Klebsiella Pneumoniae Producing Extended-Spectrum Β-Lactamases seen in the Laboratory of the University Hospital of Befelatanana Antananarivo Madagascar
Article Information
Fidiniaina Mamy Randriatsarafara1, Zafindrasoa Domoina Rakotovao-Ravahatra2*, Njaramahery Williame Andriamampandry3, Andriamiadana Luc Rakotovao4
1Public Health Specialist. Public Health Department of the Faculty of Medicine Antananarivo, Madagascar
2Biologist doctor. Laboratory of Joseph Raseta Befelatanana University Hospital Antananarivo, Madagascar
3Medical Student. Laboratory of Joseph Raseta Befelatanana University Hospital Antananarivo, Madagascar
4Professor in biological hematology. Medical Biology Department of the Faculty of Medicine Antananarivo, Madagascar
*Corresponding Author: Zafindrasoa Domoina Rakotovao-Ravahatra, Laboratory of Joseph Raseta Befelatanana University Hospital Antananarivo, Madagascar
Received: 21 September 2021; Accepted: 27 September 2021; Published: 06 October 2021
Citation: Fidiniaina Mamy Randriatsarafara, Zafindrasoa Domoina Rakotovao-Ravahatra, Njaramahery Williame Andriamampandry, Andriamiadana Luc Rakotovao. Klebsiella Pneumoniae Producing Extended-Spectrum Β-Lactamases seen in the Laboratory of the University Hospital of Befelatanana Antananarivo Madagascar. Journal of Environmental Science and Public Health 5 (2021): 424-432.
Share at FacebookAbstract
Background: Klebsiella pneumoniae producing extended-spectrum β-lactamases is an important nosocomial pathogen. The objective of this study is to describe the factors associated with Klebsiella pneumoniae producing extended-spectrum β-lactamases infections.
Methods: It is a prospective study of 113 isolates of K. pneumonia for a period of 18 months from January 2020 to June 2021 in the laboratory of the University Hospitals of Befelatanana.
Results: Among 113 isolates of Klebsiella pneu-moniae, 78 (69%) were represented by Klebsiella pneumoniae producing extended-spectrum β-lactamases. Men (79.3%;p=0.01), subjects less than 20 years (85.2%; p=0.001), and with infectious syndrome (77.9%; p= 0.002) were the most affected by Klebsiella pneumoniae producing extended-spectrum β-lactamases infections. Among these subjects, newborns hospitalized in intensive care units (75%;p=0.01) were the most affected by these infections. Moreover, these infections were more common in summer (69.1%; p=10-2).
Conclusion: Strict hygiene measures are very important in hospital wards to fight against these Klebsiella pneumoniae producing extended-spectrum β-lactamases, especially in neonatal intensive care units.
Keywords
Klebsiella pneumoniae; Infection; Beta-lactamases
Klebsiella pneumoniae articles; Infection articles; Beta-lactamases articles
Klebsiella pneumoniae articles Klebsiella pneumoniae Research articles Klebsiella pneumoniae review articles Klebsiella pneumoniae PubMed articles Klebsiella pneumoniae PubMed Central articles Klebsiella pneumoniae 2023 articles Klebsiella pneumoniae 2024 articles Klebsiella pneumoniae Scopus articles Klebsiella pneumoniae impact factor journals Klebsiella pneumoniae Scopus journals Klebsiella pneumoniae PubMed journals Klebsiella pneumoniae medical journals Klebsiella pneumoniae free journals Klebsiella pneumoniae best journals Klebsiella pneumoniae top journals Klebsiella pneumoniae free medical journals Klebsiella pneumoniae famous journals Klebsiella pneumoniae Google Scholar indexed journals Infection articles Infection Research articles Infection review articles Infection PubMed articles Infection PubMed Central articles Infection 2023 articles Infection 2024 articles Infection Scopus articles Infection impact factor journals Infection Scopus journals Infection PubMed journals Infection medical journals Infection free journals Infection best journals Infection top journals Infection free medical journals Infection famous journals Infection Google Scholar indexed journals Beta-lactamases articles Beta-lactamases Research articles Beta-lactamases review articles Beta-lactamases PubMed articles Beta-lactamases PubMed Central articles Beta-lactamases 2023 articles Beta-lactamases 2024 articles Beta-lactamases Scopus articles Beta-lactamases impact factor journals Beta-lactamases Scopus journals Beta-lactamases PubMed journals Beta-lactamases medical journals Beta-lactamases free journals Beta-lactamases best journals Beta-lactamases top journals Beta-lactamases free medical journals Beta-lactamases famous journals Beta-lactamases Google Scholar indexed journals bacterial infections