Management of Stroke in Public Teaching Hospitals, A Cross Sectional Study, Khartoum-Sudan, February 2021
Article Information
Ahmed Ali Eltayeb Elamin1, Ahmed Osman Ahmed Mohamed1*, Musaab DM Dafaalla1, Mohamed Anwer1, Mohamed Alebeed1, Elfatih A Hasabo1, Abdalla abbas adam massry1, Osman Taleballah2, Ihab B Abdalrahman3
1University of Khartoum, Faculty of Medicine, Khartoum, Sudan
2Alzaiem Alazhari University, Faculty of medicine, Khartoum, Sudan
3Consultant of Acute Care Medicine, Soba University Hospital, Professor of Medicine, University of Khartoum, Khartoum, Sudan
*Corresponding author: Ahmed Osman Ahmed Mohamed, University of Khartoum, Faculty of Medicine, Khartoum, Sudan
Received: 13 June 2022; Accepted: 24 June 2022; Published: 16 July 2022
Citation: Ahmed Ali Eltayeb Elamin, Ahmed Osman Ahmed Mohamed, Musaab DM Dafaalla, Mohamed Anwer, Mohamed Alebeed, Elfatih A Hasabo, Abdalla abbas adam massry, Osman Taleballah, Ihab B Abdalrahman. Management of Stroke in Public Teaching Hospitals, A Cross Sectional Study, Khartoum-Sudan, February 2021. Archives of Internal Medicine Research 5 (2022): 319-324.
Share at FacebookAbstract
Introduction: Stroke is considered a growing health issue with high burden.The study was conducted among 258 participants in Soba university hospital, Ibrahim Malik teaching hospital, and Bahri teaching hospital. The study aimed to compare the clinical practice of the management protocol to the NICE guidelines for stroke 2016, and to determine the level of appropriate reporting of stroke management in the medical records.
Materials and methods: Observational cross-sectional hospital-based study. Total coverage of stroke patients’ medical records in the period between February to March 2021. Data were coded, and analyzed by SPSS version 23.
Results: About two third of the participants had their blood pressure lowered within the primary management. The hospitals were 100% adherent to secondary prevention measures’ guidelines. However, Lower adherence was reported for the early hospital management (81.4%) and the primary management (83.8%). Furthermore, there was marked under-documentation of cases in both primary and secondary management with only ( 35.4%) and (20.8% ) of stroke patients were reported respectively.
Conclusion: Three-quarters of the participants received an emergency assessment by a specialist physician and were monitored closely. Moreover, The majority of the hemorrhagic stroke had their blood pressure lowered with minimum surgical intervention, this was explained by lack of adequate surgical infrastructure due to poor health finance in Sudan. Fortunately, high overall adherence rates to the stroke management guidelines were shown among different hospitals in this study. However, under-documentation of cases and their details was noticed.
Keywords
Hemorrhagic Stroke, Ischemic Stroke, NICE Guidelines, Reporting
Article Details
1. Introduction
Stroke is considered one of the leading worldwide causes of death, it is the second killer and the third leading cause of disability [1].Stroke is defined as a syndrome in which focal or global rapidly developing signs of cerebral dysfunction appear lasting more than 24 hours or leading to death [2]. It is caused by a lack of oxygenation in brain tissues due to either block in the blood supply or hemorrhage. It shares risk factors for coronary heart diseases such as hypertension, diabetes, and sedentary lifestyle [3]. Moreover, in Sudan sickle cell anemia is considered a major cause, especially among people and children [3].The incidence rate of stroke among third world countries has doubled during the last three decades. In 2019, a report depicted an upward pattern in the incidence of stroke [1], and it is expected that Africa to reach an incidence up to two to three folds higher than the incidence in western countries [1]. In addition, stroke health burden will lead to uncontrollable results if no interventions are taken, especially with the low-quality health services in Africa.
