Indications for Glenoid Bone Graft Surgery Associated with Favorable Functional Outcomes: A Systematic Review
Article Information
Paulo HS Lara*, Leandro M Ribeiro, Carlos V Andreoli, Alberto C Pochini, Paulo S Belangero, Benno Ejnisman
Center of Sports Medicine, Graduate Program in Medicine (Clinical Radiology), Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil
*Corresponding Author: Paulo Henrique Schmidt Lara, Center of Sports Medicine, Graduate Program in Medicine (Clinical Radiology), Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.
Received: 03 November 2023; Accepted: 15 November 2023 2023; Published: 20 November 2023
Citation: Paulo HS Lara, Leandro M Ribeiro, Carlos V Andreoli, Alberto C Pochini, Paulo S Belangero, Benno Ejnisman. Indications for Glenoid Bone Graft Surgery Associated with Favorable Functional Outcomes: A Systematic Review. Journal of Orthopedics and Sports Medicine. 5 (2023): 420-427.
Share at FacebookAbstract
Background: Bony lesions are prevalent in anterior shoulder instability and can be a signifivant cause of failure of stabilisation procedures if they are not adequately addressed. Determining the best surgical treatments for anterior shoulder instability is debatable, with several procedures developed over time. The bone block procedures showed a lower recurrence when compared to Bankart repair but a higher rate of complications.
Purpose: To determine group of indications for bone block procedures for anterior shoulder instability associated with better functional results. This will help in choosing this type of surgery appropriately for shoulder instability.
Study design: Systematic Review.
Methods: This systematic review was conducted in accordance with the International Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) guidelines. The studies were subdivided according to the main criteria used to indicate glenoid bone graft surgery, Radiological indications group (R), Radiological and clinical indications group (R + C) and Arthroscopic indications group (A). Only randomized clinical trials and prospective studies were included. The extracted and evaluated outcomes were: functional scores (ROWE, WOSI, Constant, SSV, SANE, and VAS).
Results: In the electronic search conducted in April 2022, 1567 articles were identified. After applying the inclusion criteria, a total of 23 articles were selected for the systematic review. Regarding the functional scores, we observed that group A had a greater number of statistically better results (Constant, SSV and VAS). Regarding the functional scores that are specific for shoulder instability, the group R was the group tha showed statisticatlly better results in the ROWE score (Group R;Mean: 91,9; Group R+C;Mean: 85,4; Group A: 83,3, p<0,001). This highlights the variability of the functional scores used to evaluate the results of bone grafting procedures. Conclusion: The radiographic indications group presented the better results in the specific score for shoulder instability and the arthroscopic indications group presented the better results in general and our systematic review is the first to determine indications for bone block procedures that would lead to better functional outcomes in prospective studies.
Keywords
Shoulder; Systematic review; Orthopedic surgery; Shoulder instability; Bone block procedures; Latarjet
Sports medicine articles Sports medicine Research articles Sports medicine review articles Sports medicine PubMed articles Sports medicine PubMed Central articles Sports medicine 2023 articles Sports medicine 2024 articles Sports medicine Scopus articles Sports medicine impact factor journals Sports medicine Scopus journals Sports medicine PubMed journals Sports medicine medical journals Sports medicine free journals Sports medicine best journals Sports medicine top journals Sports medicine free medical journals Sports medicine famous journals Sports medicine Google Scholar indexed journals Clinical radiology articles Clinical radiology Research articles Clinical radiology review articles Clinical radiology PubMed articles Clinical radiology PubMed Central articles Clinical radiology 2023 articles Clinical radiology 2024 articles Clinical radiology Scopus articles Clinical radiology impact factor journals Clinical radiology Scopus journals Clinical radiology PubMed journals Clinical radiology medical journals Clinical radiology free journals Clinical radiology best journals Clinical radiology top journals Clinical radiology free medical journals Clinical radiology famous journals Clinical radiology Google Scholar indexed journals Surgical treatments articles Surgical treatments Research articles Surgical treatments review articles Surgical treatments PubMed articles Surgical treatments PubMed Central articles Surgical treatments 2023 articles Surgical treatments 2024 articles Surgical treatments Scopus articles Surgical treatments impact factor journals Surgical treatments Scopus journals Surgical treatments PubMed journals Surgical treatments medical journals Surgical treatments free journals Surgical treatments best journals Surgical treatments top journals Surgical treatments free medical journals Surgical treatments famous journals Surgical treatments Google Scholar indexed journals Bankart repair articles Bankart repair Research articles Bankart repair review articles Bankart repair PubMed articles Bankart repair PubMed Central articles Bankart repair 2023 articles Bankart repair 2024 articles Bankart repair Scopus articles Bankart repair impact factor journals Bankart repair Scopus journals Bankart repair PubMed journals Bankart repair medical journals Bankart repair free journals Bankart repair best journals Bankart repair top journals Bankart repair free medical journals Bankart repair famous journals Bankart repair Google Scholar indexed journals Anterior shoulder instability articles Anterior shoulder instability Research articles Anterior shoulder instability review articles Anterior shoulder instability PubMed articles Anterior shoulder instability PubMed Central articles Anterior shoulder instability 2023 articles Anterior shoulder instability 2024 articles Anterior shoulder instability Scopus articles Anterior shoulder instability impact factor journals Anterior shoulder instability Scopus journals Anterior shoulder instability PubMed journals Anterior shoulder instability medical journals Anterior shoulder instability free journals Anterior shoulder instability best journals Anterior shoulder instability top journals Anterior shoulder instability free medical journals Anterior shoulder instability famous journals Anterior shoulder instability Google Scholar indexed journals Bone lesions articles Bone lesions Research articles Bone lesions review articles Bone lesions PubMed articles Bone lesions PubMed Central articles Bone lesions 2023 articles Bone lesions 2024 articles Bone lesions Scopus articles Bone lesions impact factor journals Bone lesions Scopus journals Bone lesions PubMed journals Bone lesions medical journals Bone lesions free journals Bone lesions best journals Bone lesions top journals Bone lesions free medical journals Bone lesions famous journals Bone lesions Google Scholar indexed journals Latarjet articles Latarjet Research articles Latarjet review articles Latarjet PubMed articles Latarjet PubMed Central articles Latarjet 2023 articles Latarjet 2024 articles Latarjet Scopus articles Latarjet impact factor journals Latarjet Scopus journals Latarjet PubMed journals Latarjet medical journals Latarjet free journals Latarjet best journals Latarjet top journals Latarjet free medical journals Latarjet famous journals Latarjet Google Scholar indexed journals Shoulder arthrosis articles