Medical Cannabis in Lebanon: History & Therapeutic, Ethical, and Social Challenges. A Narrative Review
Article Information
Battoul Fakhry1, Mostafa Abdulrahim1, Mirna N Chahine2*
1Department of Medical Ethics, Lebanese University, Faculty of Medical Sciences, Beirut, Lebanon
2Department of Basic Sciences, Lebanese University, Faculty of Medical Sciences, Beirut, Lebanon
*Corresponding author: Prof. Mirna Chahine, Department of Basic Sciences, Lebanese University, Faculty of Medical Sciences, Hadath, Beirut, Lebanon
Received: 15 February 2021; Accepted: 24 February 2021; Published: 10 March 2021
Citation: Battoul Fakhry, Mostafa Abdulrahim, Mirna N Chahine. Medical Cannabis in Lebanon: History & Therapeutic, Ethical, and Social Challenges. A Narrative Review. Archives of Clinical and Biomedical Research 5 (2021): 137-157.
Share at FacebookAbstract
Legalizing cannabis for both medical and recreational purposes is currently a worldwide trend. Lebanon, a Middle Eastern country, recently became the first Arabic state to legalize the cultivation of medical and industrial cannabis amid a huge economic crisis and the COVID 19 pandemic. However, the state of the art regarding the Lebanese cannabis is still poorly defined. Hence, our aim is to highlight medical and social concerns, and to clearly define the ethical framework for medical cannabis prescription and usage. Studies showed cannabis therapeutic potentials in treating numerous diseases such as epilepsy (high level of evidence), multiple sclerosis (moderate level of evidence), PTSD (low level of evidence), as well as in alleviating symptoms related to other conditions, for instance weight loss in HIV patients and chemotherapy induced nausea and vomiting (high level of evidence in both cases). Nonetheless, legalizing a drug known worldwide for its abuse potential could hinder several ethical principles. Whenever prescribing medical cannabis, the physician should respect patient’s autonomy, assess the risk benefit ratio of his actions, and act by justice. Moreover, authorizing cannabis usage for medical purposes could give rise to stigmatization, and further increase the burden on a society already struggling with the issues of self-medication, unemployment, and drugs diversion phenomena. By legalizing medical cannabis, Lebanon has entered a new chapter that warrants assessments, regulations, and readiness in order to insure a safe and successful experience.
Keywords
Medical Cannabis, Ethics, Public Health, Lebanon
Medical Cannabis articles; Ethics articles; Public Health articles; Lebanon articles
Article Details
Abbreviations:
2-AG: 2-arachidonyl glycerol; ADHD: Attention deficit hyperactivity disorder; CB: Cannabinoid Receptor; CB1: Cannabinoid Receptor type 1; CB2: Cannabinoid Receptor type 2; CBD: Cannabidiol; FDA: Food and Drug Administration; GAD: Generalized Anxiety disorder; HIV: Human Immunodeficiency Virus; MC: Medical Cannabis; PTSD: Post-traumatic stress disorder; SUD: Sub-stance Use Disorder; THC: Tetrahydrocannabinol; UNODC: United Nations Office of Drugs and Crime; UN: United Nations; WHO: World Health Organization
1. Introduction
For thousands upon thousands of years, cannabis was being cultivated due to its interesting properties and used by Homo sapiens in many aspects [1, 2]. Food crops, fabric, and papers were the earliest applications [3]. Cannabis also held an important place in ancient Arabic medicine [3]. In 2018, the United States (US) Food and Drug Administration (FDA) approved the first cannabis-based medication, Epidiolex, for the treatment of epilepsy [4]. Moreover, the legalization of cannabis for medical use has been on the 21st century’s agenda of many countries. For instance, Germany, United Kingdom, Netherlands, Italy, and 33 North-American states have legalized cannabis for medicinal purposes [5-7]. In 2020, amid an economic hardship and COVID-19 pandemic, Lebanon joined these countries by legalizing cultivation of cannabis for medical and industrial applications [8]. However, legalizing cannabis will allow ‘‘physicians to recommend a substance whose abuse potential is well documented; but whose benefits are poorly characterized’’[9] thus, undermining several ethical principles [10]. Moreover, in a society where religious principles are highly valued, people of faith strongly object usage of cannabis as it is considered a substance that pollutes the body and the mind [11]. Furthermore, few studies have been performed to define a clear situation regarding the Lebanese cannabis [12-15]. The latter is still considered a national ethical dilemma, taboo subject in the society, and a huge burden on physicians and lawmakers. In light of the forgoing, we aimed in this review to establish the current situation of medical cannabis (MC) in Lebanon by drawing its history in Lebanon, summarizing recent evidence regarding its therapeutic usage, identifying ethical and social challenges facing its future medicinal practice and determining medical, ethical, and social factors influencing the patient-doctor relationship when prescribing or using cannabis medication.
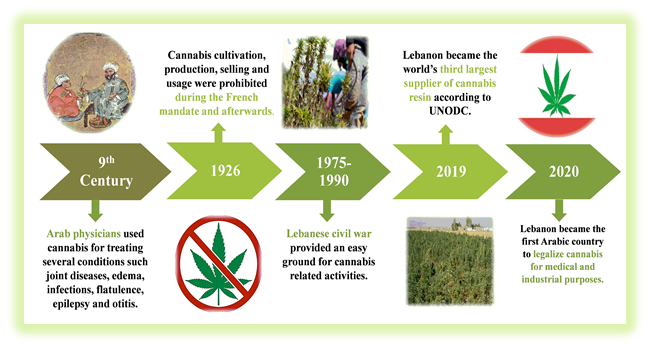
2. History of Cannabis in Lebanon
The earliest documented therapeutic application of Medical Cannabis (MC) in Arab medicine was in the 9th century when it was used to treat ear diseases. Later on, notable Arabic physicians discovered other therapeutic benefits for MC [16]. Ibn al-Baytar uncovered the anti-parasitic property of MC, Al-Razi mentioned the use of MC for skin diseases and Avicenna applied MC to heal joint diseases, ophthalmitis, edema, and wounds. Cannabis products were also prescribed for their diuretic, anti-epileptic, analgesic, and anti-inflammatory properties and administered to treat flatulence, infections and vomiting [3, 16]. However, the 20th century witnessed the downfall of this plant followed by international prohibition due to the emergence of new efficacious drugs and the spread of marijuana for recreational usage [17].
