Isolated Palpebral Tuberculosis
Article Information
Rafanomezantsoa Rindra1*, Miray Louis De Gonzague2, Rakotonirina Vero Herinjaka Dinaniaina3, Ramanarivo Norotiana Mihaja4, Rakotoarivelo Rivonirina Andry5, Raobela Léa6.
1Ophthalmologist, Ophthalmology Department, University hospital Joseph Ravoahangy, Andrianavalona Antananarivo Madagascar
2Ophthalmologist, Ophthalmology Department, University hospital Tambohobe Fianarantsoa Madagascar
3Ophthalmologist, Ophthalmology Department, University Hospital PZAGA Mahajanga Madagascar,
4Specialist in occupational Health at public health Department Analakely Antanananarivo Madagascar.
5Associate Professor, head of infectious disease Department, University hospital Tambohobe Fianarantsoa Madagascar
6Associate Professor, head of ophthalmology department, University hospital Joseph Ravoahangy Andrianavalona Antananarivo Madagascar
*Corresponding Author: Miray Louis de Gonzague, Ophthalmologist, Ophthalmology Department, University hospital Tambohobe Fianarantsoa
Received: 26 May 2021; Accepted: 4 June 2021; Published: 15 June 2021
Citation: Miray Louis De Gonzague, Rafanomezantsoa Rindra, Rakotonirina Vero Herinjaka Dinaniaina, Ramanarivo Norotiana Mihaja, Rakotoarivelo Rivonirina Andry, Raobela Léa. Isolated Palpebral Tuberculosis. Journal of Ophthalmology and Research 4 (2021): 199-204.
Share at FacebookAbstract
Tuberculosis is highly prevalent in Madagascar and virtually all the patients were infected in the cours of their childhood. Cutaneous tuberculosis is a rare condition which accounts for 1% to 2% of all cases of tuberculosis. Worldwide eyelid tuberculosis is underreported in Madagascar. We report a case of 13-year-old male patient presenting a prolapsed granuloma and papillomatous lesion in external part of the right upper eyelid conjunctiva. Histopathological findings show Malpighian epithelium ulceration. The chorion was the site of granulomatous inflammatory infiltrate, epithelioid with giant cells in hematoxylin and eosin stain. There were no granulomas, caseous necrosis. The diagnosis of follicular tuberculosis is posed. An excellent response was seen with antitubercular therapy with complete eyelid wound healing. In the face of chronic lesion of eyelid, including granuloma, ulcer as well as a swelling even a lesion mimicking a chalazion, histology is crucial to detect tuberculosis.
Keywords
granuloma; papillomatous lesion
Article Details
1. Introduction
Tuberculosis remains a public health problem in Madagascar [1]. Tuberculosis is highly prevalent in Madagascar and most patients are infected in the course of their childhood [2]. Worldwide, cutaneous TB comprises 1% to 2% of all cases of TB [3]. Cutaneous tuberculosis is a rare condition which accounts for between 0.5 and 2% of all Extrapulmonary Tuberculosis EPTB cases in developed countries [4]. Whereas eyelid tuberculosis is uncommon in Madagascar and underreported. For a period of 36 months retrospective study conducted in Fianarantsoa, 448(60,7%) cases of extrapulmonary were detected, there was no case of palpebral localisation[5]. Here in we report a case of 13-year-old male patient presenting an isolated palpebral tuberculosis.
2. Observation
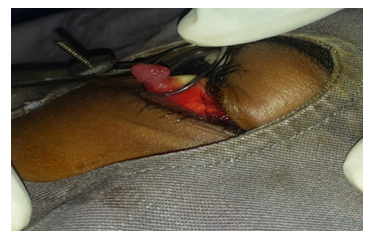
A 13-year-old immunocompetent male patient presented to the hospital with chief complaints of tumefaction over left eyelid for 5 months.The patient did not complain about There was no pain nor vision loss. There was no record of tuberculosis.He was vaccined completely.There was record of complete exeresis of the tumor located at the same place without anatomopathological finding, associated with application of corticosteroid ointment 45 days before his admission. Despite the treatment, there was a reccurence of the lesion. Ophtalmological examination revealed a red prolapsed granuloma and papillomatous lesion of dimensions 9mm x 4mm in external part of the right upper eyelid conjunctiva on eversion (Figure 1.A, 1.B).