Regarding the situation in Sudan, there are no data about the incidence and prevalence of stroke among the general population. However, a previous study in Sudan reported an increased prevalence (2.6 times) of stroke among diabetes patients [4]. World Health Organization has published a report in 2017 showing mortality in Sudan due to stroke, which was found to be 27,222 (10.17% of the total deaths) [5]. Furthermore, a new multicenter study revealed a 30% death rate among stroke patients [4]. This rang alarms to investigate the reasons behind such a high number of deaths. According to the Royal College of Physicians [6], the management of stroke patients can be divided into three phases: acute care, recovery and rehabilitation care, and secondary prevention. Acute care is further divided into pre-hospital care and early hospital intervention. While suspected stroke patients are in an ambulance, some measures should be commenced; starting with screening tools such as face arm speech test (FAST), maintaining airways, and monitoring. The acute hospital management includes assessment of emergency management, imaging, administration of thrombolytic and antiplatelet in case of ischemic stroke, and monitoring of vital signs, oxygen saturation, and swallowing. The long-term hospital management consists ofthe assessment of treatments, referral to neurosurgery in case of unresolved hemorrhagic stroke, blood pressure-lowering, statins, as well as prevention against deep vein thrombosis and psychological and mobility assessment. Finally, the discharge plan is according to the patient’s case [6].
Unfortunately, the situation in Sudan is not clear. There are no available data regarding the management of stroke. However, it is obvious from the lack of proper health facilities and the high death rates among Sudanese stroke patients that the appropriate management plan is not fulfilled.According to the situation in Sudan, quality improvement studies are crucial to assess the management of stroke. This will spot the light on the main drawbacks in the hospital systems and will help to build a modified management plan for stroke management that suits the situation in terms of health structure. Appropriate reporting of medical records constitutes a crucial aspect of a patient's care. Their clarity and accuracy are fundamental for better communication between healthcare professionals and patients; to ensure a comprehensive assessment of the patient's needs. In Sudan, management plans are poorly reported in medical records; which might lead to medical errors and litigation cases. This study aimed to compare the clinical practice of the management protocol to the NICE national clinical guidelines for stroke 2016, and to determine the degree of reporting of stroke management in the medical records of the stroke patients.
2. Methods
The study was an observational cross-sectional hospital-based study. It was conducted in Ibrahim Malik teaching hospital, Soba university hospital, and Bahri teaching hospital, which are public hospitals located in Khartoum state. Retrospective data collection was conducted in the period between February to March 2021. Study participants included all patients diagnosed with stroke and aged more than 18 years old. The exclusion criteria include patients diagnosed with transient ischemic attack. The stroke cases were selected through retrospective review of the hospitals’ medical records. Using convenient non-random selection of medical records, the sample size included all the medical records of stroke cases that were presented between the first of June 2020 to the first of January 2021 in Ibrahim Malik teaching hospital, between the first of October 2020 to the first of March 2021 in Soba university hospital, between the first of September 2019 to the first of May 2021 in Bahri teaching hospital. Within these periods, the total number of medical records was found to be 406, divided as: 248, 135, 23 medical records in Ibrahim Malik teaching hospital, Soba university hospital and Bahri teaching hospital respectively.
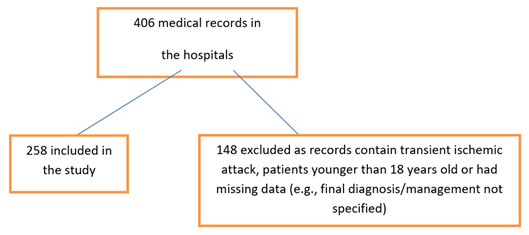
Data was collected retrospectively within the period between February to March 2021, from the medical records of stroke patients. Data were collected using checklist developed from The National Guidelines of Stroke NICE 2016 developed by The Royal College of Physicians at United Kingdom. The checklist consists from seven sections: demographic characteristic of the participants, pre-hospital care of stroke, early hospital intervention, in ward management, secondary prevention, discharge plan and final outcome. No data piloting was undertaken. A total of 406 medical records were recognized from the hospitals, of which 258 records were eligible and 148 were excluded from the study due to incompliance to inclusion criteria and some records had extensive missing data. The process of data collection is shown in Figure 1. Data were coded, and SPSS version 23 was used to perform both descriptive and inferential statistics. Data are presented using frequency tables. Kruskal Wallis H test was performed to investigate the relationship between adherence to the guidelines between different hospitals, and also the relationship between the reporting rate among different hospitals. Since the sampling technique was convenient, no attempts had been done to address selection bias. The authors declare no conflicts of interest. The study was approved by the department of community medicine-university of Khartoum, federal ministry of health, the administrations of Soba University hospital, Ibrahim Malik teaching hospital and Bahri teaching hospital. No institutions have funded this study.
3. Results
This study included 258 participants from three major tertiary public hospitals in Khartoum state. Males represented 50.8% of the participants. The mean age was 64.7 (±14.6) years. Most of the cases were from Ibrahim Malik teaching hospital. Three-quarters of the cases had ischemic strokes, detailed in Table 1.