Lebanon, an Arabic country, had an official prohibition policy on all illicit drugs in 1926, during the era of the French mandate [18]. Regardless, between 1975 and 1990, marijuana market grew greatly because of the civil war [12]. In 1998, the Lebanese government issued the narcotic law that banned the cultivation, production, and usage of any illegal drug, including cannabis in all sorts and forms [19]. Despite being prohibited, cannabis was openly cultivated in Lebanon in an estimated area of 400 000 hectares, mainly in the Bekaa region with around 20 000 families involved in this illegal industry [20, 21]. Lebanese farmers also benefited from the Syrian conflict to increase their marijuana production, taking advantage of the open borders and lack of governmental surveillance [22]. In 2019, Lebanon which is well known worldwide for its high quality cannabis, was considered by the United Nations Office of Drugs and Crime (UNODC) as the world’s third largest supplier of cannabis resin [23]. Marijuana remained as well the most used substance after alcohol (12.3%) with a wide availability among youth [24]. On the 17th of October 2019, the subcommittee for cannabis cultivation released the draft law regarding cannabis legalization [25]. The main purposes were to enable the government to expand its authority on the cannabis industry by restricting its accessibility to medical and industrial purposes. In addition, it aimed to achieve a sustainable development and attempt to reduce the burden on the criminal justice system. Other reasons encompassed protecting public health, ensuring safety by imposing strict requirements, and raising awareness regarding health adverse event related to illegal cannabis use [25]. On the 21st of April 2020, amidst an economic crisis and Coronavirus pandemic, the draft bill regarding legalization of cannabis was approved by the Lebanese parliament. Thus, Lebanon became the first Arabic country to legalize cultivation of cannabis for medical and industrial purposes [26]. Remarkably, the cannabis consumption was not confronted in the new law, thus all cannabis related activities, except cultivation, are still prohibited. It should be underlined that cultivation was solely authorized for exportation and research purposes without decriminalizing local medicinal consumption. Figure 1 summarizes major events in the history of cannabis in Lebanon. Evidence is increasing regarding medical cannabis applications; however, its usage has been facing many medical, ethical, and social challenges following cannabis legalization.
UNODC: United Nations Office on Drug and Crimes
3. Medical Cannabis and Recent Evidence of its Usage
3.1 The endocannabinoid system
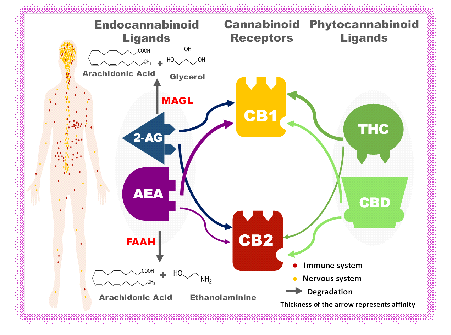
The endocannabinoid system is mainly composed of a Guanine nucleotide-binding protein (G-protein) coupled Cannabinoid receptors (CB), ligands, and metabolic enzymes [27-34] (Figure 2). This apparatus is involved in the regulation of the immune system, the nervous system (cognition, memory, emotion, coordination, sleep, appetite...), as well as the overall homeostasis of many organs including the skin, gut, liver, heart, bone, and testis [33-35]. As a matter of fact, the endocannabinoid system (enzymes, ligands and receptors) could be subject to alteration in many pathologies [31, 33, 34, 36].
Moreover, two exogenous CB ligands belonging to the phytocannabinoid category constitute the basis of Medical Cannabis (MC) preparations; Tetrahydro-cannabinol (THC) and Cannabidiol (CBD), the most studied cannabis components, account for the psychoactive and non-psychoactive phytocanna-binoid, respectively [6, 30]. THC is a partial agonist to endocannabinoid receptors with higher affinity to CB1 which could explain its intoxicating effect [30, 37, 38] (Figure 2). THC targets the dopaminergic pathway which can result in addiction and abuse potential [6, 27]. It also induces tolerance when chronically used [37]. In contrast, CBD has an allosteric action; it helps in enhancing the effect of the endogenous cannabinoid system instead of taking over this system, and as a result, CBD has no documented abuse or dependence potential [6, 30, 38] (Figure 2). CBD has many therapeutic benefits and is associated with safer outcomes than THC [6, 30, 39]. Notably, the potency of cannabis is defined by its THC/CBD ratio. In contrast to recreational marijuana, low THC/CBD ratio is found in MC [6].
3.2 Therapeutic applications of medical cannabis
Following the discovery of the Cannabinoid receptors (CB), a new epoch for cannabis began with a revived scientific curiosity [37]. Many studies and clinical trials highlighted the therapeutic benefits of MC. The latter was mainly used as an alternative in case conventional treatments failed to show any benefits. Moreover, studies showed the efficacy of MC in treating numerous diseases, as well as in alleviating symptoms related to other conditions. Tables 1, 2 and 3 summarize the major medical application of cannabis (psychiatric, neurological, and other medical applications such as insomnia, nausea and vomiting, chronic pain, weight loss in HIV patients, COVID-19) [37-68]. All studies agreed that further investigations were still needed to draw more clear and robust scientific evidence on the benefits of MC. Nonetheless, research on this topic is facing challenges on many levels. Ethically, the placebo issue and the recruitment of vulnerable demented population are barriers to clinical trials [69]. From a scientific perspective, past clinical trials are qualified of poor evidence due to many reasons particularly, ineffective blinding, and the choice of route of administration that should be suitable for the patient, the dosing, and the objective of the study [70, 71].
3.3 Route of administration of cannabis medications
As any other medication, cannabis active substances could reach their target system through different route of administration [47]. The most common mode among patients is by way of inhalation into the respiratory tract, either smoked or vaporized. This route induces the fastest onset and a short duration of action [30, 47, 72]. Nonetheless, the smoked form was associated with the highest pulmonary symptoms, thus, should be avoided in asthma and COPD patients [47]. One of the advantages favoring the oil-based medication is the fact that cannabis concentration could be well controlled, unlike the smoked form, thus minimizing undesirable effect [73]. Furthermore, the oromucosal, transdermal, and rectal routes by the mean of capsules, edibles, tea, oils, sprays, topicals, and suppositories represent an alternative discrete doorway for MC [47, 72, 74].
