Modified Shock Index to Predict In-Hospital Outcome among Patients Presenting with ST-Segment Elevation Myocardial Infarction
Article Information
Md. Asifudduza1*, Nazir Ahmed2, Md. Owashak Faysal3, Rahatul Quadir4, Sharmin Ali5, Md. Rakibul Hasan6, Nurul Islam7, Sharmeen Sultana8
1Junior Consultant, Department of Cardiology, Labaid Cardiac Hospital, Dhaka, Bangladesh
2Professor, Department of Cardiology, National
Heart Foundation Hospital and Research Institute, Dhaka, Bangladesh
3Medical Officer, Department of Cardiology, National Institute of Cardiovascular Disease (NICVD), Dhaka, Bangladesh
4Assistant Registrar, Department of Cardiology, National Institute of Cardiovascular Diseases(NICVD), Dhaka, Bangladesh
5Medical Officer, Department of Cardiology, National Institute of Cardiovascular Diseases & Hospital (NICVD), Dhaka Bangladesh
6Junior Consultant, Department of Cardiology, Labaid Cardiac Hospital, Dhaka, Bangladesh
7Senior Medical Officer, Department of
Cardiology, National Heart Foundation Hospital & Research Institute, Dhaka, Bangladesh
8Associate Professor, Department of Microbiology, Monno Medical College and
Hospital, Manikganj, Bangladesh
Corresponding author: Dr. Md. Asifudduza, Junior Consultant, Department of Cardiology, Labaid Cardiac Hospital, Dhaka, Bangladesh
Received: May 06, 2023; Accepted: May 15, 2023; Published: July 07, 2023
Citation: Md. Asifudduza, Nazir Ahmed, Md. Owashak Faysal, Rahatul Quadir, Sharmin Ali, Md. Rakibul Hasan, Nurul Islam, Sharmeen Sultana. Modified Shock Index to Predict In- Hospital Outcome among Patients Presenting with ST-Segm2t Elevation Myocardial Infarction. Cardiology and Cardiovascular Medicine. 7 (2023): 229-240.
Share at FacebookAbstract
Background: Prompt identification of higher-risk patients presenting with ST-segment elevation myocardial infarction (STEMI) is crucial to pursue a more aggressive approach.
Objective: To evaluate the Modified Shock Index (MSI), as a predictor of in-hospital outcome among patients with STEMI. Methods: This cross sectional observational study was carried out in the Department of Cardiology, National Heart Foundation Hospital and Research Institute, Mirpur, Dhaka from January 2020 to December 2020. A total of 100 patients were selected with acute STEMI admitted in the department of Cardiology, NHFH&RI, within the study period, who fulfilled the inclusion and exclusion criteria.
Results: The mean age 55.6±10.2 years in Group I and 56.1±12.0 years in Group II. Male patients were predominant in both the groups. Regarding MSI 40(40.0%) patients had high admission MSI (≥0.91) and 60(60.0%) patients had normal admission MSI (<0.91). Regarding risk factors, hypertension, diabetes mellitus, smoking, dyslipidemia and family H/O CAD were not statistically significant (p>0.05) between the two groups. There was a significant (p<0.05) difference observed for NT-pro-BNP which was higher in group I than group II (77.5% vs 40.0%), but other investigations were not statistically significant (p>0.05) between the two groups. LVEF was found lower in Group I than group II (38.0±4.7 percent vs 42.6±5.2 percent), which was statistically significant (p<0.05) between the two groups. Regarding ECG findings 72.5% of patients were found with anterior MI in group I and 33.3% in group II, which was statistically significant (p<0.05) between the two groups. During the period of hospitalization patients in group I developed heart failure more than group II patients (67.5% vs 26.7%, p value=0.001). Development of cardiogenic shock was also significant in group I patients compared to group II patients (57.5% vs 1.7%, p value=0.001). Although the mortality rate was higher in group I patients, it was not significant between the two groups.
Conclusion: Heart failure and cardiogenic shock were significantly higher in MSI ≥ 0.91 group in comparison to MSI < 0.91 group. MSI was shown to be a valuable bedside tool which can rapidly identify high-risk STEMI patients at presentation.
Keywords
ST-segment elevation myocardial infarction (STEMI); Modified Shock Index (MSI); ECG findings
ST-segment elevation myocardial infarction (STEMI) articles; Modified Shock Index (MSI) articles; ECG findings articles
Article Details
Introduction
Cardiovascular diseases (CVDs) account for more than 17 million deaths globally each year, 80% of which occur in low-income and middle-income countries [1]. Coronary artery disease (CAD) is the predominant manifestation of CVD and was responsible for 7 million deaths worldwide in 2010 [2]. The prevalence of CAD in Bangladesh was first reported in 1976, which was 0.33% (Malik, 1976). More recent data indicate CAD prevalence to be 3.4% in rural [3] and 19.6% in an urban sample of working professionals in Bangladesh [4-6]. ACS is a major cause of mortality in developing countries and is responsible for a large number of hospitalizations annually [7]. ACS refers to a spectrum of conditions compatible with acute myocardial ischemia and/or infarction that are usually due to an abrupt reduction in coronary blood flow [8]. This includes acute STEMI and NSTE-ACS comprising of NSTEMI and UA. ST-segment elevation myocardial infarction (STEMI) results from a disruption of a vulnerable coronary atherosclerotic plaque complicated by intraluminal thrombus formation, embolization and variable degrees of coronary obstruction. Patients with total or near-total occlusion may present with acute ST-segment elevation Myocardial Infarction (STEMI) requiring emergency reperfusion therapy [9]. Effective and timely reperfusion of the infarct-related coronary artery is central to optimal treatment for both STEMI and NSTE- ACS and as expeditiously and efficiently achieved by the PCI [10]. Primary PCI is the preferred reperfusion strategy in cases of STEMI [11]. Furthermore, rescue PCI and early routine post-thrombolysis angiography with subsequent PCI has shown to reduce the rates of re-infarction and recurrent ischemia, in comparison to a more conservative strategy [12]. Though