3.1 Pre-hospital and early hospital care
In this study, 96.5% of the patients arrived at the hospital by ambulance, and 98.3% alerted the hospital before their arrival. All patients had a pre-hospital assessment in FAST assessment (Face, Arm, Speech, Time) or airway assessment and management. Details in Table 2. Regarding early hospital intervention, three-quarters of the patients received an emergency assessment by a specialist physician, and 94.1% received brain imaging (CT or MRI) within one hour of arrival. The majority of the patients (86.6%) were monitored by measuring glucose, BP, consciousness level, O2 saturation, temperature, cardiac rhythm, and hydration. Of those suspected of having a hemorrhagic stroke, 98.1% were properly managed by: stopping any anticoagulant, lowering systolic BP to 140, performing immediate surgery if needed (significant bleeding or Glasgow Coma Scale below five), and monitoring conscious level and complications continuously. Details in Table 2.
3.2 Primary management of stroke
In the primary management, 74.7% of stroke patients had their blood pressure lowered when it has raised above the guidelines level, and statins were prescribed for 81% in the proper context. The patients were assessed by: a physiotherapy specialist in 89.6%, an occupational therapist in 98.3%, a social worker in 98.3%, and a nutritionist in 93.8%. Cognition, mood, and pain levels were assessed in 88.4%, 100%, and 98.2% of the patients respectively. The rest of the details are in Table 3.
3.3 Secondary prevention and discharge plan
The hospitals were 100% adherent to secondary prevention measures’ guidelines, such as prescribing statins, lowering blood pressure, and giving appropriate lifestyle advice - table 4. Regarding the discharge plan, patients were well taught about their condition and given a discharge summary for their general practitioner in all the cases—details in table 4. Although most of the participants (63.1%) were discharged home, 23% died at the hospital—a summary of the patients’ outcomes in Table 4.
3.4 Adherence to guidelines
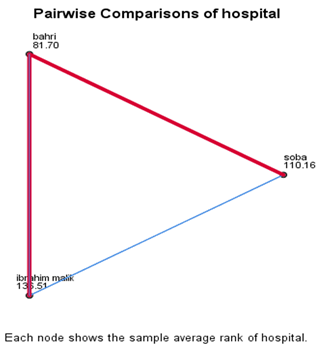
The hospitals strongly adhered to guidelines in pre-hospital management (97%) and secondary management and discharge (98.4%). Lower adherence was reported for the early hospital management (81.4%) and the primary management (83.8%)—Table 5. The relationship between adherence to the guidelines and different hospitals was investigated using the Kruskal Wallis H test. The data were skewed and kurtotic; a preliminary analysis was performed to ensure no violation of the test assumption. A Kruskal-Wallis H test showed a statistically significant difference in adherence rate between hospitals with a p-value of less than 0.0001— detailed in Table 6. The pairwise analysis of hospitals showed a statistically significant difference between Ibrahim Malik teaching hospital and Soba teaching hospital, and between Ibrahim Malik teaching hospital and Bahri teaching hospital, the significance value was adjusted by Bonferroni correction for multiple tests. Ibrahim Malik Teaching Hospital had the highest mean rank followed by Soba Teaching Hospital— Figure 1
3.5 Reporting cases
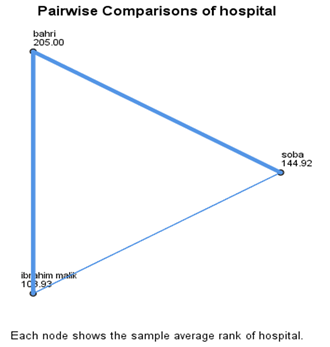
There was marked under-documentation of cases and their details. Pre-hospital management was reported in only 21.5% of the audited cohort, secondary management and discharge in 20.8%, and primary management in 35.4%. Table 5. Details of individual questions reporting are in Table 2, Table 3, and Table 4. The relationship between reporting among different hospitals was investigated using the Kruskal-Wallis H test. A preliminary analysis was performed to ensure no violation of the test assumption. A Kruskal-Wallis H test showed a statistically significant difference in the reporting rate between different hospitals with a p-value of less than 0.0001. details at Table 6. On the pairwise analysis, there was a statistical difference between each pair of hospitals, the significance values were adjusted by Bonferroni correction for multiple tests. Bahri Teaching Hospital had the highest mean rank, followed by Soba Teaching Hospital, and then Ibrahim Malik Teaching Hospital— Figure 2.
