Nest of Evil
Article Information
Maryam Nasera, Parizad Hooshib, Danielle Westfallc, Wayne Schultheisc, Nafiseh Hashemia*
aHashemi Eye Care, Encino, CA, USA
bNorthridge Specialty Imaging Center, Northridge, CA, USA
cPathology Department, Los Robles Hospital,Thousand Oaks, CA, USA
*Corresponding Author: Nafiseh Hashemi, MD, Hashemi Eye Care, 5353 Balboa Blvd #110, Encino, CA, 91316, USA
Received: 29 July 2020; Accepted: 04 August 2020; Published: 07 August 2020
Citation: Maryam Naser, Parizad Hooshi, Danielle Westfall, Wayne Schultheis, Nafiseh Hashemi. Nest of Evil. Journal of Ophthalmology and Research 3 (2020): 41-44.
Share at FacebookAbstract
Abstract
An 83 year-old patient was referred to the neuro-ophthalmology service with symptoms of headaches and vision loss. She had been diagnosed with stable size meningioma one year prior to presentation. She had a history of breast cancer treated by lumpectomy and radiation 20 years ago. MRI of the orbit showed encasement of the optic nerve on the right orbital apex. Craniotomy was performed and the specimen was diagnosed as a meningioma. After resection, the tumor grew rapidly. When it was resected for the second time, the diagnosis was metastatic breast adenocarcinoma.
Keywords
Tumor to tumor metastasis; Meningioma; Breast cancer; Visual loss; Third nerve palsy; Sellar tumor
Article Details
Case Report
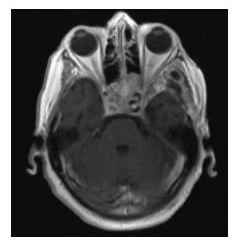
An 83 year-old Caucasian female was referred to the neuro-ophthalmology clinic with concern of GCA. The patient had a meningioma that had remained stable in size on brain MRI over the past year, therefore the new onset of symptoms of headaches and vision loss in an 83 year-old were assumed to be related to GCA. Temporal artery biopsy was done and her headaches improved slightly with steroids. Since the clinical and laboratory criteria were not completely consistent with GCA, MRI of the orbit was requested which showed encasement of the optic nerve by meningioma on the right orbital apex. Craniotomy was performed. The specimen diagnosed as meningioma. She came back to the clinic three months later with complete ptosis, vision loss on the left eye, inability in adduction, elevation and depression, dilated pupil on the left eye, VA 20/250 OD, LP OS. RAPD OS. Both optic nerves seemed swollen. MRI brain and orbit was done and reported recurrence of tumor (Figure 1).
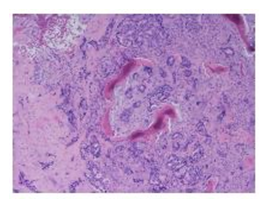
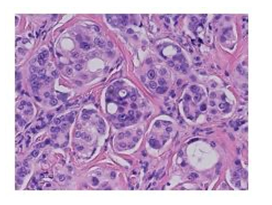
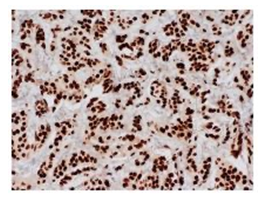
The tumor was re-excised and the diagnosis was metastatic breast adenocarcinoma. The resection specimen shows fibrous tissue and infiltration of tuberculum sellar region by a poorly differentiated carcinoma. On hematoxylin & eosin stained slides, the neoplastic cells are arranged as poorly formed glands, cribriform glands and nests of cells with a desmoplastic stromal response (Figure 2). The neoplastic cells are characterized by medium to large-sized nuclei with prominent nucleoli and moderate eosinophilic cytoplasm (Figure 3). There is moderate to severe nuclear pleomorphism. Poorly formed lumens may be seen in some areas. Larger cribriform glands show necrosis. The tumor cells are positive for pankeratin (AE1/AE3), CK7 and GATA3 immunohistochemical stains (Figure 4). Tumor cells are negative for CK20, CDX2, Pax8 and TTF1 immunohistochemical stains. The Ki-67 immunohistochemical stain shows a high proliferative index at 40%. Tumor cells are negative for ER and PR by immunohistochemistry; Her2 testing is equivocal by immunohistochemistry (2+ staining) and negative by Fluorescence In Situ Hybridization (FISH) with a Her-2 signal copy number of 4.2 signals/nu- cleus and a Her2:CEN 17 ratio of 1.9. Given immunohistochemical positivity for GATA3, this is most consistent with metastasis from a breast primary.
The patient had breast cancer treated by lumpectomy and radiation 20 years ago. Oncology work up did not reveal any tumor in the breast. The patient deferred the proposed chemotherapy and radiation. She passed away 3 months later in a rehabilitation facility.
Established Facts and Novel Insights
Tumor to tumor metastasis from breast cancer to meningioma has been described in the literature before. In our case, the patient has a remote history of breast cancer treated with lumpectomy and radiation 20 years ago. Poorly differentiated adenocarcinoma was found only in the bed of prior meningioma resection with no evidence of tumor elsewhere.
Discussion
Tumor-to-tumor metastasis is an uncommon phenomenon. Imaging, selecting best tissue for biopsy and pathology information are important for final diagnosis and appropriate patient management [1]. Meningioma is known as the most common intracranial tumor to host metastases based on having low metabolic activity, high vascularity and being slow growing. The most commonly reported tumor to tumor intracranial metastases are from primary breast and lung neoplasms although, there are few reported cases of metastasis from renal, prostate, hematopoietic, gastrointestinal primaries [2,3,4]. Our case showed that a stable benign meningioma may change behavior due to metastasis from distant tumor. Remote treated cancer, may still have distant seeding, which may grow years later despite of the absence of the original tumor.
Disclosure Statement
The authors do not have any financial disclosures.
Funding Sources:
None
References
- Syed S, Karambizi DI, Baker A, et al. A comparative report on intracranial tumor-to-tumor metastasis and collision tumors. World Neurosurgery 116 (2018): 454-463.
- Pham JT, Kim RC, Nguyen A, et al. Intracranial meningioma with carcinoma tumor-to-tumor metastasis: two case reports. CNS Oncology 7 (2018): CNS09.
- Dietterle J, Frydrychowicz C, Müller W, et al. Tumor-to-Tumor Metastasis of Multiple Meningiomas and Clear Cell Renal Cell Carcinoma Metastasis as First Clinical Appearance of Kidney Cancer: A Case Report and Analysis. Journal of Neurological Surgery Reports 81 (2020): e10.
- Farrag A, Ansari J, Ali M, et al. Intracranial meningioma as primary presentation for an undiagnosed collision metastatic breast cancer: Case report and literature review. Molecular and Clinical Oncology 8 (2018): 661-664.