Neuroendocrine Small Cell Carcinoma of the Bladder: Rare and Aggressive Entity
Article Information
Rkik, M. Modeste, A. Ettanji, A. Kbiro, M. Dakir, R. Aboutaib, A. Debbaghi
Departement of Urology, CHU Ibn Rochd, Casablanca, Morocco
*Corresponding Author: Dr. Mustapha Rkik, Departement of Urology, CHU Ibn Rochd, Casablanca, Morocco
Received: 02 March 2020; Accepted: 18 March 2020; Published: 30 March 2020
Citation: M. Rkik, M. Modeste, A. Ettanji, A. Kbiro, M. Dakir, R. Aboutaib, A. Debbaghi. Neuroendocrine Small Cell Carcinoma of the Bladder: Rare and Aggressive Entity. Archives of Nephrology and Urology 3 (2020): 001-004.
Share at FacebookAbstract
Neuroendocrine small cell carcinoma of the bladder is a rare cancer, rapidly aggressive and metastatic with a very pejorative behavior. The diagnosis is based on histological analysis coupled with immunohistochemical study. Because it is rare, there is no consensus to date. Its management should be multidisciplinary, involving surgery, chemotherapy, and radiotherapy. We report two new cases of neuroendocrine small cell carcinoma of the bladder, one is pure and the other associated with urothelial carcinoma. The poor outcome illustrates the quick evolution of this tumor. A review of the literature on this topic is also presented.
Keywords
Neuroendocrine; Cell carcinoma; Bladder; Cancer
Neuroendocrine articles, Cell carcinoma articles, Bladder articles, Cancer articles
Neuroendocrine articles Neuroendocrine Research articles Neuroendocrine review articles Neuroendocrine PubMed articles Neuroendocrine PubMed Central articles Neuroendocrine 2023 articles Neuroendocrine 2024 articles Neuroendocrine Scopus articles Neuroendocrine impact factor journals Neuroendocrine Scopus journals Neuroendocrine PubMed journals Neuroendocrine medical journals Neuroendocrine free journals Neuroendocrine best journals Neuroendocrine top journals Neuroendocrine free medical journals Neuroendocrine famous journals Neuroendocrine Google Scholar indexed journals Cell carcinoma articles Cell carcinoma Research articles Cell carcinoma review articles Cell carcinoma PubMed articles Cell carcinoma PubMed Central articles Cell carcinoma 2023 articles Cell carcinoma 2024 articles Cell carcinoma Scopus articles Cell carcinoma impact factor journals Cell carcinoma Scopus journals Cell carcinoma PubMed journals Cell carcinoma medical journals Cell carcinoma free journals Cell carcinoma best journals Cell carcinoma top journals Cell carcinoma free medical journals Cell carcinoma famous journals Cell carcinoma Google Scholar indexed journals Bladder articles Bladder Research articles Bladder review articles Bladder PubMed articles Bladder PubMed Central articles Bladder 2023 articles Bladder 2024 articles Bladder Scopus articles Bladder impact factor journals Bladder Scopus journals Bladder PubMed journals Bladder medical journals Bladder free journals Bladder best journals Bladder top journals Bladder free medical journals Bladder famous journals Bladder Google Scholar indexed journals Cancer articles Cancer Research articles Cancer review articles Cancer PubMed articles Cancer PubMed Central articles Cancer 2023 articles Cancer 2024 articles Cancer Scopus articles Cancer impact factor journals Cancer Scopus journals Cancer PubMed journals Cancer medical journals Cancer free journals Cancer best journals Cancer top journals Cancer free medical journals Cancer famous journals Cancer Google Scholar indexed journals small cell carcinoma of the bladder articles small cell carcinoma of the bladder Research articles small cell carcinoma of the bladder review articles small cell carcinoma of the bladder PubMed articles small cell carcinoma of the bladder PubMed Central articles small cell carcinoma of the bladder 2023 articles small cell carcinoma of the bladder 2024 articles small cell carcinoma of the bladder Scopus articles small cell carcinoma of the bladder impact factor journals small cell carcinoma of the bladder Scopus journals small cell carcinoma of the bladder PubMed journals small cell carcinoma of the bladder medical journals small cell carcinoma of the bladder free journals small cell carcinoma of the bladder best journals small cell carcinoma of the bladder top journals small cell carcinoma of the bladder free medical journals small cell carcinoma of the bladder famous journals small cell carcinoma of the bladder Google Scholar indexed journals Cystoscopy articles Cystoscopy Research articles Cystoscopy review articles Cystoscopy PubMed articles Cystoscopy PubMed Central articles Cystoscopy 2023 articles Cystoscopy 2024 articles Cystoscopy Scopus articles Cystoscopy impact factor journals Cystoscopy Scopus journals Cystoscopy PubMed journals Cystoscopy medical journals Cystoscopy free journals Cystoscopy best journals Cystoscopy top journals Cystoscopy free medical journals Cystoscopy famous journals Cystoscopy Google Scholar indexed journals hypercalcemia