Laparoscopic Transperitoneal Pyeloplasty Outcomes in Adult Patients with Ureteropelvic Junction Obstruction
Article Information
Md. Shahidul Islam1*, Anirudha Sardar2, Mitheel-Ibna Islam3, Md. Tarikul Islam4
1Department of Surgery, Khulna Medical College Hospital, Khulna, Bangladesh 2Department of Surgery, Khulna Medical College Hospital, Khulna, Bangladesh 3Department of Gynnae & Obs, Khulna Medical College Hospital, Khulna, Bangladesh
4Department of Burn & Plastic Surgery, Khulna Medical College Hospital, Khulna, Bangladesh
*Corresponding Author: Md. Shahidul Islam, Assistant Professor, Department of Surgery, Khulna Medical College Hospital, Khulna, Bangladesh.
Received: 09 August 2023; Accepted: 18 August 2023; Published: 12 September 2023
Citation: Md. Shahidul Islam, Anirudha Sardar, Mitheel-Ibna Islam, Md. Tarikul Islam. Laparoscopic Transperitoneal Pyeloplasty Outcomes in Adult Patients with Ureteropelvic Junction Obstruction. Journal of Surgery and Research. 6 (2023): 310-316.
Share at FacebookAbstract
Background: Ureteropelvic junction obstruction (UPJO) is a frequently observed abnormality in the ureters of children. It has been reported that UPJO is approximately 5 cases per 100,000 infants each year. The obstruction at the ureteropelvic junction can be attributed to factors originating within the ureter itself (intrinsic UPJO). In contrast, cases caused by external factors are uncommon and usually result from abnormal vessels crossing the area crossing aberrant vessels.
Aim of the study: The objective of the research was to assess the results of laparoscopic Tran's peritoneal pyeloplasty in the treatment of ureteropelvic junction obstruction.
Methods: This is a retrospective study, a total of 42 patients were enrolled and analyzed. The study was conducted at the Department of Urology, Shaheed Sheik Abu Naser Specialized Hospital, and Khulna Bangladesh. The study duration was 3 years, from January 2016 to December 2019.
Result: A retrospective study analyzed 42 patients (mean age: 29.5 years) with renal abnormalities. Most had left kidney involvement (59.52%), while 40.48% had right kidney involvement. Clinical features included pain (50%), asymptomatic cases (26.19%), urinary system infections (8), and hematuria (2). The study population comprised 66.67% males and 33.33% females. The pre-operative findings showed an average operation time of 124 minutes, a bleeding amount of 38 ml, and a postoperative hematocrit level of 37.8. Most cases used the colon reflecting approach (92.86%) and the Dismembered technique (90.48%). Postoperative results showed a mean creatinine level of 0.93, a 2- 11 days hospitalization time, and a mean follow-up duration of 44 months. Complications included grade 3 (2.38%) according to Satava and Clavien classifications. Overall, 92.86% of cases were successful, with a 7.14% recurrence rate.
Conclusion: Our study identified that an elevated anterior-posterior diameter of the renal pelvis prior to surgery was associated with a higher likelihood of failure in Tran's peritoneal laparoscopy-assisted pyeloplasty. Despite the need for skilled laparoscopic skills, the procedure can be safely performed and is equally familiar as the traditional open procedure. In UPJ obstruction cases, laparoscopic pyeloplasty is a valuable alternative to open pyeloplasty.