3.4 Adverse events of medical cannabis
Practitioners prescribing MC could encounter many cannabis related side effects. General adverse events such as allergy, ataxia, blurred vision, nausea, vomiting, headache, diarrhea, hypotension, somnolence, sedation, lethargy, hallucination, psychosis, vertigo, dizziness, dry mouth, and asthenia are described in many studies [37, 47, 75, 76]. It has been proven that chronic use of MC might impair cognition and lead to substance use disorder (SUD) with higher risk when administered to children and teenagers [37, 51, 76]. In addition, studies demonstrated that short term use of MC in children and young adult caused seizure exacerbation or status epilepticus [51]. In the same context, researches showed that MC used for treating anorexic HIV patients aggravated their weight loss [75]. Furthermore, accidental overdosing leads to sympathomimetic toxidrome and sudden abstention induces withdrawal syndrome [76]. Besides, medication toxicity due to drug interaction with cannabis is witnessed in patients under rifampicin, ketoconazole, warfarin, omeprazole, fentanyl, antivirals, anticonvulsants, and chemotherapeutic agents [76]. It was also reported that Cannabidiol (CBD) causes an increase in hepatic enzymes leading to drug discontinuation. This implies that special considerations should be taken in patients with hepatic impairment, or under medications with hepatotoxic effect [75]. Caution should be adopted when prescribing MC for patient with history of SUD, psychiatric conditions or under psychiatric medications [76].
3.5 Medical community attitude regarding medical cannabis
Although medical cannabis usage is still prohibited in Lebanon, the medical community attitude and beliefs regarding the therapeutic values of cannabis should not be disregarded since they are considered the gatekeeper for the use of MC [77, 78] Farhat et al [13] revealed that 75% of 12 different Lebanese physicians specialists (oncologists, neurologists, anesthesiologists, and psychiatrists) were in favor of MC legalization. Furthermore, the majority concurred on the potential benefits of MC as a supportive care medicine. Nonetheless, only 60% of these health care providers expressed their keenness to include MC in their practice [13]. Besides, the Lebanese psychiatric society statement acknowledged the potential therapeutic benefits of MC along with its economic welfare. They emphasized on the need to conduct extensive researches in order to assess the impact of such legalization on the affected parties, and the importance of a scientific debate on this matter [79]. A survey conducted to assess the knowledge and attitude among Lebanese pharmacists toward MC legalization showed that 45.5% of participants favored this legalization. However, 57.9% expressed their concerns about the abuse potential of this drug. Furthermore, this study revealed that only 35.6% of participants had answered correctly to more than half of the questions regarding MC knowledge. Therefore, many Lebanese pharmacists revealed the necessity for training programs to improve their knowledge on this matter [14].
Outside Lebanon, studies showed that the likelihood of prescribing MC varies depending on the medical specialties and sometimes even in the same discipline [80, 81]. Doctors, who were reluctant or completely opposed to MC prescription, reported several concerns: the lack of enough evidence, standardized guidelines, absence of cannabis subject from the medical school curriculum, potentials risks, harm as well as practitioners ambiguous responsibility [37, 82, 83]. Moreover, hesitancy out of fear of associating their name with cannabis was another obstacle [84]. This attitude was further influenced by some institutional policies that might forbid providing cannabinoid based medicine, in addition to news and social media who portray cannabis as an evil weed [85]. Some view the word cannabis and medicine ‘‘as an uneasy combination’’ and too potent to be denoted as a herbal medication [86].
Cannabinoid receptor CB1 is copiously expressed in the nervous system (central and enteric) particularly in presynaptic terminal neuron of the mesocorticolimbic dopaminergic pathway which regulates emotions, cognition and memory.(27–30) On the other hand, CB2 is expressed mainly in the immune system and lack psychotropic effects.(27,30–32) Two lipophilic endocannabinoid ligands exist: anandamide (AEA), a partial agonist with higher affinity to CB1 and 2-arachidonyl glycerol (2-AG) a full agonist with affinity for both CB1 and CB2 receptors.(27,33) AEA is biosynthesized by N-acylphosphatidylethanolamine-hydrolyzing phospholipase D (NAPE-PLD) and degraded by fatty acid amide hydrolase (FAAH). Whereas, 2-AG is formed by diacylglycerol (DAG) lipase and destroyed by monoacylglycerol lipase (MAGL).(31,33,34) As for phytocannabinoid ligands, Tetrahydrocannabinol (THC) and Cannabidiol (CBD) exhibit respectively a partial agonist and an allosteric activity on both cannabinoid receptors. 2-AG, 2-arachidonoylglycerol; AEA, N-arachidonoylethanolamine; Anandamide; CB1/CB2, type 1 and type 2 cannabinoid receptors;CBD, Cannabidiol; FAAH, fatty acid amide hydrolase; MAGL, Monoacylglycerol lipase; THC, tetrahydrocannabinol .
1PTSD: Post traumatic stress disorder
2ADHD: Attention deficit hyperactivity disorder
3GAD: Generalized anxiety disorder
Table 1: Summary of medical marijuana outcomes on psychiatric disorders.
1FDA: Food and Drug Administration
Table 2: Summary of medical marijuana outcomes on neurological conditions.
1FDA: Food and Drug Administration
2HIV: Human Immunodeficiency Virus
Table 3: Summary of medical marijuana outcomes on miscellaneous diseases.
4. Defining the Ethical Framework for Medical Cannabis Prescription
It is of great importance to define the ethical framework for MC prescription which is still considered a dilemma since, although its application could follow the 4 basics ethical principles, it might jeopardize them as well [87].
According to the principle of autonomy, MC should not be eliminated as a therapeutic option, since what is perceived as good by a competent patient might differ from a physician’s perspective. Moreover, according to the same fundament, a patient’s right to decide on his treatment should always be honored [88]. However, this principle might not apply in certain situations: 1) When the patient is considered vulnerable and incompetent due to his condition and age; 2) when the mean of administration of a drug could inflict a potential harm for the patient’s surroundings [87]. Therefore, the physician is strongly advised to adopt the shared decision making process as the patient becomes involved in establishing his own treatment protocol by expressing his wishes and concerns, while the physician has the duty to teach and advise him [90].