fibrinolysis and primary PCI are the two options for the patients presenting with STEMI, real-life data confirm that primary PCI is performed faster and results in lower mortality if performed in high-volume PCI centers [13]. Randomized clinical trials in high volume, experienced centers have repeatedly shown that, if the delay to treatment is similar, primary PCI is superior to fibrinolysis in reducing mortality, reinfarction, or stroke [14-17]. Nevertheless, in some circumstances, primary PCI is not an immediate option and fibrinolysis could be initiated expeditiously. If the reperfusion strategy is fibrinolysis, the goal is to inject the bolus of fibrinolytic within 10 minutes from STEMI diagnosis [18]. Fibrinolytic therapy is an important reperfusion strategy in settings where primary PCI cannot be offered on time and prevents 30 early deaths per 1,000 patients treated within 6 hours after symptom onset Fibrinolytic Therapy Trialist’s (FTT) Collaborative Group, 1994 [19]. The largest absolute benefit is seen among patients at the highest risk, including the elderly, and when treatment is offered < 2 h after symptom onset [20, 21]. Fibrinolytic therapy is recommended within 12 hours of symptom onset if primary PCI cannot be performed within 120-minutes from STEMI diagnosis in absence of contraindications. The later the patient presents (particularly after 3 hours) [22, 23,18] the more consideration should be given to transfer for primary PCI because the efficacy and clinical benefit of fibrinolysis decrease as the time from symptom onset increases [23]. In a meta-analysis of six randomized trials (n=6434), pre-hospital fibrinolysis reduced early mortality by 17% compared with in-hospital fibrinolysis [24]. Predominantly when administered in the first 2 hours of symptom onset. These and more recent data support pre- hospital initiation of fibrinolytic treatment when a reperfusion strategy is indicated [25-28]. Risk stratification for patients with STEMI is very important to identify those who deserve advanced measures. This can be done through the integration of various patient characteristics into a semi-quantitative score that can convey an overall estimate of a patient’s prognosis [29]. At present, several systems of risk stratification such as TIMI, GRACE, CADILLAC risk score and Euro Heart risk score are used but the sophisticated calculation usually makes them inconvenient to operate at the bedside in daily clinical practice [30-32]. The concept of shock index, defined as the ratio of heart rate and systolic blood pressure, first introduced by Allgower and Burri (1967) [33] as a simple and effective means for gauging the degree of hypovolemia in a hemorrhagic and infectious shock state. Subsequently, experimental and clinical studies demonstrated that SI was inversely related to physiologic parameters, such as cardiac index, stroke volume, left ventricular stroke volume and mean arterial pressure [34]. A new index, MSI is created by Liu et al. (2012) [35] as the HR and MAP. It has been noticed that SI uses only SBP, but DBP is also of undeniable importance when determining patient’s clinical severity. Hence diastolic blood pressure was incorporated and the MSI was developed [36]. MSI is an easily reachable index which does not depend on subjective information, previous patient history or blood tests. It only depends on measurement of blood pressure and heart rate on admission, which are less susceptible to fill-in errors [37]. It has been demonstrated to be a valid prognostic tool in medical or trauma patients admitted to the emergency department [35, 38, 39]. Liu et al. (2012) [35] showed that MSI of ≥1.3 was associated with an increased probability of intensive care unit admission or death. In patients with established Cardiogenic Shock, complete revascularization is recommended [40]. However, no study or recommendation has suggested any benefit from such an approach in patients at risk of developing cardiogenic shock and this may be an area for future studies. A high MSI denotes a sign of hypo dynamic circulation, a value of low stroke volume and low systemic vascular resistance, therefore, the patient may be compensating and the decompensation is rapid. MSI is a more important clinical predictor than blood pressure and heart rate because high MSI indicates a hypo dynamic state [35]. In these circumstances, MSI can be a valuable tool in predicting disease severity in the case of ACS patients. There are very few studies regarding MSI as the predictor of in- hospital outcome among patients presenting with STEMI in our country.
Objectives
General objective
To evaluate the Modified Shock Index (MSI), as a predictor of in-hospital outcome among patients with STEMI.
Specific objectives
- To calculate the modified shock index of the patients presenting with
- To assess the in-hospital outcomes (cardiogenic shock, acute left ventricular failure, Arrhythmia and death).
- To compare the in-hospital outcomes of the patients of two groups which are made based on MSI cut off
Materials and Methods
This was a cross sectional observational study. The patients were selected purposively. A total of 100 patients were included in this study in two groups. The study was conducted in the Department of Cardiology, National Heart Foundation Hospital and Research Institute, Mirpur, Dhaka. Bangladesh from the period of January, 2020 to December, 2020.
Inclusion criteria
- Newly diagnosed acute STEMI within 12 hours from symptom onset
- Those who were thrombolysed
Exclusion criteria
- On presentation:
- Cardiogenic shock
- Cardiac arrest
- Acute heart failure
- Significant tachy or brady arrhythmia (VT, VF, SVT, CHB)
- Previous coronary artery bypass graft (CABG).
- Previous history of myocardial infarction (MI).
- Pacemaker or internal cardioverter
- Having cardiomyopathy, any valvular heart disease, congenital heart disease, pericardial
- Severe co-morbid conditions such as liver disease, renal disease, thyroid disorder, malignancy.