|
Variable |
Frequency |
Percent |
|
|
Gender |
Male |
131 |
50.8% |
|
Female |
127 |
49.2% |
|
|
Hospital |
Soba |
63 |
24.3% |
|
Ibrahim Malik |
174 |
67.2% |
|
|
Bahri |
22 |
8.5% |
|
|
Diagnosis |
Hemorrhagic stroke |
58 |
24.2% |
|
Ischemic stroke |
182 |
75.8% |
|
Table1: Participants’ characteristics (n=258).
|
Variable |
Frequency of right protocol |
% |
Frequency of reporting |
% |
|
Pre-hospital intervention |
||||
|
Arriving by ambulance |
55 |
96.5% |
57 |
22.4% |
|
Receiving FAST test (facial weakness, speech disturbance or unilateral limb Weakness) |
54 |
100% |
54 |
21.2% |
|
Airway assessment and management |
54 |
100% |
54 |
21.3% |
|
Hospital alert |
57 |
98.3% |
58 |
22.9% |
|
Early hospital intervention |
||||
|
Assessed for emergency stroke treatments by a specialist physician without delay |
61 |
74.3% |
82 |
31.8% |
|
Brain imaging (CT or MRI) within 1 hour |
48 |
94.1% |
51 |
19.8% |
|
Thrombolysis treatment within 3 hours |
52 |
85.2% |
61 |
33.5% |
|
Antiplatelet therapy within 24 hours |
57 |
83.8% |
68 |
37.4% |
|
Monitoring: glucose, BP, consciousness, O2, temperature, cardiac rhythm, and hydration |
58 |
86.6% |
67 |
26.4% |
|
Monitoring arrhythmias |
61 |
89.7% |
67 |
27% |
|
O2 supplement if < 95% |
54 |
96.4% |
56 |
22.2% |
|
CT angiogram for ischemic stroke when CT was not conclusive |
53 |
91.4% |
58 |
31.9% |
|
MRI with stroke-specific sequences ‘T2’ (uncertainty) |
54 |
93.1% |
58 |
23% |
|
Proper management of suspected haemorrhagic stroke |
51 |
98.1% |
52 |
89.7% |
|
Swallowing assessment |
52 |
92.9% |
56 |
21.7% |
|
Referral for dietitian when swallowing was affected |
56 |
96.6% |
58 |
23.3% |
|
NG tube when swallowing was affected |
83 |
85.6% |
97 |
37.9% |
Table 2: Pre-hospital and early hospital intervention (n=258).
|
Variable |
Frequency of right protocol |
% |
Frequency of reporting |
% |
|
Assessment of thrombolysis treatment by re-imaging |
71 |
88.8% |
80 |
44% |
|
Intra-arterial clot extraction |
54 |
90% |
60 |
33% |
|
Referral to neurosurgery |
57 |
85.1% |
67 |
100% |
|
BP lowering if Systolic BP > 185 or Diastolic BP>110 |
65 |
74.7% |
87 |
33.9% |
|
Statins prescription |
132 |
81% |
163 |
63.2% |
|
Physiotherapy specialist assessment |
95 |
89.6% |
106 |
41.1% |
|
Early Mobilization |
76 |
97.4% |
78 |
30.4% |
|
Prevention of Deep Vein Thrombosis |
108 |
87.8% |
123 |
47.7% |
|
Occupational therapist assessment |
58 |
98.3% |
59 |
23% |
|
Social workers assessment |
59 |
98.3% |
60 |
23.3% |
|
Mobility assessment |
92 |
87.6% |
105 |
41.2% |
|
Cognition assessment |
99 |
88.4% |
112 |
43.7% |
|
Apraxia assessment |
101 |
87.8% |
115 |
44.7% |
|
Speech assessment |
97 |
88.2% |
110 |
42.8% |
|
Incontinence assessment |
80 |
93% |
86 |
43.7% |
|
Incontinence management |
77 |
93.9% |
82 |
31.9% |
|
Hydration assessment |
99 |
82.5% |
120 |
46.5% |
|
Nutrition assessment |
75 |
93.8% |
80 |
31% |
|
Mood assessment |
198 |
100% |
258 |
23.3% |
|
Mouth care |
59 |
96.7% |
61 |
23.6% |
|
Pain management |
56 |
98.2% |
57 |
22.2% |
|
Vision assessment |
108 |
90% |
120 |
46.7% |
Table 3: management interventions (n=258).