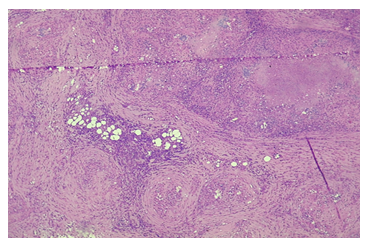
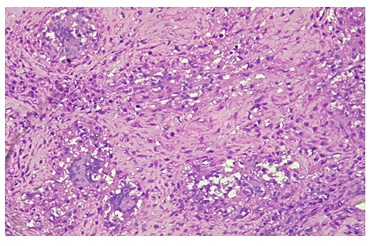
There were no regional lymph nodes on palpation. Chest X ray finding was apparently normal. The patient sustained a complete exercises of the lesion and the operative piece was submitted for histopathology. As a result, Malpighian epithelium was ulcerated. The chorion was the site of granulomatous inflammatory infiltrat, Epithelioid with giant cells in stain, hematoxylin, and eosin stain. Granulomas, and caseous necrosis were absent (Figure 2.A, 2.B). A diagnosis of follicular tuberculosis was made.
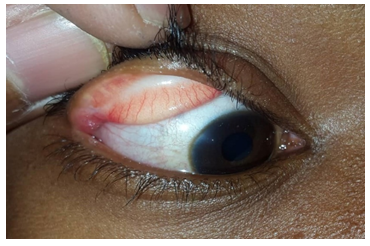
An excellent response was seen with antitubercular therapy with complete eyelid wound healing (Figure 3)
3. Discussion
Tuberculosis is highly prevalent in Madagascar and most patient were infected in course of childhood [1]. Eyelid localization appeared to be underreported. We presented a case of 13-year-old male patient suffering from a chronic recidivating granulomatous and papillomatous lesion of the conjunctiva of right upper eyelid. The histopathology unveiled the diagnoses of follicular Tuberculosis. Several manifestations of eyelid tuberculosis have been reported. Taneja et al reported a case of 6-year-old patient presenting a chronic swelling over left eyelid for 4 months with a record of antibiotherapy that did not improve the lesion. The histopathology confirms the diagnosis. Chest X ray showed an anomaly [6]. Besides, Mittal et al observed a 17-year-old patient presenting with a prolapsed granuloma of the lower lid of about 3 weeks’ duration mimicking a chalazion. Histopathology was not fulfilled. Inspite of, antibiotics, the wound healing was delayed. The histopathology confirmed the diagnosis of cutaneous tuberculosis at the end [7]. Our case did not present any symptome nor clinical manifestation like regional nodes and pulmonary lesion.
Although uncommon, tuberculosis also has skin manifestations, and the diagnosis is difficult to make [8]. In the face of chronic lesion of eyelid, including granuloma, ulcer as well as a swelling even a lesion mimicking a chalazion, histology is indispensable to detect tuberculosis. Malagasy ophthalmologist should be aware of the existence of this rare localization of TB, especially among children, because most people are infected in the course of their childhood in Madagascar.
4. Conclusion
In conclusion, although the incidence of cutaneous TB is rare. Through our case presentation, each ophthalmologist should be aware of the presence of eyelid tuberculosis even though it is underreported in Madagascar. In the face of suspect lesion including the chalaza, a routine histopathologic finding is of paramount importance. A research should be conducted in Madagascar to evaluate the incidence palpebral tuberculosis.
References:
- M Tiaray, J Rajaoarifetra, K Ravahatra, et al. Retreatment tuberculosis cases observed in Pulmonology Unit at the CHU Mahajanga, Madagascar (2008-2011) méd. Madag 5 (2015): 566-570.
- Razanamparany R, Ramarokoto H, Clouzeau J, et al. La tuberculose chez les enfants de moins de 11 ans: résistance primaire et variants génétiques dominants de Mycobacterium tuberculosis à AntananarivoArch Inst Pasteur de Madagascar 68 (2002): 41-44.
- Caminero J Guia de la. tuberculosis para medicos especialistas. Paris7 International Union against Tuberculosis and Respiratory Diseases (2003): p. 35- 37.
- Santos JB, Figueiredo AR, Ferraz CE, et al. Cutaneous tuberculosis:epidemiologic, etiopathogenic and clinical aspects. A Bras Dermatol 89 (2014): 219-228.
- JL Rakotoson, J Rajaoarifetra, H Raherimandimby, et al. Ralison. Issues du traitement de la tuberculose dans le service de Pneumo-phtisiologie du Centre Hospitalier Universitaire de Fianarantsoa, Madagascar. Rev. méd. Madag 3 (2013): 230-234.
- Taneja A, Taneja GK. Chronic Ulcerative Eyelid Lesion: A Rare Manifestation of Tuberculosis. Emerg Med (Los Angel) 8 (2018): 1.
- Mittal R, Tripathy D, Sharma S, et al. Tuberculosis of Eyelid Presenting as a Chalazion. Ophthalmology 120 (2013).
- Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clinics in Dermatology 25 (2007): 173.