- Study subjects who were not
Study procedure
100 of the patients admitted into National Heart Foundation Hospital & Research Institute, Dhaka, Bangladesh with acute STEMI fulfilling the inclusion and exclusion criteria were included in this study. The study subjects were first assessed by the attending doctors and then were evaluated by the principal investigator. All demographic data were recorded in predesigned semi-structured questionnaire and checklist. Meticulous history was taken regarding symptoms and a detailed clinical examination was performed upon admission & throughout the hospitalization period and was recorded in predesigned semi-structured forms. SBP & DBP was measured in the Emergency Department by a well- calibrated sphygmomanometer & >2 readings were taken with 1 min interval and averaged. 12 lead ECG was obtained from all patients at admission. Heart rate was obtained at the same time from the corresponding 12 lead ECG. MAP was calculated using the formula {(2×DBP)+SBP}/3 [41]. MSI was calculated using the formula Heart rate/MAP [35]. The cut-off value of MSI was 0.91 based on previous study results, which showed MSI ≥0.91 was significant independent predictor of mortality in STEMI patients. MSI ≥0.91 was considered as high MSI and that of <0.91 was considered as normal MSI (Gouda et al., 2016) [42]. The patients were divided into two groups based on the MSI. Dual antiplatelet therapy, statins, ß-blockers, Angiotensin converting enzyme inhibitors and intravenous diuretics were given as per guidelines if there were no contraindication. Killip’s classification, chest examination- with emphasis on detecting pulmonary edema or presence of pulmonary congestion, Cardiac examinations- with emphasis on detecting S3 Gallop, murmurs suspecting presence of mechanical complications. Laboratory investigations: Cardiac enzymes, CBC, Kidney function, blood sugar, liver function and coagulation profile in selected patients. Echocardiography & chest X-ray were performed in the first 48 hours following admission and was recorded. Patients were admitted to our CCU for at least 48 hours to continue anti-ischemic treatment. The study subjects were followed up for in-hospital outcome, from hospital admission till discharge or death. The in-hospital outcomes were acute left ventricular failure, cardiogenic shock, arrhythmia (VT, VF, AF) and death. These variables were assessed and compared for each group.
Statistical analysis
All the statistical analyses were performed by using SPSS version 23.0 for windows. The mean values were calculated for continuous variables. The quantitative variables were expressed as mean with standard deviation and the qualitative variables were expressed as frequency (%). Chi-square test was used to analyze the categorical variables and student t-test was performed to analyze continuous variables. Multivariate regression analysis was considered to evaluate the influence of potential risk factors. Risk measurement was done by Odds ratio (OR). P-value <0.05 was considered statistically significant in all cases.
Results
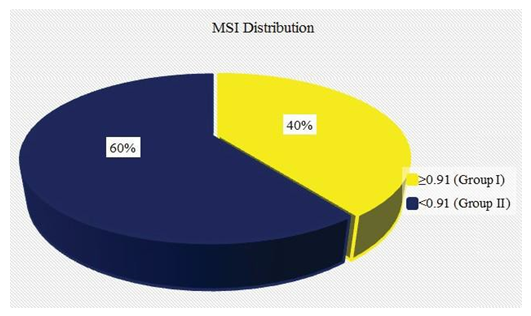
This cross-sectional observational study was conducted in the Department of Cardiology, National Heart Foundation Hospital and Research Institute, Mirpur, Dhaka, over one year from January 2020 to December 2020 to evaluate the MSI, as a predictor of in-hospital outcome among patients with STEMI. A total of 100 patients were selected among the patients admitted in the department of cardiology, National
Heart Foundation Hospital and Research Institute with acute STEMI, within the study period and who fulfilled the inclusion and exclusion criteria. The main objective of this study was to evaluate the MSI, as a predictor of in-hospital outcome among patients with STEMI. MSI on admission was measured and patients were divided into two groups. Patients with 'high modified shock index (MSI ≥0.91) were included in Group I and those with 'normal modified shock index (MSI
<0.91) were included in Group II.
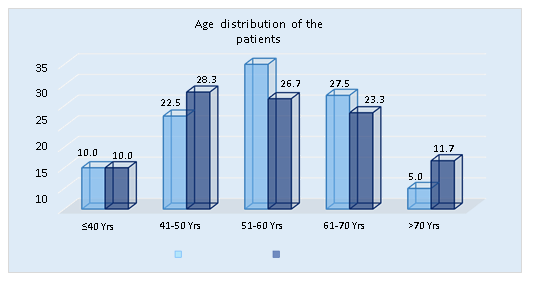
Table 1: Distribution of the study patients according to age. (N=100)
|
Age (years) |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
≤40 yrs. |
4 |
10.0 |
6 |
10.0 |
|
|
41-50 yrs. |
9 |
22.5 |
17 |
28.3 |
|
|
51-60 yrs. |
14 |
35.0 |
16 |
26.7 |
|
|
61-70 yrs. |
11 |
27.5 |
14 |
23.3 |
|
|
>70 yrs. |
2 |
5.0 |
7 |
11.7 |
|
|
Mean ± SD |
55.6±10.2 |
56.1±12.0 |
0.829 |
||
|
Range (min-max) |
35-74 |
30-85 |
|||
Table 1 showed group wise age distribution of the patients.
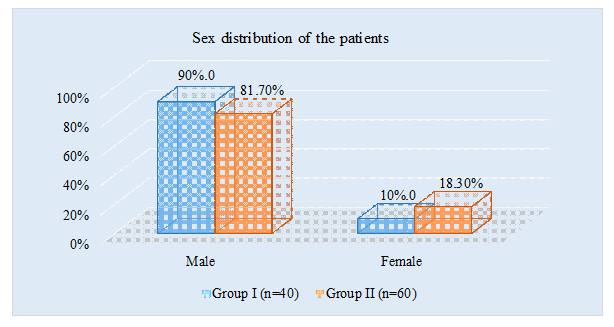
Table 2: Distribution of the study patients according to gender. (N=100)
|
Gender |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
0.252 |
|
|
Male |
36 |
90.0 |
49 |
81.7 |
|
|
Female |
4 |
10.0 |
11 |
18.3 |
|
Table 2 showed male patients were predominant in both the groups. But gender distribution was similar between the groups (N=100).
Table 3: Distribution of the study patients according to body mass index. (N=100)
|
BMI (kg/m2) |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
18.5-24.9 (Normal) |
29 |
72.5 |
37 |
61.7 |
|
|
25.0-29.0 (Overweight) |
11 |
27.5 |
22 |
36.7 |
|
|
≥30 (Obese) |
0 |
0.0 |
1 |
1.7 |
|
|
Mean ± SD |
23.9±2.4 |
24.3±2.6 |
0.439 |
||
|
Range (min-max) |
19.1-29.4 |
18.6-31.3 |
|||
Table 3 showed mean BMI was found 23.9±2.4 kg/m2 in group I and 24.3±2.6 kg/m2 in group II. The difference was not statistically significant (p >0.05) between two groups.
