Musculoskeletal Disorders among the Mothers having Children with Cerebral Palsy
Article Information
Zannatul Mawa1, Mohima Benojir2, Ruksana Akter3, Shameem Ahammad4, Faruq Ahmed5, Mohammad Nazmul Hasan6, Nadia Afrin Urme7*, Shahid Afridi8
1Junior Consultant Physiotherapist, Incharge of paediatric PT services, Centre for the Rehabilitation of the Paralyzed (CRP), Dhaka- 1343 Bangladesh; ORCID: 0000-0002-0919-1021
2M. Phil Public Health Lecturer & Course Coordinator, Department of Public Health, ASA University Bangladesh
3Assistant Professor, Department of Physiotherapy , Mymensingh College of Physiotherapy & Health Sciences
4Assistant Professor, Department of Occupational Therapy, Mymensingh College of Physiotherapy & Health Sciences
5Senior Clinical Physiotherapist, William & Marie Taylor School, Centre for the Rehabilitation of the Paralysed (CRP), Savar, Dhaka-1343, Bangladesh
6Junior Consultant Physiotherapist, Centre for the Rehabilitation of the Paralyzed (CRP), Dhaka- 1343 Bangladesh
7Lecturer, Bangladesh Health Professions Institute, CRP, Bangladesh
8Intern Physiotherapist, Centre for the Rehabilitation of the Paralyzed (CRP), Bangladesh; ORCID: 0000-0002-9558-5640
*Corresponding Author: Nadia Afrin Urme, Lecturer, Bangladesh Health Professions Institute, CRP, Bangladesh.
Received: 10 May 2023; Accepted: 28 August 2023; Published: 07 September 2023
Citation: Zannatul Mawa, Mohima Benojir, Ruksana Akter, Shameem Ahammad, Faruq Ahmed, Mohammad Nazmul Hasan, Nadia Afrin Urme, Shahid Afridi. Musculoskeletal Disorders among the Mothers having Children with Cerebral Palsy. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 173-183.
Share at FacebookAbstract
Background: Cerebral Palsy (CP) is a collection of mobility and postural problems. Parents, particularly mothers, care for CP children. Caring for a kid with CP can be physically taxing and cause moms to acquire musculoskeletal ailments. CP moms have a greater risk of musculoskeletal issues than mothers of generally developing children. There is little study on musculoskeletal issues in Bangladeshi moms of CP children. This study examined the frequency and symptoms of musculoskeletal diseases in Bangladeshi moms of CP children.
Purpose: To assess musculoskeletal disorders among mothers having a child with Cerebral Palsy. Methods: A cross-sectional study was conducted at Centre for the Rehabilitation of the Paralysed (CRP) and a purposive sampling technique was used to select the sample. Data were collected from pediatrics unit of Savar and Mirpur under the Centre for the Rehabilitation of the Paralysed, Bangladesh. A total of 200 mothers recruited for this study followed by eligibility criteria. Primary outcome measurement common musculoskeletal symptoms among the mother of CP child which was measured by pain measures and Scandinavian Musculoskeletal System Questionnaire. Secondary outcome measurement includes socio-demographic characteristics, pain related information, common treatment taken by participants for musculoskeletal pain relief.
