine and Rehabilitation, BSMMU, in collaboration with the Department of Orthopaedic Surgery, BSMMU, and Dr. Sirajul Islam Medical College Hospital, Dhaka. Special thanks to my research assistant with staff, their unpaid support and cooperation at every step of this study.
References
- Schroeder GD, Guyre CA, Vaccaro AR. The epidemiology and pathophysiology of lumbar disc herniations. Semin Spine Surg 28 (2016): 2-7.
- Lurie JD, Tosteson TD, Tosteson ANA, et al. Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial. Spine 39 (2014): 3-16.
- Mukherjee U, Kundu S, Gulati R, et al. Lumbosacral Angle Variations in Middle Aged Patients with Chronic Low Back Pain - A Retrospective Study. J Evid Based Med Healthc 8 (2021): 208-212.
- Cummins J, Lurie JD, Tosteson TD, et al. Descriptive epidemiology and prior healthcare utilization of patients in the Spine Patient Outcomes Research Trial’s (SPORT) three observational cohorts: disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spin 31 (2006): 806-814.
- Hasan SA, Rahim MA, Siddiq MAB, et al. Study of Spectrum of Rheumatic Diseases in the Department of Physical Medicine & Rehabilitation, Chittagong Medical College Hospital, Bangladesh. J Chittagong Med Coll Teach Assoc 20 (2009): 6-11.
- Hoy D, Brooks P, Blyth F, et al. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol 24 (2010): 769-781.
- Warwick D. Apley and Solomon’s System of Orthopaedics and Trauma [Internet]. Routledge and CRC Press (2017).
- Arden NK, Price C, Reading I, et al. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: the WEST study. Rheumatol Oxf Engl 44 (2005): 1399-1406.
- Carette S, Leclaire R, Marcoux S, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med 336 (1997): 1634-1640.
- Samartzis D, Karppinen J, Luk KD, et al. Body Mass Index and its Association with Lumbar Disc Herniation and Sciatica: A Large-Scale, Population-Based Study. Glob Spine J 4 (2014): s-0034-1376593.
- Gadiya A. Lumbar Prolapsed Intervertebral Disc – A Treatment Algorithm [Internet]. Journal of Clinical Orthopaedics (2016).
- Manchikanti L, Singh V, Cash KA, et al. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: a randomized, controlled, double blind trial with a two-year follow-up. Pain Physician 15 (2012): 273-286.
- MacVicar J, King W, Landers MH, et al. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med Malden Mass 14 (2013): 14-28.
- Dincer U, Kiralp MZ, Cakar E, et al. Caudal epidural injection versus non-steroidal anti-inflammatory drugs in the treatment of low back pain accompanied with radicular pain. Joint Bone Spine 74 (2007): 467-471.
- Sharma AK, Vorobeychik Y, Wasserman R, et al. The Effectiveness and Risks of Fluoroscopically Guided Lumbar Interlaminar Epidural Steroid Injections: A Systematic Review with Comprehensive Analysis of the Published Data. Pain Med Malden Mass 18 (2017): 239-251.