Table 4: Distribution of the study patients according to clinical profile. (N=100)
|
Clinical profile |
Group I (n=40) |
Group II (n=60) |
P value |
|
Mean ±SD |
Mean ±SD |
||
|
Duration of chest pain (hours) |
6.5±3.6 |
5.7±2.6 |
0.200 |
|
Heart rate (beats/ min) |
97.8±15.6 |
71.9±13.0 |
0.001 |
|
Systolic blood pressure (mmHg) |
113.5±17.5 |
131.3±19.6 |
0.001 |
|
Diastolic blood pressure (mmHg) |
72.5±10.0 |
83.3±11.1 |
0.001 |
|
Mean arterial pressure (mmHg) |
86.8±12.3 |
99.3±13.3 |
0.001 |
Table 4 showed patients in group I were hemodynamically more unstable than those in group II as evidenced by increased mean heart rate (97.8±15.6 vs 71.9±13.0 beats/ min, p=0.001), decreased systolic blood pressure (113.5±17.5 vs 131.3±19.6 mmHg, p=0.001), decreased diastolic blood pressure (72.5±10.0 vs 83.3±11.1 mmHg, p=0.001) and decreased mean arterial pressure (86.8±12.3 vs 99.3±13.3 mmHg, p=0.001).
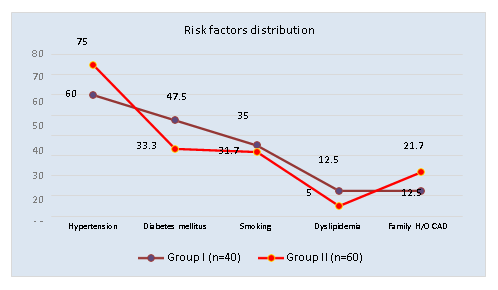
Table 5: Distribution of the study patients according to risk factors. (N=100)
|
Risk factors |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
Hypertension |
24 |
60.0 |
45 |
75.0 |
0.112 |
|
Diabetes mellitus |
19 |
47.5 |
20 |
33.3 |
0.155 |
|
Smoking |
14 |
35.0 |
19 |
31.7 |
0.728 |
|
Dyslipidemia |
5 |
12.5 |
3 |
5.0 |
0.164 |
|
Family H/O CAD |
5 |
12.5 |
13 |
21.7 |
0.242 |
Table 5 showed out of 100 patients, hypertensive, diabetes mellitus, smoking, dyslipidemia and family H/O CAD were not statistically significant (p>0.05) between the two groups.
Table 6: Distribution of the study patients according to pulmonary crackles on auscultation. (N=100)
|
Pulmonary crackles on auscultation |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
Yes |
25 |
62.5 |
14 |
23.3 |
0.001 |
|
No |
15 |
37.5 |
46 |
76.7 |
|
Table 6 showed the number of patients with pulmonary crackles on auscultation were higher in group I than group II (62.5% vs 23.3%, p=0.001), which was statistically significant.
Table 7: Distribution of the study patients according to investigations. (N=100)
|
Investigations |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
Mean ±SD |
Mean ±SD |
||||
|
Random blood glucose (mmol/L) |
10.7±4.8 |
9.2±3.1 |
0.060 |
||
|
HbA1c (%) |
7.3±1.9 |
6.8±1.3 |
0.121 |
||
|
Hs- cTnI (ng/ml) |
74.2±23.0 |
71.3±28.2 |
0.590 |
||
|
S. creatinine (mg/dl) |
1.36±0.43 |
1.25±0.29 |
0.130 |
||
|
NT-pro-BNP (pg/ml) |
n |
% |
n |
% |
|
|
<450 |
9 |
22.5 |
36 |
60.0 |
0.001 |
|
≥450 |
31 |
77.5 |
24 |
40.0 |
|
Table 7 showed distribution of patients according to biochemical parameters. There was a significant (p<0.05) difference observed for NT-pro- BNP which was higher in group I than group II (77.5% vs 40.0%), but other investigations were not statistically significant (p>0.05) between the two groups.
Table 8: Distribution of the study patients according to LVEF. (N=100)
|
LVEF (%) |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
≤40 |
29 |
72.5 |
19 |
31.7 |
|
|
>40 |
11 |
27.5 |
41 |
68.3 |
|
|
Mean ± SD |
38.0±4.7 |
42.6±5.2 |
0.001 |
||
|
Range (min-max) |
30-48 |
30-54 |
|||
Table 8 showed LVEF was found higher in group II patients compared to group I (42.6±5.2 percent vs 38.0±4.7 percent), which was statistically significant (p<0.05) between the two groups.
Table 9: Distribution of the study patients according to pulmonary congestion on CXR. (N=100)
|
Pulmonary congestion on CXR |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
Yes |
25 |
62.5 |
12 |
20.0 |
0.001 |
|
No |
15 |
37.5 |
48 |
80.0 |
|
Table 9 showed distribution of patients according to pulmonary congestion by groups. There was statistically significant (p<0.05) difference observed for pulmonary congestion which was higher in group I than group II (62.5% vs 20.0%, p=0.001).
Table 10: Distribution of the study patients according to ECG characteristics. (N=100)
|
ECG characteristics |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
Anterior |
29 |
72.5 |
20 |
33.3 |
|
|
Anterior+ Inferior |
0 |
0.0 |
1 |
1.7 |
0.001 |
|
Inferior |
11 |
27.5 |
39 |
65.0 |
|
Table 10 showed 72.5% of patients were found with anterior MI in group I and 33.3% in group II, which was statistically significant (p<0.05) between the two groups.