Shoulder arthrosis Research articles Shoulder arthrosis review articles Shoulder arthrosis PubMed articles Shoulder arthrosis PubMed Central articles Shoulder arthrosis 2023 articles Shoulder arthrosis 2024 articles Shoulder arthrosis Scopus articles Shoulder arthrosis impact factor journals Shoulder arthrosis Scopus journals Shoulder arthrosis PubMed journals Shoulder arthrosis medical journals Shoulder arthrosis free journals Shoulder arthrosis best journals Shoulder arthrosis top journals Shoulder arthrosis free medical journals Shoulder arthrosis famous journals Shoulder arthrosis Google Scholar indexed journals Glenoid bone graft surgery articles Glenoid bone graft surgery Research articles Glenoid bone graft surgery review articles Glenoid bone graft surgery PubMed articles Glenoid bone graft surgery PubMed Central articles Glenoid bone graft surgery 2023 articles Glenoid bone graft surgery 2024 articles Glenoid bone graft surgery Scopus articles Glenoid bone graft surgery impact factor journals Glenoid bone graft surgery Scopus journals Glenoid bone graft surgery PubMed journals Glenoid bone graft surgery medical journals Glenoid bone graft surgery free journals Glenoid bone graft surgery best journals Glenoid bone graft surgery top journals Glenoid bone graft surgery free medical journals Glenoid bone graft surgery famous journals Glenoid bone graft surgery Google Scholar indexed journals Randomized clinical trials articles Randomized clinical trials Research articles Randomized clinical trials review articles Randomized clinical trials PubMed articles Randomized clinical trials PubMed Central articles Randomized clinical trials 2023 articles Randomized clinical trials 2024 articles Randomized clinical trials Scopus articles Randomized clinical trials impact factor journals Randomized clinical trials Scopus journals Randomized clinical trials PubMed journals Randomized clinical trials medical journals Randomized clinical trials free journals Randomized clinical trials best journals Randomized clinical trials top journals Randomized clinical trials free medical journals Randomized clinical trials famous journals Randomized clinical trials Google Scholar indexed journals Bone grafting articles Bone grafting Research articles Bone grafting review articles Bone grafting PubMed articles Bone grafting PubMed Central articles Bone grafting 2023 articles Bone grafting 2024 articles Bone grafting Scopus articles Bone grafting impact factor journals Bone grafting Scopus journals Bone grafting PubMed journals Bone grafting medical journals Bone grafting free journals Bone grafting best journals Bone grafting top journals Bone grafting free medical journals Bone grafting famous journals Bone grafting Google Scholar indexed journals Sport articles Sport Research articles Sport review articles Sport PubMed articles Sport PubMed Central articles Sport 2023 articles Sport 2024 articles Sport Scopus articles Sport impact factor journals Sport Scopus journals Sport PubMed journals Sport medical journals Sport free journals Sport best journals Sport top journals Sport free medical journals Sport famous journals Sport Google Scholar indexed journals Shoulder instability articles Shoulder instability Research articles Shoulder instability review articles Shoulder instability PubMed articles Shoulder instability PubMed Central articles Shoulder instability 2023 articles Shoulder instability 2024 articles Shoulder instability Scopus articles Shoulder instability impact factor journals Shoulder instability Scopus journals Shoulder instability PubMed journals Shoulder instability medical journals Shoulder instability free journals Shoulder instability best journals Shoulder instability top journals Shoulder instability free medical journals Shoulder instability famous journals Shoulder instability Google Scholar indexed journals
Article Details
1. Introduction
The rate of recurrent instability one year following first-time traumatic anterior shoulder dislocation is up to 60% [1,2]. Determining the best surgical treatments for anterior shoulder instability is debatable, with several procedures developed over time. According to studies, Bankart repair, also known as anatomic repair, is the initial procedure in cases of anterior shoulder instability, which is being extensively used in more than 90% of cases [3,4]. The popularity of open Bankart repair has led to the development of the efficient arthroscopic Bankart repair, which has a recurrence rate of 6% and a re-operation rate of 4.7%, according to a systematic review [5]. However, Burkhart et al. [6] demonstrated that the recurrence rate of instability was 67% in patients with large bone lesions (bony Bankart or Hill-Sachs) who underwent Bankart repair and 89% in contact athletes with similar diseases. This suggests that the efficiency of Bankart repair might be limited in the presence of bone lesions.
Consequently, the number of indications for bone block procedures has increased. Early studies on this type of surgery showed recurrence rates of 10% and surgical revision rates of 14% for the Latarjet technique [7-9] causing some institutions to abandon this procedure [10]. However, recent studies have shown better success rates. A systematic review by Griesser et al. [11] demonstrated a recurrence rate of 2.9% and a subluxation rate of 5.8%. Specifically, in patients with bone lesions, the Latarjet technique had a recurrence rate of 4.7%, demonstrating an advantage over Bankart repair [12]. However, the Latarjet technique is also associated with a high rate of postoperative complications, occurring in up to 30% of cases [11].
In previous studies, bone block procedures have shown lower recurrence rates and good functional results, making them more frequently indicated [6,11]. However, they are associated with complications such as neurological injury and shoulder arthrosis. Therefore, the main objective of this systematic review was to determine indications for bone grafting procedures associated with better functional results. This will help in choosing this type of surgery appropriately for shoulder instability.
Previous systematic reviews have evaluated different aspects of bone block procedures, such as return to sport [13], long-term outcomes [14] and complications [11]. However, to the best of our knowledge, no systematic review has determined indications that would lead to better functional results and lower complication rates. Therefore, we sought to analyze the current literature qualitatively and quantitatively to determine indications for bone block procedures.
Our hypothesis is that when using clinical criteria associated with radiological criteria, there would be a more adequate selection of patients.
2. Methods
2.1 Literature search strategy
This systematic review was officially registered with PROSPERO on October 23, 2020 (CRDXXXXXXXXXX). This systematic review was conducted in accordance with the International Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Electronic searches were performed using the Cochrane Library, PubMed, EMBASE, and LILACS databases in April 2023. These databases were searched following the Cochrane Collaboration, PRISMA, and Meta-analysis of Observational Studies in Epidemiology recommendations. To achieve the maximum sensitivity of the search strategy, we combined the terms “Latarjet” OR “Bristow” OR “Eden-Hybinette” OR “Bone block procedures” AND “Shoulder instability” as either keywords or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. The studies were then assessed using inclusion and exclusion criteria. There was no time limit specified for the publication date. There was no restriction on the language of publication (Appendix 1).