According to Beneficence and non-maleficence, the physician responsibility when prescribing cannabis is to assess the Risk/Benefits ratio in every patient case [37, 89]. It has been proven that medical hashish has several benefits, especially when treating chronic diseases that impair patient’s quality of life, thus acting by beneficence would not deny them the advantage of standard comfort and health [89, 90]. Nonetheless, the physician should reconsider this approach when the cannabinoid drug could inflict serious adverse effects, for example the possible damage that could follow MC administration, is either due to the substance itself (neurotoxicity) or to the route of delivery such as inhalation which affects the respiratory system [70, 91]. Furthermore, when the practitioner abstains from prescribing MC in a particular condition where the patient pain and suffer are refractory to conventional medications, is equivalent to harm [87]. Hence, in a complex situation where the attempt to heal a patient could lead to a potential damage, does acting by beneficence outweigh the likely mischief?
The principle of Justice where by every patient has the right to healthcare access regardless of his ethnicity, religion, sex, economic status, and background. Moreover, justice refers to fairness when it comes to sharing the burden and benefits of every medical act [92]. Since MC is still under trials for some diseases, physicians should avoid exploiting vulnerable patients (elderly, terminally ill, low socio economical classes, prisoners, minorities, children, pregnant women…) by offering this drug to obtain clinical results. On the other hand, the benefits of well documented FDA approved MC should be granted to all patients in need [93]. For instance, studies showed that vulnerable population, such as HIV patients, children with epilepsy resistant to treatment and other chronic conditions, face many difficulties when it comes to MC access due to: high prices, lack of insurance reimbursement, confusing, complicated application process, and the requirement of yearly renewal [94, 95]. Similarly, physicians and health care providers could be subject to injustice. Even though they might benefit from MC for treating their chronic back pain, burn out syndrome, and even Post-traumatic stress disorder (PTSD) as a result of long work hours in stressful conditions, MC is rarely justifiable as a cure option for health professionals owing to stringent regulations. Hence, there is a need to “equalize the access to treatment rather than discriminate’’ [96]. Therefore, ethics should always prevail when prescribing any medication, particularly cannabis-based medicines. Ethical principles should triumph over legality as what is considered legal is not always ethical and vice versa [97]. For instance, a physician would be ethically plausible to recommend MC for conditions where scientific evidences favor its usage regardless of its juridical status. Conversely, even if MC prescription is considered lawful, but the scientific evidences are still ill-defined, physicians “should not accept legality as the ethical foundation for recommending cannabis” [89].
5. Social Challenges Facing Medical Cannabis
After legalizing MC, the Lebanese society will face many challenges that other countries already confronted: mainly stigma, diversion phenomena, as well as consequences on employment, repercussions of self-medications and religious conflicts.
First, stigma phenomena, present on different levels, is due to a lack of awareness on the potential benefits of MC. Patients on MC are considered by their surroundings as drug addicts who exploit the law [98]. Society is still struggling to acknowledge cannabis as a treatment; they rather portray it as a medicine in a joint [99]. Stigmatization is the crucial reason behind patients retreating from their therapy despite experiencing welfare [98]. The fear of being stigmatized by their physicians as well, pushed MC users to resort to MC clinics rather than their healthcare providers, in order to gain access to their medication [98]. This emphasizes on the importance of campaign awareness that should not only cover recreational cannabis topic but also will tend to educate society to welcome the culture of MC. Furthermore, self-stigmatization is also observed among MC patients hiding their medical treatment in fear of being stigmatized by their family and friends. Satterlund et al [98] reported that patients under MC were skeptical about this cannabis-based drug, as they did not consider it as a relevant treatment initially. They even saw MC legalization as a mean for drug addict to get more weed [98]. Here comes the role of the physician as an informant to increase the knowledge of his patients on MC with evidence-based arguments. Therefore, boosting their confidence and encouraging these individuals to be open about their medication to their close surrounding [96, 100].
Second, many jobs impose regular drug testing even prior to enrollment. In fact, Schuster et al [101] demonstrated that cannabis could be detected in a urine specimen even after one month of abstinence. Since the majority of MC patients are subject to long-term therapy, this might jeopardize their employment, either by terminating their work career or being rejected from a possible job opportunity. Even sometimes, their MC card cannot save their place [102]. In addition, it can decrease job performance, render the worker prone to unemployment and expose the public to danger if the patient under influence has a safety sensitive job [37]. This is why it is crucial to reform job policies regarding this issue [96].
Third, the cannabis diversion phenomenon constitutes another challenge facing MC whereby individuals with recreational motives might gain access to their desired drug through MC card holders or prescriptions [86, 88]. This could also occur by MC patients selling and sharing their prescribed drugs. In addition, unattended storage of prescribed MC further facilitates acquiring this drug particularly by minors accidentally or on purpose [103, 104]. Fearing an opioid style crisis, it is of great need to tightly control MC prescriptions in order to avoid diversion and to ensure public safety [71, 88].
Fourth, self-medication represents a major concern regarding patient’s safety. A study showed that in the Middle East the misuse of drugs was prevalent among patients for both prescription-only and over-the-counter medicines [105]. Moreover, Awada et al showed that this practice is common among the Lebanese population. Therefore, self-medication constitutes a significant challenge to stakeholders such as lawmakers, physicians, and pharmacists. They should prioritize first solving this issue prior to further exposing the community to a drug known to have a high abuse potential [106]. Furthermore, self-medication with cannabis could put the person safety at risk due to a range of associated adverse. Bursani et al described self-medication as a substance abuse trend that merits surveillance and more exploration [105].
Fifth, Lebanon is distinguished by its diverse religious communities, with Islam and Christianity being the 2 leading religions [107]. Lebanese highly value their beliefs; Religions are integrated in their social life and influence their decision making [108]. Regarding Islam, the permissibility of MC is still a debate given the lack of a clear statement which prohibits the use of hashish in the Koran. However, it is safe to say that Islam prohibits the use of any substance that could potentially intoxicate the body and the mind. Nevertheless, certain conditions described as ‘‘necessity’’/ “darurah’’ where patient life is at stake, forbidden substances can be allowed if they could: save the patient’s life, with minimal harm, when safer alternatives are not available [109]. Christianity permits the medical use of cannabis for the same reasons mentioned above mainly when conventional medications have failed [110]. In addition, as stated in the Bible: “let every soul be subject unto the higher powers, for there is no authority except that which God has established.’’ (Roman 13:1), hence, every Christian should follow the law and regulations of his society becausethey are"established by God". In a recent Lebanese study, religious representatives of the different sects of the Lebanese community were interviewed, 71% encouraged MC legalization and 29% showed their concern regarding this matter [13].
