Laparoscopic Management of Giant Paraesophageal Hernia: Case Report and Review
Article Information
Luis Espinosa Torres, Alfonso Montes de Oca Navarro, Stephanie Serrano Collazos, Manuel Alejandro Meza Jasso*
Departament of General Surgery, General hospital of Ecatepec, “Las Americas”, Mexico
*Corresponding Author: Alejandro Meza Jasso. Departament of general surgery, General hospital of Ecatepec, “Las Americas”, Mexico
Received: 20 August 2022; Accepted: 05 September 2022; Published: 19 June 2023
Citation: Luis Espinosa Torres, Alfonso Montes de Oca Navarro, Stephanie Serrano Collazos, Manuel Alejandro Meza Jasso. Laparoscopic Management of Giant Paraesophageal Hernia: Case Report and Review. Journal of Surgery and Research 6 (2023): 232-236.
Share at FacebookAbstract
There are 4 types of hiatal hernia, being type IV the rarest of all. The management today remains controversial about the ideal approach (abdominal, thoracic, mixed approach, laparoscopic or open surgery), the use or not of mesh, what type of fundoplication (anterior, posterior, total or parcial). We will present a giant paraesophageal hernia with gastric herniation and transverse colon resolved by laparoscopy, in an emergency surgery.
Keywords
Paraesophageal hernia, Laparoscopic, Biologic mesh, Emergency
Paraesophageal hernia articles; Laparoscopic articles; Biologic mesh articles; Emergency articles
Paraesophageal hernia articles Paraesophageal hernia Research articles Paraesophageal hernia review articles Paraesophageal hernia PubMed articles Paraesophageal hernia PubMed Central articles Paraesophageal hernia 2023 articles Paraesophageal hernia 2024 articles Paraesophageal hernia Scopus articles Paraesophageal hernia impact factor journals Paraesophageal hernia Scopus journals Paraesophageal hernia PubMed journals Paraesophageal hernia medical journals Paraesophageal hernia free journals Paraesophageal hernia best journals Paraesophageal hernia top journals Paraesophageal hernia free medical journals Paraesophageal hernia famous journals Paraesophageal hernia Google Scholar indexed journals Laparoscopic articles Laparoscopic Research articles Laparoscopic review articles Laparoscopic PubMed articles Laparoscopic PubMed Central articles Laparoscopic 2023 articles Laparoscopic 2024 articles Laparoscopic Scopus articles Laparoscopic impact factor journals Laparoscopic Scopus journals Laparoscopic PubMed journals Laparoscopic medical journals Laparoscopic free journals Laparoscopic best journals Laparoscopic top journals Laparoscopic free medical journals Laparoscopic famous journals Laparoscopic Google Scholar indexed journals Biologic mesh articles Biologic mesh Research articles Biologic mesh review articles Biologic mesh PubMed articles Biologic mesh PubMed Central articles Biologic mesh 2023 articles Biologic mesh 2024 articles Biologic mesh Scopus articles Biologic mesh impact factor journals Biologic mesh Scopus journals Biologic mesh PubMed journals Biologic mesh medical journals Biologic mesh free journals Biologic mesh best journals Biologic mesh top journals Biologic mesh free medical journals Biologic mesh famous journals Biologic mesh Google Scholar indexed journals Emergency articles Emergency Research articles Emergency review articles Emergency PubMed articles Emergency PubMed Central articles Emergency 2023 articles Emergency 2024 articles Emergency Scopus articles Emergency impact factor journals Emergency Scopus journals Emergency PubMed journals Emergency medical journals Emergency free journals Emergency best journals Emergency top journals Emergency free medical journals Emergency famous journals Emergency Google Scholar indexed journals Gastro-esophageal junction articles Gastro-esophageal junction Research articles Gastro-esophageal junction review articles Gastro-esophageal junction PubMed articles Gastro-esophageal junction PubMed Central articles Gastro-esophageal junction 2023 articles Gastro-esophageal junction 2024 articles Gastro-esophageal junction Scopus articles Gastro-esophageal junction impact factor journals Gastro-esophageal junction Scopus journals Gastro-esophageal junction PubMed journals Gastro-esophageal junction medical journals Gastro-esophageal junction free journals Gastro-esophageal junction best journals Gastro-esophageal junction top