articles bacterial infections Research articles bacterial infections review articles bacterial infections PubMed articles bacterial infections PubMed Central articles bacterial infections 2023 articles bacterial infections 2024 articles bacterial infections Scopus articles bacterial infections impact factor journals bacterial infections Scopus journals bacterial infections PubMed journals bacterial infections medical journals bacterial infections free journals bacterial infections best journals bacterial infections top journals bacterial infections free medical journals bacterial infections famous journals bacterial infections Google Scholar indexed journals hygiene articles hygiene Research articles hygiene review articles hygiene PubMed articles hygiene PubMed Central articles hygiene 2023 articles hygiene 2024 articles hygiene Scopus articles hygiene impact factor journals hygiene Scopus journals hygiene PubMed journals hygiene medical journals hygiene free journals hygiene best journals hygiene top journals hygiene free medical journals hygiene famous journals hygiene Google Scholar indexed journals β-lactamases articles β-lactamases Research articles β-lactamases review articles β-lactamases PubMed articles β-lactamases PubMed Central articles β-lactamases 2023 articles β-lactamases 2024 articles β-lactamases Scopus articles β-lactamases impact factor journals β-lactamases Scopus journals β-lactamases PubMed journals β-lactamases medical journals β-lactamases free journals β-lactamases best journals β-lactamases top journals β-lactamases free medical journals β-lactamases famous journals β-lactamases Google Scholar indexed journals infections articles infections Research articles infections review articles infections PubMed articles infections PubMed Central articles infections 2023 articles infections 2024 articles infections Scopus articles infections impact factor journals infections Scopus journals infections PubMed journals infections medical journals infections free journals infections best journals infections top journals infections free medical journals infections famous journals infections Google Scholar indexed journals pneumoniae articles pneumoniae Research articles pneumoniae review articles pneumoniae PubMed articles pneumoniae PubMed Central articles pneumoniae 2023 articles pneumoniae 2024 articles pneumoniae Scopus articles pneumoniae impact factor journals pneumoniae Scopus journals pneumoniae PubMed journals pneumoniae medical journals pneumoniae free journals pneumoniae best journals pneumoniae top journals pneumoniae free medical journals pneumoniae famous journals pneumoniae Google Scholar indexed journals antibiotics articles antibiotics Research articles antibiotics review articles antibiotics PubMed articles antibiotics PubMed Central articles antibiotics 2023 articles antibiotics 2024 articles antibiotics Scopus articles antibiotics impact factor journals antibiotics Scopus journals antibiotics PubMed journals antibiotics medical journals antibiotics free journals antibiotics best journals antibiotics top journals antibiotics free medical journals antibiotics famous journals antibiotics Google Scholar indexed journals
Article Details
1. Introduction
Over the four past decades, the worldwide spread of extended-spectrum β-lactamases Enterobacterales has become a significant threat [1-3]. The recent emergence of carbapenem-resistant Enterobacterales has further restricted antimicrobial treatment options and has amplified the threat to public health [4]. Carbapenem-resistant and extended-spectrum β-lactamases-producing Enterobacterales are in the WHO priority pathogens list for research and development of new antibiotics [5]. Among Enterobacterales, K. pneumonia producing extended-spectrum β-lactamases (ESBL-Kp) is an important nosocomial pathogen with the potential to cause serious infectious diseases such as bacteremia and pneumonia [6-8]. Recently multi-drug-resistant K. pneumoniae emergence has led to incurable infections [9-12]. In the last 15 years, the proportion of K. pneumoniae isolates from bloodstream infections resistant to third-generation cephalosporins increased from 4% (in 2005) to 29% (in 2017) with more than 80% of this resistance being due to ESBL production [13]. On the other hand the proportion of carbapenem-resistant K. pneumoniae was to 1% in 2019 [14]. In order to improve the management of K. pneumoniae infections, the objective of this study is to describe the factors associated with ESBL-Kp infections in hospitals.