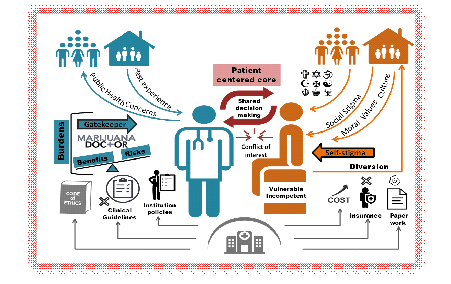
6. Medical, Ethical, and Social Factors Influencing Medical Cannabis Usage and Prescription
When prescribing MC, the physician, as the gatekeeper of such substance, faces many burdens (Figure 3). In addition to being called a Marijuana Doctor and having possibly past family experience with cannabis dependence, he/she is also in charge of calculating the Risk/Benefit ratio of this action for each patient requiring MC [37]. Lack of unified clinical guidelines, ethical dilemmas, and institutional policies are other factors originating from the healthcare system and that might render the doctor hesitant in such cases [85]. Furthermore, this century is highlighted by the patient centered care; hence, a shared decision between the physician and the patient preceded by a righteous informed consent should take place. But, when dealing with MC prescription, conflict of interest could arise from patients with illicit use intent and physicians who tend to exploit their patients for research or industrial purposes [86, 111]. Regarding the patient, vulnerability (being a fetus, child, pregnant woman, elderly or incompetent), and self-stigma are major elements that affect the final judgment as well [47, 112]. The healthcare system also burdens the patient with difficult paper work, increased cost and lack of insurance [47]. While doctors’ prescriptions raise public health concerns, diversion phenomena can be another problem arising from the side of the patient [113]. Nonetheless, the society with its moral, values, culture, religions, and stigma can shape the decision of the patient [114]. In short, the physician-patient relationship, in case of MC prescription, should not be restricted to a provider-client business contract rather than a correspondence of care with proper follow-up while embracing all determinant of this communication and acknowledging the human person within the patient. Factors affecting the patient doctor relationship are summarized in Figure 3.
Factors represented in this figure are written in bold within section 6 of the text.
7. Conclusion
In conclusion, the subject of cannabis remains controversial in every aspect: medical, ethical and social. Table 4 summarizes major findings of this review. Recent studies showed the efficacy of MC in treating several diseases with promising results for other conditions. On the other hand, it was also associated with adverse effects, ethical and social challenges, and public health concerns. Hence, physicians could face difficulties and hesitate when prescribing MC, whereas patients might develop insecurities related to MC usage and request and the society could confront social issues. Regarding Lebanon, cultivation of cannabis for industrial and medical purposes is solely legalized; consumption even with medical prescription is still prohibited. The position of the Lebanese medical and religious communities as well as the society is still not clear and merits further investigation. Moreover, it is of critical need to evaluate the aftermath of MC legalization and benefit from other countries’ experience. Additional research could study as well the Lebanese cannabis strain and its therapeutic applications. In the end, the most interesting questions to ask is how can we preserve the values of our society and protect the concept of the human person amid this medicinal cannabis era?. Based on other countries’ experience, it seems that legalization cannabis for medical and industrial purposes is one-step before cannabis decriminalization. So, is Lebanon on the path of legalizing cannabis for recreational usage.
|
Medical Cannabis in Lebanon: History & Therapeutic, Ethical, and Social Challenges. A Narrative Review |
|
|
History of cannabis in Lebanon |
• Since antiquity, Arabs used medical cannabis to treat several conditions such as gout, edema, infections, flatulence and otitis. • Despite the fact that cannabis was prohibited in Lebanon in the past century, it was openly cultivated and frequently used for recreational purposes mainly among youth. • In 2020, Lebanon became the first Arabic country to legalize cannabis for industrial and medicinal purposes. |
|
Medical cannabis |
• The endocannabinoid system (enzymes, ligands and receptors) could be subject to alteration in many pathologies. • Studies showed the efficacy of medical cannabis in treating numerous diseases mainly epilepsy and chronic pain, as well as in alleviating symptoms related to other conditions such as chemotherapy induced nausea and vomiting and weight loss in HIV patients. • Cannabis medications have several route of administration with smoking being the most frequently used mean of application. However, it presents many disadvantages. • Caution should be adopted when prescribing medical cannabis and patients should be properly followed-up because of possible adverse events. |
|
Ethical challenges |
• Cannabis prescription and usage raise ethical dilemmas. • Principle of autonomy should always guide the doctor while prescribing medical cannabis, unless the patient is vulnerable, incompetent or when medical cannabis usage might inflict harm to others. • In every case of medical marijuana request or prescription, the physician should draw the risk and benefit ratio of such act. • Principle of justice refers to fairness when it comes to sharing the burden and benefits of medical cannabis use. |
|
Social challenges |
• Medical cannabis usage can generate several social problems such as stigma, unemployment and diversion phenomena. • Self –medication is frequent in Lebanon and risks exposing the community to a drug with high abuse potentials. • No clear statement that prohibits the use of cannabis for medical purposes in Christianity and Islam. |
Table 4: Key findings regarding the history of cannabis in Lebanon, recent evidence regarding medical cannabis, ethical, and social challenges facing its legalization.
Competing Interests
The authors declare that they have no competing interests.
Funding
The authors received no funding for this work
Author’s Contributions
BF and MA contributed equally in the literature review and the writing of the manuscript with input of MNC who was in charge of supervising the work. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to acknowledge Prof. Fadi Abou Mrad for his expert advices in addressing the subject of MC as well as the laboratory of medical ethics in the Lebanese University for its exceptional mentorship.
References
- Russo EB. Beyond Cannabis: Plants and the Endocannabinoid System. Trends Pharmacol Sci [Internet] 37 (2016): 594-605.
- Bridgeman MB, Abazia DT. Medicinal Cannabis: History, Pharmacology, And Implications for the Acute Care Setting. P T 42 (2017): 180-188.