2.2 Selection criteria
The inclusion criteria were as follows: (1) randomized controlled trials (glenoid bone graft surgery vs. Bankart repair or glenoid bone graft surgery vs. glenoid bone graft surgery); and (2) prospective studies (cohort) in which a glenoid bone graft surgery technique was evaluated. The exclusion criteria were: (1) retrospective studies, (2) case reports (less than five cases), and (3) studies in which the inclusion criteria did not take into account radiological criteria, radiological criteria associated with clinical criteria, and arthroscopic criteria.
2.3 Data extraction and analysis
Relevant information regarding study characteristics, assessment of the methodological quality of the studies, clinical outcome measures, and follow-up time were independently collected by two authors using a pre-established form. The Downs and Black checklist [15] and the Cochrane risk of bias tool for randomized trials 16-18 were used to assess the quality of the included cohort studies and the randomized clinical trials, respectively. The Downs and Black checklist [15] ranges from 0–28, with a score of 26–28 points considered excellent, 20–25 good, 15–19 fair, and <15 as bad. Interobserver agreement (3 authors) was performed using the kappa test.
The studies were subdivided according to the main criteria used to indicate glenoid bone graft surgery.
- Radiological indications group (R) (>10% anterior glenoid wear and/or off-track lesions – evaluated by X-Rays, Computerized Tomography or Magnetic Resonance Imaging)
- Radiological and clinical indications group (R + C) (same as previous radiological indications + contact sports and/or instability severity index score (ISIS) ≥ 4)
- Arthroscopic indications group (A) (Hill-Sachs lesion with engagement)
The extracted and evaluated outcomes were: functional scores (ROWE, WOSI, Constant, SSV, SANE, Walch-Duplay, ASORS and VAS).
2.4 Statistical analysis
A significance level of 0.05 (5%) was defined. A complete descriptive analysis of the quantitative factors was performed using mean, median, standard deviation, coefficient of variation, and confidence interval. The Z test was used to compare the groups in the parameters. Owing to the qualitative characteristics of the systematic review, it was not possible to carry out a meta-analysis. The agreement between the three authors for the Downs and Black checklist [15] was measured using Fleiss’ kappa test for simultaneous analysis and Cohen’s kappa test for paired analysis [16-18].
3. Results
3.1 Search results and quality of the studies
In the electronic search conducted in April 2023, 1567 articles were identified. After applying the inclusion criteria, 43 articles were selected, and 19 were excluded (14 due to association of techniques (Bankart repair), 1 for using the same patients from another study, 4 due to non-standard inclusion criteria, and 1 due to lack of functional analysis). Thus a total of 23 articles were selected for the systematic review, which included 20 prospective cohort studies [12,19-37] and 3 randomized controlled trials [38-40]. A flow diagram based on PRISMA is shown in Figure 1. In addition, the characteristics of the included studies and their methodological quality are presented in Table 1.
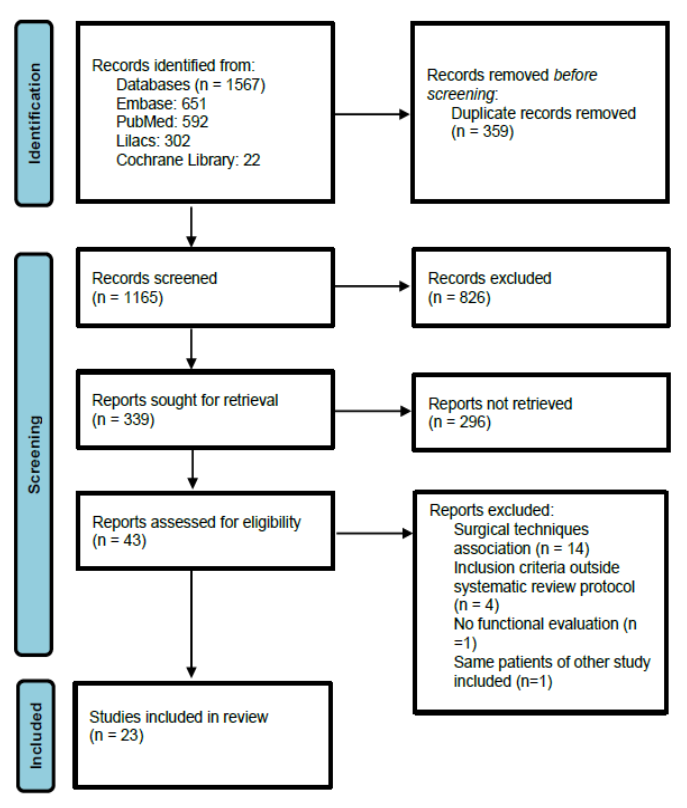
Figure 1: Flow diagram based on PRISMA.
Table 1: Characteristics of the included studies and their methodological quality.
|
Kappa |
P-value |
Inferior limit |
Superior limit |
|
|
Fleiss |
0,842 |
<0,001 |
0,719 |
0,965 |
|
A1 × A2 |
0,882 |
<0,001 |
0,760 |
1000 |
|
A1 × A3 |
0,843 |
<0,001 |
0,706 |
0,980 |
|
A2 × A3 |
0,803 |
<0,001 |
0,656 |
0,950 |
|
A1: First author |
||||
Table 2: Author’s agreement.
Of the 20 included cohort studies that were assessed using the Downs and Black checklist [15], 14 (70%) were classified as weak, five (25%) as regular, and one (5%) as good. The randomized controlled trials were assessed using the Cochrane risk of bias tool for randomized trials [16-18] (Appendix 2). Regarding the authors' agreement, the Fleiss’ kappa test of the three authors showed a value of 0.842, which was classified as excellent. Table 2 presents the complete results.
3.2 Demographics
In total, the studies involving 1306 shoulders were included, of which 1105 (84,60%) belonged to males, 159 (12,17%) females, and 42 (3,23%) had no specification of sex in the study. The mean follow-up was 40.19 months (18.5–90 months). It was not possible to calculate the mean age since it was not mentioned in any of the studies.