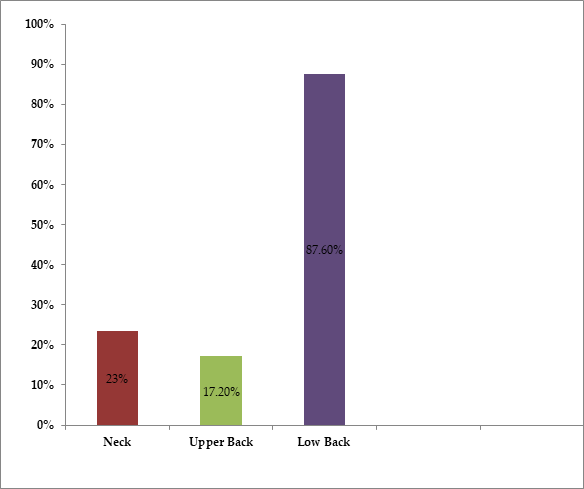
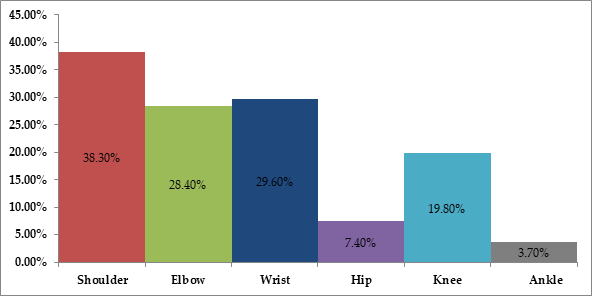
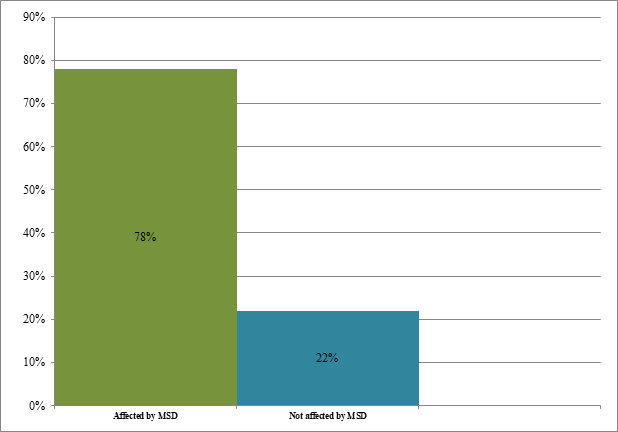
Results: Analysis demonstrated that prevalence of musculoskeletal problems among mothers of Cerebral palsy children was (78%). Common symptoms were lower back pain at 87.60% (n=127) followed by shoulder pain at 38.30% (n=31) and wrist pain at 29.60% (n=24). Among 200 mothers of CP children most (82.0%) participants complain that their symptoms were mostly worse during lifting and carrying 54.50% (n=109), transferring 33.30% (n=67), also some other factors are involved. Participants of the study were most commonly taking medications (89.70%) for symptom relief, some others take physiotherapy (16.10%), apply heat (13.80%), and homeopathy (1.10%).
Conclusion: In this study most of the mothers having children with cerebral palsy complain of musculoskeletal disorders. The child's age, and the caregiver’s work are influential factors in these disorders.
Keywords
Musculoskeletal disorders; Mothers; Children with Cerebral palsy
Musculoskeletal disorders articles; Mothers articles; Children with Cerebral palsy articles
Article Details
Key message:
Researchers in Bangladesh revealed that nearly eighty percent of moms caring for children with cerebral palsy had themselves had musculoskeletal difficulties. Eighty-eight percent of respondents reported experiencing lower back discomfort, making it the most often reported complaint. The most prevalent causes of worsened symptoms were found to be related to lifting and carrying. The majority of people who sought help for their discomfort turned to pharmaceuticals. It was discovered that the child's age and the caregiver's occupation play a role in the development of these illnesses.
1. Introduction
According to the World Health Organization, work-related musculoskeletal problems affect at least 100,000 women each year [1]. Mothers of a cerebral palsy child often put their children in and out of car seats, move from room to room, walk outside, and use high chairs [2-4]. Some persons suffer from musculoskeletal problems of the lower back, neck, shoulders, wrists, and knees [5]. Because the mother is regularly carrying and lifting the children for daily activities. Physical limitations are widespread in nations of the mother where socioeconomic progress is uneven [6]. For chronic musculoskeletal pain, 39 percent of men and 45 percent of women had chronic problems, with the hip and wrist/hand having the largest female preponderance, while the lower back and knee had the lowest and statistically insignificant sex differences [2]. Although in a family father is playing a role as an earner and all responsibilities of caring for children are on the primary caregiver. In Bangladesh, Jordanian, and Indian families’ mothers take the role of primary caregiver for caring for their children [7]. According to one study, mothers of children with cerebral palsy are more probable to experience musculoskeletal pain, especially low back pain 44.7% [8]. Another study represents that musculoskeletal related pain is more prevalent in mothers when lifting and carrying their disabled children and their involvement percentage of neck and shoulder pain at 72.5%, back pain at 84.1%, leg pain at 46.4%, elbow pain at 47.8% and wrist pain at 68.1% [6,9]. Musculoskeletal disorders commonly affect the human support systems such as muscle, tendon, nerves, blood vessels, bones, and joints. Musculoskeletal disorders can occur from a single event or repeated trauma [3]. The most commonly reported musculoskeletal disorders (MSDs) and stress, that results from a sudden exertion (e.g., lifting a heavy object), repetitive strain, or repeated exposure to force vibration, or awkward posture, and can affect many different parts of the body including the upper and lower back, neck, shoulders, and legs [4].