journals Gastro-esophageal junction free medical journals Gastro-esophageal junction famous journals Gastro-esophageal junction Google Scholar indexed journals Endoscopy Surgeons articles Endoscopy Surgeons Research articles Endoscopy Surgeons review articles Endoscopy Surgeons PubMed articles Endoscopy Surgeons PubMed Central articles Endoscopy Surgeons 2023 articles Endoscopy Surgeons 2024 articles Endoscopy Surgeons Scopus articles Endoscopy Surgeons impact factor journals Endoscopy Surgeons Scopus journals Endoscopy Surgeons PubMed journals Endoscopy Surgeons medical journals Endoscopy Surgeons free journals Endoscopy Surgeons best journals Endoscopy Surgeons top journals Endoscopy Surgeons free medical journals Endoscopy Surgeons famous journals Endoscopy Surgeons Google Scholar indexed journals giant paraesophageal hernia articles giant paraesophageal hernia Research articles giant paraesophageal hernia review articles giant paraesophageal hernia PubMed articles giant paraesophageal hernia PubMed Central articles giant paraesophageal hernia 2023 articles giant paraesophageal hernia 2024 articles giant paraesophageal hernia Scopus articles giant paraesophageal hernia impact factor journals giant paraesophageal hernia Scopus journals giant paraesophageal hernia PubMed journals giant paraesophageal hernia medical journals giant paraesophageal hernia free journals giant paraesophageal hernia best journals giant paraesophageal hernia top journals giant paraesophageal hernia free medical journals giant paraesophageal hernia famous journals giant paraesophageal hernia Google Scholar indexed journals emergency room articles emergency room Research articles emergency room review articles emergency room PubMed articles emergency room PubMed Central articles emergency room 2023 articles emergency room 2024 articles emergency room Scopus articles emergency room impact factor journals emergency room Scopus journals emergency room PubMed journals emergency room medical journals emergency room free journals emergency room best journals emergency room top journals emergency room free medical journals emergency room famous journals emergency room Google Scholar indexed journals stenosis articles stenosis Research articles stenosis review articles stenosis PubMed articles stenosis PubMed Central articles stenosis 2023 articles stenosis 2024 articles stenosis Scopus articles stenosis impact factor journals stenosis Scopus journals stenosis PubMed journals stenosis medical journals stenosis free journals stenosis best journals stenosis top journals stenosis free medical journals stenosis famous journals stenosis Google Scholar indexed journals
Article Details
Introduction
Hiatal hernias were first described by Henry Ingersoll Bowditch in 1853 [1]. They are characterized by a lengthening of the space between the diaphragmatic pillars, and weakness of the brake-esophageal membrane, with the consequent protrusion of the stomach inside the thoracic cavity [1]. Four subtypes are described, type 1 or "sliding hernia" where only the Gastro-esophageal junction is found inside the thorax and is the most common 95%. The other 3 types are classified as paraesophageal and together they are the remaining 5-15%. Type 2 is a true paraesophageal hernia, with herniation of the gastric fundus through a weak paraesophageal membrane. Type 3 is a combination of type 1 and 2, with herniation of the Gastro-esophageal junction and the gastric fundus within the thorax, encompassing 90% of the true paraesophageal hernias.
Type 4 are the result of defects in the phrenoesophageal membrane that lead to a displacement of the stomach with another organ, such as spleen, colon, pancreas inside the thoracic cavity [2,3]. The Society of American Gastrointestinal and Endoscopy Surgeons (SAGES) recommends its repair in patients with symptomatic paraesophageal hernia, as well as patients with obstructive symptoms or gastric volvulus require urgent repair, as it can progress to strangulation and ischemia leading to necrosis and perforation with high mortality [4]. The approach of choice today is to perform laparoscopic fundoplication even in giant paraesophageal hernias, in our case we will present a giant paraesophageal hernia with gastric herniation and transverse colon resolved by laparoscopy.