- Pisanti S, Bifulco M. Medical Cannabis: A plurimillennial history of an evergreen. J Cell Physiol 234 (2019): 8342-8351.
- Billakota S, Devinsky O, Marsh E. Cannabinoid therapy in epilepsy. Curr Opin Neurol 32 (2019): 220-226.
- Schlag A K. An Evaluation of Regulatory Regimes of Medical Cannabis: What Lessons Can Be Learned for the UK?. Med Cannabis Cannabinoids 3 (2020): 76-83.
- Papaseit E, Pérez-Mañá C, Pérez-Acevedo AP, et al. Cannabinoids: from pot to lab. Int J Med Sci Aug 15 (2018): 1286-1295.
- Chouvy P-A. Cannabis cultivation in the world: heritages, trends and challenges [Internet]. EcoGeo (2019): 48.
- The license to grow the hemp plant for medical and industrial use [Internet] (2020).
- Nussbaum AM, Boyer JA, Kondrad EC. “But my doctor recommended pot”: medical marijuana and the patient-physician relationship. J Gen Intern Med 26 (2011): 1364-1367.
- Sagy I, Peleg-Sagy T, Barski L, et al. Ethical issues in medical cannabis use. Eur J Intern Med 49 (2018): 20-22.
- Badr LK, Taha A, Dee V. Substance abuse In Middle Eastern adolescents living in two different countries: spiritual, cultural, family and personal factors. J Relig Health 53 (2014): 1060-1074.
- Nadeen Hilal, Lama Bou-Karroum, Noor Ataya FEJ. K2P Rapid Response: LegalizingCannabis Cultivation: What we need to know& is Lebanon Ready?. Beirut, Lebanon (2018).
- Farhat A, Elhaj A, Abou Haidar M, et al. Guidelines and implementation strategy for the use of cannabis (lebanon). International Journal of Current Research 12 (2020): 10043-10048.
- Jaffal LH, Lahoud N, Zein S, et al. Lebanese Pharmacists’ Knowledge and Attitude toward Cannabis Medical Use Legality. Dr. Sulaiman Al Habib Medical Journal 2 (2020): 106-114.
- Aaraj RA. Lebanon’s green plans: Exploring the contribution of cannabis legalisation to sustainable rural development in Lebanon (Master’s thesis) (2020).
- Lozano I. The therapeutic use of Cannabis sativa (L.) in Arabic medicine. Journal of Cannabis Therapeutics 1 (2001): 63-70.
- Pisanti S, Bifulco M. Modern History of Medical Cannabis: From Widespread Use to Prohibitionism and Back. Trends Pharmacol Sci 38 (2017): 195-198.
- Report on the situation of Lebanon and Syria-National Printing Press France (1925).
- Law No. 673 of 1998 on Narcotics, Psychotropic Substances and Precursors as Amended by Law No. 77 of (1999).
- Afsahi K, Darwich S. Hashish in Morocco and Lebanon: A comparative study. Int J Drug Policy 31 (2016): 190-198.
- Ministry of Public Health (MOPH). 2017 National Report on Drug Situation in Lebanon. Beirut: Lebanon (2017).
- Ghiabi M. Deconstructing the Islamic bloc: The Middle East and North Africa and pluralistic drugs policy. InCollapse of the Global Order on Drugs: From UNGASS 2016 to Review 2019 (2018).
- World Drug Report 2019 (United Nations publication, Sales No. E.19.XI.8) (2019).
- Salameh P, Rachidi S, Al-Hajje A, et al. Substance use among Lebanese university students: prevalence and associated factors. East Mediterr Health J 21 (2015): 332-341.
- Draft law on regulation of cannabis cultivation for medical use.Lebanon (2019).
- The license to grow the hemp plant for medical and industrial use (2020).
- Scherma M, Masia P, Satta V, et al. Brain activity of anandamide: a rewarding bliss?. Acta Pharmacol Sin 40 (2019): 309-323.
- Maccarrone M, Guzmán M, Mackie K, et al. Programming of neural cells by (endo) cannabinoids: from physiological rules to emerging therapies. Nat Rev Neurosci 15 (2014): 786-801.
- Mlost J, Wasik A, Starowicz K. Role of endocannabinoid system in dopamine signalling within the reward circuits affected by chronic pain. Pharmacol Res 143 (2019): 40-47.
- World Health Organization. CANNABIDIOL (CBD) Critical Review Report Expert Committee on Drug Dependence Fortieth Meeting. Expert Committee on Drug DependenceFortieth Meeting (2018).
- Sharkey KA, Wiley JW. The Role of the Endocannabinoid System in the Brain-Gut Axis. Gastroenterology 151 (2016): 252-266.
- Oddi S, Scipioni L, Maccarrone M. Endocannabinoid system and adult neurogenesis: a focused review. Curr Opin Pharmacol 50 (2020): 25-32.
- Hourani W, Alexander SPH. Cannabinoid ligands, receptors and enzymes: Pharmacological tools and therapeutic potential. Brain Neurosci Adv (2018).
- Chanda D, Neumann D, Glatz JFC. The endocannabinoid system: Overview of an emerging multi-faceted therapeutic target. Prostaglandins Leukot Essent Fatty Acids 140 (2019): 51-56.
- Haugh O, Penman J, Irving AJ, et al. The Emerging Role of the Cannabinoid Receptor Family in Peripheral and Neuro-immune Interactions. Curr Drug Targets 17 (2016): 1834-1840.
- Murillo-Rodriguez E, Pastrana-Trejo JC, Salas-Crisóstomo M, et al. The Endocanna-binoid System Modulating Levels of Consciousness, Emotions and Likely Dream Contents. CNS Neurol Disord Drug Targets 16(2017): 370-379.
- Schrot RJ, Hubbard JR. Cannabinoids: Medical implications. Ann Med 48 (2016): 128-141.
- Ebbert JO, Scharf EL, Hurt RT. Medical Cannabis. Mayo Clin Proc 93 (2018): 1842-1847.
- Englund A, Freeman TP, Murray RM, et al. Can we make cannabis safer?. Lancet Psychiatry 4 (2017): 643-648.
- Sarris J, Sinclair J, Karamacoska D, et al. Medicinal cannabis for psychiatric disorders: a clinically-focused systematic review. BMC Psychiatry 20 (2020): 24.