In Bangladesh, more than half of woman carer (58.7%) spent fewer than 6 hours per day on their child (CP) care responsibilities. The frequency of LBP in the last 12 months was 66.70% among female caregivers [10,11] but there have been no studies to identify the prevalence of common musculoskeletal pain disorder among the mother of cerebral palsy children though cerebral palsy is not an uncommon condition in Bangladesh. Hence, this study is focused on exploring common musculoskeletal complaints among mothers having cerebral palsy children and establishing proper ergonomic guidelines for mothers.
Objectives
- To find out the common musculoskeletal disorders prevalence among the mothers having children with cerebral palsy.
- To know about which posture could aggravate the symptom.
- To get idea about commonly received treatment to relief their symptoms.
2. Methods
The researcher chose a quantitative research approach in the form of a cross-sectional type of survey in this study since it is the best way to estimate prevalence. The study followed the guideline for strengthening the Reporting of Observational studies in Epidemiology (STROBE) [Annexure 1]. The research was conducted at the Centre for the Rehabilitation of the Paralyzed (CRP), a nonprofit organization formed in 1979 that focuses on rehabilitation and community integration for people with disabilities [12]. The population of this study was the mothers having children with cerebral palsy admitted to both outpatient and inpatient Pediatric units, Centre for the Rehabilitation of the Paralysed (CRP) Savar and Mirpur branch, Bangladesh and the study was carried out from January to April 2022. In this study, the subject inclusion criteria were: (1) only mothers who are housewives and aged less than 40 years have cerebral palsy children, (2) Subject who wants to willingly participate in the study and carry the child for at least one year. The exclusion criteria were: (1) Any history of known active infection, such as TB spine, or any history of acute trauma to the back, which might cause pain as an immediate inflammatory reaction, (2) Mothers with CP children under the age of two were not allowed to participate since they needed to be carried, (3) Mother looking after more than one disabled child, and (4) Back surgery or fracture history.
2.1 Sampling procedure and data collection technique
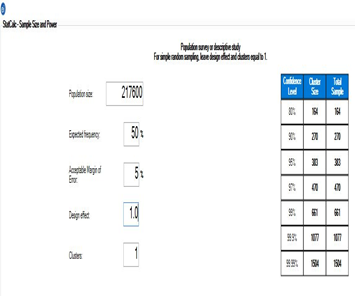
We have conducted sample size calculation via Epi Info V 7.7.5.0 (Figure 1). From study, we found the Observed prevalence of Cerebral Palsy was 3.4 per 1000 children [13]. Bangladesh has 64,000,000 children according to UNICEF [14]. From the calculations (Figure 1) among the calculated 217,600 CP populations, 164 samples can reach 50% expected frequency, 5% acceptable margin of error, 80% Confidence interval, and 1.0 design effect. For this a total number of 200 participants were chosen by the Purposive sampling technique. Before starting written informed consent with study details was provided to the participants. Primary outcome measurement was common musculoskeletal symptoms among the mother of CP child which was measured by Scandinavian Musculoskeletal System Questionnaire (The Nordic Musculoskeletal System Questionnaire).The participants were questioned if the pain that had grown during the previous year prohibited them from carrying out regular tasks (at home or away from home) or if hospitalization was necessary as a result of this discomfort (The individuals were considered to have musculoskeletal pain if they answered "Yes" to the first two questions [15]. Secondary outcome measurement was included socio-demographic characteristics, pain-related information, and common treatment taken by participants for musculoskeletal symptom relief.