Keywords
Laparoscopy, Pyeloplasty, Ureter pelvic junction, Obstruction
Laparoscopy articles; Pyeloplasty articles; Ureter pelvic junction articles; Obstruction articles
Laparoscopy articles Laparoscopy Research articles Laparoscopy review articles Laparoscopy PubMed articles Laparoscopy PubMed Central articles Laparoscopy 2023 articles Laparoscopy 2024 articles Laparoscopy Scopus articles Laparoscopy impact factor journals Laparoscopy Scopus journals Laparoscopy PubMed journals Laparoscopy medical journals Laparoscopy free journals Laparoscopy best journals Laparoscopy top journals Laparoscopy free medical journals Laparoscopy famous journals Laparoscopy Google Scholar indexed journals Pyeloplasty articles Pyeloplasty Research articles Pyeloplasty review articles Pyeloplasty PubMed articles Pyeloplasty PubMed Central articles Pyeloplasty 2023 articles Pyeloplasty 2024 articles Pyeloplasty Scopus articles Pyeloplasty impact factor journals Pyeloplasty Scopus journals Pyeloplasty PubMed journals Pyeloplasty medical journals Pyeloplasty free journals Pyeloplasty best journals Pyeloplasty top journals Pyeloplasty free medical journals Pyeloplasty famous journals Pyeloplasty Google Scholar indexed journals Ureter pelvic junction articles Ureter pelvic junction Research articles Ureter pelvic junction review articles Ureter pelvic junction PubMed articles Ureter pelvic junction PubMed Central articles Ureter pelvic junction 2023 articles Ureter pelvic junction 2024 articles Ureter pelvic junction Scopus articles Ureter pelvic junction impact factor journals Ureter pelvic junction Scopus journals Ureter pelvic junction PubMed journals Ureter pelvic junction medical journals Ureter pelvic junction free journals Ureter pelvic junction best journals Ureter pelvic junction top journals Ureter pelvic junction free medical journals Ureter pelvic junction famous journals Ureter pelvic junction Google Scholar indexed journals open pyeloplasty articles open pyeloplasty Research articles open pyeloplasty review articles open pyeloplasty PubMed articles open pyeloplasty PubMed Central articles open pyeloplasty 2023 articles open pyeloplasty 2024 articles open pyeloplasty Scopus articles open pyeloplasty impact factor journals open pyeloplasty Scopus journals open pyeloplasty PubMed journals open pyeloplasty medical journals open pyeloplasty free journals open pyeloplasty best journals open pyeloplasty top journals open pyeloplasty free medical journals open pyeloplasty famous journals open pyeloplasty Google Scholar indexed journals cystoscopy articles cystoscopy Research articles cystoscopy review articles cystoscopy PubMed articles cystoscopy PubMed Central articles cystoscopy 2023 articles cystoscopy 2024 articles cystoscopy Scopus articles cystoscopy impact factor journals cystoscopy Scopus journals cystoscopy PubMed journals cystoscopy medical journals cystoscopy free journals cystoscopy best journals cystoscopy top journals cystoscopy free medical journals cystoscopy famous journals cystoscopy Google Scholar indexed journals general anaesthesia articles general anaesthesia Research articles general anaesthesia review articles general anaesthesia PubMed articles general anaesthesia PubMed Central articles general anaesthesia 2023 articles general anaesthesia 2024 articles general anaesthesia Scopus articles general anaesthesia impact factor journals general anaesthesia Scopus journals general anaesthesia PubMed journals general anaesthesia medical journals general anaesthesia free journals general anaesthesia best journals general anaesthesia top journals general anaesthesia free medical journals general anaesthesia famous journals general anaesthesia Google Scholar indexed journals renal pelvis articles renal pelvis Research articles renal pelvis review articles renal pelvis PubMed articles renal pelvis PubMed Central articles renal pelvis 2023 articles renal pelvis 2024 articles renal pelvis Scopus articles renal pelvis impact factor journals renal pelvis Scopus journals renal pelvis PubMed journals renal pelvis medical journals renal pelvis free journals renal pelvis best journals renal pelvis top journals renal pelvis free medical journals renal pelvis famous journals renal pelvis Google Scholar indexed journals surgical outcome articles surgical outcome Research articles surgical outcome review articles surgical outcome PubMed articles surgical outcome PubMed Central articles surgical outcome 2023 articles surgical outcome 2024 articles surgical outcome Scopus articles surgical outcome impact factor journals surgical outcome Scopus journals surgical outcome PubMed journals surgical outcome medical journals surgical outcome free journals surgical outcome best journals surgical outcome top journals surgical outcome free medical journals surgical outcome famous journals surgical outcome Google Scholar indexed journals urinary system infections articles urinary system infections Research articles urinary system infections review articles urinary system infections PubMed articles urinary system infections PubMed Central articles urinary system infections 2023 articles urinary system infections 2024 articles urinary system infections Scopus articles urinary system infections impact factor journals urinary system infections Scopus journals urinary system infections PubMed journals urinary system infections medical journals urinary system infections free journals urinary system infections best journals urinary system infections top journals urinary system infections free medical journals urinary system infections famous journals urinary system infections Google Scholar indexed journals