2. Materials and Methods
2.1 Type of study
It is a prospective study of 113 isolates of K. pneumonia for a period of 18 months from January 2020 to June 2021 in the laboratory of the University Hospitals of Befelatanana.
2.2 Inclusion and exclusion criteria
This study includes all patients who have applied for a bacteriological examination during the study period with bacterial K.pneumoniae infections. This study excluded non-compliant samples during the study and patients with bacterial infections other than K.pneumoniae infections.
2.3 Study variables
The dependent variable was constituted by the positivity of the microbiological culture identifying ESBLs- producing K. pneumoniae in an antibiogram. The independent variables were constituted by the associated factors with K. pneumoniae infections.
2.4 Sample collection
Samples were collected in sterile vials (stool, urine and respiratory samples), swabs (pus), sterile tube (pleural fluid, ascites fluid, cerebrospinal fluid and other fluids) or blood culture bottles. The samples were transported quickly to the laboratory (less than 2 hours of transport) at room temperature.
2.5 Bacterial culture
Specific culture media were used according to each type of sample (for examples: blood agar, chocolate agar, brain heart broth….), associated with a chromogenic culture medium (Uriselect® supplied by Bio-Rad company) to specifically identify the enterobacteria.
2.6 Bacterial identification
When Klebsiella colonies grew in uriselect® agar, they were identified by colony color (dark blue), microscopic appearances after gram staining (gram negative bacilli) and identification test results. The specific identification tests for Klebsiella were the oxidase test (negative) and the Api 20E® strips (manufactured by bioMérieux company). These strips were identified the species K. pneumonia.
2.7 Antibiotic resistance test
For the antibiogram, discs of antibiotics (brand OXOID® supplied by Termo Fisher Scientific company) were used. Resistance to antibiotics was determined by the Mueller / Hinton agar diffusion method, according to the recommendations of the “comité de l'antibiogramme de la société française de Microbiologie”(Société Française de Microbiologie, 2019) [15]. Mueller / Hinton agar were provided by Rapid Labs Company. The detection of ESBLs was carried out by a method of synergy between the clavulanic acid of the AMC and ceftriaxone or else cefotaxime, characterized by a“champagne cork” image and signs the presence of an ESBLs [16]. Study parameters were the gender, the age, the clinical information, the departments, the types of sampling and the seasons.
2.8 Ethical considerations
This study was authorized by the Director of Establishment and Department Head of laboratory of the University Hospital of Befelatanana before its implementation. Notion of anonymity and confidentiality were respected.
2.9 Statistical analysis
The data entry and processing was performed on the software Epi-info 3.5.2. The comparison of percentages used the Chi-square tests. The statistical significance threshold used was p = 0.05.
3. Results
Among 113 isolates of K.pneumoniae, 78 (69%) were represented by ESBL-Kp (Figure 1).
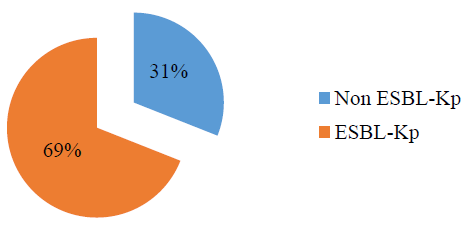
Figure 1: Microbiological results of bacteriological cultures.