2.2 Statistical analysis
Data were analyzed by using the software SPSS v.20. The descriptive analysis of sociodemographic variables was analyzed by frequency and percentage for categorical data, and mean and standard deviation for continuous variables (Table 1). Furthermore, the distribution of respondents according to mother’s age, severity of pain, child’s age, GMFCS level, referral source and musculoskeletal disorder experience has been presented by frequency and percentage (Table 2-5). There was no missing data.
|
Variables |
Involvement Number (n) |
% |
|
Living area |
102 |
51 |
|
Urban Semi |
23 |
11.5 |
|
Urban Slum |
75 |
37.5 |
|
Total (N) |
200 |
100 |
|
Mother age (In years) |
||
|
Mean ± SD |
200 |
27.7 ± 4.8 |
|
Height (in cm) |
||
|
Mean ± SD |
200 |
152.6 ± 7.7 |
|
Weight (kg) |
||
|
Mean ± SD |
200 |
57.0 ± 8.4 |
|
Educational level |
||
|
Illiterate |
8 |
4 |
|
Primary |
33 |
16.5 |
|
Secondary |
64 |
32 |
|
Higher secondary |
44 |
22 |
|
Graduate |
28 |
14 |
|
Post graduate |
23 |
11.5 |
|
Income (Taka) |
||
|
Mean ± SD |
200 |
27,945 ± 22,882 |
|
Number of children |
||
|
1 |
88 |
44 |
|
2 |
78 |
39 |
|
3 |
31 |
15.5 |
|
4 |
3 |
1.5 |
|
GMFCS level of the CP child |
||
|
Grade-II |
56 |
28 |
|
Grade-III |
52 |
26 |
|
Grade-IV |
49 |
24.5 |
|
Grade-V |
43 |
21.5 |
|
Age of CP child (in month) |
||
|
Mean ± SD |
200 |
48.2 ± 27.9 |
|
Height of CP child (cm) |
||
|
Mean ± SD |
200 |
36.9 ± 7.4 |
|
Weight of CP child (kg) |
||
|
Mean ± SD |
200 |
14.2 ± 5.5 |
Table 1: Distribution of the respondents by Socio-demographic characteristics.
2.3 Ethical considerations
The study undertook ethical approval from Centre for the Rehabilitation of the Paralyzed Ethics Committee (Ref no: CRP-R&E-0401). Before the respondents' data was collected, they gave their informed consent and confidentiality as well as privacy was maintained throughout the study. Data has been collected according to Helsinki guidelines. Anytime participants wanted to refuse and withdraw from the study was accepted.
3. Results
3.1 Socio-demographic information of the participants
Among 200 participants, 54.5% (n=109) were from Urban area, and the mean age of respondents was 27.7 ± 4.8 years and mean weight was 57.0 ± 8.4. Majority of the respondent’s complete secondary level of education (32%). The average income of the family member means was 27945 ± 22882 Bangladeshi taka. Most of the child 28.0 % (n=56), had GMFCS level Grade-II Grade-III 26.0% (n=52), Grade-IV 24.5% (n=49), Grade-V 21.5 (n=43). The mean age of the children with cerebral palsy was 48.2 ± 27.9 months, the mean height was 36.9 ± 7.4 and the mean weight was 14.2 ± 5.5. These Socio-demographic characteristics of the respondents showed in Table 1.
The distribution of the respondents by mother’s age and MSD has been presented in Table 2. Table 3 shows that among 200 participants, the child (CP) age group from 6-12 years, 90.3% of mother developed MSD, 83.9% was from 4-6 years, 77.8% was 2-4 years, and lastly, 60.0% was 0-2 years. Table 4 displayed the distribution of the respondents by their severity of pain and GMFCS level of the cerebral palsy child. Table 5 presented that only 10% of participants have taken treatment for musculoskeletal disorders and from that maximum participants' response they have taken treatment referred by GP.
|
Mothers age |
MSD |
Not Affected MSD |
Total |
|||
|
Frequency |
Percentage |
Frequency |
Percentage |
Frequency |
Percentage |
|
|
18-25 years |
35 |
0.686 |
16 |
0.314 |
51 |
1 |
|
25-30 years |
53 |
0.815 |
12 |
0.185 |
65 |
1 |
|
30-34 Years |
68 |
0.82 |
16 |
0.19 |
84 |
1 |
|
Total |
156 |
0.78 |
44 |
0.22 |
200 |
1 |
Table 2: Distribution of the respondents by mother’s age and MSD.