3.3 Indications
10 included studies [21,25-28,32,34,37,38,40] used only radiological criteria and contained a total of 405 shoulders. 10 included studies [19,20,22-24,29,31,33,35,39] used clinical and radiographic criteria, with 673 shoulders. Three included studies [12,30,36] used arthroscopic criteria, with a total of 228 shoulders.
3.4 Surgical technique
Different surgical techniques were described in the articles selected for this systematic review and were performed according to the surgeons' preferences and experiences. The open Latarjet technique was performed in 1003 (76,79%) shoulders, arthroscopic Latarjet technique in 159 (12,17%) shoulders, open distal tibia graft in 50 (3,82%) shoulders, open Bristow technique in 48 (3,67%) shoulders, and open Eden–Hybinette technique in 46 (3,52%) shoulders.
3.5 Functional and pain scores
All functional scores improved postoperatively. Clinical outcomes were evaluated using ROWE in 13 studies [12,19,20,23,25,28-30,33,35,37,40], WOSI in nine studies [20,22,24,27,31,33,35,36,39], ASES in eight studies [26,27,28,32,33,37,39,40], Constant in seven studies [12,21,25,33,35,37,40], SANE in five studies [24,26,27,32,36], Walch-Duplay in four studies [12/29/30/34], SSV in three studies [28,30,33] and ASORS in one study [39]. In addition, the pain was assessed using the visual analog pain scale in 12 studies [20,21,26,27,29,30,31,32,33,36,38,39]. The complete results are shown in Table 3.
|
N |
ROWE |
WOSI |
Constant |
Walch-Duplay |
SANE |
SSV |
VAS |
|
|
Group R |
||||||||
|
Abouelsoud and Abdelrahman [38] |
16 |
84,62 |
NE |
NE |
NE |
NE |
NE |
3.88 |
|
Auffarth et al. [21] |
46 |
94.3 |
NE |
93.5 |
NE |
NE |
NE |
0.6 |
|
Ebrahimzadeh et al. [25] |
36 |
95.7 |
NE |
96.6 |
NE |
NE |
NE |
NE |
|
Erickson et al. [26] |
21 |
NE |
NE |
NE |
NE |
84 |
NE |
0.9 |
|
Frank et al. [27] |
100 |
NE |
0.849 |
NE |
NE |
88.06 |
NE |
1.13 |
|
Gouch et al. [28] |
50 |
88 |
NE |
NE |
NE |
NE |
89 |
NE |
|
Mook et al. [32] |
38 |
NE |
NE |
NE |
NE |
87 |
NE |
NE |
|
Omidi-Kashani et al. [34] |
35 |
NE |
NE |
NE |
89.24 |
NE |
NE |
NE |
|
Zarezade et al. [40] |
19 |
87.4 |
NE |
58.7 |
NE |
NE |
NE |
NE |
|
Zhu et al. [37] |
44 |
97.1 |
NE |
96.5 |
NE |
NE |
NE |
NE |
|
Total/Means/SD |
405 |
91.9 (6.3) |
84.90% (14.6%) |
87.07 (5.12) |
89.2 (10) |
87.27 (13.1) |
89 (23) |
2.18 (1.7) |
|
Group R + C |
||||||||
|
Abdelhady et al. [19] |
14 |
91.07 |
NE |
NE |
NE |
NE |
NE |
NE |
|
Ali et al. [20] |
48 |
79 |
0.7338 |
NE |
NE |
NE |
NE |
1.75 |
|
Belangero et al. [39] |
41 |
NE |
0.7438 |
NE |
NE |
NE |
NE |
1.88 |
|
Bohu et al. [22] |
46 |
NE |
75,79% |
NE |
NE |
NE |
NE |
NE |
|
Cautiero et al. [23] |
26 |
94.7 |
NE |
NE |
NE |
NE |
NE |
NE |
|
Di Giacomo et al. [24] |
344 |
NE |
0.5565 |
NE |
NE |
88 |
NE |
NE |
|
Kordasiewicz et al. [29] |
47 |
87.8 |
NE |
NE |
83.9 |
NE |
NE |
0.77 |
|
Marion et al. [32] |
58 |
NE |
0.804 |
NE |
NE |
NE |
NE |
1.85 |
|
Moroder et al. [33] |
25 |
77 |
73,52% |
65 |
NE |
NE |
70 |
1.4 |
|
Vadala et al. [35] |
24 |
93.8 |
0.94 |
95.6 |
NE |
NE |
NE |
NE |
|
Total/Mean/SD |
673 |
85.4 |
0.854 |
79.98 |
83.9 |
88 |
70 (22) |
1.27 (1.78) |
|
Group A |
||||||||
|
Burkhart et al. [12] |
47 |
NE |
NE |
94.4 |
91.7 |
NE |
NE |
NE |
|
Kordasiewicz et al. [30] |
90 |
81 |
NE |
NE |
79 |
NE |
90 |
1 |
|
Yang et al. [36] |
91 |
NE |
0.7392 |
NE |
NE |
85.3 |
NE |
1.69 |
|
Total/Mean/SD |
228 |
81 (18,5) |
73.92% (13%) |
94.4 (5) |
83.35 (11.1) |
85.3 (9.6) |
90 (11.5) |
1.15 (1.92) |
Table 3: Functional and pain scores.
3.6 Comparisons between the evaluated groups
Functional and pain scores
The following parameters were evaluated in all groups:
- ROWE
The better results were found in group R, with a statistically significant difference compared with the other groups. The results are shown in Table 4.
|
Mean |
SD |
N |
|
|
Group R |
91,9 |
6,3 |
229 |
|
Group R + C |
85,4 |
12,3 |
137 |
|
Group A |
83,3 |
18,5 |
137 |
|
Grp R |
Grp R+C |
||
|
ROWE |
Grp R |
||
|
Grp R+C |
<0,001 |
||
|
Grp A |
<0,001 |
0,267 |
|
|
SD: Standard deviation; Grp: Group |
|||
Table 4: ROWE Functional results.
- WOSI
The better results were found in groups R and R+C, with a statistically significant difference compared with the group A. The results are shown in Table 5.
|
Mean |
SD |
N |
||
|
WOSI |
Grp R |
84,90% |
14,60% |
100 |
|
Grp R + C |
85,40% |
15,70% |
600 |
|
|
Grp A |
0.7392 |
13,00% |
91 |
|
|
Grp R |
Grp R+C |
|||
|
WOSI |
Grp R+C |
0,753 |
||
|
Grp A |
<0.001 |
<0.001 |
||
|
SD: Standard deviation Grp: Group |
||||
Table 5: WOSI functional results.