articles hypercalcemia Research articles hypercalcemia review articles hypercalcemia PubMed articles hypercalcemia PubMed Central articles hypercalcemia 2023 articles hypercalcemia 2024 articles hypercalcemia Scopus articles hypercalcemia impact factor journals hypercalcemia Scopus journals hypercalcemia PubMed journals hypercalcemia medical journals hypercalcemia free journals hypercalcemia best journals hypercalcemia top journals hypercalcemia free medical journals hypercalcemia famous journals hypercalcemia Google Scholar indexed journals chemotherapy articles chemotherapy Research articles chemotherapy review articles chemotherapy PubMed articles chemotherapy PubMed Central articles chemotherapy 2023 articles chemotherapy 2024 articles chemotherapy Scopus articles chemotherapy impact factor journals chemotherapy Scopus journals chemotherapy PubMed journals chemotherapy medical journals chemotherapy free journals chemotherapy best journals chemotherapy top journals chemotherapy free medical journals chemotherapy famous journals chemotherapy Google Scholar indexed journals
Article Details
1. Introduction
Neuroendocrine small cell carcinoma of the bladder (SCCB) is a rare tumor and of very bad evolution. It has morphological and immunohistochemical characteristics common to neuroendocrine tumors found in other organs [1]. It is a particular histological entity characterized by a very early metastatic potential and a very severe prognosis [2]. Bladder localization is little known and its frequency is low (0.5% of bladder tumors) but certainly underestimated [3]. Its management must be multidisciplinary, combining surgery, chemotherapy and radiotherapy [2]. The authors report two new observations of small cell carcinoma of the bladder. This series, although short, can be considered important given the rarity of this entity.
2. Case 1
60 year old patient was referred for management of high hematuria. The abdominopelvic CT scan showed the presence of a tumor of the right posterolateral bladder wall associated with numerous deep lymphadenopathies and multiple secondary hepatic foci (Figure 1). Histological analysis of the samples taken during a cystoscopy revealed a tumor proliferation largely dissociating the bladder muscle, made of two contingents, intimately mixed, one high-grade infiltrating urothelial, the other small cell neuroendocrine made of layers and spans of small cells, fairly monomorphic with a salt and pepper aspect chromatin. The mitotic index is very high. The immunohistochemical study confirmed the neuroendocrine nature of the small cell component by their positivity to chromogranin and synaptophysin. The patient received two courses of chemotherapy using cisplatin four weeks apart. He died after six months' follow-up.
3. Case 2
49-year-old patient admitted for total hematuria associated with right lumbar pain. Radiology showed a tumor of the right lateral bladder wall and a homolateral ureterohydronephrosis requiring an emergency percutaneous nephrostomy. Cystoscopy showed the presence of a sessile formation of the right retrotrigonal lateral face. A deep resection was performed. Anatomopathological examination of the resection chips showed on certain fragments the existence of a dense tumor proliferation, largely necrotic and very infiltrating, largely dissociating the bladder muscle. It is made of cords, sheets and cell spans that are fairly homogeneous with small nuclei, hyperchromatic with strong mitotic activity (Figure 2). The immunostaining was positive for NSE and synaptophysin. He was chromogranin and PSA negative. The diagnosis of SCCB was retained. The patient underwent a cystoprostatectomy with left nephro-ureterectomy. Fifteen months after the intervention, the control CT scan revealed a local recurrence with bone metastasis in the left iliac bone. The patient received external radiation therapy (45 Gy) which improved the pain symptomatology. He died four months later (19 months after the procedure).
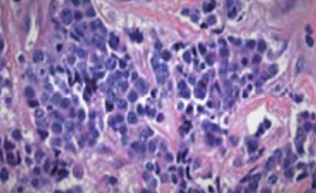
Figure 1: High-magnification microphotograph showing dense tumor proliferation, largely necrotic made up of small nucleus, hyperchromatic cells with high mitotic activity (HE, G 40).
4. Discussion
Neuroendocrine small cell carcinoma of the bladder was first described in 1981 by Cramer et al. [4]. It represents 0.5 to 1% of all bladder tumors and occurs in the elderly, between the fifth and ninth decades. The sex ratio is 3.6 men / 1 woman. Smoking was reported in 67% of the cases [2]. Its clinical symptomatology is not very specific. Hematuria is the most frequent telltale sign, present in 88% of the observations [5]. This symptom was reported in our two patients. Exceptionally, a paraneoplastic syndrome (Cushing's syndrome, hypercalcemia) is noted [6]. Endoscopic data usually show polyploid lesions of 4 to 10 cm, frequently ulcerated and necrotic [7]. These lesions are found on the lateral walls in 54% of cases [2].