|
CP Child age |
MSD |
Not Affected MSD |
Total |
|||
|
Frequency |
Percentage |
Frequency |
Percentage |
Frequency |
Percentage |
|
|
0-2 years |
18 |
0.6 |
12 |
0.4 |
30 |
1 |
|
2-4 years |
84 |
0.778 |
24 |
0.222 |
108 |
1 |
|
4-6years |
26 |
0.839 |
5 |
0.161 |
31 |
1 |
|
6-12years |
28 |
0.903 |
3 |
0.097 |
31 |
1 |
|
Total |
156 |
0.78 |
44 |
0.22 |
200 |
1 |
Table 3: Distribution of the respondents by child (CP) age and mother MSD.
|
What is the severity of your pain |
GMFCS level of CP child |
Total |
||||
|
Grade-II |
Grade-III |
Grade-IV |
Grade-V |
Frequency |
Percentage |
|
|
Maximum |
4 |
7 |
7 |
4 |
22 |
0.11 |
|
Moderate |
31 |
29 |
33 |
22 |
115 |
0.575 |
|
Minimum |
3 |
7 |
4 |
5 |
19 |
0.095 |
|
Total |
38 |
43 |
44 |
31 |
156 |
0.78 |
Table 4: Distribution of the respondents by their severity of pain and GMFCS level of cerebral palsy child.
|
Variables |
Involvement Number |
% |
|
Physiotherapy treatment seek for musculoskeletal disorders |
||
|
Yes |
20 |
10 |
|
No |
180 |
90 |
|
Sources of information about physiotherapy treatment |
||
|
Referred by GP |
10 |
50 |
|
Mass media |
0 |
0 |
|
Relatives |
4 |
20 |
|
Self |
4 |
20 |
|
Ex-patient |
1 |
5 |
|
Sources of information about physiotherapy treatment |
||
|
Child neurologist |
70 |
35 |
|
Mass media |
7 |
3.5 |
|
Relatives |
50 |
25 |
|
Self |
13 |
26 |
|
Ex-patient |
50 |
25 |
|
Others |
10 |
5 |
|
*GMFCS= Gross Motor Functional Classification Scale, MSD= Musculoskeletal Disorders |
||
Table 5: Distribution of the respondents by source of referral.
Figure 2 presented, 200 participants out of 156 participants, who have suffered from musculoskeletal disorders 78% and among them 23% (n=34) Neck pain, 17.20% (n=25) Upper back pain and 87.60% (n=127). Low back pain showed 30% (n=31) Shoulder pain, 28.40% (n=23) Elbow pain, 29.60% (n=24) wrist pain, 7.40% (n=6) Hip pain, 19.80% (n=16) Knee pain and 3.70% (n=3) Ankle pain in Figure 3. Study also shows that most of the participants feel more pain during lifting and carrying a cerebral palsy child without maintaining appropriate posture and not considering children age 78% (Figure 4).
4. Discussion
The musculoskeletal disorders of mothers of children with cerebral palsy were investigated in this study. Most MSDs developed by mothers their child (CP) age group was 6-12 years than 4-6 years and 2-4 years and the least MSDs developed age group was 0-2 years. In the same way, one study found that there were higher levels of back pain among childcare workers caring for children aged between 4 and 6 years than those aged 3 or 4 years [16]. Similarly, another study found that parents of children aged 4 - 7 years had higher levels of musculoskeletal pain than those of children aged 2-4 years [17].
This study found that more than three fourth 78% suffered from musculoskeletal disorders. A similar study was Turkey in 2016, which found that the age of the mothers who were having children with cerebral palsy 34.77 ± 4.8 years, were significantly experienced musculoskeletal disorders [8]. This study revealed that the affected spine was mostly in the lower back than the neck and upper back. Study also found that Mother who have children with cerebral palsy said that they cannot maintain proper posture when lifting and carrying their cerebral palsy child and also impossible for them to consider the child's age. 69% of mothers reported that they have no assistance to help during child care tasks or treatment and help with lifting and carrying and also transferring time. The findings are similar to those of a study conducted in the United States, which found that the prevalence of LBP was 80.3 percent when the kid required physical aid with transfers, compared to 40.5 percent when the child did not require physical assistance with transfers [18]. Another study published in 2016 found that moms of children with cerebral palsy had considerably more low back pain in the previous year than mothers of healthy children in the control group [8]. The findings reveal a high frequency of LBP among the subjects, necessitating ergonomic considerations. This could be because they were frequently exposed to physical load for a long time when moving their child [19].