|
Associated factors |
Non ESBL-Kp (n=35) |
ESBL-Kp (n=78) |
Total (N=113) |
p- value |
|||
|
n |
% |
n |
% |
||||
|
Age (years) |
20-39 |
4 |
44,4 |
5 |
55,6 |
9 |
0,001 |
|
40-59 |
3 |
18,8 |
10 |
62,5 |
16 |
||
|
≥ 60 |
16 |
59,3 |
11 |
40,7 |
27 |
||
|
<20 |
12 |
19,7 |
52 |
85,2 |
61 |
||
|
Gender |
Female |
23 |
41,8 |
32 |
58,2 |
55 |
0,01 |
|
Male |
12 |
20,7 |
46 |
79,3 |
58 |
||
|
Clinical Information |
Infectious syndrome |
17 |
22,1 |
60 |
77,9 |
77 |
0,002 |
|
Others |
18 |
50,0 |
18 |
50,0 |
36 |
||
|
Departments |
Neonatal resuscitation |
21 |
25 |
63 |
75 |
84 |
0,01 |
|
Others (surgery, pediatrics, internal medicine) |
14 |
48,3 |
15 |
51,7 |
29 |
||
|
Season |
Summer |
30 |
30,9 |
67 |
69,1 |
97 |
10-2 |
|
Winter |
5 |
31,3 |
11 |
68,8 |
16 |
||
Table 1: Associated factors with ESBL-Kp infections.
Men (79.3%;p=0.01), subjects less than 20 years (85.2%; p=0.001), and with infectious syndrome (77.9%; p= 0.002) were the most affected by ESBL-Kp infections. Among these subjects, newborns hospitalized in intensive care units (75%;p=0.01) were the most affected by these infections. Moreover, these infections were more common in summer (69.1%; p=10-2) (Table 1).
4. Discussion
ESBLs induce bacterial resistance by hydrolyzing penicillins, first, second, and third generation cephalosporins and aztreonam, but not cephamycins or carbapenems. β -lactamase inhibitors such as, clavulanic acid, sulbactam, and tazobactam usually inhibit them. Most ESBLs are derived from broad-spectrum β -lactamases TEM-1 and SHV-1. Mutations of these genes result in alteration of the amino acid configuration around the active site of β -lactamases. Genes for ESBL are frequently encoded by plasmids [17]. Several class of ESBLs have been described in K. pneumoniae. ESBLs that derived from penicillinases TEM and SHV emerged in the 1980s and CTX-M type enzymes such as CTX-M-15 have arisen during the 2000s [18]. This change reflects an important capacity for gene transfer, possibly between epidemic clones [19-21]. The pandemic clones ST258, ST11, ST15, and ST147 spread since two decades and recently, the CTX-M-15-producing ST307 clone emerged globally [22]. Most hospital outbreaks are due to this multidrug-resistant K. pneumoniae clones [22-24]. The emergence of carbapenem-resistant strains further complicates the management of these infections [25].
This study showed 69% isolates of ESBL-Kp. This rate is low compared to that of a study in Côte d’Ivoire which found 84% of ESBL-Kp [26]. Indeed, not all patients with bacterial infections have laboratory tests explaining the lower rate compared to this study. Moreover, this rate is high compared to that of a study in Tunisia which found 20.2% of ESBL-Kp [27]. This study showed that more than half of the K. pneumoniae isolates were ESBL-Kp thus representing multi-resistant bacteria. And all these bacteria have been found in hospital patients. In France, K. pneumoniae is the 5th most prevalent pathogen responsible for healthcare-associated infection [28]. In the last 15 years, the proportion of K. pneumoniae isolates from bloodstream infections resistant to third-generation cephalosporins increased from 4% (in 2005) to 29% (in 2017) with more than 80% of this resistance being due to ESBL production [29]. On the other hand the proportion of carbapenem-resistant K. pneumoniae was to 1% in 2019 [30]. This situation is worrying and health workers should take strict measures to limit the spread of these multi-resistant bacteria.
Concerning the associated factors with ESBL-Kp infections, men were the most affected with a significant difference. Men are more likely to work outside the home compared to women and are more exposed to pathogens, probably explaining this difference. The infectious syndrome was the most frequent clinical information in patients because ESBL bacteria are very resistant and the infection always manifests itself by more or less marked symptoms. Subjects less than 20 years in particular children and newborns hospitalized in intensive care units were the most affected by these infections representing 75% of cases. According to a study carried out in Kazan, in neonates with sepsis, testing of K. pneumoniae isolates for ESBL production was positive in 60% of cases and in neonates with UTI-in 40% of cases [31].The prevalence of virulent strains of K. pneumoniae among neonates with sepsis and other neonatal infection is higher than we think. The most severe forms of neonatal sepsis with an unfavorable outcome were due to virulent strains of K. pneumoniae. According to a study carried out by Naas et al in Madagascar, neonates are exposed to external risks factors, particularly deficient hygiene that put them at high risk of neonatal infection and if neonatal culture confirmed sepsis rates is of 1-3 per 1000 live births reported from industrialized countries, this rate can reached 37 per 1000 live births in developing countries. Poor quality of care in developing countries are a major source of neonatal infections for hospital-born infants. Lack of infection-control procedures, inadequate sterilization of multiuse instruments, understaffing and overcrowded nurseries are responsible for nosocomial infections in most hospitals in developing countries and promotes neonatal infections due to environmental pathogens as reflected in this study by the positivity of the gastric samples cultures with E. cloacae and K. pneumonia [32].