The diagnosis is based on histological examination coupled with the immunohistochemical study. The anatomopathological analysis finds an undifferentiated tumor proliferation of small basophil cells organizing themselves in cords, in spans or realizing aspects of pseudorosettes. Tumor infiltration is often significant with damage to the muscle or perivesical adipose tissue [7]. In more than 50% of cases, it is associated with another tumor component such as urothelial carcinoma, more rarely adenocarcinoma or squamous cell carcinoma [8]. The diagnosis is confirmed by the immunohistochemical study, which reveals the expression of at least one neuroendocrine marker (synaptophysin, chromogranin A, specific neuron enolase) and the absence of expression of the common leukocyte antigen, thus eliminating lymphoma and anti-PSA antibody, eliminating metastasis from a prostate carcinoma. The search for a composite character is a decisive factor in eliminating a metastasis of the bladder from a small cell carcinoma of another origin, in particular pulmonary [9].
These tumors are aggressive, often discovered at an advanced stage even in the case of small lesions [3]. Metastases are present in 28 to 50% of cases at the time of diagnosis and occur in the lymph nodes, liver, bones, lungs and brain [10], requiring a complete extension assessment. The stage of the disease is defined by the TNM classification of the American Joint Committee on Cancer (AJCC) of 2002 [11]. By analogy to small cell carcinoma of the lung, some authors recommend to distinguish localized tumors and disseminated tumors, and not to use the TNM classification, which would seem not to be appropriate for this type of tumor [12]. The therapeutic modalities are not precisely defined due to the rarity of these tumors and only small series have been published [2]. In the absence of prospective trials, there is currently no therapeutic consensus and the results of the different therapies used vary widely from one study to another. From the literature, it appears that the treatment of choice for bladder SCCB is surgical excision combined with cisplatin-based chemotherapy. Despite therapeutic advances, the prognosis of SCCB remains extremely poor [13]. The overall five-year survival rate for all stages combined is 19% (16 to 25%) [10].
5. Conclusion
Bladder SCC usually presents at a later stage than urothelial carcinoma and therefore confers a worse prognosis. Multiple treatment algorithms have been used to treat local and metastatic disease, including cystectomy, partial cystectomy, radiation therapy, and neoadjuvant/adjuvant chemotherapy as well as chemotherapy alone. Low disease incidence makes it difficult to exclusively advocate for one treatment algorithm. Prospective studies need to be done to elucidate the most effective treatment by stage for bladder SCC.
References
- Navarra S, Pfister C, Gobet F, et al. Tumeur neuroendocrine maligne de vessie : une entité à ne pas méconnaître. Progr Urol 9 (1999): 129-132.
- Chekrine T, De Baria B, Cassierc P, et al. Carcinome neuroendocrine à petites cellules de la vessie : à propos d’une observation et revue de littérature. Cancer Radiother 15 (2011): 250-253.
- Henno S, Guiraud P, Rioux-Leclercq N, et al. Une tumeur vésicale rare : le carcinome à petites cellules. Bull Cancer 87 (2000): 307-310.
- Cramer SF, Aikawa M, Cebelin M. Neurosecretory granules in small cell invasive carcinoma of the urinary bladder. Cancer 47 (1981): 724-730.
- Grignon DJ, Ro JY, Ayala GA, et al. Small cell carcinoma of the urinary bladder: a clinico-pathologic analysis of 22 cases. Cancer 69 (1992): 527-536.
- Abrahams NA, Moran C, Reyes AO, et al. Small cell carcinoma of the bladder: a contemporary clinicopathological study of 51 cases. Histopathology 46 (2005): 57-63.
- Sved P, Gomez P, Manoharan M, et al. Small cell carcinoma of the bladder. BJU Int 94 (2004): 12-17.
- Ismaili N, Elkarak F, Heudel PE, et al. Small cell cancer of the bladder: the Leon-Berard cancer centre experience. Indian J Urol 24 (2008): 494-497.
- Châari C, Krichen-Makni S, Toumi SN, et al. Les carcinomes endocrines à petites cellules de la vessie : à propos d’une observation. Oncologie 11 (2009): 53-57.
- Choong NWW, Fernando Quevedo J, et al. Small cell carcinoma of the urinary bladder. Cancer 103 (2005): 1172-1178.
- Greene FPLD, Fleming ID, Fritz AG, et al. AJCC cancer staging manual. 6th ed. Springer, New York (2002).
- Bex A, de Vries R, Pos F, et al. Long-term survival after sequential chemoradiation for limited disease small cell carcinoma of the bladder. World J Urol 27 (2009): 101-106.
- Karmouni T, Rioux-Leclercq N, Bensalah K, et al. Carcinomes neuroendocrines primitifs de vessie : diagnostic et traitement. Prog Urol 10 (2000): 590-594.