- CONSTANT
The better results were found in group A, with a statistically significant difference compared with the other groups. The results are shown in Table 6.
|
Mean |
SD |
N |
|
|
Group R |
87,07 |
5,12 |
145 |
|
Group R + C |
79,98 |
10,5 |
49 |
|
Group A |
94,4 |
5 |
47 |
|
Grp R |
Grp R+C |
||
|
CONSTANT |
Grp R+C |
<0,001 |
|
|
Grp A |
<0,001 |
<0,001 |
|
|
SD: Standard deviation; Grp: Group |
|||
Table 6: Constant functional results.
- d) SSV
The better results were found in groups R and A, with a statistically significant difference compared to group (R + C). The results are shown in Table 7.
|
Mean |
SD |
N |
|
|
Group R |
89 |
23 |
50 |
|
Group R + C |
70 |
22 |
25 |
|
Group A |
90 |
11,5 |
90 |
|
Grp R |
Grp R+C |
||
|
SSV |
Grp R+C |
<0,001 |
|
|
Grp A |
0,773 |
<0,001 |
|
Table 7: SSV – functional outcomes.
- e) SANE
The better results were found in the (R + C) group, with a statistically significant difference observed only in group A. The results are shown in Table 8.
|
Mean |
SD |
N |
|
|
Group R |
87,27 |
13,1 |
159 |
|
Group R + C |
88 |
13 |
358 |
|
Group A |
85,3 |
9,6 |
91 |
|
Grp R |
Grp R+C |
||
|
SANE |
Grp R+C |
0,558 |
|
|
Grp A |
0,174 |
0,057 |
|
Table 8: SANE – functional outcomes.
- f) VAS
The better results were found in groups (R + C) and A, with a statistically significant difference compared with group R. The results are shown in Table 9.
|
Mean |
SD |
N |
|
|
Group R |
2,18 |
1,70 |
274 |
|
Group R + C |
1,27 |
1,78 |
325 |
|
Group A |
1,15 |
1,92 |
181 |
|
Grp R |
Grp R+C |
||
|
VSA |
Grp R+C |
0,003 |
|
|
Grp A |
0,001 |
0,516 |
|
Table 9: Visual Scale Analogic of pain – results.
ASES, Walch-Duplay and ASORS were not evaluated in all the groups and a comparison was not possible to be done.
The summary of functional and pain scores’ results are shown in Table 10.
|
Statistically better results |
Statistically worse results |
|
|
ROWE |
Group R |
|
|
WOSI |
Group R |
Group A |
|
Group R + C |
||
|
Constant |
Group A |
Group R + C |
|
SSV |
Group R |
Group R + C |
|
Group A |
||
|
SANE |
Group R + C |
Group A |
|
VAS |
Group R + C |
Group R |
|
Group A |
Table 10: Summary of functional and pain scores.
4. Discussion
In this systematic review, 23 studies were included, comprising 1320 shoulders. Only prospective studies were included in which the indications for choosing glenoid bone graft procedures for shoulder instability were explicitly described to avoid selection bias that may occur in retrospective studies. However, the analysis of the included studies showed a low methodological quality. As a result, the indications for choosing bone grafting procedures are highly variable in the literature and are controversial. This systematic review aimed to determine the criteria for choosing bone grafting procedures that would lead to better functional results. Hence, we divided the indications into three types: radiological, clinical and radiological, and arthroscopic.
Among the subgroups of indications included in this systematic review, the largest number of shoulders undergoing the glenoid bone graft procedure was the group of radiological indications associated with clinical indications (636 shoulders). In general, variable results were observed, with no group showing better results for all variables studied.
In the radiological indication group (R group), the indications were 10–25% anterior glenoid wear and/or off-track injury. According to Burkhart et al. [6], glenoid bone loss has become a significant risk factor for recurrent instability after Bankart repair. Initially, the critical amount of glenoid bone loss was believed to be 25% [6,41]. However, a recent cadaver study suggested that a 20% defect decreased shoulder stability after the Bankart surgery [42]. Yamamoto et al. [43] performed a study to assess the subcritical bone loss that would lead to postoperative instability and found a glenoid bone loss of 17–25%.
As described by Giacomo et al. [44], it is important to assess both glenoid and humeral bone loss, and there is a relationship between them, as well as the measurements of the glenoid track. Recent biomechanical studies on bipolar bone loss and the glenoid track concept have revealed a significant decrease in shoulder stability, with glenoid defects as small as 10-15% [45].
In the (R + C) group, studies were included in which the indications were the same as the R group, in addition to the practice of contact sports and/or ISIS ≥ 4. The score takes into account clinical and gradiological criteria. Initially, starting from a score of 6, glenoid bone graft surgery was indicated, and above this score, a failure rate of 70% was reported in a retrospective study by the authors who performed anatomical surgery [46]. It is noteworthy that this score uses radiographs for indication, and in our study, only three included studies used radiographs for deciding which surgery to indicate. Currently, the glenoid track instability management score (GTIMS) has been derived [44], which incorporates the glenoid track concept into the (ISIS) using only tomography as a radiological parameter and not radiographs as in ISIS. Patients with an on-track injury score of 0 and off-track injuries scored 4 points. The rest of the parameters evaluated were equal to the ISIS, and scores equal to or greater than 4 indicated glenoid bone graft surgery. It is worth mentioning that in the GTIMS, the presence of an off-track lesion already scores 4 points indicating glenoid bone graft surgery, without the need for evaluation of other parameters.
In group A, the main indication was the presence of a Hill-Sachs lesion with engagement. We consider this mode of indication valid since it also allows the evaluation of associated injuries, but as a critical mode, we can mention that with the patient anesthetized, there may be an over-indication of glenoid bone graft surgery. Therefore, we believe that the indication for glenoid bone graft surgery should be made in advance based on the patient's clinical and radiological data. If arthroscopy is feasible, it should be performed to evaluate associated injuries. This group of patients presented variable results in the evaluated parameters; however, it presented good results in the evaluated functional scores. One hypothesis for these findings is that there was an over-indication of cases, and patients who did not need glenoid graft surgery were administered this treatment modality.
Regarding the functional scores, we observed that the groups A, R and R+C had the same amount of statistically better results in the functional scores, whereas the (R + C) group had a greater number of statistically worse results. Regarding the functional scores that are specific for shoulder instability (ROWE and WOSI), the Group R had statistically better results in both. This highlights the variability of the functional scores used to evaluate the results of bone grafting procedures.