The study result showed that the shoulder, wrist and elbow joint is also vulnerable for pain, which showed the similar result like one study in Iran, with shoulder pain at 72.5%, wrist pain at 68.1%, and elbow pain at 47.8% [6]. Contributing factors of musculoskeletal disorders most of the participants complain of their symptoms worse forward bending during lifting and carrying their child and that was 54.50% and also aggravated their symptoms while transferring child and that was 33.30%. One study showed that pain intensity, duration, and musculoskeletal symptoms were significantly higher in mothers of non-ambulatory disabled children (p < 0.05) [16]. Another study found that risk factors for MSDs are present when moms lift cerebral palsy children at home [5]. In this study, 43.5% received treatment for musculoskeletal disorders, but only 16.10% had any physiotherapy for their musculoskeletal difficulties, implying that there is only a rudimentary understanding of physiotherapy treatment among them.
Despite the researcher's best efforts, the current study was not entirely devoid of limitations and obstructions. The study setting was insufficient to generalize the study's findings. Because this study was conducted over a short period, all factors relating to musculoskeletal problems in mothers may not have been highlighted, and there were only a few relevant studies conducted in Bangladesh. As a result, broad support for all factors proved challenging. All individuals did not have access to laboratory diagnoses (X-ray, MRI, uric Acid, and relevant tests) to diagnose musculoskeletal problems and to exclude other diagnoses. This could be a study's limitation. There has no specific valid scale to measure muscle strength in the spine and limb, as well as time and resources, were limited. Further study can be done with more samples to investigate the factors responsible for such musculoskeletal complaints or related risk factors and quality of life of mothers with cerebral palsy child.
Acknowledgments
Lecturer - K M Amran Hossain and Dr. Mohammad Abdul Bari not only for their valuable suggestion and guidelines and heartful thanks go to Md. Sha Al Emran for his technical support.
Author Contributions:
Zannatul Mawa
GROUP 1: Conception of the work, Acquisition and Analysis of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Mohima Benojir
GROUP 1: Design of the work, Analysis and Interpretation of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
GROUP 4: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Ruksana Akter
GROUP 1: Analysis of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
Shameem Ahammad
GROUP 1: Analysis and Interpretation of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Faruq Ahmed
GROUP 1: Interpretation of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
Mohammad Nazmul Hasan
GROUP 1: Design of the work
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Final approval of the version to be published
Nadia Afrin Urme
GROUP 1: Design of the work
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Shahid Afridi
GROUP 1: Analysis and Interpretation of data
GROUP 2: Revising the work critically for important intellectual content
GROUP 3: Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Funding: No funding source
Institutional Review Board Statement: (Ref no: CRP-R&E-0401)
Conflicts of Interest: No conflict of interest
References
- World Health Organization. The world health report 2002: Reducing risks, promoting healthy life. Genève, Switzerland: World Health Organization (2002).
- Malmivaara A. Evidence-based intervention for musculoskeletal disorders. Scandinavian Journal of Work, Environment and Health 23(1997): 161-163.
- Yoosefinejad AK, Hosseini A, Ashjaei HP, et al. Prevalance of Musculoskeletal Pain Disorder in Mothers with Disabled Children in Iran. Journal of Pharmaceutical and Biomedical Sciences 24 (2012): 74-76.
- Al-Gamal E, Long T. Anticipatory grieving among parents living with a child with cancer. Journal of Advanced Nursing 66 (2010): 1980-1990.
- TeRzi R, Tan G. Musculoskeletal system pain and related factors in mothers of children with cerebral palsy. Agri 28 (2016): 18-24.
- Bálint GP, Korda J, Hangody L, et al. Foot and ankle disorders. Best practice & research Clinical rheumatology 17 (2003): 87-111.
- Habib MM, Khanam F, Hafez MA, et al. Prevalence of low back pain (LBP) and its affect on everyday life among female caregivers of children with cerebral palsy (CP). Indian Journal of Physiotherapy and Occupational Therapy 8 (2014): 176.
- Mahmuda J. Demographic profile of cerebral palsy: a retrospective study(Dissertation): Department of Physiotherapy, Bangladesh Health Professions Institute, CRP (2013).
- Imran MH, Alam S, Haque KI, et al. Impact of sports on psychological status: Anxiety and depression for the spinal cord injury patients. Edorium Journal of Disability and Rehabilitation 19 (2018): 4.