Article Details
Introduction
Ureteropelvic junction obstruction (UPJO) refers to an obstruction occurring where the ureter meets the renal pelvis. This condition is frequently identified through prenatal ultrasounds and is the leading cause of hydronephrosis detected before birth [1]. UPJO affects approximately 1 in every 1500 live births and is more commonly observed in males. Moreover, it involves the left ureter twice as often as the right ureter [2]. In most cases, UPJO obstruction is temporary. It occurs more frequently in males, with a ratio of 2:1 compared to females. The left side affects about two-thirds of patients, and bilateral involvement occurs in 10-46% of cases [3]. In 1949, Anderson and Hynes introduced an open- dismembered pyeloplasty technique as a treatment for UPJO [4]. This technique has since been widely utilized due to its high success rate. However, the traditional lumbotomy approach is associated with increased morbidity, leading to minimally invasive alternatives such as antegrade or retrograde endopyelotomy, balloon dilation, and cause endopyelotomy [5-7]. Despite employing these techniques, their rates of success remain inferior to those of open pyeloplasty [8]. The initial description of laparoscopic pyeloplasty was provided by Schuster et al. during the early 1990s [9]. Over the past decade, laparoscopic pyeloplasty has evolved to deliver comparable outcomes to open surgery while reducing morbidity and complications [10]. This study aimed to assess the effectiveness of laparoscopic Tran's peritoneal pyeloplasty in treating ureteropelvic junction obstruction.
Methodology and Materials
Surgical procedures
To confirm UPJ obstruction, patients underwent cystoscopy with retrograde pyelography. All procedures were performed transperitoneally under intubated general anaesthesia. The patients' positions and trocar sites are shown in figure 1. The Told line was incised, and the colon on the affected side was reflected medially. Gerota's fascia was incised, freeing the ureter and the renal pelvis. The UPJ was cleaned of perirenal fat, and a stay suture was placed in the medial edge of the renal pelvis just below the renal vein (Figure 2a). The suture was pulled out through the abdominal wall using a 3-0 vicryl suture and secured with appropriate tension. In cases of severe hydronephrosis (over 150 mL), the renal pelvis was reduced. The redundant portion of the pelvis, between the stay suture (upper edge) and the UPJ (lower edge), was resected circumferentially with scissors. The pelvis was closed with running 3-0 polyglycolic acid sutures, terminating 1 cm above the lower edge of the incision (Figure 2b). Suturing before transection of the ureter provided tension between the stay suture and the ureter, significantly facilitating the procedure. Subsequently, the stenotic segment of the UPJ was transected horizontally, and the lateral aspect was spatulated longitudinally toward a point 1 cm below the stenotic segment. The ureteropelvic anastomosis was performed using interrupted 4-0 polyglycolic acid sutures (Figure 2c). A suture was passed outside-in at the apex of the incised renal pelvis and inside- out at the apex of the spatulated ureter and then tied. The ureteric stent was advanced back into the renal pelvis, remaining in the ureter and extending into the urinary bladder. The tip of the proximal ureter and the cephalad edge of the pelvic opening were sutured. The interrupted anastomosis was initiated from the caudal to the cephalad edge, first on the anterior side, then on the posterior side. Maintaining this direction of suturing was essential to ensure reliable stitching at the distal edge of the ureteropelvic anastomosis, which was critical for a successful surgical outcome (Figure 2d). A 5-mm suction drain was inserted through the 5-mm port and removed when the suctioned material decreased to less than 10 mL. A Foley catheter was usually left in place for 48 hours. The double pigtail stent remained indwelling for 4-6 weeks.
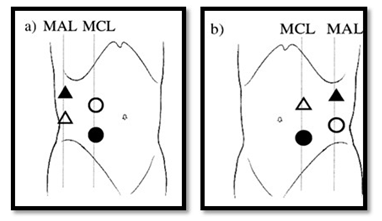
Figure 1: Patients’ position and trocar sites for (a) right and (b) left side laparoscopic pyeloplasty. Patient was placed in semilateral position. A camera port (?) was on midclavicular line 3cm below the umbilicus using an open laparoscopic method. ?,10 mm camera port; O, 10 mm for surgeon’s right hand; Δ; 5 mm port for surgeon’s left hand; ?, 5 mm for assistant; MAL, mid-axillary line; MCL, mid-clavicular line.