The Rowe questionnaire [47] assesses functional results in the anterior shoulder instability postoperatively. It consists of 100 points divided into three domains: 1) stability (50 points), 2) mobility (20 points), and 3) function (30 points). The score is considered excellent when it ranges from 90–100 points, good (89–75), regular (74–51), and poor when <50 points. Only the R group presented with an excellent score (average: 91.9). Groups A and (R + C) showed good results (averages: 85.4 and 83.3 respectively). It is worth mentioning that all groups showed good results with the surgery, with the groups R showing statistically better results than the other groups.
The Western Ontario Shoulder Instability Index (WOSI) [48] is a quality of life (QOL) questionnaire that was prepared and validated for application in patients with shoulder instability. It encompasses aspects of the QOL relevant to this disease. It contains 21 questions spanning four domains: 1) physical symptoms; 2) sports, recreation, and work; 3) lifestyle; and 4) emotional state. All the groups presented results above 80% and the groups R and R+C had statistically better results when compared to group A.
The Constant Murley score [49] is a non-specific scale including different domains of shoulder function (pain, activities of daily living, range of motion, and power). Higher scores represent a better function. This questionnaire is composed of four subscales: three self-reported subscales and a shoulder lift force subscale, which is performed by an external evaluator. The better results were found in group A (average: 94.4), which presented statistically better results compared to the group (R + C) (average: 79.98) but showed no statistical significance compared to group R (average: 87.07). This score is not specific for instability; therefore, it has a less practical effect in comparing results.
The subjective shoulder score (SSV) [50] is defined as the patient's subjective assessment of shoulder function and is expressed as a percentage of the score of a normal shoulder. The scores ranged from 0 to 100. The better results were found in group A (average: 90), with statistical significance compared to the (R + C) group (average: 70) and without statistical significance compared to the R group (average: 89).
The single assessment numeric evaluation (SANE) [51] is a score in which patients respond with a whole number to the question ‘On a scale of 0 to 100, how would you rate your injured limb?’ It is normally used as global classification of functions, and the definition of normality is determined by the individual patient. Since the SANE is assessed at baseline and during follow-up, it can be used to assess changes in function (i.e., recovery) during this period. The better results were found in the (R + C) group, with a statistically significant difference observed only in group A. Regarding the visual analog scale, the better results were found in groups R and A.
An important aspect to be evaluated is that, among the scores evaluated, only ROWE [47] and WOSI [48] are specific for shoulder instability. In the ROWE [47] assessment, the R group presented the better results with statistical significance, and in the WOSI [48] assessment, the groups R and R+C had statistically better results. We hypothesized that the (R + C) group would present better results, but this was not the case. Although we found variable results in the systematic review, the (R + C) patients presented the highest statistically worse results for the evaluated parameters (Constant, SSV). We believed that when using clinical criteria associated with radiological criteria, there would be a more adequate selection of patients; however, according to the results, the groups of radiological and arthroscopic indications presented better results. Regarding the ROWE [47] score, the R group presented the better results with statistical significance. As a result, when considering only radiological criteria for indication, there were better results. Therefore, there is doubt whether the clinical parameters have little influence or, instead, the clinical criteria used may not be the most relevant for surgical indication.
In previous studies, glenoid bone graft surgery has shown good functional results, despite a relatively high complication rate [11]. The objective of our study was to determine which surgical indications present better functional results since this surgery is indicated in many cases in active young patients and/or athletes in whom the expectation from surgery is high. Our study seeks to help by suggesting the better indications to have the best possible results with the treatment.
The overall quality of the studies was uniformly low. This is a factor that influenced the results of systematic reviews and meta-analyses. Most of the included studies were classified by the Downs and Black score [15] as weak (15 studies) or regular (5 studies), with only one study rated as good.
Limitations of this systematic review: the parameters evaluated in the studies and the types of surgeries were considerably variable. The techniques used by the surgeons in the studies and the indications in each subgroup were not equal in the selected studies. The other limitations of this study are consistent with those of the systematic reviews. The patient population included a wide selection of patients of different ages, functional demands, frequency of instability episodes, and time to surgery, making it challenging to apply the results to a particular patient. Nevertheless, our systematic review is the first to determine indications for glenoid bone graft surgery that would lead to better functional outcomes in prospective studies.
5. Conclusion
The radiological indications group presented the better results in the specific scores for shoulder instability and the radiological + clinical indications group presented the biggest amount of worse results in the parameters evaluated.
Author Contributions:
All authors made a significant contribution to the work reported (conception, study design, execution, acquisition of data, analysis and/or interpretation). All authors have drafted, written, and/or substantially revised and/or critically reviewed the article. All authors have agreed on the journal to which the article will be submitted. All authors reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. All authors agree to take responsibility and be accountable for the contents of the article.
Ethical Approval:
This study was submitted to the ethics committee of the Federal University of São Paulo 9738310820- (Universidade Federal de São Paulo – UNIFESP).
Funding:
There was no funding to the development of this study.
References
- Olds M, Ellis R, Donaldson K, et al. Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med 49 (2015): 913-922.
- Robinson CM, Howes J, Murdoch H, et al. Functional outcome and risk of recurrent instability after primary traumatic anterior dislocation in young patients. J Bone Joint Surg Am 88 (2006): 2326-2336.
- Berendes TD, Pilot P, Nagels J, et al. Survey on the management of acute first-time anterior shoulder dislocation amongst Dutch public hospitals. Arch Orthop Trauma Surg 135 (2015): 447-454.
- Chong M, Karataglis D, Learmonth D. Survey of the management of acute traumatic first-time anterior shoulder dislocation among trauma clinicians in the UK. Ann R Coll Surg Engl 88 (2006): 454-458.
- Petrera M, Patella V, Patella S, et al. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc 18 (2010): 1742-1747.
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 16 (2000): 677-694.
- Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 80 (1998): 841-852.
- Ferlic DC, DiGiovine NM. A long-term retorspective study of the modified Bristow procedure. Am J Sports 16 (1998): 469-474.
- Torg JS, Balduini FC, Bonci C, et al. A modified Bristow-Helfet-May procedure for recurrent dislocation and subluxation of the shoulder. Report of two hundred and twelve cases. J Bone Joint Surg Am 69 (1987): 904-913.