Case
76-year-old female patient, open appendectomy at 19 years, bilateral salpingoclasis at 36 years, right inguinal plasty at 40 years, open hysterectomy at 61 years, 3 wall plasty by incisional hernia, the last with mesh at 75 years. 8 years with diagnosis of stable angina in medical management with acetylsalicylic acid and Diltiazem. The patient has a 5-year history of progression of dyspnea from medium to small efforts as well as dizziness and the use of 2 pillows to sleep, with multiple assessments by a private doctor. In addition, dyspepsia, early satiety and postprandial regurgitation are added, as well as dizziness without reaching post prandial syncope, with worsening of dyspnea, so she goes to the emergency room for assessment and imaging studies are performed (figures 1 and 2). Fundoplication was performed in French position, with 5 ports and hepatic separator, it proceeds to reduce hernia content (stomach and transverse colon), (figures 3 and 4); the hernia sac is dissected, pillars are released and the esophagus is dissected until 3cm of the intra-abdominal portion is obtained. Crura is reapproximadated with 4 points with Ethibon # 2, (figure 5), intraabdominal esophageal position is corroborated, proceeds to perform Dor type plasty, making 2 simple points with Ethibon # 2, gastric fundus to right pillar (figure 6). The patient presented improvement in her ventilatory pattern during the surgery, she managed to intubate without complications, started orally at 8 h post surgery, and tolerated the progression to the same, a postoperative esophagogram was performed in which abdominal fundoplication was observed, without stenosis or leakage (figure 7), the patient is discharged 24 hrs after surgery.
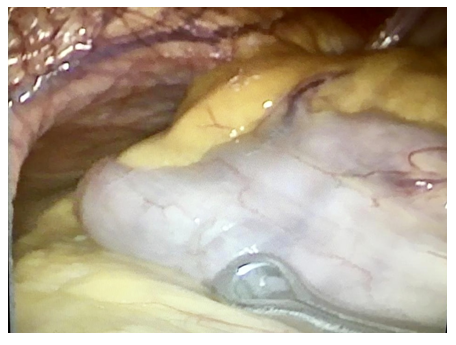
Figure 1: Transverse colon coming out from thorax.
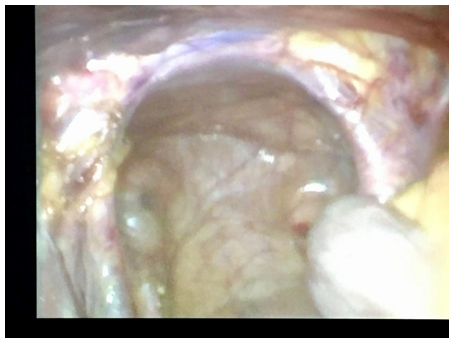
Figure 2: Real defect, after pulling down colon, stomach and jejunum. Size 10cm aprox

Figure 3: Dor fundoplication done.
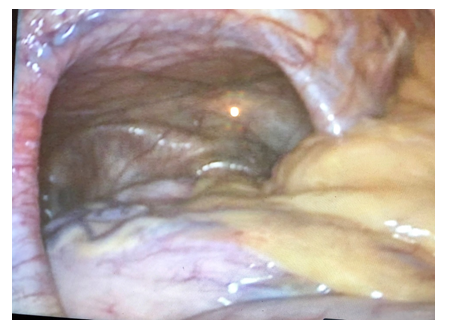
Figure 4: All the stomach inside the hiatus defect
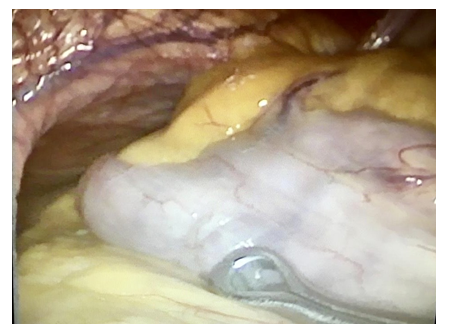
Figure 5:
Discussion
Paraesophageal hernia is rare and uncommon, however the management of asymptomatic patients is not clear since the risk of progressing to symptomatic hernia is 14% per year, and the risk of requiring emergency surgery is not greater than 2% annual [5]. Due to the rareness of the pathology and lack of randomized studies comparing different types of surgical management, there is controversy about which should be the choice, transabdominal vs trans.toracic, open vs laparoscopic, hiatus closure with suture vs mesh use and when fundoplication is necessary [6,7]. Historically, hiatus surgery was performed by thoracotomy and / or laparotomy, however the results of several series have shown that Laparoscopic repair is feasible and safe with immediate results and with comparable recurrence with open surgery in expert hands, becoming the approach of choice for its repair [8,9].