- Benda W, McGibbon NH, Grant KL. Improvements in muscle symmetry in children with cerebral palsy after equine-assisted therapy (hippotherapy). The Journal of Alternative & Complementary Medicine 9 (2003): 817-825.
- Sanders MJ, Morse T. The ergonomics of caring for children: an exploratory study. The American journal of occupational therapy 59 (2005): 285-295.
- Tong HC, Haig AJ, Nelson VS, et al. Low back pain in adult female caregivers of children with physical disabilities. Archives of pediatrics & adolescent medicine 157 (2003): 1128-1133.
- Khandaker G, Muhit M, Karim T, et al. Epidemiology of cerebral palsy in Bangladesh: a population-based surveillance study. Developmental Medicine & Child Neurology 61 (2019): 601-609.
- Children in Bangladesh. Unicef.org. [cited 2022 Nov 10]. Available from: https://www.unicef.org/bangladesh/en/children-bangladesh
- TeRzi R, Tan G. Musculoskeletal system pain and related factors in mothers of children with cerebral palsy. Agri 28 (2016): 18-24.
- Tonga E, Düger T. Factors affecting low back pain in mothers who have disabled children. Journal of Back and Musculoskeletal Rehabilitation 21 (2008): 219-226.
- Wijnhoven H, de Vet H, Picavet H. Prevalence of Musculoskeletal Disorders Is Systematically Higher in Women Than in Men. The Clinical Journal of Pain 22 (2006): 717-724.
- Buckle PW, Devereux JJ. The nature of work-related neck and upper limb musculoskeletal disorders. Applied ergonomics 33 (2002): 207-217.
- Kaya K, Unsal-Delialioglu S, Ordu-Gokkaya NK, et al. Musculo-skeletal pain, quality of life and depression in mothers of children with cerebral palsy. Disability and Rehabilitation 32 (2010): 1666-1672.
Supplementary File:
Appendix A:
STROBE Statement—checklist of items that should be included in reports of observational studies.
|
Title and abstract |
Item No |
Recommendation |
Page No |
|
1 |
(a) Indicate the study’s design with a commonly used term in the title or the abstract |
1 |
|
|
(b) Provide in the abstract an informative and balanced summary of what was done and what was found |
1 |
||
|
Introduction |
|||
|
Background/rationale |
2 |
Explain the scientific background and rationale for the investigation being reported |
2-3 |
|
Objectives |
3 |
State specific objectives, including any prespecified hypotheses |
3 |
|
Methods |
|||
|
Study design |
4 |
Present key elements of study design early in the paper |
3 |
|
Setting |
5 |
Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection |
3-4 |
|
Participants |
6 |
Cross-sectional study—Give the eligibility criteria, and the sources and methods of selection of participants |
4 |
|
Variables |
7 |
Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable |
4 |
|
Data sources/ measurement |
8* |
For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group |
4 |
|
Bias |
9 |
Describe any efforts to address potential sources of bias |
4 |
|
Study size |
10 |
Explain how the study size was arrived at |
4,5 |
|
Quantitative variables |
11 |
Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why |
|
|
Statistical methods |
12 |
(a) Describe all statistical methods, including those used to control for confounding |
4 |
|
(b) Describe any methods used to examine subgroups and interactions |
|||
|
(c) Explain how missing data were addressed |
4 |
||
|
Results |
|||
|
Participants |
13* |
(a) Report numbers of individuals at each stage of study— eg: numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed |
NA |
|
(b) Give reasons for non-participation at each stage |
|||
|
(c) Consider use of a flow diagram |
|||
|
Descriptive data |
14* |
(a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders |
4,5 |
|
(b) Indicate number of participants with missing data for each variable of interest |
|||
|
Cross-sectional study—Report numbers of outcome events or summary measures |
5 |
||
|
Main results |
16 |
(a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included |
|
|
(b) Report category boundaries when continuous variables were categorized |
|||
|
(c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period |
|||
|
Other analyses |
17 |
Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses |
|
|
Discussion |
|||
|
Key results |
18 |
Summarise key results with reference to study objectives |
9,10 |
|
Limitations |
19 |
Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias |
10 |
|
Interpretation |
20 |
Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence |
9 |
|
Generalisability |
21 |
Discuss the generalisability (external validity) of the study results |
9 |
|
Other information |
|||
|
Funding |
22 |
Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based |
10 |