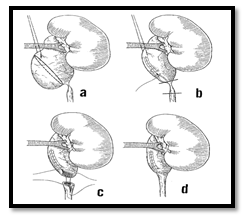
Figure 2: Dismembered Anderson- Hynes pyeloplasty (a) A stay suture and cutting line of redundant pelvis; (b) closure of the pelvis with running sutures. Transection line of narrow segment of the ureter (c) Ureteropelvic anastomosis; and (d) plasty completed.
Assessment of surgical outcome
Patients were scheduled to return for a follow-up visit within 4 to 6 weeks to have their stent removed. Two months after the procedure, a patient underwent an intravenous pyelogram (IVP) or nuclear renography and received semiannual assessments. Patients received clinical examinations every 3 to 12 months depending on their symptoms. Radiographic success was defined as enhanced drainage observed on diuretic renography or the observation of a patent ureteropelvic junction (UPJ) with improved hydronephrosis on IVP.
In all cases, a laparoscopic approach was used. Complications during the operation were classified according to the Satava classification, while postoperative complications were classified using the Clavien classification [11,12]. Postoperatively, patients were monitored based on radiological and laboratory findings. Ultrasonography (US) was performed within the first three months after the operation for assessment purposes, and mercaptoacetyltriglycine (MAG-3) scintigraphy was conducted in the sixth month. The timing of follow-up intervals was planned accordingly. The patients were divided into two groups based on the presence of crossing vessels. Demographic data such as age, age group, gender, affected side, history of previous renal surgery, and presence of kidney stones were investigated in both groups.
· Inclusion criteria:
This study included an assessment of all patients with UPJO, and solely those who had undergone pyeloplasty were considered.
· Exclusion criteria:
The following conditions were considered as exclusion criteria: the presence of neurological lesions, anatomical abnormalities in the lower urinary tract (BPH), bilateral hydronephrosis, small bilateral kidneys, horseshoe kidneys, multicystic dysplastic kidney, and vesicoureteral reflux (VUR), as well as chronic renal failure.
All numerical data were organized in appropriate tables or graphs based on similarity. A detailed description accompanied each table and graph to facilitate a clear understanding of the information presented. Statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS) software on a Windows operating system. Mean ± standard deviation (SD) was used to express continuous variables, while categorical variables were presented as frequency and percentage. To compare continuous variables between groups, the student’s t-test was employed. The Chi-Square test was utilized to compare categorical variables. A significance level of 95.0% confidence interval and a p-value less than 0.05 were considered statistically significant in determining the results.
Result
A retrospective study enrolled and analyzed a total of 42 patients. The characteristics and demographical data of the patients are presented in table 1. The patients ranged in age from 19 to 51 years, with a mean age of 29.5 years. The mean levels of HCT and creatinine were 39 and 0.9, respectively, with a range of 26-45 for HCT and 0.5-1.3 for creatinine. Left kidney involvement was observed in most patients (25, 59.52%), while 40.48% had right kidney involvement. Renal abnormalities included crossing vessels (35.71% of patients), kidney stones (14.29% of patients), and one case of horseshoe kidney. Clinical features indicated that 50% of the patients had pain, 26.19% had no symptoms, 8 had urinary system infections, and two had hematuria (Table 1). The distribution of the study population by sex is illustrated in figure 1, where 66.67% were male and 33.33% were female. Table 2 displays the pre-operative findings, revealing an average operation time of 124 minutes (range: 80-245 minutes), an average bleeding amount of 38 millilitres (range: 22-53 millilitres), and average postoperative hematocrit (HCT) level of 37.8 (range: 26-43). Most cases (92.86%) utilized the colon reflecting approach, while the remaining 7.14% used the Transmesocolic approach. The Dismembered technique was employed in 90.48% of cases, and the Y-V plasty was used in 9.52% of patients (Table 2). Postoperative findings presented in table 3 include the mean postoperative creatinine level of 0.93 (normal range: 0.5-1.3), hospitalization time ranging from 2 to 11 days (average: 3.05 days), and mean follow-up duration of 44 months (range: 12-120 months). The table also reports postoperative complications based on the Satava and Clavien classifications. According to the Satava classification, grade 3 complications were observed in one case (2.38% of total cases). The Clavien classification identified three cases of grade 1 and grade 2 complications, each accounting for 7.14% of the cases and one case of grade 3 complications (2.38% of total cases). Finally, the table summarizes the results, indicating that 92.86% of cases (39 patients) were successful, while 7.14% (three cases) experienced a recurrence.