As demonstrated by Draaisma at al. in their review of the literature compared the 2 approaches in paraesophageal hernia surgery, reporting a shorter hospital stay in the laparoscopic group (3 days vs 10 days) and lower morbidity (4.3% vs 16.3% respectively) [10].
Despite the controversies, in practice there are certain guidelines for laparoscopic hiatal hernia repair, such as: reduction of the hernial sac and contents, dissection of crura and esophagogastric junction, re-approximation of tension-free hiatus, and 3cm of intrA-abdominal esophagus [11].
As demonstrated in a meta-analysis of 5 randomized clinical trials, in which partial fundoplication (n = 227) vs total (n = 231) were compared and reported that esophageal acid exposure (SMD), 0.19 , P = 0.15), esophagitis (19% goes 13%, P = 0.34), heartburn score (SMD, 1.27, P = 0.13), average dilatation (1.4% vs. 2.8%, P = 0.39), reoperation (5.7 % vs. 2.8%, P = 0.13), regurgitation, use of pump inhibitors, LES pressure, and satisfaction of patients with partial fundoplication was similar to patients with total fundoplication at 1 year post-surgery [12].
In addition, 5 years after surgery, the Dakkak dysphagia score, flatulence, inability to burp, inability to relieve distension were lower after partial fundoplication, while the reflux score, average dilatation, re-operation rate, use of Pump inhibitor and patient satisfaction was similar [13].
A meta-analysis of 7 randomized clinical studies comparing anterior fundoplication (n = 345) vs posterior (n = 338) reported esophageal acid exposure (3.3% vs. 0.8%, P <0.001), heartburn (21% vs. 8%, P <0.001), and re-intervention rate (8% vs. 4%, P = 0.06) were higher in the short-term anterior fundoplication. On the other hand, the Dakkak dysphagia score (2.5 vs. 5.7, P <0.001) was lower in the anterior fundoplication. Esophagitis, regurgitation and perioperative results were similar. In the long term, heartburn (31% vs. 14%, P <0.001), use of pump inhibitor (25% vs. 10%, P = 0.002), and re-operation rate (10% vs. 5%, P = 0.03) were higher in the anterior fundoplication, while the Dakkak dysphagia score and the inability to burp, distension and patient satisfaction were similar [14].
The use of meshes is a topic of discussion among surgeons, where certain studies have shown that, with the use of prosthetic material for hiatus closure, a lower recurrence rate is obtained [15]; However, its use is not exempt from complications such as adhesion formation, mesh shrinkage, foreign body reaction, and tissue erosion caused by surgical intervention, as demonstrated by Stadlhuber et al. [7,16]; in addition to late dysphagia, a prevalence of up to 13% was reported [17].
Alberto Chousleb et al; recommend that in patients with giant paraesophageal hernia repair with mesh when the abutments are thinned or the suture line is under tension, however in our patient the tissues were lax, a tension-free closure was performed [18].
Due to the fact that in our case there was no complete gastroesophageal reflux disease protocol and because the patient was admitted to surgery as an emergency, total fundoplication was not performed, since it is contraindicated in patients with motor disorders, reason why it was decided to perform a Dorr-type plasty to avoid post-surgical dysphagia. At 6-month follow-up, the patient is asymptomatic, with an adequate quality of life without heartburn or regurgitation.