- Weaver JK, Derkash RS. Don’t forget the Bristow-Latarjet procedure. Clin Orthop Relat Res 308 (1994): 102-110.
- Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg 22 (2013): 286-292.
- Burkhart SS, De Beer JF, Barth JRH, et al. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 23 (2007): 1033-1041.
- Hurley ET, Montgomery C, Jamal MS, et al. Return to Play Aafter Latarjet Procedure for Anterior Shoulder Instability: A Systematic Review. Am J Sports Med 47 (2019): 3002-3008.
- Gilat R, Lavoie-Gagne O, Haunschild ED, et al. Outcomes of the Latarjet procedure with a minimum 5- and 10-year follow-up: A systematic review. Shoulder Elbow 12 (2020): 315-329.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52 (1998): 377-384.
- Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64 (2011): 401-406.
- Higgins JPT, Altman DG, Gotzsche PC, et al. Cochrane bias methods group Cochrane statistical methods group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343 (2011): d5928.
- Higgins JPT, Savovic J, Page MJ, et al. Revised Cochrane risk-of-bias toll for randomized trials (RoB 2) 2019. Available at www.riskofbias.info. Accessed May 25, 2020.
- Abdelhady A, Abouelsoud M, Eid M. Latarjet prcodeure in patients with multiple recurrent anterior shoulder dislocation and generalized ligamentous laxity. Eur J Orthop Surg Traumatol 25 (2015): 705-708.
- Ali J, Altintas B, Pulatkan A, et al. Open Versus Arthroscopic Latarjet Procedure for the Treatment of Anterior Glenohumeral Instability With Glenoid Bone Loss. Arthroscopy 36 (2020): 940-949.
- Auffarth A, Schauer J, Matis N, et al. The J-bone graft for anatomical glenoid reconstruction in recurrent posttraumatic anterior shoulder dislocation. Am J Sports Med 36 (2008): 638-647.
- Bohu Y, Klouche S, Gerometta A, et al. Outpatient Latarjet surgery for gleno-humeral instability: Prospective comparative assessment of feasibility. Orthop Traumatol Surg Res 102 (2016): 507-512.
- Cautiero F, Russo R, Di Pietto F, et al. Computerized tomographic assessment and clinical evaluation in shoulder instability treated with the Latarje-Patte procedure using one screw and washer. Muscles Ligaments Tendon J 7 (2017): 26-33.
- Di Giacomo G, Peebles LA, Midtgaard KS, et al. Risk Factors for Recurrent Anterior Glenohumeral Instability and Clinical Failure Following Primary Latarjet Procedures: An Analysis of 344 Patients. J Bone Joint 102 (2020): 1665-1671.
- Ebrahimzadeh MH, Moradi A, Zarei AR. Minimally invasive modified latarjet procedure in patients with traumatic anterior shoulder instability. Asian J Sports Med 6 (2015): e26838.
- Erickson BJ, Shishani Y, Jones S, et al. Clinical and radiographic outcomes after Latarjet using suture-button fixation. JSES Int 5 (2020): 175-180.
- Frank RM, Romeo AA, Richardson C, et al. Outcomes of Latarjet versus Distal Tibia Allograft for Anterior Shoulder Instability Repair: A Matched Cohort Analysis. Am J Sports Med 46 (2018): 1030-1038.
- Gough A, Guyver P, Franklin M, et al. The Latarjet Procedure for Anterior Shoulder Instability: A Consecutive Prospective Series of 50 Cases. Acta Orthop Belg 83(2017): 599-604.
- Kordasiewicz B, Malachowski K, Kicinski M, et al. Comparative study of open and arthroscopic coracoid transfer for shoulder anterior instability (Latarjet)-clinical results at short term follow-up. Int Orthop 41 (2017): 1023-1033.
- Kordasiewicz B, Kicinski M, Malachowski K, et al. Arthroscopic Latarjet Stabilization: Analysis of the Learning Curve in the First 90 Primary Cases: Early Clinical Results and Computed Tomography Evaluation. Arthroscopy 35 (2019): 3221-3237.
- Marion B, Klouche S, Deranlot J, et al. A Prospective Comparative Study of Arthroscopic Versus Mini-Open Latarjet Procedure with a Minimum 2-Year Follow-up. Arthroscopy 33 (2017): 269-277.
- Mook WR, Petri M, Greenspoon JA, et al. Clinical and Anatomic Predictors of Outcomes after the Latarjet Procedure for the Treatment of Anterior Glenohumeral Instability with Combined Glenoid and Humeral Bone Defects. Am J Sports Med 44 (2016): 1407-1416.
- Moroder P, Stefanitsch V, Auffarth A, et al. Treatment of recurrent anterior shoulder instability with the Latarjet or Bristow procedure in older patients. J Shoulder Elbow Surg 27 (2018): 824-830.
- Omidi-Kashani F, Sadri-Mahvelati E, Mazlumi SM, et al. Is Bristow-Latarjet operation effective for every recurrent anterior shoulder dislocation? Arch Iran Med 11 (2008): 270-273.
- Vadalà A, Lanzetti RM, De Carli A, et al. Latarjet procedure: evolution of the bone block and correspondente clinical relevance-a clinical and radiological study. Musculoskelet Surg 101 (2017): 113-120.
- Yang JS, Mehran N, Mazzocca AD, et al. Remplissage versus Modified Latarjet for Off-Track Hill-Sachs Lesions with Subcritical Glenoid Bone Loss. Am J Sports Med 46 (2018): 1885-1891.
- Zhu Y, Jiang C, Song S. Arthroscopic versus Open Latarjet in the Treatment of Recurrent Anterior Shoulder Dislocation with Marked Glenoid Bone Loss: A Prospective Comparative Study. Am J Sports Med 45 (2017): 1645-1653.
- Abouelsoud MM, Abdelrahman AA. Recurrent anterior shoulder dislocation with engaging Hill-Sachs defect: remplissage or Latarjet? Eur Orthop Traumatol 6 (2015): 151-156.
- Belangero PS, Lara PHS, Figueiredo EA, et al. Bristow versus Latarjet in high-demand athletes with anterior shoulder instability: a prospective randomized comparison. JSES Int 5 (2021): 165-170.
- Zarezade A, Dehghani M, Rozati AR, et al. Comparison of Bristow procedure and Bankart arthroscopic method as the treatment of recurrent shoulder instability. Adv Biomed Res 3 (2014): 256.