|
Characteristics |
Frequency/Mean |
Percentage/Range |
|
Age (year) |
29.5 |
19-51 |
|
HCT level (preoperative) |
39 |
(26-45) |
|
Creatinine level (preoperative) |
0.9 |
0.5-1.3 |
|
Side |
||
|
Left kidney |
25 |
59.52 |
|
Right kidney |
17 |
40.48 |
|
Primer/seconder |
||
|
Primer |
39 |
92.86 |
|
Seconder |
2 |
4.76 |
|
ASA score (mean) |
1 |
2.38 |
|
Concomitant renal abnormality |
||
|
Crossing vessel |
15 |
35.71 |
|
Kidney stone |
6 |
14.29 |
|
Solitary kidney |
2 |
4.76 |
|
Horseshoe kidney |
1 |
2.38 |
|
Clinical features |
||
|
Pain |
21 |
50 |
|
No symptom |
11 |
26.19 |
|
Urinary system infection |
8 |
19.05 |
|
Hematuria |
2 |
4.76 |
Table 1: Characteristics of patients and demographic data.
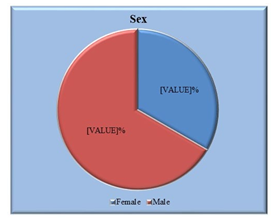
Figure 1: Sex distribution of the study population (N=42)
|
Findings |
Frequency/Mean |
Percentage/Range |
|
Operation time (min) |
124 |
80-245 |
|
Bleeding (mL) |
38 |
22-53 |
|
HCT level (postoperative) |
37.8 |
26-43 |
|
Approach |
||
|
Colon reflecting |
39 |
92.86 |
|
Transmesocolic |
3 |
7.14 |
|
Technique |
||
|
Dismembered |
38 |
90.48 |
|
Y-V plasty |
4 |
9.52 |
Table 2: Per-operative findings of the study population.
|
Findings |
Frequency/Mean |
Percentage/Range |
|
Creatinine level (postoperative) |
0.93 |
0.5-1.3 |
|
Hospitalization time (days) |
3.05 |
02-11 |
|
Follow-up (months) |
44 |
12-120 |
|
Perioperative complications according to |
||
|
Satava classification |
1 |
2.38 |
|
Grade 3 |
1 |
2.38 |
|
Postoperative complications according to |
||
|
Clavien classification |
3 |
7.14 |
|
Grade 1 |
1 |
2.38 |
|
Grade 2 |
3 |
7.14 |
|
Grade 3 |
1 |
2.38 |
|
Results |
||
|
Succeed |
39 |
92.86 |
|
Recurrence |
3 |
7.14 |
Table 3: Per-operative findings of the study population.
Discussion
Since its initial definition by Schuster et al. in 1993, laparoscopic management of ureteropelvic junction obstruction (UPJO) has emerged as a favorable alternative to open and endoscopic techniques [9]. The selection among open, laparoscopic, endoscopic, or robotic approaches relies on the surgeon's inclination and expertise and the respective benefits and drawbacks of each technique. The advancements in endoscopic and laparoscopic procedures over the past two decades and recent developments in robotic surgery over the past 5-10 years have led to a growing preference for minimally invasive techniques among surgeons. Factors such as cost, availability of surgical equipment, and expertise play a crucial role in determining the preferred technique. Studies have shown that open pyeloplasty generally has a shorter operative time than laparoscopic pyeloplasty. However, laparoscopic pyeloplasty has become the gold standard therapy in some centres due to the advantages of shorter hospitalization and reduced need for pain medication [13,14]. In our investigation, we utilized the laparoscopic method for treating all cases. We attained a success rate of 93.1%, which aligns with the outcomes documented by skilled laparoscopic surgeons in the existing literature [15-17]. The most common symptom in adults with UPJO is pain, which may be accompanied by urinary tract infections or hematuria. However, UPJO can also be incidentally discovered during diagnostic tests for unrelated issues, even without symptoms [18]. In our study, 50% of the patients presented with pain, 18.1% had urinary tract infections, 5.2% had hematuria, and 26.7% were asymptomatic. Nearly 30% of the patients had a crossing vessel at the UPJ [19]. In our study, 41 (35.3%) patients had a crossing vessel, 17 (14.6%) had a kidney stone, 4.3% had a solitary kidney, and 2.5% had a horseshoe kidney anomaly. The relationship between the presence of a crossing vessel and UPJO and the impact of vascular transposition or ligation on the outcomes of pyeloplasty is a topic of debate. Some studies have found crossing vessels in approximately 20% of patients with a normal UPJ, while patients with UPJO are more likely to have crossing vessels than the general population [20,21]. In our study, 35.3% of the patients had a crossing vessel, and there was no statistically significant relationship between the presence of a crossing vessel and any demographic feature. Dismembered pyeloplasty is the most commonly