Table 11: Distribution of the study patients according to in-hospital outcome. (N=100)
|
In-hospital outcome |
Group I (n=40) |
Group II (n=60) |
P value |
||
|
n |
% |
n |
% |
||
|
Arrhythmias (VT, VF, AF) |
9 |
22.5 |
7 |
11.7 |
0.148 |
|
Heart failure |
27 |
67.5 |
16 |
26.7 |
0.001 |
|
Cardiogenic shock |
23 |
57.5 |
1 |
1.7 |
0.001 |
|
Death |
5 |
12.5 |
2 |
3.3 |
0.088 |
Table 11 showed during hospital admission patients in group I developed heart failure more than group II patients (67.5% vs 26.7%, p value=0.001). Development of cardiogenic shock was also significant in group I patients compared to group II patients (57.5% vs 1.7%, p value=0.001). Although the mortality rate was higher in group I patients, it was not significant between the two groups.
Table 12: Multivariate logistic regression analysis for in-hospital outcome in STEMI patients. (N=100)
|
Variables |
Regression coefficient (β) |
Odds Ratio (OR) |
95% CI for OR |
P value |
|
Heart rate (>100 beats/ min) |
1.299 |
3.667 |
0.526-25.549 |
0.190 |
|
Pulmonary crackles on auscultation |
20.357 |
6.932 |
0.016-96.310 |
0.997 |
|
Pulmonary congestion |
20.084 |
5.278 |
0.099-97.418 |
0.997 |
|
Modified shock index (≥0.91) |
2.005 |
7.429 |
2.905-18.997 |
0.001 |
Table 12 showed Multivariate logistic regression model was constructed with hypertension, heart rate >100 beats/min, pulmonary crackles on auscultation, pulmonary congestion and modified shock index ≥0.91 as independent variables and presence of in-hospital outcome as the dependent variable. Admission modified shock index (≥0.91) was found to be significantly associated with in-hospital outcome in acute STEMI patients (OR=7.429, p value=0.001).
Discussion
This cross-sectional observational study was conducted in the Department of Cardiology, National Heart Foundation Hospital and Research Institute, Mirpur, Dhaka, Bangladesh over one year from January 2020 to December 2020 to evaluate the Modified Shock Index (MSI), as a predictor of in-hospital outcome among patients with STEMI. A total of 100 patients admitted in the department of cardiology, National Heart Foundation Hospital and Research Institute with acute STEMI, within the study period who fulfilled the inclusion and exclusion criteria were included in this study. The main objective of this study was to evaluate the Modified Shock Index (MSI), as a predictor of in-hospital outcome among patients with STEMI. Modified Shock Index (MSI) on admission was measured and patients were divided into two groups. Patients with 'high modified shock index (MSI ≥0.91) were included in Group I and those with 'normal modified shock index (MSI <0.91) were included in Group II. In this study high admission modified shock index (≥0.91) had no significant association with acute STEMI patients in regards to age. Gouda et al. (2016) [42] reported that the mean age was found 57.83±11.49 years in MSI >0.91 group and 52.5±9.47 years in MSI <0.91 group. The difference was statistically significant (p<0.05) between the two groups. Abreu et al. (2018) [37] reported the mean age was found 61±13 years in MSI <0.93 group and 62±14 years in MSI ≥0.93 group. The difference was not statistically significant (p>0.05) between the two groups. Ali et al. (2019) [43] reported that the mean age of the patients in the normal MSI group was 57.42±11.32 years and in raised MSI group was 56.03±12.48 years. In this study, we observed that male patients were predominant in both groups. But gender distribution was similar between the groups (p=0.252). Gouda et al. (2016) [42] reported male patients was found 72.4% in MSI >0.91 group and 77.1% in MSI <0.91 group. The difference was not statistically significant (p>0.05) between the two groups. Abreu et al. (2018) [37] observed 16.5% of patients were found female in MSI <0.93 group and 21.9% in MSI ≥0.93 group. The difference was statistically significant (p<0.05) between the two groups. Ali et al. (2019) [43] reported about 58(48.33%) patients were males. The male to female ratio of the patients was 0.9:1. This study showed among 100 patients, 40(40.0%) patients had high admission MSI (≥0.91) and 60(60.0%) patients had normal admission MSI (<0.91). Gouda et al. (2016) [42] observed 120(55.6%) patients were found in the MSI >0.91 group and 96(44.4%) in MSI <0.91 group. The mean MSI was found 1.03±0.45. Abreu et al. (2018) [37] 324(28.0%) patients had MSI ≥0.93 and 843(72.0%) patients had MSI <0.93. Ali et al. (2019) [43] reported mean value MSI of the patients was 1.54±0.52 with minimum and maximum MSI values of 0.8 & 2.5 respectively. This study showed that mean BMI was found 23.9±2.4 kg/m2 in group I and 24.3±2.6 kg/m2 in group II. The difference was not statistically significant (p>0.05) between the two groups. Abreu et al. (2018) [37] observed that the mean BMI was found 27±4 kg/m2 in MSI <0.93 and 27±4 kg/m2 in MSI ≥0.93 group. The difference was not statistically significant (p>0.05) between the two groups. This study showed that the clinical profile of patients in group I were more unstable than those in group II as evidenced by increased mean heart rate (97.8±15.6 vs 71.9±13.0 beats/ min, p=0.001), decreased systolic blood pressure (113.5±17.5 vs 131.3±19.6 mmHg, p=0.001), decreased diastolic blood pressure (72.5±10.0 vs 83.3±11.1 mmHg, p=0.001) and decreased mean arterial pressure (86.8±12.3 vs 99.3±13.3 mmHg, p=0.001). Gouda et al. (2016) [42] reported in their observation a highly statistically significant increase in HR (p<0.001), while there was a highly statistically significant decrease in SBP and DPB (all p<0.001) in patients with high MSI compared to patients with normal MSI. Abreu et al. (2018) [37] observed that the mean heart rate, SBP, DBP and MAP were significantly higher in MSI <0.93 that MSI ≥0.93 group. It was observed that, out of 100 patients, hypertension, diabetes mellitus, smoking, dyslipidemia and family H/O CAD were not statistically significant (p>0.05) between the two groups. Gouda et al. (2016) [42] reported there was no statistically significant increase in cardiac enzymes (p=0.859), DM (p=0.38), HTN (p=0.51), history of IHD (p=0.65), history of previous PCI (p=0.27), positive family history of premature CAD (p=0.09), pre-infarction angina (p=0.19), or sinus rhythm (p=0.45), and no statistically significant decrease in smoking (p=0.87), or history of stroke (p=0.78) in patients with high MSI compared to patients with normal MSI. Abreu et al. (2018) [37] observed 21.6% of patients were found diabetic in MSI <0.93 and 28.4% in MSI ≥0.93 group, which was statistically significant (p<0.05) but other risk factors were not statistically significant (p>0.05) between the two groups. In the current study, it also revealed that NT-pro-BNP (≥450) was found higher in group I than group II (77.5% vs 40.0%)patients, which was statistically significant (p<0.05) but other investigations were not statistically significant (p>0.05) between two groups. Abreu et