- Khan R, Naveed S, Mian N, et al. The therapeutic role of Cannabidiol in mental health: a systematic review. J Cannabis Res 2 (2020): 2.
- Stetten N, Pomeranz J, Moorhouse M, et al. The level of evidence of medical marijuana use for treating disabilities: a scoping review. Disabil Rehabil 42 (2020): 1190-1201.
- Turna J, Patterson B, Van Ameringen M. Is cannabis treatment for anxiety, mood, and related disorders ready for prime time?. Depress Anxiety 34 (2017): 1006-1017.
- Jetly R, Heber A, Fraser G BD. The efficacy of nabilone, a synthetic cannabinoid, in the treatment of PTSD-associated nightmares: A preliminary randomized, double-blind, placebo-controlled cross-over design study. Psychoneuroendocrinology 51 (2015): 585-588.
- Black N, Stockings E, Campbell G, et al. Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis. Lancet Psychiatry 6 (2019): 995-1010.
- Hupli A M M. Medical Cannabis for Adult Attention Deficit Hyperactivity Disorder: Sociological Patient Case Report of Cannabinoid Therapeutics in Finland. Med Cannabis Cannabinoids 1 (2018): 112-118.
- MacCallum CA, Russo EB. Practical considerations in medical cannabis administration and dosing. Eur J Intern Med 49 (2018): 12-19.
- Schoevers J, Leweke JE, Leweke FM. Cannabidiol as a treatment option for schizophrenia: recent evidence and current studies. Curr Opin Psychiatry 33 (2020): 185-191.
- McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an Adjunctive Therapy in Schizophrenia: A Multicenter Randomized Controlled Trial. Am J Psychiatry 175 (2018): 225-231.
- Fiani B, Sarhadi KJ, Soula M, et al. Current application of cannabidiol (CBD) in the management and treatment of neurological disorders. Neurol Sci 41 (2020): 3085-3098.
- Friedman D, French JA, Maccarrone M. Safety, efficacy, and mechanisms of action of cannabinoids in neurological disorders. Lancet Neurol 18 (2019): 504-512.
- Tapley P, Kellett S. Cannabis-based medicines and the perioperative physician. Perioper Med (Lond) 8 (2019): 19.
- Rubin R. The Path to the First FDA-Approved Cannabis-Derived Treatment and What Comes Next. JAMA 320 (2018): 1227-1229.
- Mohanty D, Lippmann S. Marijuana for Parkinson’s Disease?. Innov Clin Neurosci 16 (2019): 33-34.
- Banerjee S, McCormack S. Medical Cannabis for the Treatment of Chronic Pain: A Review of Clinical Effectiveness and Guidelines [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health (2019).
- Maharajan MK, Yong YJ, Yip HY, et al. Medical cannabis for chronic pain: can it make a difference in pain management?. J Anesth 34 (2020): 95-103.
- Krishnan S, Cairns R, Howard R. Cannabinoids for the treatment of dementia. Cochrane Database Syst Rev 2009 (2009): CD007204.
- Talarico G, Trebbastoni A, Bruno G, et al. Modulation of the Cannabinoid System: A New Perspective for the Treatment of the Alzheimer’s Disease. Curr Neuropharmacol 17 (2019): 176-183.
- Peprah K, McCormack S. Medical Cannabis for the Treatment of Dementia: A Review of Clinical Effectiveness and Guidelines [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health (2019).
- van den Elsen GA, Ahmed AI, Verkes RJ, et al. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia: A randomized controlled trial. Neurology 84 (2015): 2338-2346.
- Weier M, Hall W. The Use of Cannabinoids in Treating Dementia. Curr Neurol Neurosci Rep 17 (2017): 56.
- Lim K, See YM LJA. Systematic Review of the Effectiveness of Medical Cannabis for Psychiatric, Movement and Neurodegenerative Disorders. Clin Psychopharmacol Neurosci 15 (2017): 301-312.
- Shelef A, Barak Y, Berger U, et al. Safety and Efficacy of Medical Cannabis Oil for Behavioral and Psychological Symptoms of Dementia: An-Open Label, Add-On, Pilot Study. J Alzheimers Dis 51 (2016): 15-19.
- Braithwaite I, Bhagavan C, Doppen M, et al. Medicinal applications of cannabis/ canna-binoids. Curr Opin Psychol 38 (2020): 1-10.
- Zelira Therapeutics Ltd . Zelira Therapeutics Completes World’s First Clinical Trials for Treatment of Insomnia with Medical Cannabis (2020).
- Mortimer TL, Mabin T, Engelbrecht AM. Cannabinoids: the lows and the highs of chemotherapy-induced nausea and vomiting. Future Oncol 15 (2019): 1035-1049.
- Kramer JL. Medical marijuana for cancer. CA Cancer J Clin 65 (2015): 109-122.
- Hill KP. Cannabinoids and the Coronavirus. Cannabis Cannabinoid Res 5 (2020): 118-120.
- Abou-Mrad F, Tarabey L. Attitudes Toward Placebo Use in Lebanon. Clin Ther 37 (2015): 1138-1145.
- Casarett D. The Achilles Heel of Medical Cannabis Research-Inadequate Blinding of Placebo-Controlled Trials. JAMA Intern Med 178 (2018): 9-10.
- Reiman A, Aggarwal SK, Reinarman C. Medicalization of marijuana. JAMA 312 (2014): 1931.
- Russell C, Rueda S, Room R, et al. Routes of administration for cannabis use - basic prevalence and related health outcomes: A scoping review and synthesis. Int J Drug Policy 52 (2018): 87-96.
- Solymosi K, Köfalvi A. Cannabis: A Treasure Trove or Pandora’s Box?. Mini Rev Med Chem 17 (2017): 1223-1291.
- Costantino RC, Felten N, Todd M, et al. A Survey of Hospice Professionals Regarding Medical Cannabis Practices. J Palliat Med 22 (2019): 1208-1212.
- Brown JD, Winterstein AG. Potential Adverse Drug Events and Drug-Drug Interactions with Medical and Consumer Cannabidiol (CBD) Use. J Clin Med 8 (2019): 989.