preferred surgical technique [22]. It offers the advantage of removing the narrowed segment but is technically more challenging than non-dismembered pyeloplasty because the ureter needs to be divided [9]. In non-dismembered pyeloplasty, the ureter is not divided, allowing the first suture to be placed without tension and reducing the anastomosis time. However, more scientific evidence is needed to determine which method is superior for patients. In our study, 82% of the patients underwent dismembered pyeloplasty. While the Anderson-Hynes dismembered pyeloplasty is the most commonly used technique, various techniques can be applied depending on the pelvic anatomy. Foley Y-V plasty is the most commonly used non-dismembered technique, mainly when there is a need for high ureteral access. However, this technique may not be suitable when the lower pole vessel needs to be transposed. It is worth noting that crossing vessels are not always responsible for UPJO [23]. Moreover, the success rate of Y-V plasty applied in the presence of a crossing vessel is comparable to that of Anderson-Hynes pasty [16]. In our study, 1 out of 10 patients undergoing Foley Y-V plasty had a crossing vessel. In these cases, it was determined that the crossing vessels were not responsible for the external compression since they were localized proximal to the UPJ. Additionally, the Y-V plasty technique moves the UPJ further away from the crossing vessel. Our study, which presents our 14-year experience with laparoscopic pyeloplasty, confirms the shift from Y-V plasty to predominantly using dismembered pyeloplasty. Similar trends have been observed in other studies reporting their first 100-case experiences [15-17]. However, these studies did not specify when and to what extent the Y-V technique was used during the learning curve. The presence of a kidney stone does not hinder the laparoscopic technique for UPJO. In 2002, Ramakumar et al. published a series of 20 cases where simultaneous pyelotomy was performed laparoscopically. Similarly, in our study, the preoperative assessment revealed stones in 17 (14.6%) cases, leading to the application of laparoscopy-guided simultaneous pyelolithotomy. While a horseshoe kidney may pose a challenge for the laparoscopic approach, a few studies have reported successful outcomes [24-26]. In our study, laparoscopic pyeloplasty was performed in 3 (2.5%) patients with horseshoe kidney anomalies. Therefore, laparoscopic pyeloplasty has been proven to be a thriving option for patients with renal anomalies. Laparoscopic pyeloplasty can also be effectively performed in patients with recurrent UPJO who have previously undergone surgery. However, creating a favourable surgical space and performing ureter dissection can be more challenging due to adhesions resulting from the previous surgery. Advanced laparoscopic skills are required to achieve tension-free anastomosis [27]. In our study, 8 (6.9%) patients had a history of open pyeloplasty. Among them, 6 (5.2%) did not experience recurrence during follow-up, while 2 (1.7%) patients developed recurrent obstruction. One (0.8%) patient underwent endopyelotomy; the other (0.8%) had a failed procedure and required nephrectomy. The trans mesocolic approach was utilized in our study's 8 (6.9%) patients. For left-sided UPJOs, the transperitoneal approach, which involves incision and dissection through the Toldt line for colon mobilization, can limit laparoscopic visibility due to bleeding and fogging, thus prolonging the operating time. For this reason, specific centres prefer the trans mesocolic approach for left-sided UPJOs. Other studies have reported shorter operating times with the trans mesocolic method than the transperitoneal approach [28,29]. However, the trans mesocolic technique is not widely preferred as it is suitable mainly for younger, lean patients with low mesenteric adipose tissue [30]. Only 8 (6.9%) patients underwent the trans mesocolic approach in our study. Due to the limited number of patients with this approach, no comparison was made. Some series in the literature have reported performing pyeloplasty without using a double-J stent [31,32]. These studies suggest that stentless pyeloplasty is a safe and feasible technique. In 