al. (2018) [37] observed the mean NT-pro-BNP was found 2228±4515 pg/ml in MSI <0.93 and 2816±4401 pg/ml in MSI ≥0.93 group, which was not statistically significant (p>0.05) between two groups. Regarding Echocardiography, LVEF (%) was found higher in group II patients compared to group I (42.6±5.2 percent vs 38.0±4.7 percent), which was statistically significant (p<0.05) between the two groups. Gouda et al. (2016) [42] reported a statistically significant decrease in EF (p=0.004) in patients with high MSI compared to patients with normal MSI. Abreu et al. (2018) [37] observed 39.1% of patients was found LVEF ≤40 percent in MSI <0.93 and 45.9% in MSI ≥0.93 group, which was statistically significant (p<0.05) between the two groups. Da Mota et al (2018) [44] showed on admission, patients with a MSI ≥1.3 had a lower LVEF (%) (43.95% vs 56.46%, p<0.001) in comparison to the patients with MSI <1.3. This study also revealed that 72.5% of patients were found with anterior MI in group I and 33.3% in group II, which was statistically significant (p<0.05) between the two groups. Abreu et al. (2018) [37] reported 65.9% of patients was found with anterior myocardial infarction in MSI <0.93 and 63% in MSI ≥0.93 group, which was not statistically significant (p>0.05) between the two groups. Da Mota et al. (2018) [44] reported on admission, patients with a MSI ≥1.3 had more frequently an anterior MI (71.9% vs 41.1%, p<0.001). In this study, we observed that patients in group I developed heart failure more than group II patients (67.5% vs 26.7%, p value=0.001) during hospital admission. The development of cardiogenic shock was also significant in group I patients compared to group II patients (57.5% vs 1.7%, p value=0.001). Although the mortality rate was higher in group I patients, it was not significant between the two groups. Gouda et al. (2016) [42] reported to in-hospital MACE and mortality their study demonstrated a highly statistically significant increase in HF (p<0.001), and there was a statistically significant increase in cardiogenic shock (p =0.019), fatal arrhythmia (p=0.007), bleeding (p=0.026), arrest (p=0.005), and mortality (p=0.008), while there was no statistically significant increase in re- infarction (p=0.37), non-fatal arrhythmia (p=0.43), or stroke (p=0.2) in patients with high MSI compared to patients with normal MSI. Studies results show that in patients with a high MSI, there is an increased probability of ICU admission and death. MSI is a more important clinical predictor than blood pressure and heart rate because high MSI indicates a hypo dynamic state (Liu et al., 2012) [35]. Elevated MSI was associated with a significant increase in the incidence of cardiogenic shock, fatal arrhythmia, bleeding, arrest and mortality. This was associated with a highly significant increase in the incidence of HF. That was in agreement with the results of Shangguan et al. (2015) [45], who showed that with MSI >1.4, there was a highly significant increase of incidence of 7-day MACE, fatal arrhythmia, and all-cause mortality, and there was a significant increase in the incidence of Killip class, but he found no significant increase in the incidence of cardiogenic shock. Abreu et al. (2015) [46], who enrolled 1140 consecutive STEMI patients treated by both types of reperfusion (pharmacological and mechanical) retrospectively, and with MSI cut off=1.3 showed that with MSI >1.3 there was a significant increase of incidence of in- hospital mechanical complications, malignant arrhythmia, and there was a highly significant increase of incidence of respiratory tract infections, and all-cause mortality. Abreu et al. (2018) [37] reported that the proportion of patients with acute heart failure (36.1% vs. 24.6%; p<0.001) and cardiogenic shock (6.5% vs. 2.4%; p=0.001) was higher in patients with MSI ≥0.93. Ali et al. (2019) [43] observed in- hospital mortality occurred in 27 cases in which 4 were from normal MSI and 23 were from raised MSI group. In the current study, a multivariate logistic regression model was constructed with hypertension, heart rate >100 beats/min, pulmonary crackles on auscultation, pulmonary congestion and modified shock index ≥0.91 as independent variables and presence of in-hospital outcome as the dependent variable. Admission modified shock index (≥0.9) was found to be significantly associated with in-hospital outcome in acute STEMI patients (OR=7.429, p value=0.001). agreement with Shangguan et al. (2015) [45], where multifactor analysis showed that, in addition to MSI or ASI, age was an independent factor for the 7-day MACE, with the OR of MSI was higher than that of age (3.05 vs 1.07). These results indicated that the poorer outcome in the increased MSI groups is not because of the older age, as the older patients may have higher SBP and lower DBP and then had higher MSI. Abreu et al. (2018) [37] reported that the right ventricular dysfunction (adjusted odds ratio [OR] 5.0, 95% CI 2.05-12.21; p<0.001) and left ventricular dysfunction (adjusted OR 4.87,95% CI 1.12-4.78; p=0.001) were the strongest independent predictors, although the presence of acute heart failure on admission (adjusted OR 3.41, 95% CI 1.63-7.16; p<0.001)
and MSI ≥0.93 (adjusted OR 2.731, 95% CI 1.12-4.78; p=0.023) provided additional information. Reinstadler et al. (2016) [47] statistically 5.75 times protective effect of in- hospital mortality was noted in raised MSI group compared to normal group patients i.e. RR=5.75 [95% CI; 2.1160 to 15.6252]. Da Mota et al. (2018) [44] reported multivariate statistical analysis, a MSI ≥1.3 was a strong independent predictor of AHF at admission or during hospitalization (OR 3.66, 95% CI 1.7–8.1, p=0.001). Liu et al. (2012) [35] observed MSI or SI was used instead of heart rate and blood pressure, MSI>1.3 or <0.7 served as a stronger predictor of death. In contrast to traditional beliefs, SI of 0.5-0.9 was not correlated with the mortality rate of emergency department patients. We aimed to evaluate the relationship of the modified shock index (MSI) with short term outcome in acute STEMI patients. After taking into account the potential confounding effect of various factors, it was found that modified shock index (MSI) ≥0.91 can be considered as an independent predictor of adverse short term outcome in acute STEMI patients (OR=7.429, p value=0.001). The simple algorithm also makes its use accessible during the first contact with the patients. In our study, the MSI was shown to be valuable in identifying more critical and morbid patients presenting at a pre-shock stage. By identifying patients with worse prognosis, this index can enable closer monitoring and increase alertness for possible complications. In the early management of high- risk patients with relative hypotension and tachycardia, this tool can be used not only to assess risk but also to prevent iatrogenic cardiogenic shock by avoiding certain therapies, such as beta-blockers or ACE inhibitors.