- Brunetti P, Pichini S, Pacifici R, et al. Herbal Preparations of Medical Cannabis: A Vademecum for Prescribing Doctors. Medicina (Kaunas) 56 (2020): 237.
- Eggertson L. Marijuana strains doctor-patient relationship. CMAJ 186 (2014): E511-E512.
- Thompson JW Jr, Koenen MA. Physicians as gatekeepers in the use of medical marijuana. J Am Acad Psychiatry Law 39 (2011): 460-464.
- Official Statement by the Lebanese Psychiatric Society on the legalization of cannabis in Lebanon (2020).
- Charuvastra A, Friedmann PD, Stein MD. Physician attitudes regarding the prescription of medical marijuana. J Addict Dis 24 (2005): 87-93.
- Sharon H, Goldway N, Goor-Aryeh I, et al. Personal experience and attitudes of pain medicine specialists in Israel regarding the medical use of cannabis for chronic pain. J Pain Res 11 (2018): 1411-1419.
- Evanoff AB, Quan T, Dufault C, et al. Physicians-in-training are not prepared to prescribe medical marijuana. Drug Alcohol Depend 180 (2017): 151-155.
- Glauser W. Are medical schools keeping up with the times?. CMAJ 190 (2018): E996-E997.
- Michalec B, Rapp L, Whittle T. Assessing physicians’ perspectives and knowledge of medical marijuana and the Delaware Medical Marijuana Act. The Journal of Global Drug Policy and Practice 9 (2015): 1-24.
- Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med 26 (2013): 52-60.
- Bersani FS, Santacroce R, Coviello M, et al. Cannabis: a self-medication drug for weight management? The never ending story. Drug Test Anal 8 (2016): 177-179.
- Sally Bean JD. Medical cannabis: identifying ethical and policy implications for healthcare organizations in Canada. J Pain Manag 9 (2016): 473
- Stevens A. Medical cannabis in the UK. BMJ 363 (2018): k4844.
- Glickman A, Sisti D. Prescribing medical cannabis: ethical considerations for primary care providers. J Med Ethics 46 (2020): 227-230.
- Zhang H, Xie M, Archibald SD, et al. Association of Marijuana Use With Psychosocial and Quality of Life Outcomes Among Patients With Head and Neck Cancer. JAMA Otolaryngol Head Neck Surg 144 (2018): 1017-1022.
- Mechoulam R, Parker LA. The endocannabinoid system and the brain. Annu Rev Psychol 64 (2013): 21-47.
- Sims JM. A brief review of the Belmont report. Dimens Crit Care Nurs 29 (2010): 173-174.
- Dauda B, Denier Y, Dierickx K. What Do the Various Principles of Justice Mean Within the Concept of Benefit Sharing? J Bioeth Inq 13 (2016): 281-293.
- Elliott J, DeJean D, Potter BK, et al. Barriers in accessing medical cannabis for children with drug-resistant epilepsy in Canada: A qualitative study. Epilepsy Behav [Internet] 111 (2020): 107-120.
- Belle-Isle L, Hathaway A. Barriers to access to medical cannabis for Canadians living with HIV/AIDS. AIDS care 19 (2007): 500-506.
- Mazzarisi EL, Swartzwelder K, Clements PT. Marijuana for medical use: Implications for health care providers. Journal of Inter-profess-ional Education & Practice (2020).
- Riddick FA Jr. The code of medical ethics of the american medical association. Ochsner J 5 (2003): 6-10.
- Satterlund TD, Lee JP, Moore RS. Stigma among California’s Medical Marijuana Patients. J Psychoactive Drugs 47 (2015): 10-17.
- Bottorff JL, Bissell LJ, Balneaves LG, et al. Perceptions of cannabis as a stigmatized medicine: a qualitative descriptive study. Harm Reduct J 10 (2013): 2.
- Ko GD, Bober SL, Mindra S, et al. Medical cannabis - the Canadian perspective. J Pain Res 9 (2016): 735-744.
- Schuster RM, Potter K, Vandrey R, et al. Urinary 11-nor-9-carboxy-tetrahydrocanna-binol elimination in adolescent and young adult cannabis users during one month of sus-tained and biochemically verified abstinence. J Psychopharmacol 34 (2020): 197-210.
- Calvasina G. Human resource management policy and practice issues and medical marijuana. J Manag Mark Res 6 (2011): 1-8.
- Thurstone C, Lieberman SA, Schmiege SJ. Medical marijuana diversion and associated problems in adolescent substance treatment. Drug Alcohol Depend [Internet] 118 (2011): 489-492.
- Nussbaum AM, Thurstone C, McGarry L, et al. Use and diversion of medical marijuana among adults admitted to inpatient psychiatry. Am J Drug Alcohol Abuse 41 (2015): 166-172.
- Khalifeh MM, Moore ND, Salameh PR. Self-medication misuse in the Middle East: a systematic literature review. Pharmacol Res Perspect 5 (2017): e00323.
- Awada S, Diab B, Khachman D, et al. Self-medication Practices and Knowledge among Lebanese Population: A Cross-sectional Study. Dr Sulaiman Al Habib Med Journal 2 (2020): 56-64.
- Hager A. ‘Lebanon is more than a nation, more than a country. It is a message.’Lebanon as a model of Christian–Muslim relations. Journal of Beliefs & Values 38 (2017): 286-295.
- Al Ariss A. Religious diversity in Lebanon: lessons from a small country to the global world. Managing cultural diversity in Asia: A research companion (2010): 56-72.
- Ghiabi M, Maarefvand M, Bahari H, et al. Islam and cannabis: Legalisation and religious debate in Iran. Int J Drug Policy 56 (2018): 121-127.
- Leffel J. What about Medical Marijuana?. XENOS Christian Fellowship (2019).
- McCoy MS, Joffe S, Emanuel EJ. Sharing Patient Data Without Exploiting Patients. JAMA 323 (2020): 505-506.
- Aran A, Cayam-Rand D. Medical Cannabis in Children. Rambam Maimonides Med J 11 (2020): e0003.
- Zvonarev V, Fatuki TA, Tregubenko P. The Public Health Concerns of Marijuana Legalization: An Overview of Current Trends. Cureus 11 (2019): e5806.
- Vyshka G. The unlikely legalization of medical cannabis in Albania: a case study. J Med Ethics Hist Med 12 (2018): 10.