2007, Shalhav et al. published the outcomes of 5 patients in whom they performed laparoscopic stentless pyeloplasty [33]. However, in our study, all patients who underwent laparoscopic pyeloplasty had a double-J stent placed. The stents were typically removed one month after the surgery. During the perioperative period, 1 (0.8%) patient experienced a grade 3 complication according to the Satava classification. In the postoperative period, 2 (1.7%) patients had grade 1 complications, 7 (6%) patients had grade 2 complications, and 1 (0.8%) patient had a grade 3 complication according to the Clavien classification (Table 2). One patient (0.8%) suffered a left colon injury during port insertion, which was repaired laparoscopically without further complications. The overall postoperative complication rate was 8.6%. Two (1.7%) patients experienced high fever (grade 1), 3 (2.6%) patients had prolonged extravasation of urine (grade 2), and 5 (4.3%) patients developed paralytic ileus (grade 2). These patients showed improvement during postoperative follow-up with medical treatment. In one case (0.8%), a percutaneous nephrostomy catheter was inserted due to extravasation of urine (grade 3 complication). The average follow-up time was 44 (12-120) months, and the specific follow-up intervals were determined based on ultrasound (US) at 1-3 months postoperatively and MAG-3 scintigraphy at 6 months postoperatively for assessment purposes. During the follow-up period, 8 (6.9%) patients experienced recurrent obstruction. Endopyelotomy was performed in 7 (6.1%) patients to address the recurrence. Among these cases, 2 (1.7%) were tertiary cases that underwent laparoscopic pyeloplasty following open pyeloplasty. One patient (0.8%) ultimately required a nephrectomy. The rate of complications in our study is consistent with those reported in the literature [15-17].
Limitations of the study
This study presents the outcomes and complication rates of adult patients who underwent LTP at our centre. The findings of this study indicate that LTP can be successfully performed in adult patients with UPJO. However, it is essential to acknowledge the limitations of our study. The data collection was conducted over time and verified retrospectively, which may have introduced some errors. Additionally, our study did not include a comparison with open surgery, although we followed the general principles of open surgery during the LTP procedure. Notwithstanding these limitations, our results indicate that LTP is a safe and viable treatment option for managing UPJO. In order to address these limitations, future studies should be designed prospectively.
Conclusion and recommendations
LTP proves to be a reliable and secure method for performing surgery on adult patients diagnosed with UPJO. It can serve as a primary treatment option due to its minimal complication rates, suitability for patients with anatomical differences, and the advantage of a brief hospital stay.
Funding:
No funding sources
Conflict of interest:
None declared
References
- Kher K, Schnaper HW, Makker Clinical pediatric nephrology. CRC Press (2006).
- Alan SL, Chertow GM, Luyckx V, et Brenner y Rector. El riñón. Elsevier Health Sciences (2021).
- Wood Pediatric emergencies. Urological Emergencies In Clinical Practice 12 (2013): 247-258.
- Anderson JC, Hynes Retrocaval Ureter: A Case diagnosed pre-operatively and treated successfully by a Plastic Operation. British journal of urology 21(1949): 209-214.
- Wickham JE, Kellet Percutaneous pyelolysis. European Urology 9 (1983): 122-124.
- Clayman RV, Basler JW, Kavoussi L, et Ureteronephroscopic endopyelotomy. The Journal of Urology 144 (1990): 246-251.
- Chandhoke ps, Clayman rv, Stone, et Endopyelotomy and endoureterotomy with the Acucise ureteral cutting balloon device: preliminary experience. Journal of Endourology 7 (1993): 45-51.
- Motola JA, Badlani GH, Smith Results of 212 consecutive endopyelotomies: An 8-year followup. The Journal of urology 149 (1993): 453-456.
- Schuessler WW, Grune MT, Tecuanhuey LV, et Laparoscopic dismembered pyeloplasty. The Journal of urology 150 (1993): 1795-1799.
- Arun N, Kekre NS, Nath V, et Is open pyeloplasty still justified?. British journal of urology 80 (1997): 379-381.