Conclusions
We conclude that in the paraesophageal hernia type IV, in which there are doubts about the ideal approach, it is safe to perform the procedure laparoscopically, since in trained hands, it is a safe procedure even as emergency surgery, also with the benefits of being a minimally invasive procedure, such as shorter hospital stay, less pain, less morbidity and mortality, recovery and early normal life, better aesthetic results, and a lower metabolic response to trauma that is very important in elderly patients with previous comorbidities as in our patient. In addition, the use of meshes is not mandatory in all hiatus defects, since each case must be individualized and it is safe to perform the hiatus plasty without them.
Conflict of interest
We do not have any conflict of interest.
References
- Arafat FO, Teitelbaum EN, Hungness ES. Modern treatment of paraesophageal hernia: preoperative evaluation and technique for laparoscopic repair. Surg Laparosc Endosc Percutan Tech 22 (2012): 297-303.
- Steve RS, James PD, John GH. Modern diagnosis and treatment of hiatal hernias. Langenbecks Arch Surg. 402 (2017): 1145-1151.
- Jesus Villegas-Talavera. Hernia paraesofagica tipo vi gigante: presentación de caso y revisión de literatura, Rev Med Hosp Gen Mex 75 (2012): 37-40.
- Peters JH. SAGES guidelines for the management of hiatal hernia. Surg Endosc 27 (2013): 4407-4408
- Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal hernias: operation or observation? Ann Surg 236 (2002): 492-500.
- Livingston CD, Jones HL, Askew RE, et al. Laparoscopic hiatal hernia repair in patients with poor esophageal motility or paraesophageal herniation. Am Surg 67 (2001): 987-991.
- Davis SS Jr. Current controversies in paraesophageal hernia repair. Surg Clin North Am 88 (2008): 959-978.
- Mumnoon H, Atif I, Vanessa S, et al. Filipi Surgical repair of recurrent hiatal hernia. Hernia 10 (2006): 13-19.
- Dimitry O, Jennifer M. Paraesophageal hernia. Surg Clin N Am 95 (2015) 555-565.
- Draaisma WA, Gooszen HG, Tournoij E, et al. Controversies in paraesophageal hernia repair: a review of literature. Surg Endosc 19 (2005): 1300-1308.
- Oleynikov D, Ranade A, Parcells J, et al. Paraesophageal Hernias and Nissen Fundoplication. In: Oleynikov D, Bills ND, editors. Robotic Surgery for the General Surgeon, Chapter 6. Hauppauge (NY): Nova Science Publishers (2014): 65-74.
- Broeders JA, Roks DJ, Ahmed AU, et al. Laparoscopic anterior 180-degree versus nissen fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis of randomized clinical trials. Ann Surg 257 (2013): 850-859.
- Broeders JA, Roks DJ, Jamieson GG, et al. Five-year outcome after laparoscopic anterior partial versus Nissen fundoplication: four randomized trials. Ann Surg 255 (2012): 637-642.
- Broeders JA, Roks DJ, Ahmed Ali U, et al. Laparoscopic anterior versus posterior fundoplication for gastroesophageal reflux disease: systematic review and meta-analysis of randomized clinical trials. Ann Surg 254 (2011): 39-47.
- Granderath FA, Carlson MA, Champion JK, et al. Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 20 (2006): 367-379.
- Stadlhuber RJ, Sherif AE, Mittal SK, et al. Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 23 (2009): 1219-1226.
- Antoniou SA, Pointner R, Granderath FA. Hiatal hernia repair with the use of biologic meshes: a literature review. Surg Laparosc Endosc Percutan Tech 21 (2011): 1-9.
- Alberto C, Samuel S, Soni C. Complicaciones de cirugía antirreflujo. Complicaciones en cirugia laparoscopica y toracoscopica, primera edición 8 (2007) 87-102.