|
Variable |
Frequency of right protocol |
% |
Frequency of reporting |
% |
|
|
Secondary prevention |
|||||
|
Discussing medication with patients |
58 |
100% |
58 |
22.5% |
|
|
Appropriate BP lowering. |
48 |
100% |
48 |
18.6% |
|
|
Statins |
49 |
100% |
49 |
19% |
|
|
Anti-thrombotic |
49 |
98% |
50 |
27.5% |
|
|
Life style advice |
58 |
100% |
58 |
22.5% |
|
|
Oral contraceptive advice |
59 |
98.3% |
60 |
23.3% |
|
|
Complication and co-morbidity assessment |
52 |
100% |
52 |
20.3% |
|
|
Discharge plan |
|||||
|
Patients’ education |
56 |
100% |
56 |
21.8% |
|
|
Caregiver training |
56 |
100% |
56 |
21.8% |
|
|
Caregiver assessment |
56 |
100% |
56 |
21.8% |
|
|
GP sent discharge summery |
58 |
100% |
58 |
22.6% |
|
|
Outcome |
frequency |
% |
|||
|
Discharge home |
159 |
63.1% |
|||
|
Died in hospital |
58 |
23% |
|||
|
Discharge to inpatients rehabilitation |
0 |
0% |
|||
|
Independent on Discharge |
6 |
2.4% |
|||
|
Not reported |
29 |
11.5% |
|||
Table 4: Secondary prevention and discharge plan (n=258).
|
Variable |
Adherence |
Reporting |
||
|
Mean |
SD |
Mean |
SD |
|
|
Pre-hospital intervention |
97% |
18.1% |
21.5% |
40.7% |
|
Early hospital intervention |
81.4% |
35% |
27.2% |
32.3% |
|
Primary management |
83.8% |
34.4% |
35.4% |
28.5% |
|
Secondary management and discharge |
98.4% |
12% |
20.8% |
38.1% |
Table 5: Adherence and reporting rate among different management steps range (range: 0 – 100) (n=258).
|
Hospitals |
Reporting |
Adherence |
||||
|
Reporting % |
Std error |
P value |
Adherence % |
Std error |
P value |
|
|
Soba teaching hospital |
14.8% |
0.5 |
0.0001 |
85.2% |
0.04 |
0.0001 |
|
Ibrahim Malik teaching hospital |
22.8% |
2.6 |
82.2% |
0.03 |
||
|
Bahri teaching hospital |
77.7% |
3.6 |
85.3% |
0.05 |
||
Table 6: Adherence and reporting among hospitals.
4. Discussion
Stroke is considered a growing health issue with a high burden, especially in the developing countries, where 86% of stroke deaths took place. However, it still receives very little attention [7]. The study was conducted among 258 participants in Soba university hospital, Ibrahim Malik teaching hospital, and Bahri teaching hospital. The study aimed to compare the clinical practice of the management protocol to the NICE national clinical guidelines for stroke 2016 and to determine the level of appropriate reporting of stroke management in the medical records.
This study was designed to measure the adherence to the recommended guidelines of stroke management, which are proven to be the optimum evidence-based practice to improve patient outcomes. Furthermore, the results of this study will provide an insight into the reporting process of the interventions which have been made by health providers. Time is considered a vital factor that determines the stroke patient outcome, hence; The more quickly treatment is delivered, the more chance patients have of making a good recovery. Therefore, increasing public awareness of the use of ambulance services to reach the hospital should be considered important, as well as reinforcing the paramedics with good training to provide an accurate pre-hospital assessment. Fortunately, all stroke patients in our study were provided with both FAST and airwayassessments. Moreover, 96.5% of them reached the hospital by ambulance, this finding was justified by theresidency of the participants in rural areas, where the ambulance is used to be the main transportation method for high morbid patients as stroke patients. A lower percentage (82%) of patients who used the ambulance and had their initial scan was observed in the United Kingdom. But fortunately, an improvement in this issue was recorded as a result of 5 years of continuous prospective audit in the UK [8].
Early brain scans are essential to diagnose the stroke and define its type either ischemic or hemorrhagic, as well as the exclusion of other possible medical causes with a similar clinical presentation. Accordingly, most of the patients (94.1%) in this study received the primary CT or MRI imaging within 1 hour, and three-quarters of them received an emergency assessment by a specialist physician. But only 86.6% were monitored by measuring glucose, BP, consciousness level, O2 saturation, temperature, cardiac rhythm, and hydration status. In a similar study in London, the same parameters were closely monitored by admitting 95% of patients to specialized stroke units after confirming the diagnosis. However, only half of the suspected stroke cases had the chance to get their brain image within the first 24 hours [8].