Conclusion
In our study, a MSI ≥0.91 was a strong independent predictor of in hospital outcome among STEMI patients. Acute left ventricular failure and cardiogenic shock were significantly more in patients with admission modified shock index ≥0.91.
Limitations of the Study
Although the result of this study supported the hypothesis there were some facts that might have affected the results: This is a single-centre study and purposive sampling was done instead of random sampling. Therefore, the results of the study may not reflect the exact picture of the country. Lack of long term follow up. Data regarding medication that might influence HR and BP before admission were not available and whether the modified shock index was representative of this critical stress in these patients deserved further study.
Recommendations
Admission modified shock index can be assessed in all patients with acute STEMI. Patients with a modified shock index of ≥0.91 should be paid more attention and early intervention should be planned in this group of patients. It can also be used to prevent cardiogenic shock by avoiding some therapies in the early management of high-risk patients with relative hypotension and tachycardia. Further prospective study with a larger sample and longer follow up period is recommended.
Ethical Issue
The study was approved by the Ethics Review Committee of National Heart Foundation Hospital & Research Institute, Dhaka, Bangladesh.
References
- Mendis S, Puska P, Norrving B, eds. Global Atlas on Cardiovascular Disease Prevention and [pdf] Geneva:WHO Press (2011): 1-166.
- Wong Epidemiological studies of CHD and the evolution of preventive cardiology. Nature Reviews Cardiology 11 (2014): 276.
- Zaman MM, Ahmed J, Choudhury SR, Numan SM, Parvin K, et al. Prevalence of ischemic heart disease in a rural population of Bangladesh. Indian Heart J 59 (2007): 239-241.
- Ahsan SA, Haque KS, Salman M, Bari AS, Nahar H, et Detection of ischaemic heart disease with risk factors in different categories of employees of University Grants Commission. University Heart Journal 5 (2009): 20-23.
- Saquib N, Saquib J, Ahmed T, Khanam MA, Cullen Cardiovascular diseases and type 2 diabetes in Bangladesh: a systematic review and meta-analysis of studies between 1995 and 2010. BMC Public Health 12 (2012): 434.
- Islam, Majumder AKMMAAS. Coronary artery disease in Bangladesh: A Indian Heart Journal 65 (2013): 424-435.
- Murray CJL, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 349 (1997): 1269-1276.
- Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, et 2014 AHA/ACC guideline for the management of patients with non STelevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130 (2014): e344-e426.
- Iqbal KM, Ahsan SA, Rahman MM, Chowdhury MT, Ahmed K, et al. Prediction of MACE by Angiographic Perfusion Score (APS) in Risk Stratification following Percutaneous Coronary Stenting in STEMI without Thrombolytic University Heart Journal 15 (2019): 16-21.
- Bagai A, Dangas GD, Stone GW, Granger Reperfusion Strategies in Acute Coronary Syndromes. Circulation Research 114 (2014): 1918-1928.
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli- Ducci C, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Euro Heart Journal 239 (2017): 119-177.
- Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, et 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio- Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). European Heart Journal 35 (2014): 2541-2619.
- West RM, Cattle BA, Bouyssie M, Squire I, de Belder M, et al. Impact of hospital proportion and volume on primary percutaneous coronary intervention performance in England and Wales. European heart journal 32 (2011): 706-711.
- Zijlstra F, Hoorntje JC, de Boer MJ, Reiffers S, Miedema K, et al. Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial New England Journal of Medicine 341 (1999): 1413-1419.
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. The Lancet 361 (2003): 13-20.
- Widimský P, Budešínský T, Vorác D, Groch L, Zelízko M, et al. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction: final results of the randomized national multicentre trial— PRAGUE-2. European heart journal 24 (2003): 94-104.
- Andersen HR, Nielsen TT, Rasmussen K, Thuesen L, Kelbaek H, et al. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. New England journal of medicine 349 (2003): 733-742.
- Armstrong PW, Gershlick AH, Goldstein P, Wilcox R, Danays T, et al. Fibrinolysis or primary PCI in ST- segment elevation myocardial infarction. N Engl J Med 368 (2013): 1379-1387.
- Fibrinolytic Therapy Trialists’ (FTT) Collaborative Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. The lancet 343 (1994): 311-322.
- Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. The Lancet 348 (1996): 771-775.
- White HD. Thrombolytic therapy in the elderly. Lancet 356 (2000): 2028-2030.