Moreover, these infections were more common in summer in this study. Another study also showed that ESBL bacteria are more common in summer than in winter [33]. This is logical since the majority of bacteria only grow during incubation at 37 °C in an incubator in the laboratory. Thus, their growth is favorable at a high temperature.
At the end of this article, we recommend improving hygiene measures in hospital services, especially neonatal intensive care units, in order to fight against the spread of these ESBL-Kp. Likewise, bacteriological examinations in the laboratory should be carried out as much as possible, especially during the summer when bacteria grow more rapidly.
5. Conclusion
This study highlighted the high rate of ESBL-Kp in hospitals, especially in neonatal intensive care units. Men were more exposed compared to women probably because of their work. And these infections were more common in the summer. Thus, hygiene measures should be improved in inpatient and neonatal intensive care units. Likewise, bacteriological examinations with antibiogram should be carried out quickly in case of suspicion of bacterial infection to ensure rapid management in order to improve the life expectancy of patients.
Acknowledgements
We would like to thank all the staff of the laboratory of University Hospital of Befelatanana and all the laboratory technicians. Similarly, we would like to express our gratitude to the director of establishment for authorizing us to carry out this study.
Conflicts of Interest
The authors do not declare any conflict of interest.
References
- Paterson DL, Bonomo RA. Extended-spectrum β-lactamases: a clinical update. Clinical Microbiology Reviews 18 (2005): 657-686.
- Pitout JD, Laupland KB. Extended-spectrum β-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infectious Diseases 8 (2008) : 159-166.
- Tal Jasper R, Coyle JR, Katz DE, et al. The complex epidemiology of extended-spectrum β-lactamase-producing Enterobacteriaceae. Future Microbiology 10 (2015) : 819-839.
- Pitout JD, Nordmann P, Poirel L. Carbapenemase-producing Klebsiella pneumoniae, a key pathogen set for global nosocomial dominance. Antimicrobial Agents and Chemotherapy 59 ( 2015) : 5873-5884.
- World Health Organisation. News release (2017).
- Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clinical Microbiology Reviews 11 (1998): 589-603.
- Gupta A, Ampofo K, Rubenstein D, et al. Extended spectrum β-lactamase-producing Klebsiella pneumoniae infections: a review of the literature. Journal of Perinatology 23 (2003) : 439-443.
- Becker L, Fuchs S, Pfeifer Y, et al. Whole genome sequence analysis of CTX-M-15 producing Klebsiella isolates allowed dissecting a polyclonal outbreak scenario. Frontiers in Microbiology 9 (2018): 322.
- Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infectious Diseases 9 (2009): 228-236.
- Bowers JR, Kitchel B, Driebe EM, et al. Genomic analysis of the emergence and rapid global dissemination of the clonal group 258 Klebsiella pneumoniae PLoS One 10 (2015): e0133727.
- Paczosa MK, Mecsas J. Klebsiella pneumoniae: going on the offense with a strong defense. Microbiology and Molecular Biology Reviews 80 (2016) : 629-661.
- Dong N, Zhang R, Liu L, et al. Genome analysis of clinical multilocus sequence Type 11 Klebsiella pneumoniae from China. Microbial Genomics 4 (2018) : 1-12.
- Santé publique France. EARS-Net France, 2002-2017 (2019).
- European Centre for Disease Prevention and Control. Surveillance Atlas of Infectious Diseases (2021).