- Satava Identification and reduction of surgical error using simulation. Minimally Invasive Therapy & Allied Technologies 14 (2005): 257-261.
- Dindo D, Demartines N, Clavien Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of surgery 240 (2004): 205.
- Symons SJ, Bhirud PS, Jain V, et Laparoscopic pyeloplasty: our new gold standard. Journal of endourology 23 (2009): 463-467.
- Moon DA, El-Shazly MA, Chang CM, et Laparoscopic pyeloplasty: evolution of a new gold standard. Urology 67 (2006): 932-936.
- Jarrett TW, Chan DY, Charambura TC, et al. Laparoscopic pyeloplasty: the first 100 cases. The journal of urology 167 (2002): 1253-1256.
- Szydelko T, Kasprzak J, Lewandowski J, et al. Dismembered laparoscopic Anderson-Hynes pyeloplasty versus nondismembered laparoscopic YV pyeloplasty in the treatment of patients with primary ureteropelvic junction obstruction: a prospective Journal of endourology 26 (2012): 1165-1170.
- Singh O, Gupta SS, Arvind NK. Laparoscopic pyeloplasty: an analysis of first 100 cases and important lessons International urology and nephrology 43 (2011): 85-90.
- Park JM, Bloom DA. The pathophysiology of UPJ obstruction: current concepts. Urologic Clinics of North America 25 (1998): 161-169.
- Van cangh PJ, Nesa S, Galeon M, et al. Vessels around the ureteropelvic junction: significance and imaging by conventional Journal of endourology 10 (1996): 111-1119.
- Zeltser IS, Liu JB, Bagley DH. The incidence of crossing vessels in patients with normal ureteropelvic junction examined with endoluminal The Journal of urology 172 (2004): 2304-2307.
- Sampaio FJ. Vascular anatomy at the ureteropelvic junction. Urologic Clinics of North America 25 (1998): 251-258.
- Gallo F, Schenone M, Giberti C. Ureteropelvic junction obstruction: which is the best treatment today?. Journal of Laparoendoscopic & advanced surgical techniques 19 (2009): 657-662.
- Lawler LP, Jarret TW, Corl FM, et al. Adult Ureteropelvic Junction Obstruction: Insights with Three- dimensional Multi–Detector Row Radiographics 25 (2005): 121-134.
- Ramakumar S, Lancini V, Chan DY, et al. Laparoscopic pyeloplasty with concomitant pyelolithotomy. The Journal of urology 167 (2002): 1378-1380.
- Hsu TH, Presti Jr JC. Anterior extraperitoneal approach to laparoscopic pyeloplasty in horseshoe kidney: a novel Urology 62 (2003): 1114-1116.
- Janetschek G, Peschel R, Altarac S, et al. Laparoscopic and retroperitoneoscopic repair of ureteropelvic junction Urology 47 (1996): 311-316.
- Parma P, Samuelli A, Luciano M, et al. Salvage laparoscopic pyeloplasty in the worst case scenario: after failed open repair and endoscopic salvage 20 (2006): 808-812.
- Porpiglia F, Billia M, Volpe A, et Transperitoneal left laparoscopic pyeloplasty with transmesocolic access to the pelvi-ureteric junction: technique description and results with a minimum follow-up of 1 year. BJU international 101 (2008): 1024-1028.
- Han HH, Ham WS, Kim JH, et Transmesocolic approach for left side laparoscopic pyeloplasty: comparison with laterocolic approach in the initial learning period. Yonsei medical journal 54 (2013): 197- 203.
- Shadpour P, Nayyeri RK, Daneshvar R, et Prospective clinical trial to compare standard colon-reflecting with transmesocolic laparoscopic pyeloplasty. BJU international 110 (2012): 1814-1818.
- Khawaja AR, Dar TI, Bashir F, et al. Stentless laparoscopic pyeloplasty: A single center experience. Urology Annals 6 (2014):
- Smith KE, Holmes N, Lieb JI, et Stented versus nonstented pediatric pyeloplasty: a modern series and review of the literature. The Journal of urology 168 (2002): 1127-1130.
- Shalhav AL, Mikhail AA, Orvieto MA, et Adult stentless laparoscopic pyeloplasty. JSLS: Journal of the Society of Laparoendoscopic Surgeons 11 (2007): 8.