- Bonnefoy E, Steg PG, Boutitie F, Dubien PY, Lapostolle F, et Comparison of primary angioplasty and pre-hospital fibrinolysis in acute myocardial infarction (CAPTIM) trial: a 5-year follow-up. Eur Heart J 30 (2009): 1598- 1606.
- Pinto DS, Frederick PD, Chakrabarti AK, Kirtane AJ, Ullman E, et Benefit of transferring ST-segment– elevation myocardial infarction patients for percutaneous coronary intervention compared with administration of onsite fibrinolytic declines as delays increase. Circulation 124 (2011): 2512-2521.
- Morrison LJ, Verbeek PR, McDonald AC, Sawadsky BV, Cook DJ. Mortality and prehospital thrombolysis for acute myocardial infarction: a meta-analysis. Jama 283 (2000): 2686-2692.
- Steg PG, Bonnefoy E, Chabaud S, Lapostolle F, Dubien PY, et al. Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty: data from the CAPTIM randomized clinical trial. Circulation 108 (2003): 2851-2856.
- Danchin N, Coste P, Ferrieres J, Steg PG, Cottin Y, et al. FAST-MI Investigators. Comparison of thrombolysis followed by broad use of percutaneous coronary intervention with primary percutaneous coronary intervention for ST-segmentelevation acute myocardial infarction: Data from the French registry on acute ST- elevation myocardial infarction (FAST-MI). Circulation 118 (2008): 268-276.
- Kalla K, Christ G, Karnik R, Malzer R, Norman G, et Implementation of guidelines improves the standard of care: The Viennese registry on reperfusion strategies in ST-elevation myocardial infarction (Vienna STEMI registry). Circulation 113 (2006): 2398-2405.
- Kristensen SD, Laut KG, Fajadet J, Kaifoszova Z, Kala P, et al. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: current status in 37 ESC European heart journal 35 (2014): 1957-1970.
- O'gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American college of cardiology 61 (2013): e362-e425.
- Morrow DA, Antman EM, Charlesworth A, Cairns R, Murphy SA, et TIMI risk score for ST elevation MI: a convenient, bedside, clinical score for risk asseessment at presentation: an intravenous n PA for treatment of infarcting myocardium early II trial sub- study. Circulation 102 (2000): 2031-2037.
- Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, et al. Predictors of hospital mortality in the global registry of acute coronary events. Archive Internal Medicine 163 (2003): 2345-2353.
- De Mulder M, Gitt A, Van Domburg R, Hochadel M, Seabra-Gomes R, et Euro heart Score for the evaluation of in-hospital Mortality in patients undergoing percutaneous coronary intervention. European Heart Journal 32 (2011): 1398-1408.
- Allgeower M, Burri Shock index. Deutsche Medizinische Wochenschrift 92 (1967): 1947-1950.
- Rady MY, Rivers EP, Martin GB, Smithline H, Appelton T, et al. Continuous central venous oximetry and shock index in the emergency department: use in the evaluation of clinical shock. The American journal of emergency medicine 10 (1992): 538-541.
- Liu YC, Liu JH, Fang ZA, Shan GL, Xu J, et Modified shock index and mortality rate of emergency patients. World journal of emergency medicine 3 (2012): 114-117.
- Zarzaur BL, Croce MA, Fischer PE, Magnotti LJ, Fabian New vitals after injury: shock index for the young and age× shock index for the old. Journal of Surgical Research 147 (2008): 229-236.
- Abreu G, Azevedo P, Braga CG, Vieira C, Pereira MÁ, et al. Modified shock index: a bedside clinical index for risk assessment of ST-segment elevation myocardial infarction at Revista Portuguesa de Cardiologia (English Edition) 37 (2018): 481-488.
- Singh A, Ali S, Agarwal A, Srivastava Correlation of shock index and modified shock index with the outcome of adult trauma patients: a prospective study of 9860 patients. North American journal of medical sciences 6 (2014): 450.
- Torabi M, Mirafzal A, Rastegari A, Sadeghkhani Association of triage time shock index, modified shock index, and age shock index with mortality in emergency severity index level 2 patients. The American journal of emergency medicine 34 (2016): 63-68.
- Hochman JS, Sleeper LA, Webb JG, Sanborn TA, White HD, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic SHOCK Investigators. Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock. The New England Journal of Medicine 341 (1999): 625-634.
- Papaioannou TG, Protogerou AD, Vavuranakis M, Tousoulis D. Mean arterial pressure estimation by a non- traditional formula and fractional pulse pressure. Journal of the American College of Cardiology 68 (2016): 668-
- Gouda M, Saad AM, Al-Daydamony M. Modified Shock Index as a predictor of in Hospital outcome in cases of ST-Segment Elevation Myocardial Infarction Treated with Primary Percutaneous Coronary J Cardiol Curr Res 7 (2016): 00255.
- Ali M, Butt UM, Hameed MH. Raised Modified Shock Index (MSI) as a predictor of inhospital mortality in patients with St-Segment Elevation Myocardial Infarction (STEMI). Pakistan Heart Journal 51 (2019): 286-290.
- Da Mota TF, Azevedo P, Bispo J, Fernandes R, Guedes JP, et al, August. Modified shock index-an independent predictor of acute heart failure and in-hospital mortality in patients with ST-segment elevation myocardial In European Heart Journal 39 (2018): 1353-1353.
- Shangguan Q, Xu JS, Su H, Li JX, Wang WY, et al. Modified shock index is a predictor for 7-day outcomes in patients with The American journal of emergency medicine 33 (2015): 1072-1075.
- Abreu G, Braga C, Martins J, Quina-Rodrigues C, Vieira C, et Modified shock index-a strong preditor of outcome among patients presenting ST-segment elevation myocardial infarction. World J Emerg Med 3 (2015): 114- 117.
- Reinstadler SJ, Fuernau G, Eitel C, de Waha S, Desch S, et Shock index as a predictor of myocardial damage and clinical outcome in ST-elevation myocardial infarction. Circulation Journal 80 (2016): 924-930.