- Société Française de Microbiologie. Tables of critical concentrations for the interpretation of MICs and critical diameters of inhibition zones. In: CASFM / EUCAST: Société Française de Microbiologie (2019): 38-34.
- Sbiti M, Lahmadi K, Louzi L. Epidemiological profile of uropathogenic enterobacteria producing extended spectrum beta-lactamases. Pan African Medical Journal 28 (2017): 9.
- Dolma K, Summerlin TL, Wongprasert H, et al. Early-Onset Neonatal Sepsis with Extended Spectrum Beta-Lactamase Producing Escherichia Coli in Infants Born to South and South East Asian Immigrants: A Case Series. American Journal of Perinatology Reports 8 (2018): e277-e279.
- Liu H, Wang Y, Wang G, et al. The prevalence of Escherichia coli strains with extended spectrum β-lactamases isolated in China. Frontiers in Microbiology 6 (2015) : 335.
- Canton R, Gonzalez-Alba JM, Galan JC. CTX-M enzymes: origin and diffusion. Frontiers in Microbiology 3 (2012): 110.
- Woodford N, Turton JF, Livermore DM. Multiresistant Gram-negative bacteria: the role of high-risk clones in the dissemination of antibiotic resistance. FEMS Microbiology Reviews 35 (2011): 736-755.
- Elhani D, Bakir L, Aouni M. The changing epidemiology of extended spectrum β-lactamase-producing Klebsiella pneumoniae. Annales de Biologie Clinique 69 (2011): 523-529.
- Wyres KL, Hawkey J, Hetland MAK, et al. Emergence and rapid global dissemination of CTX-M-15-associated Klebsiella pneumoniae strain ST307. Journal of Antimicrobial Chemotherapy 74 (2019): 577-581.
- Lee MY, Ko KS, Kang CI, et al. High prevalence of CTX-M-15-producing Klebsiella pneumoniae isolates in Asian countries: diverse clones and clonal dissemination. International Journal of Antimicrobial Agents 38 (2011): 160-163.
- Rodrigues C, Machado E, Ramos H, et al. Expansion of ESBL-producing Klebsiella pneumoniae in hospitalized patients: a successful story of international clones (ST15, ST147, ST336) and epidemic plasmids (IncR, IncFIIK). International Journal of Medical Microbiology 304 (2014): 1100-1108.
- Bonura C, Giuffre M, Aleo A, et al. An update of the evolving epidemic of blaKPC carrying Klebsiella pneumoniae in Sicily, Italy, 2014: emergence of multiple non-ST258 clones. PLoS One 10 (2015): 1-9.
- Müller-Schulte E, Tuo MN, Akoua-Koffi C, et al. High prevalence of ESBL-producing Klebsiella pneumoniae in clinical samples from central Côte d’Ivoire. International journal of infectious diseases 91 (2020): 207-209.
- Khalifa ABH, Khedher M. Epidemiological study of Klebsiella spp. uropathogenic strains producing extended-spectrum β-lactamase in a Tunisian university hospital. Pathologie biologie 60 (2012): e1-e5.
- Santé publique France. Enquête nationale de prévalence des infections nosocomiales et des traitements anti-infectieux en établissements de santé, mai-juin 2017 (2019).
- Sante ´ publique France. EARS-Net France, 2002–2017 (2019).
- European Centre for Disease Prevention and Control. Surveillance Atlas of Infectious Diseases (2021).
- Khaertynov KS, Anokhin VA, Rizvanov AA, et al. Virulence Factors and Antibiotic Resistance of Klebsiella pneumonia Strains Isolated From Neonates with Sepsis. Frontiers in Medicine 5 (2018): 1-9.
- Naas T, Cuzon G, Robinson AL, et al. Neonatal infections with multidrug-resistant ESBL-producing E. cloacae, K. pneumoniae in Neonatal Units of two different Hospitals in Antananarivo, Madagascar. BMC Infectious Diseases 16 (2016).
- Kaier K, Frank U, Conrad A, et al. Seasonal and ascending trends in the incidence of carriage of extended-spectrum ß-lactamase-producing Escherichia coli and Klebsiella species in 2 German hospitals. Infection Control and Hospital Epidemiology 31 (2010): 1154-1159.