When the type of stroke has been identified, an urgent intervention would be necessary. Therefore, 85.2% of our ischemic stroke patients received thrombolysis treatment, and 83.8% of them were given antiplatelets within 3 hours and 24 hours, respectively. A better percentage of antiplatelet administration to ischemic stroke patients was reported in Western Sudan, where aspirin was given to 93% of them [7]. Three-quarters of the patients with hemorrhagic stroke had their blood pressure lowered, and 90% of them underwent thrombectomy. Comparable higher numbers were reported in the UK, as the national health system stated that 781 patients out of 86,651 stroke patients in England, Wales, and Northern Ireland received surgical intra-arterial clot retrieval [8]. while other studies in Sudan showed only medical intervention with antihypertensive medications took place in managing hemorrhagic stroke, with minimum surgical intervention [7].this was explained by the lack of adequate surgical infrastructure due to poor health finance, as Sudan is considered as one of the low-income countries [7]. All of the audited cohort patients were provided with a discharge plan and secondary prevention measures. Statins, antihypertensives, and Anti-thrombotic were prescribed. Moreover, a healthier lifestyle modification was also advised. When comparing this with the results of the National Stroke Foundation (NSF) in Australia, fewer percent of adherence to the guidelines were found, where two-thirds of the patients discharged on antihypertensives, half of them received education regarding their health status and only 38% of them received lifestyle tips (National Stroke Audit: The Australian experience).
Details of stroke patients' outcomes would provide useful information about what system of care works the best and should be followed as guidelines. Furthermore, comparing hospital data to reflect the adherence to these guidelines could also be achieved by using such data. Around 63.1% of stroke patients in our study were discharged home, while 23% were deceased at the hospital. A lower percentage of the crude death rate of 13.7% was reported in the UK [8]. But a higher mortality rate was reported in another study conducted in 2020 among Sudanese stroke patients when half of them passed away before leaving the hospital, which was justified by poor health care facilities and infrastructure [7]. High overall adherence rates to the stroke management guidelines were shown among different hospitals in this study. But unfortunately, low reporting rates were observed, as the lowest percentage was detected in Soba teaching hospital (14.8%). In a similar study , the overall adherence to the Royal College of Physicians guidelines on acute stroke management was improved by 10% by a structured audit intervention. While the recording of the management plan was enhanced by 23%. A significant improvement in the stroke patient care was concluded in the United Kingdom (Improving documentation within the acute stroke unit: Introducing a stroke specific clerking proforma).
Acknowledgment
Special thanks to the administrations of Ibrahim Malik teaching hospital, Soba university hospital, Bahri teaching hospital, and Sudan federal ministry of health.
Authors' Contributions
All authors had equally contributed to conducting this research.
Conflicts of Interest
All authors have no conflict of interest in writing and conducting this study.
References
- Akinyemi RO, Ovbiagele B, Adeniji OA, et al. Stroke in Africa: profile, progress, prospects and priorities. Nat Rev Neurol 17 (2021): 634-656.
- Mohamed A, Elfaki H. Clinical profile and pattern of management of stroke at Elobeid hospital, West Sudan Objectives: To assess the prevalence of stroke and pattern of management at Elobeid teaching hospital (2013): 6-9.
- Benamer HT, Grosset D. Stroke in Arab countries: A systematic literature review. J Neurol Sci 284 (2009): 18-23.
- Sokrab TEO, Sid-Ahmed FM, Idris MNA. Acute stroke type, risk factors, and early outcome in a developing country: A view from Sudan using a hospital-based sample. J Stroke Cerebrovasc Dis 11 (2002): 63-65.
- Mohammed OAA, Ahmed FAAO, Koko AEA, et al. Awareness about stroke among high and low risk individuals in Khartoum, Sudan: A cross-sectional study. Pan Afr Med J 36 (2020): 1-12.
- Frank A. The latest national clinical guideline for stroke. Clin Med J R Coll Physicians London 17 (2017): 478.
- Sayedahmed AMS, Alkhair MSA. Comparative study of risk factors in young adults and elderly stroke patients in Sudan. Interdiscip Neurosurg Adv Tech Case Manag 23 (2019): 100955.
- SSNAP, School of Population Health and Environmental Sciences KCL, Party on behalf of the ISW. Sentinel Stroke National Audit Programme (SSNAP) Annual Public Report (2018).