- Lo IK, Nonweiler B, Woolfrey M, et al. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med 32 (2): 301-307.
- Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect. On anterior shoulder stability: A Cadaveric study. Am J Sports Med 37 (2009): 949-954.
- Yamamoto N, Kawakami J, Hatta T, et al. Effect of subcritical glenoid bone loss on activities of daily living in patients with anterior shoulder instability. Orthop Traumatol Surg Res 105 (2019): 1467-1470.
- Di Giacomo G, Peebles LA, Pugliese M, et al. Glenoid Track Instability Management Score: Radiographic Modification of the Instability Severity Index Score. Arthroscopy 36 (2020): 56-57.
- Gottschalk LJ, Walia P, Patel RM, et al. Stability of the Glenohumeral Joint with Combined Humeral Head and Glenoid Defects: A Cadaveric Study. Am J Sports Med 44 (2016): 933-940.
- Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 89 (2007): 1470-1477.
- Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am 60 (1978): 1-16.
- Kirkley A, Griffin S, McLintock H, et al. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability. The Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med 26 (1998): 764-772.
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214 (1987): 160-164.
- Gilbart MK, Gerber C. Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg 16 (2007): 717-721.
- Williams GN, Gangel TJ, Arciero RA, et al. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med 27 (1999): 214-221.
Appendix File:
Appendix 1:
Literature search strategy
MEDLINE (Pubmed)
(((((dislocation, shoulder[MeSH Terms]) AND (Latarjet[Text Word])) OR (Bristow[Text Word])) OR (Eden-Hybinette[Text Word])) OR (Bone block procedures[Text Word])) OR (Coracoid transfer[Text Word])
EMBASE (Elsevier)
('shoulder dislocation'/exp OR 'shoulder dislocation') AND 'latarjet procedure':ti,ab,kw OR 'bristow procedure':ti,ab,kw OR 'eden hybinette':ti,ab,kw OR 'bone block procedures':ti,ab,kw OR 'coracoid transfer':ti,ab,kw
LILACS
(( (mh:luxação do ombro) OR (luxación glenohumeral) OR (dislocation, glenohumeral) OR (dislocation, shoulder) OR (dislocations, glenohumeral) OR (dislocations, shoulder) OR (glenohumeral dislocation) OR (glenohumeral dislocations) OR (glenohumeral subluxation) OR (glenohumeral subluxations) OR (shoulder dislocations) OR (subluxation, glenohumeral) OR (subluxations, glenohumeral) OR mh:c05.550.518.750* OR mh:c26.289.750* OR mh:c26.803.125*) AND (latarjet) OR (bristow) OR (eden-hybinette ) OR (bone block procedures ) OR (coracoid transfer) AND ( db:("LILACS")) (mh:luxação do ombro) OR (luxación glenohumeral) OR (dislocation, glenohumeral) OR (dislocation, shoulder) OR (dislocations, glenohumeral) OR (dislocations, shoulder) OR (glenohumeral dislocation) OR (glenohumeral dislocations) OR (glenohumeral subluxation) OR (glenohumeral subluxations) OR (shoulder dislocations) OR (subluxation, glenohumeral) OR (subluxations, glenohumeral) OR mh:c05.550.518.750* OR mh:c26.289.750* OR mh:c26.803.125*) AND (latarjet) OR (bristow) OR (eden-hybinette ) OR (bone block procedures ) OR (coracoid transfer) AND ( db:("LILACS"))
The Cochrane Library
#1 Shoulder dislocation: ti,ab,kw
#2 Latarjet: ti,ab,kw
#3 Bristow: ti,ab,kw
#4 Eden-Hybinette: ti,ab,kw
#5 Bone block procedures: ti,ab,kw
#6 Coracoid transfer: ti,ab,kw
#7 (#1 AND #2 OR #3 OR #4 OR #5 #6)
Appendix 2:
|
1=Low risk of bias/2=High risk of bias/3=nuclear risk of bias |
||
|
Study Abouelsoud 2015 |
||
|
Author 1 |
||
|
Random sequence generation |
1 |
|
|
Allocation concealment |
1 |
|
|
Blinding of participants and personnel |
3 |
|
|
Blinding of outcome assessment |
2 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
1 |
|
|
Other bias |
3 |
|
|
Author 2 |
||
|
Random sequence generation |
1 |
|
|
Allocation concealment |
1 |
|
|
Blinding of participants and personnel |
3 |
|
|
Blinding of outcome assessment |
3 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
1 |
|
|
Other bias |
3 |
|
|
Author 3 |
||
|
Random sequence generation |
1 |
|
|
Allocation concealment |
1 |
|
|
Blinding of participants and personnel |
2 |
|
|
Blinding of outcome assessment |
3 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
1 |
|
|
Other bias |
3 |
|
|
Belangero 2021 Author 1 |
||
|
Random sequence generation |
1 |
|
|
Allocation concealment |
1 |
|
|
Blinding of participants and personnel |
2 |
|
|
Blinding of outcome assessment |
1 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
1 |
|
|
Other bias |
3 |
|
|
Author 2 |
||
|
Random sequence generation |
1 |
|
|
Allocation concealment |
1 |
|
|
Blinding of participants and personnel |
3 |
|
|
Blinding of outcome assessment |
1 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
1 |
|
|
Other bias |
3 |
|
|
Author 3 |
||
|
Random sequence generation |
1 |
|
|
Allocation concealment |
1 |
|
|
Blinding of participants and personnel |
2 |
|
|
Blinding of outcome assessment |
1 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
1 |
|
|
Other bias |
3 |
|
|
Zarezade 2014 |
||
|
Author 1 |
||
|
Random sequence generation |
2 |
|
|
Allocation concealment |
2 |
|
|
Blinding of participants and personnel |
3 |
|
|
Blinding of outcome assessment |
3 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
3 |
|
|
Other bias |
3 |
|
|
Author 2 |
||
|
Random sequence generation |
2 |
|
|
Allocation concealment |
3 |
|
|
Blinding of participants and personnel |
3 |
|
|
Blinding of outcome assessment |
3 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
3 |
|
|
Other bias |
3 |
|
|
Author 3 |
||
|
Random sequence generation |
2 |
|
|
Allocation concealment |
2 |
|
|
Blinding of participants and personnel |
3 |
|
|
Blinding of outcome assessment |
3 |
|
|
Incomplete outcome data |
1 |
|
|
Selective reporting |
3 |
|
|
Other bias |
3 |
|
